Abstract
Background
Persistent Mϋllerian duct syndrome is a rare condition marked by the presence of Mϋllerian duct derivatives (uterus and fallopian tubes) in males who are seemingly (phenotypically and karyotypically) normal. Diagnosis can be made with physical examination, radiological investigations and karyotyping. The management aims at preserving fertility and removing Mϋllerian duct structures.
Case presentation
We report a case of PMDS encountered in a patient presenting with bilateral non-palpable testes since birth who was treated with orchidopexy and removal of Mϋllerian duct structures.
Conclusion
A remote possibility of persistent Mϋllerian duct syndrome should be borne in mind while dealing with a case of undescended testes. If such an encounter occurs, orchidopexy with removal of Mullerian duct structures is the preferred management.
Similar content being viewed by others
1 Background
Persistent Mϋllerian duct syndrome (PMDS) is a rare entity wherein persistence of Mϋllerian duct structures (uterus, fallopian tubes, upper vagina) is seen in a phenotypically and karyotypically normal male. It is an autosomal recessive disorder of sexual development in which a seemingly normal male patient can present with cryptorchidism or inguinal hernia. The patient has persistence of Mϋllerian duct structures despite a normal karyotype due to defects in gene for AMH or AMH type 2 receptor. Preoperative diagnosis via physical examination, radiological modalities and karyotyping help plan the management, which aims at preserving fertility and removing Mϋllerian duct structures. The objective of this case report is to present a case of PMDS with a brief review of the literature.
2 Case presentation
A 17-year-old boy presented to the Urology OPD with complaint of bilateral non-palpable testes in scrotum since birth. He had no other complaint. On examination, the patient was well built, with normal virilization. His secondary sexual characteristics were well developed with normal density of pubic and axillary hair, however, with sparse facial hair. He had a normal penile length and girth with normally positioned meatus. His scrotal sac was normally developed but bilateral testes were not palpable in both hemiscrotum and inguinal regions. No inguinal hernia was identified on either side of inguino-scrotal region.
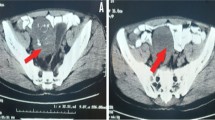
Ultrasound revealed non-visualization of testes in bilateral hemiscrotum and inguinal canals. CECT scan of the abdomen showed empty scrotal sac with iliac oval structures without any CT identifiable follicles- likely gonads. A normal sized prostate was identified at the base of the bladder, adjacent to which a uterus like structure was seen.
Semen analysis revealed azoospermia. His LH, FSH, free and total testosterone, TSH, estradiol levels were normal. His AMH levels were not elevated (13.02 ng/ml). Karyotyping showed normal male karyotype (XY).
A diagnosis of persistent Mϋllerian duct syndrome was made.
AFP, LDH and β-HCG levels were estimated to rule out possibility of malignancy in intra-abdominal testes and were within normal limits (Fig. 1).
The patient underwent diagnostic laparoscopy, which revealed presence of both testes in the iliac regions (Fig. 2a) along with the uterus and fallopian tubes (Fig. 2c). Hysterosalpingectomy and orchidopexy were done at the neck of the scrotum after testicular mobilization which could not go beyond the neck of the scrotum.
Intraoperative images on laparoscopy—testis (a) and uterus (c) with corresponding histopathological photomicrographs (b and d, respectively). Testicular tissue was identified (b); however, no spermatogenesis was seen. Endometrium and underlying myometrium (d) was seen in the specimen from the uterus
Histopathology confirmed bilateral intra-abdominal testes, which showed only Sertoli cells without evidence of spermatogenesis, and persistent Mϋllerian structures—the uterus and bilateral fallopian tubes.
The patient had no complaints on follow-up after one and three months.
3 Discussion
Persistent Mϋllerian duct syndrome is a rare disorder of sexual differentiation wherein there is persistence of Mϋllerian duct structures in a patient with normal male karyotype (XY) and external genitalia. The patient has unilateral/bilateral undescended testes, and uterus, bilateral fallopian tubes and the upper part of vagina which opens into the prostatic utricle.
The disorder may have its genetic basis in abnormal function of anti-Mϋllerian hormone (AMH), due to a defect either in the gene for AMH on the short arm of chromosome 19 or in the gene for AMH type 2 receptor on the long arm of chromosome 12 [1]. In these patients, the disorder shows an autosomal recessive inheritance pattern. However in a small percentage of cases (12%), no mutation was found in the aforementioned genes [2].
