Abstract
Purpose
To report a case of combined central retinal vein occlusion (CRVO) with cilioretinal artery occlusion (CLRAO) that heralded the development of frosted branch angiitis (FBA).
Case report
A 25-year-old healthy male presented with sudden painless visual loss in his left eye with a visual acuity (VA) of 20/300. Fundus exam and fluorescein angiography showed signs of combined CRVO and CLRAO. Without treatment, his vision gradually improved until it reached 20/30 within four months. Five months after initial presentation, he returned with severe visual loss (20/400) in the same eye and a clinical picture of severe occlusive periphlebitis resembling a frosted branch angiitis pattern associated with severe macular edema. This was promptly and successfully treated with systemic steroids and immunosuppressive medications.
Conclusion
CRVO in young population can have an unusual course and one should carefully rule out underlying uveitic etiologies in each visit. Clinical suspicion and close follow‑up are required for early detection and timely management of FBA.
Similar content being viewed by others
Introduction
Frosted branch angiitis (FBA) is a rare form of retinal vasculitis characterized by a fulminant retinal perivascular sheathing involving the venules (and occasionally both arterioles and venules), with varying degrees of uveitis, macular edema (ME) and visual loss [1,2,3].
To the best of our knowledge, there are only about 11 reported cases of FBA associated with central retinal vein occlusion (CRVO). In all of these cases, the vascular occlusion developed either concurrent or subsequent to FBA. We report the first case in which a combined CRVO and cilioretinal artery occlusion (CLRAO) preceded the development of FBA.
Case report
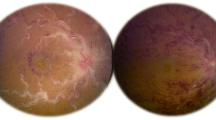
A 25-year-old healthy male presented to our clinic in 2018 with sudden painless loss of vision in the left eye (OS). The visual acuity (VA) was 20/300 at presentation. The patient had no history of recent systemic illness or vaccinations. Examination findings included normal anterior segment, clear vitreous, optic disc hyperemia, dilated and tortuous retinal veins along with retinal ischemic whitening of the cilioretinal artery territory (Fig. 1a). Fundus fluorescein angiography (FFA) revealed delayed venous filling and delayed emptying, and impaired filling of the cilioretinal artery, confirming the diagnosis of combined non-ischemic CRVO and CLRAO (Fig. 1b and c). Examination of the fellow eye was unremarkable (Fig. 1d), and remained unremarkable to the last follow-up. Systemic evaluation including blood pressure, fasting blood sugar, complete blood cell count (CBC), hemoglobin, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), urea, electrolytes, coagulation profile, cryoglobulins, antiphospholipid antibodies, factor V Leiden mutation, protein C and S levels, antithrombin III mutation, prothrombin mutation, homocysteine levels, serum protein electrophoresis, carotid ultrasound, and echocardiogram revealed no obvious abnormalities. His VA continued to improve, reaching 20/30 in four months. Five months following the initial presentation, he returned with a severe visual loss (20/400) in the left eye. He also had ciliary injection and an inflammatory anterior chamber reaction with a hypopyon of 0.2 mm height. Mild vitritis was also present accompanied by severe periphlebitis in a frosted branch pattern (Fig. 2a). A repeated FFA showed severe generalized retinal capillary non-perfusion sparing the macula (Fig. 2b and c). Spectral domain optical coherence tomography (SD-OCT) revealed a newly formed severe ME (Fig. 2d). Upon further detailed questioning, the patient recalled suffering from occasional oral ulcers. There was no history of genital ulcers, erythema nodosum of the skin, joint pain, neurological, nor gastrointestinal symptoms. The combined presence of oral and ocular lesions indicates a diagnosis of Behcet’s disease based on the international criteria for Behçet's disease [4].
