Abstract
Background
Pyrethroids have been widely used in the United States and worldwide. Few studies examined the effect of pyrethroids exposure on sleep problems among adolescents.
Objectives
This study investigated the associations between pyrethroids exposure and sleep problems in male and female adolescents.
Methods
The data were used from the National Health and Nutrition Examination Survey 2007–2014. In this study, 3-Phenoxybenzoic Acid (3-PBA) was used as a validated biomarker for pyrethroids exposure. The association between urinary 3-PBA and sleep problems was analyzed using logistic regression models.
Results
A total of 805 adolescents aged 16–20 years old were included in this study. The proportion of sleep problems was higher in females than in males (10.18% vs.7.35%, P = 0.154). A significant interaction was found between sex and 3-PBA (P interaction = 0.021) in the risk of sleep problems. A positive association of 3-PBA exposure with sleep problems was observed in male adolescents after adjusting for all the other covariates (OR = 4.04, 95% CI 1.31, 12.42). No statistically significant association was observed in female adolescents.
Conclusions
A positive association was observed between pyrethroids exposure and sleep problems in male adolescents, but not in female adolescents. More studies are required to confirm our findings.
Similar content being viewed by others
Introduction
Sleep disorders, categorized into insomnia, restless legs syndrome, and sleep apnea, are increasingly becoming severe problems in many countries [4, 13]. Sleep disorders problems are linked to a growing number of adverse health outcomes, including cardiovascular disease, obesity, and certain cancers among adult populations [9, 15, 19, 22, 28]. Besides, sleep disorders have also been related to a series of psychiatric problems, behavioral antecedents, and an increased risk of injury and motor vehicle accidents in adolescents [6, 26, 40]. Many factors can affect sleep quality such as proximity to noisy areas, alcohol consumption, smoking, and stress, etc. [12, 16, 38]. Recent studies have suggested a link between pesticide exposure and sleep problems. For example, Fuhrimann et al. found that the use of mancozeb and glyphosate could lead to an increased risk of sleep problems [14].
Pyrethroids are one of the most commonly used pesticides in the world. It is reported that more than 30% of pyrethroid pesticides are used worldwide and are commonly used in agricultural and domestic settings [5, 8]. In the general population, exposure to pyrethroids is mainly through ingestion of skin contact with contaminated house dust or ingestion of residues in food, or surface adhesion particles [29]. Zamora et al. found that longer sleep duration and later sleep timing were related to maternal prenatal chlorpyrifos exposure among adolescent offspring in a mother-adolescent pairs cohort, but found no significant associations between pyrethroids exposure(3-PBA) and sleep outcomes [42]. In another study, Zamora et al. also reported a significant association between urinary 3-PBA concentration and trouble sleeping among adults [41]. Moreover, males may tend to be easily affected by pyrethroids exposure [41, 42]. Consistently, previous studies also indicated that the toxicological effects of pyrethroid metabolites might have sex-related disparities in other health outcomes such as obesity and rheumatoid arthritis [17, 44].
Overall, few studies assessed the effect of pyrethroids pesticide exposure on sleep problems, and the associations were under-investigated in adolescents. In this study, we examined the cross-sectional associations between pyrethroids exposure and sleep problems and the potential sex differences in adolescents using a representative US (the United States) population.
Material and methods
Study population and design
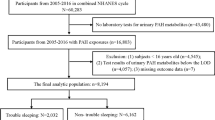
The data comes from the National Health and Nutrition Examination Survey (NHANES) which aims to evaluate the health and nutritional status among US adults and children. The survey design, sampling procedures, and methods were detailed elsewhere [23]. We included the data from four cycles (2007–2014) in which urinary 3-PBA data were collected from participants. The National Center for Health Statistics Ethics Review Board has approved the protocol and written consent was provided for all participants. Pyrethroid exposure data were available in a random subsample of participants aged ≥ 16 years [23]. Overall, 17, 551 participants aged 16–20 years old among which 899 had completed data on 3-PBA and sleep problems. After excluding missing data on body mass index (BMI), physical activity, poverty income ratio (PIR), and urine creatine, 805 participants were included in the main analysis (Fig. 1).