Three categories of PMDS were described by Clarnette et al. [3]: (1.) Most common presentation (60–70%) is that of bilateral undescended intra-abdominal testes in positions analogous to those of ovaries, as seen in our case report; (2.) less commonly (20–30%) one testis is present in the scrotum or a hernia sac and the contralateral testis, along with the uterus and fallopian tubes are present within an inguinal hernia- hence the term “hernia uteri inguinale”; (3.) The least common presentation is that of transverse testicular ectopia where both testes along with the uterus and fallopian tubes are present within the same hernia sac.
The management guidelines for PMDS aim at preserving fertility. Orchidopexy is to be attempted whenever possible to preserve fertility. Orchiectomy should be considered if testis cannot be mobilized to a palpable location or in case of high suspicion of malignancy in testis. There are conflicting opinions in management of the Mϋllerian duct structures. Since the vas deferens is closely related to the uterus in these patients, excision of the Mϋllerian duct structures may cause iatrogenic or ischemic trauma to the vas, thus impairing fertility. Hence, it was previously suggested that the Mϋllerian duct structures should not be removed [4]. However, due to a high risk of malignancy in Mϋllerian duct structures of up to 3.1–8.4%, it is currently recommended that Mϋllerian duct structures be carefully excised [5], as was done in our case report.
4 Conclusion
PMDS is a rare condition that may present with undescended testes or inguinal hernia. Preoperative diagnosis helps in planning of management. Orchidopexy should be done to preserve fertility. In case of suspicion of testicular tumor, orchiectomy must be performed. The Mϋllerian duct structures should be removed to obviate the risk of development of malignancy in later life, taking care to avoid injury to vasa deferentia which lie close to the Mϋllerian duct structures.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Abbreviations
- PMDS:
-
Persistent Mϋllerian duct syndrome
- AMH:
-
Anti-Mϋllerian hormone
- OPD:
-
Outpatient department
- CECT:
-
Contrast enhanced computed tomography
- CT:
-
Computed tomography
- LH:
-
Luteinizing hormone
- FSH:
-
Follicle-stimulating hormone
- TSH:
-
Thyroid-stimulating hormone
- AFP:
-
Alpha-fetoprotein
- LDH:
-
Lactate dehydrogenase
- β-HCG:
-
Beta human chorionic gonadotropin
References
MacLaughlin DT, Donahoe PK (2004) Sex determination and differentiation. N Engl J Med 350(4):367–378. https://doi.org/10.1056/NEJMra022784
Picard JY, Cate RL, Racine C, Josso N (2017) The persistent müllerian duct syndrome: an update based upon a personal experience of 157 cases. Sex Dev 11(3):109–125. https://doi.org/10.1159/000475516 (Epub 2017 May 20 PMID: 28528332)
Clarnette TD, Sugita Y, Hutson JM (1997) Genital anomalies in human and animal models reveal the mechanisms and hormones governing testicular descent. Br J Urol 79:99–112
Vandersteen DR, Chaumeton AK, Ireland K, Tank ES (1997) Surgical management of persistent müllerian duct syndrome. Urology 49(6):941–945. https://doi.org/10.1016/S0090-4295(97)00104-0
Shalaby MM, Kurkar A, Zarzour MA, Faddan AA, Khalil M, Abdelhafez MF (2014) The management of the persistent müllerian duct syndrome. Arab J Urol 12(3):239–244. https://doi.org/10.1016/j.aju.2014.04.001
Acknowledgements
Not applicable
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MJ and PD researched literature and conceived the study. MJ wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript. All authors agree both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. Concept and design: MJ and PD. Literature search: MJ and PD. Data acquisition: MJ, RS, PD and AB. Manuscript preparation: MJ and PD. Manuscript editing: MJ, RS, PD and AB. Manuscript review: MJ, RS, PD and AB. Approval of submitted version: MJ, RS, PD and AB. MJ, RS, PD and AB agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for publication was obtained from the parents of the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Joshi, M., Sahu, R., Dubey, P. et al. Persistent Mϋllerian duct syndrome presenting as bilateral cryptorchidism: a case report. Afr J Urol 28, 50 (2022). https://doi.org/10.1186/s12301-022-00313-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-022-00313-7