Imaging at initial presentation. a Color fundus photograph of the left eye showing dilated tortuous veins, swollen optic disc, and ischemic retinal whitening at the distribution of cilioretinal artery, Note: the two white areas above the superior retinal arcades represent a reflection artefact from the fundus camera. b A fluorescein angiogram showing disc leakage, with no abnormal vascular leakage or capillary non-perfusion (note: consecutive angiography frames revealed an obvious delay in the venous filling). c SD-OCT image showing inner retinal hyperreflectivity and thickening involving the nasal macula in the left eye. d Color fundus photo and fluorescin angiogram image of the normal right eye
Imaging five months after the initial presentation. a The same eye shows increased disc edema with hyperemia, macular edema, and thick perivascular sheathing along the major vessels (predominantly venous), typical of frosted branch angiitis. b and c Early and late fluorescein angiograms revealed extensive retinal capillary non-perfusion and leakage from the optic nerve head and retinal veins. d SD-OCT shows severe macular edema
The patient was admitted to the hospital for further investigation and management. Full medical examination was unremarkable; there were no clinical signs of lymphoma, leukemia, sarcoidosis, tuberculosis, multiple sclerosis, systemic lupus erythematosus, or other autoimmune diseases. Laboratory tests were carried out, including CBC, renal and liver function tests, angiotensin converting enzyme level, CRP, ESR, serum protein electrophoresis, HLA-B51, autoimmune markers (anticardiolipin antibodies, anti-neutrophil cytoplasmic antibodies, antinuclear antibodies, antimitochondrial antibodies, rheumatoid factor, anti-double-stranded DNA, anti-single stranded DNA, anti-Scl-70 antibodies, and anti-Jo-1 antibodies), and serological tests for syphilis, viral hepatitis and HIV. ESR was high 34 mm/h (baseline ESR = 7 mm/h). Results of all other tests were within normal limits or negative. Chest computed tomography scan and doppler ultrasonography of carotid arteries were also normal.
Two days later, following a negative tuberculin skin test, a pulse therapy of intravenous methylprednisolone (1 g/day for 3 days) was initiated followed by a tapering regimen of oral prednisolone (1 mg/kg) and immunosuppressive therapy (Azathioprine 1 mg/kg, increased later to 2 mg/kg). One week later, there was a marked resolution of the perivascular sheathing and retinal hemorrhages. Two months later, all signs of inflammation had resolved with a slight improvement in ME. Treatment for ME was started with monthly intravitreal bevacizumab (1.25 mg/0.05 ml), which resulted in a good response after completing the loading regimen (three injections). Five months later, the ME resurged after a period of non-compliance to maintenance immunosuppressive medications. The ME eventually resolved after additional two injections of bevacizumab followed by two injections of aflibercept (Fig. 3a) with a resultant VA of 20/25. Twelve months from commencing immunosuppressive therapy, there were no signs of inflammation (Fig. 3b and c). Later, sector laser photocoagulation was applied to the ischemic retina when small tufts of retinal neovascularization were noted.
Imaging following treatment. a SD-OCT showed resolved macular edema following serial anti-VEGF injections and inner retinal atrophy from previous cilioretinal artery occlusion. At 12 months following immunosuppressive therapy, b fundus photo shows resolution of inflammatory signs, residual venous tortuosity and intraretinal hemorrhages and (c) late frame of fluorescein angiogram shows resolution of leakage from the optic nerve head and retinal veins and persistence of the retinal capillary non-perfusion
Discussion
Kleiner classified FBA according to the etiology into three groups [1]. The first group involves patients with lymphoproliferative disorders who have malignant infiltration of retinal vascular tree. The second group involves patients with autoimmune diseases and infections with FBA representing an ocular manifestation. The third, more common, group is termed (acute idiopathic FBA) and occurs in otherwise healthy individuals [2, 5]. Our patient may fit into the second group of FBA given the history of oral ulcers and the presence of mobile hypopyon. FBA in the setting of Behcet’s disease has been reported previously [6,7,8,9,10,11,12].
Eleven previous cases of retinal periphlebitis resembling FBA associated with CRVO have been documented (Table 1) [13,14,15,16,17,18,19]. In all of the cases, the CRVO had either accompanied FBA at presentation or occurred later at an interval between 2 to 16 weeks. Whereas in our case, CRVO preceded the onset of periphlebitis by about five months. This might be explained by the presence of an underlying systemic vasculitis that has a prothrombotic tendency (i.e., Behcet’s disease) [20].
Anti-tumor necrosis factor therapy is becoming the first-line treatment in Behcet’s disease and it was considered at some point in the management of this patient [21, 22]. However, given the stabilization of the condition on conventional immunosuppressive therapy for several years, and the recovery of good visual acuity in the affected eye, we elected to continue the current management.