Urinary pyrethroid exposure measurement
The random daytime spot urine of the participants at enrollment was stored at − 20o C within 4 h and analyzed by National Environmental Sanitation Center. The high-performance liquid chromatography combined with electrospray chemical ionization and tandem mass spectrometry methods were used to detect urinary concentrations of pyrethroid metabolites including 3-PBA, Trans-DCCA (trans-3-(2, 2-dichlorovinyl)-2, 2-dimethylcylopropane carboxylic acid), 4-F-3-PBA (4-fluoro-3-phenoxy-benzoic acid), and Cis-DBCA (cis-(2,2-dibromovinyl)-2,2-dimethylcyclopropane-1-carboxylic acid) [1, 3]. In agreement with previous studies [37], 3-PBA was used as the primary marker for pyrethroids pesticide exposure, and other metabolites secondary markers were also tested.
Definition of sleep problems
Sleep problems included sleep disorders and trouble sleeping. Sleep problems were defined as having sleep disorders or trouble sleeping based on self-reported doctor diagnoses: “Have you ever been told by a doctor or other health professional that you have a sleep disorder?” and “Have you ever been told by a doctor or other health professional that you have a trouble sleeping?”.
Covariates
Standardized questionnaires were used to collect socio-demographic characteristics including age, sex, race/ethnicity, PIR, BMI, and physical activity. Age was modelled as a continuous variable. PIR was divided into three groups according to the total family income ratio (< 1.3, 1.3–3.5, and > 3.5) [44]. Race/ethnicity was grouped as Hispanic (Mexican American and other Hispanic), non-Hispanic white, non-Hispanic black, and others. BMI was continuously sorted into four levels (BMI < 18.5, BMI ≥ 18.5 and BMI < 25, BMI ≥ 25 and BMI < 30, and BMI ≥ 30) which was calculated by dividing weight (kg) by height (m2) [31]. The physical activity is based on the self-reported questions and classified into vigorous activities(causing heavy sweating, or large increases in breathing or heart rate), moderate activities (causing light sweating or a slight to moderate increase in breathing or heart rate), and sedentary (neither vigorous recreation activities nor moderate recreation activities) [44]. The Roche/Hitachi modular P chemical analyzer was used to determine urinary creatinine. In this enzymatic process, creatinine is converted to creatine by the action of creatinase. Creatine is then formed into sarcosine and urea by the action of creatinase.
Statistical analysis
According to the NHANES guidelines, the weight of the smallest subpopulation that includes all the variables (WTSC2YR) was used to account for the complex survey design. The mean and standard deviation are used to describe continuous variables, whereas cases (n) and percentages (%) are used to present categorical variables. Urinary 3-PBA was log-transformed, and urinary creatinine was adjusted in all the analyses [2]. The association between 3-PBA exposure (categorized into Tertiles (T)) and sleep problems was analyzed using a multivariate logistic regression model. In addition, interaction effects were estimated by adding a 3-PBA × covariable term to the model. Due to the significant interaction between sex and 3-PBA, we investigated the relationship between 3-PBA and sleep problems in males and females separately. Model 1 adjusted for urinary creatinine; Age, race/ethnicity, and urinary creatinine were adjusted in Model 2; Model 3 was further adjusted for PIR, physical activity, and BMI.
Trans-DCCA, 4-F-3PBA, and Cis-DBCA were dichotomized as detected vs. undetected due to the low detection rates (11.52%, 7.52% and 0.75%, respectively). Furthermore, the associations of trouble sleeping, and sleep disorders with 3-PBA were also tested, respectively. In sensitivity analyses, we tested the associations by not excluding participants with missing data on the covariates, and a multiple imputation approach was adopted to impute the missing data. Further, we performed more sensitive analyses, including using the covariate-adjusted standardization method [24], using unsupervised summary scores of pyrethroid metabolites, did not incorporate the complex survey design, excluding participants with poor health status, and further controlling for dietary factors and cotinine. All of the above analyses were performed using Stata software version 14 (STATA Corp, TX, US). The difference was statistically significant if a P value < 0.05 on both sides.
Results
Basic characteristics of the study population
A total of 805 eligible participants were included in our analyses, among which 52.4% were males and the average age was 17.8 years old. Significant differences were found in the general characteristics between male and female adolescents such as BMI and physical activity, as shown in Table 1. The proportion of sleep problems was higher in females than in males (10.18% vs 7.35%, P = 0.154). The geometric means of uncorrected and creatinine uncorrected 3-PBA were 0.43 and 0.31 in males.
Associations between 3-PBA and sleep problems
A significant interaction was found between sex and 3-PBA on sleep problems (P for interaction = 0.021), suggesting a potential moderating effect in the association between 3-PBA and sleep problems (Fig. 2). Sex-stratified analyses showed a positive association of 3-PBA exposure with sleep problems in male adolescents (Tertile 3 vs. Tertile 1: OR = 3.20; 95%CI: 1.10–9.30; P = 0.030). After controlling for age, sex, race, urinary creatinine, PIR, physical activity, and BMI, the results remained similar (Tertile 3 vs. Tertile 1: OR = 4.04; 95%CI: 1.31–12.42; P = 0.017). Among female adolescents, no significant association was observed (Table 2).
Association between other metabolites and sleep problems
Similarly, a positive association was observed between the 4-F-3PBA exposure and sleep problems in male adolescents after adjusting for potential confounders (Tertile 3 vs. Tertile 1: OR = 4.40; 95% CI: 1.32, 14.58; P = 0.016), but not in female adolescents (Tertile 3 vs. Tertile 1: OR = 1.25; 95% CI: 0.36, 4.35; P = 0.726). There was no significant association for Trans-DCCA in male or female adolescents (Table 3). The relationship between urinary cis-DBCA and sleep problems was not tested in our study due to a low detection rate (0.75%).
Associations of 3-PBA with trouble sleeping and sleep disorders
The associations of 3-PBA with trouble sleeping and sleep disorders were further tested in Additional file 1: Tables S1 and S2. Consistently, after adjusting for the covariates, higher 3-PBA exposure was positively associated with a higher risk of trouble sleeping (Tertile 3 vs. Tertile 1: OR: 4.42; 95% CI: 1.32, 14.79; P = 0.018) in male adolescents, but not in female adolescents (Tertile 3 vs. Tertile 1: OR: 0.78; 95% CI: 0.21, 2.88; P = 0.880). No significant association was observed between 3-PBA and sleep disorders.
Sensitivity analysis
We imputed the missing data using multiple imputations and found similar associations between 3-PBA and sleep problems (Additional file 1: Table S3). Moreover, there was no significant difference in the general characteristics between those included and those excluded (Additional file 1: Table S4). Similar results were observed in other sensitivity analyses (Additional file 1: Tables S5–S9).
Discussion
Using NHANES data, a statistical interaction was found between sex and 3-PBA exposure level on sleep problems. In the further stratified analysis, we observed a significant association between urinary 3-PBA and sleep problems in male adolescents, but not in female adolescents.
In a cross-sectional survey of 4478 adults conducted in the United States, in line with our results, the authors reported that a higher log 3-PBA level was related to a higher risk of trouble sleeping (β = 1.14, 95% CI 1.02, 1.27) among male adults [41]. Our study extended the limited evidence of the association between pyrethroids exposure and sleep problems in adolescents, especially in males.
The association between pesticides and sleep problems has been reported in human and animal studies. For example, Li et al. found adverse associations between pesticide exposure intensity and sleep problems among greenhouse vegetable farmers [20]. Other studies also showed that insomnia or disturbed sleep could result from the use of pesticides among the Southern Brazilian rural population [21]. Experimental studies have shown that there was an interaction between carbamates (one specific class of pesticides) and melatonin (sleep/wake hormone) [27]. Another pesticide chlorpyrifos was associated with a higher sleep apnea index in juvenile and adult rats [11].
The results showed that exposure to pyrethroids was significantly associated with a higher risk of sleep problems in males, but not in females. The effects of pyrethroids on health outcomes in males and females are mixed [41, 44]. One possible explanation is that the effects of pyrethroids on different health outcomes may have sex-specific pathways. It was reported that SOD and GPx activity decreased in female rats by the action of permethrin, while it increases in male rats [10]. Another animal study found sex differences in the toxicological effects of pyrethroid metabolites, which might be due to sex-related differences in metabolism and excretion kinetics [35]. In addition, 3-PBA has a function of anti-androgenic activity [33], and testosterone deficiency may have a deleterious effect on sleep quality that may be improved with testosterone replacement [39]. These results suggest that interventions targeting males tend to 3-PBA exposure need to be developed.