Retinal ischemia and proliferative retinopathy represent a clinical challenge when associated with fulminant ocular inflammation. Aggressive control of inflammation is an important prerequisite for involution of retinal neovascularization. Classically, laser photocoagulation targeting the ischemic retina has been considered as the treatment of choice [23,24,25]. Some authors advocate early laser treatment before the development of neovascularization [26]. However, laser may need to be used judiciously in an eye with fulminant inflammation as it was linked to an upregulation of cytokines and other inflammatory mediators. This pro-inflammatory effect is especially well-demonstrated in the studies of progression of diabetic macular edema following panretinal photocoagulation [27,28,29,30]. Moreover, other investigators have documented an increase in the vitreous humor levels of vascular endothelial growth factor (VEGF) and several proinflammatory cytokines in mice and rabbits following laser burns [30, 31]. This pro-inflammatory effect of retinal laser is less pronounced in the modern short-pulse laser technology [30]. In our patient, we used anti-VEGF therapy to address ME and suppress retinal neovascularization. Once we noted the development retinal neovascularization, we immediately applied laser photocoagulation to the ischemic retina.
This case presents a unique challenge as it initially presented with CRVO/CLRAO without frank signs of inflammation on clinical examination or FFA. An inflammatory etiology of CRVO in young population should be carefully investigated. Clinical suspicion and close follow‑up are required for early detection and timely management of FBA.
Availability of data and materials
Not applicable.
Abbreviations
- CRVO:
-
Central retinal vein occlusion
- CLRAO:
-
Cilioretinal artery occlusion
- OS:
-
Left eye
- VA:
-
Visual acuity
- FBA:
-
Frosted branch angiitis
- ME:
-
Macular edema
- FFA:
-
Fundus fluorescein angiography
- CBC:
-
Complete blood cell count
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- SD-OCT:
-
Spectral domain optical coherence tomography
- VEGF:
-
Vascular endothelial growth factor
References
Kleiner RC (1997) Frosted branch angiitis: clinical syndrome or clinical sign? Retina 17(5):370–371
Walker S, Iguchi A, Jones NP (2004) Frosted branch angiitis: a review. Eye 18(5):527–533
Agarwal A, Rübsam A, ZurBonsen L, Pichi F, Neri P, Pleyer U (2022) A Comprehensive Update on Retinal Vasculitis: Etiologies, Manifestations and Treatments. J Clin Med 11(9):2525
International Team for the Revision of the International Criteria for Behçet’s Disease (ITR-ICBD) (2014) The International Criteria for Behçet’s Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol 28(3):338–347. https://doi.org/10.1111/jdv.12107
Kleiner RC, Kaplan HJ, Shakin JL, Yannuzzi LA, Crosswell HH Jr, McLean WC Jr (1988) Acute frosted retinal periphlebitis. Am J Ophthalmol 106(1):27–34
Kwon SJ, Park DH, Shin JP (2013) Frosted branch angiitis as ocular manifestation of Behçet’s disease: unusual case report and literature review. Korean J Ophthalmol 27(6):466–469
Reynders S, Dewachter A, De Vriese AS (2005) A case of secondary frosted branch angiitis in Behcets disease. Bull Soc Belge Ophtalmol 298:41–44
Renard E, Chiquet C, Bouillet L, Romanet JP (2009) Frosted-branch angiitis revealing Behcet’s disease. J Fr Ophtalmol 32(9):664–668
Jackson TE, Pathak S, Doran RM (2011) Behçet disease presenting with frosted branch angiitis. Ocul Immunol Inflamm 19(1):65–66
Portero A, Herreras JM (2011) Frosted branch angiitis diagnosed as neuro-Behçet: a diagnostic and etiologic dilemma. Case Rep Ophthalmol 2(2):170–175
Al-Mujaini A, Wali UK (2011) Frosted branch angiitis, neuroretinitis as initial ocular manifestation in Behçet disease. Indian J Ophthalmol 59(3):240
Ramachandran R, Hughes E, Larkin G, Graham E, Stanford M, Lim M (2011) Secondary frosted branch angiitis in neuro-Behcet’s disease with serous macular detachment. Pediatr Int 53(2):285–286
Foss AJE, Headon MP, Hamilton AM, Lightman S (1992) Transient vessel wall sheathing in acute retinal vein occlusions. Eye 6(3):313–316