The underlying mechanisms are understudied. Pyrethroids could lead to hyperexcitation of the nervous system due to a prolonged sodium current to flow [43]. Hyperglycemia and elevated plasma levels of noradrenaline and adrenaline have also been shown in animal studies of pyrethroid toxicity [32]. Elevated plasma noradrenaline and adrenaline levels may be another possible reason for the sleep disorders. Studies also showed an association between exposure to 3-PBA and bad neurocognitive consequences [34]. Pyrethroids with the characteristics of endocrine-disrupting have been associated with obesity [18], which is linked to sleep quality [30]. In addition, exposure to pyrethroids could cause repeated firing of sensory nerve endings, resulting in abnormal sensation and irritation of the human respiratory tract [36].
We for the first time reported a significant association between urinary 3-PBA and sleep problems among adolescents. The study also has several limitations in this study. First, the cross-sectional nature of this study does not allow for inferring causality. Second, some potential confounders/covariates are not available for analysis, such as genetic factors. Third, the half-life of pyrethroids in the body of humans is short, so one-time measurement could not reflect long-term exposure [25]. Fourth, there may have recall bias in self-reported sleep problems. Fifth, urinary creatinine excretion fluctuated greatly due to specific internal and external factors such as gender, age and race. The adjustment of urinary creatinine to correct chemical concentrations in urine will not necessarily improve the correlation with all chemical exposure doses (it may worsen the result) [7]. Finally, extrapolating the results to other populations should be cautious.
Conclusions
There were sex differences regarding the associations between 3-PBA exposure and sleep problems with a stronger association in male adolescents. We still need more research to confirm our findings and explore the underlying mechanisms.
Availability of data and materials
The datasets analyzed in the current study are available in the NHANES [https://www.cdc.gov/nchs/nhanes/].
References
Baker SE et al (2004) Isotope dilution high-performance liquid chromatography-tandem mass spectrometry method for quantifying urinary metabolites of synthetic pyrethroid insecticides. Arch Environ Contam Toxicol 46:281–288. https://doi.org/10.1007/s00244-003-3044-3
Bao W et al (2020) Association between exposure to pyrethroid insecticides and risk of all-cause and cause-specific mortality in the general US adult population. JAMA Intern Med 180:367–374. https://doi.org/10.1001/jamainternmed.2019.6019
Barr DB et al (2010) Urinary concentrations of metabolites of pyrethroid insecticides in the general U.S. population: national health and nutrition examination survey 1999–2002. Environ Health Perspect 118:742–748. https://doi.org/10.1289/ehp.0901275
Benjafield AV et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7:687–698. https://doi.org/10.1016/s2213-2600(19)30198-5
Bhardwaj, K., et al. 2020. Pyrethroids: Natural Bioactive Products in Sustainable Agriculture. In: Joginder Singh, Ajar Nath Yadav (Eds). Natural Bioactive Products in Sustainable Agriculture. Singapore: Springer
Blunden S et al (2000) Behavior and neurocognitive performance in children aged 5–10 years who snore compared to controls. J Clin Exp Neuropsychol 22:554–568. https://doi.org/10.1076/1380-3395(200010)22:5;1-9;ft554
Boeniger MF et al (1993) Interpretation of urine results used to assess chemical exposure with emphasis on creatinine adjustments: a review. Am Ind Hyg Assoc J 54:615–627. https://doi.org/10.1080/15298669391355134
Bradberry SM et al (2005) Poisoning due to pyrethroids. Toxicol Rev 24:93–106. https://doi.org/10.2165/00139709-200524020-00003
Cappuccio FP, Miller MA (2017) Sleep and cardio-metabolic disease. Curr Cardiol Rep 19:110. https://doi.org/10.1007/s11886-017-0916-0
Chargui I et al (2010) Erythrocyte antioxidants enzymes imbalance following subcutaneous pyrethroid treatments in rats of different sex. Environ Toxicol Pharmacol 30:116–120. https://doi.org/10.1016/j.etap.2010.04.005
Darwiche W et al (2018) Impact of chronic exposure to the pesticide chlorpyrifos on respiratory parameters and sleep apnea in juvenile and adult rats. PLoS One 13:e0191237. https://doi.org/10.1371/journal.pone.0191237
Drake CL et al (2004) Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep 27:1453–1462. https://doi.org/10.1093/sleep/27.8.1453
Filip I et al (2017) Public health burden of sleep disorders: underreported problem. J Public Health 25:243–248. https://doi.org/10.1007/s10389-016-0781-0
Fuhrimann S et al (2022) Recent pesticide exposure affects sleep: a cross-sectional study among smallholder farmers in Uganda. Environ Int 158:106878. https://doi.org/10.1016/j.envint.2021.106878
Fund N et al (2020) The epidemiology of sleep disorders in Israel: results from a population-wide study. Sleep Med 67:120–127. https://doi.org/10.1016/j.sleep.2019.10.010
Grandner MA et al (2013) Sleep-related behaviors and beliefs associated with race/ethnicity in women. J Natl Med Assoc 105:4–15. https://doi.org/10.1016/s0027-9684(15)30080-8
Guo X et al (2023) Exploratory analysis of the association between pyrethroid exposure and rheumatoid arthritis among US adults: 2007–2014 data analysis from the national health and nutrition examination survey (NHANES). Environ Sci Pollut Res Int 30:14413–14423
Kim J et al (2014) Permethrin alters adipogenesis in 3T3-L1 adipocytes and causes insulin resistance in C2C12 myotubes. J Biochem Mol Toxicol 28:418–424. https://doi.org/10.1002/jbt.21580
Koren D, Taveras EM (2018) Association of sleep disturbances with obesity, insulin resistance and the metabolic syndrome. Metabolism 84:67–75. https://doi.org/10.1016/j.metabol.2018.04.001
Li J et al (2019) Relationship between cumulative exposure to pesticides and sleep disorders among greenhouse vegetable farmers. BMC Public Health 19:1–11. https://doi.org/10.1186/s12889-019-6712-6
Machado AKF et al (2018) Sleep problems and associated factors in a rural population of a Southern Brazilian city. Revista de Saúde Pública. https://doi.org/10.11606/s1518-8787.2018052000260
McDermott M et al (2018) Sleep disorders and the risk of stroke. Expert Rev Neurother 18:523–531. https://doi.org/10.1080/14737175.2018.1489239
NCHS, 2020. NHANES questionnaires, datasets, and related documentation Center Health Stat. https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.
O’Brien KM et al (2016) Environmental chemicals in urine and blood: improving methods for creatinine and lipid adjustment. Environ Health Perspect 124:220–227. https://doi.org/10.1289/ehp.1509693
Park J et al (2019) Environmental pyrethroid exposure and diabetes in U.S. adults. Environ Res 172:399–407. https://doi.org/10.1016/j.envres.2018.12.043
Pizza F et al (2010) Sleep quality and motor vehicle crashes in adolescents. J Clin Sleep Med 6:41–45
Popovska-Gorevski M et al (2017) Carbamate insecticides target human melatonin receptors. Chem Res Toxicol 30:574–582. https://doi.org/10.1021/acs.chemrestox.6b00301
Ryan S (2018) Sleep and diabetes. Curr Opin Pulm Med 24:555–560. https://doi.org/10.1097/mcp.0000000000000524
Saillenfait AM et al (2015) Pyrethroids: exposure and health effects—an update. Int J Hyg Environ Health 218:281–292. https://doi.org/10.1016/j.ijheh.2015.01.002
Sánchez-López AM et al (2020) Childhood obesity and its influence on sleep disorders: kids-play study. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17217948
Saydah S et al (2014) Trends in cardiovascular disease risk factors by obesity level in adults in the United States, NHANES 1999–2010. Obesity (Silver Spring) 22:1888–1895. https://doi.org/10.1002/oby.20761
Sharma P et al (2014) Pyrethroid as a substance of abuse. Case Rep Psychiatry. https://doi.org/10.1155/2014/169294
Sun H et al (2007) Antiandrogenic activity of pyrethroid pesticides and their metabolite in reporter gene assay. Chemosphere 66:474–479. https://doi.org/10.1016/j.chemosphere.2006.05.059
Tsuji R et al (2012) Mammal toxicology of synthetic pyrethroids. Top Curr Chem 314:83–111. https://doi.org/10.1007/128_2011_269