Seo MS, Woo JM, Jeong SK, Park YG (1998) Recurrent unilateral frosted branch arthritis. Jpn J Ophthalmol 42(1):56–59
Kaburaki T, Nakamura M, Nagasawa K, Nagahara M, Joko S, Fujino Y (2001) Two cases of frosted branch angiitis with central retinal vein occlusion. Jpn J Ophthalmol 45(6):628–633
Abu El-Asrar AM, Al-Obeidan SA, Abdel Gader AGM (2003) Retinal periphlebitis resembling frosted branch angiitis with nonperfused central retinal vein occlusion. Eur J Ophthalmol 13(9–10):807–812
Satoh S, Itoh C, Nakamura N (2010) A case of frosted branch angiitis associated with retinal vein occlusion as a complication of familial Mediterranean fever. Nippon Ganka Gakkai Zasshi 114(7):621–628
Greifner G, Neri P, Amer R (2016) Frosted branch angiitis complicated by retinal vein occlusion: clinical course and long-term visual outcome. Graefes Arch Clin Exp Ophthalmol 254(3):541–544
Kumawat B, Tripathy K, Venkatesh P, Chawla R, Sharma YR (2017) Central retinal vein occlusion-like appearance: a precursor stage in evolution of frosted branch angiitis. J Ophthalmic Vis Res 12(4):440
Posarelli C, Maglionico MN, Talarico R, Covello G, Figus M (2020) Behçet’s syndrome and ocular involvement: changes over time. Clin Exp Rheumatol 38(127):86–93
Posarelli C, Arapi I, Figus M, Neri P (2011) Biologic agents in inflammatory eye disease. J Ophthalmic Vis Res 6(4):309
Pleyer U, Neri P, Deuter C (2021) New pharmacotherapy options for noninfectious posterior uveitis. Int Ophthalmol 41(6):2265–2281
Retinal Vein Occlusions PPP 2019 (2019) American Academy of Ophthalmology. Published October 11, 2019. Accessed 26 Sept 2020. https://www.aao.org/preferred-practice-pattern/retinal-vein-occlusions-ppp
Central Vein Occlusion Study Group (1995) A randomized clinical trial of early panretinal photocoagulation for ischermic central vein occlusion: the Central Vein Occlusion Study Group N Report. Ophthalmology 102(10):1434–1444
Schmidt-Erfurth U, Garcia-Arumi J, Gerendas BS, Midena E, Sivaprasad S, Tadayoni R, Loewenstein A (2019) Guidelines for the management of retinal vein occlusion by the European Society of Retina Specialists (EURETINA). Ophthalmologica 242(3):123–162
Hayreh SS, Klugman MR, Podhajsky P, Servais GE, Perkins ES (1990) Argon laser panretinal photocoagulation in ischemic central retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol 228(4):281–296
Takahashi A, Nagaoka T, Sato E, Yoshida A (2008) Effect of panretinal photocoagulation on choroidal circulation in the foveal region in patients with severe diabetic retinopathy. Br J Ophthalmol 92(10):1369–1373
Oh IK, Kim SW, Oh J, Lee TS, Huh K (2010) Inflammatory and angiogenic factors in the aqueous humor and the relationship to diabetic retinopathy. Curr Eye Res 35(12):1116–1127
Shimura M, Yasuda K, Nakazawa T, Abe T, Shiono T, Iida T, Nishida K (2009) Panretinal photocoagulation induces pro-inflammatory cytokines and macular thickening in high-risk proliferative diabetic retinopathy. Graefe’s Arch Clin Exp Ophthalmol 247(12):1617–1624
Ito A, Hirano Y, Nozaki M, Ashikari M, Sugitani K, Ogura Y (2015) Short pulse laser induces less inflammatory cytokines in the murine retina after laser photocoagulation. Ophthalmic Res 53(2):65–73
Itaya M, Sakurai E, Nozaki M, Yamada K, Yamasaki S, Asai K, Ogura Y (2007) Upregulation of VEGF in murine retina via monocyte recruitment after retinal scatter laser photocoagulation. Invest Ophthalmol Vis Sci 48(12):5677–5683
Acknowledgements
Not applicable.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
A.A. acquired the data and wrote the manuscript, W.K. edited the manuscript and S.A. interpreted the data and edited the manuscript. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review board of King Khaled Eye Specialist Hospital.
Consent for publication
Consent for publication was obtained from the patient.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Albahlal, A., Khayyat, W. & Alsulaiman, S.M. Combined central retinal vein occlusion and cilioretinal artery occlusion as the initial presentation of frosted branch angiitis: a case report and literature review. J Ophthal Inflamm Infect 13, 28 (2023). https://doi.org/10.1186/s12348-023-00340-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12348-023-00340-7