Ueyama J et al (2010) Toxicokinetics of pyrethroid metabolites in male and female rats. Environ Toxicol Pharmacol 30:88–91. https://doi.org/10.1016/j.etap.2010.03.017
Vijverberg HP, van den Bercken J (1990) Neurotoxicological effects and the mode of action of pyrethroid insecticides. Crit Rev Toxicol 21:105–126. https://doi.org/10.3109/10408449009089875
Wagner-Schuman M et al (2015) Association of pyrethroid pesticide exposure with attention-deficit/hyperactivity disorder in a nationally representative sample of U.S. children. Environ Health 14:44. https://doi.org/10.1186/s12940-015-0030-y
Wetter DW et al (1994) Smoking as a risk factor for sleep-disordered breathing. Arch Intern Med 154:2219–2224. https://doi.org/10.1001/archinte.1994.00420190121014
Wittert G (2014) The relationship between sleep disorders and testosterone in men. Asian J Androl 16:262–265. https://doi.org/10.4103/1008-682x.122586
Yang CK et al (2005) Age-related changes in sleep/wake patterns among Korean teenagers. Pediatrics 115:250–256. https://doi.org/10.1542/peds.2004-0815G
Zamora AN et al (2021) Association between pesticide exposure and sleep health among a representative sample of US adults: evidence from NHANES 2009–2014. BMC Public Health 21:1–12. https://doi.org/10.1186/s12889-021-12014-x
Zamora AN et al (2022) Prenatal maternal pesticide exposure in relation to sleep health of offspring during adolescence. Environ Res 204:111977. https://doi.org/10.1016/j.envres.2021.111977
Zhorov BS, Dong K (2017) Elucidation of pyrethroid and DDT receptor sites in the voltage-gated sodium channel. Neurotoxicology 60:171–177. https://doi.org/10.1016/j.neuro.2016.08.013
Zuo L et al (2022) Pyrethroids exposure induces obesity and cardiometabolic diseases in a sex-different manner. Chemosphere 291:132935. https://doi.org/10.1016/j.chemosphere.2021.132935
Acknowledgements
The authors acknowledge the important contributions of all the staff and participants in this study.
Funding
There was no specific grant from funding agencies in the public, commercial, or not-for-profit sectors in this study.
Author information
Authors and Affiliations
Contributions
The manuscript was drafted and revised by all authors. GH, HYC and SHP were responsible for the conceptualization, supervision, and editing sections. LZ and GZL were tasked with the data collection, formal analysis, investigation, and original draft writing sections. XC, LZ, MLL, LC and CXJ critically reviewed and helped to prepare the methods sections. LZ and GZL contributed equally to this paper. GH, HYC and SHP will act as guarantors for the paper.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The National Center for Health Statistics Ethics Review Board has approved the protocol and written consent was provided for all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Associations between urinary 3-PBA level and sleep disorders. Table S2. Associations between urinary 3-PBA level and trouble sleeping. Table S3. Associations between pyrethroids exposure and sleep health (using a multiple imputation approach). Table S4. Comparison of main characteristics between those included in the analyses and those excluded due to missing data. Table S5. Associations between urinary 3-PBA level and sleep problem (not excluding participants with missing data on covariates). Table S6. Associations between urinary 3-PBA level and sleep problem (using the covariate-adjusted standardization method). Table S7. Associations between sum of pyrethroid metabolites levels and sleep problem (using unsupervised summary scores of pyrethroid metabolites). Table S8. Associations between urinary 3-PBA level and sleep problem (not using complex survey design). Table S9. Associations between urinary 3-PBA level and sleep problem (excluding poor health status participants, and further controlling for dietary factors and cotinine).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, L., Li, G., Chen, X. et al. Sex difference in the association between pyrethroids exposure and sleep problems among adolescents: NHANES 2007–2014. Environ Sci Eur 35, 53 (2023). https://doi.org/10.1186/s12302-023-00753-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12302-023-00753-0