Background
The variant of urothelial carcinoma (UCV) is a rare and aggressive histological entity; its therapeutic management remains debated.
Methods
Between January 2017 and October 2019, 39 patients were diagnosed retrospectively with urothelial carcinoma with a histological variant. The aim of this study was to analyze the clinico-pathological and therapeutic aspects of these variants to better understand this invasive disease.
Results
In 39 cases, 36 (92%) were men and 3 (8%) were women; the average age was 62 years; 54% of patients had a ≥ cT3 stage with clinical lymph node involvement in 28% and 23% had distant metastases, 36% of patients were treated with RC and 54% by other therapeutic and 10% refused RC. No patient received neoadjuvant chemotherapy. Lymph node involvement was 28.5%. The two predominant histological types were squamous and micropapillary differentiation between the operating piece and bladder biopsy 28.5%, 30% and 21.5% and 13%, respectively. The overall survival at 20 months was 70 and 40% for RC and the other therapeutic (TURB alone or a TURB with an adjuvant), respectively. There was no significant difference in survival between the two groups (p = 0.27).
Conclusion
UCVs are heterogeneous groups of tumors which are increasingly identified due to their distinct morphological characteristics with variable clinical prognosis. Therapeutic management is not in favor of cystectomy in our study. However, a prospective study using a larger cohort is still necessary to validate our results.
Similar content being viewed by others
1 Background
Urothelial bladder carcinoma (UBC) is well known for its many histological variants [1]. About 80% of the UBC is a pure or conventional urothelial carcinoma (UC), while the remaining 20% is represented by a divergent histological differentiation. The pathophysiological study of these variants has recently aroused growing interest, because the therapeutic approach is not uniform for all entities, for example, the effectiveness of NAC in the neuroendocrine variant [2,3,4,5].
These variants have important diagnostic, prognostic and therapeutic implications.
The diagnosis of these entities requires expertise to better identify them. In one study, 589 samples of transurethral resection of the bladder (TURB) interpreted by expert genitourinary pathologists confirmed the presence of a histological variant which was not reported by general pathologists in 44% of the cases [6].
In the future, a molecular and genetic study of these variants will allow them to be better defined.
An accurate diagnosis allows you to stratify the risks, determine the prognosis and choose an appropriate treatment. The published data come from small retrospective series and extrapolation of data from pure UC; this is due to the rarity of certain subgroups and the exclusion of patients with a histological variant from clinical studies [7].
The treatment of impure UC remains controversial; there is no therapeutic consensus in current practice.
These entities are frequently associated with a poor prognosis. Some authors suggest that impure UC is more aggressive than pure or conventional UC [8], although many authors show that the prognosis after radical cystectomy is identical in the two groups [9].
The aim of this study is to analyze the clinico-pathological and therapeutic aspects of these variants to better understand this invasive disease.
2 Methods
Between January 2017 and October 2019, a retrospective monocentric study including 39 patients with urothelial carcinoma with a histological variant.
Our patients were treated by a radical cystectomy (RC) or a transurethral resection of the bladder (TURB) alone or a TURB with an adjuvant treatment (systemic chemotherapy or endo-vesical immunotherapy type BCG therapy).
2.1 Inclusion criteria
This study included all patients admitted to the urology department for the treatment of bladder cancer with a histological variant, whether endoscopically or by open surgery.
All histological differentiations were included.
2.2 Exclusion criteria
The following were excluded from our study:
-
Patients receiving endoscopic treatment for another pathology
-
Patients refusing the study
-
Patients with pure urothelial carcinoma.
2.3 Statistical analysis
A rigorous statistical methodology has enabled the collection of data and parameters to study various clinical records thanks to an operating sheet including radiological imaging and standardized histological reports according to the guidelines of the French pathology association.
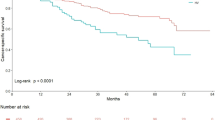
Kaplan–Meier curves were used to assess the impact of different treatments on overall survival. The log-rank test was used to compare these different curves.
The capture of the results, the evaluation of the various statistical indices were carried out using the software SPSS version 10. The results are considered statistically significant for a p < 0.05.
Consent was systematic for all patients included in the study.
3 Results
The details of the clinical and paraclinical parameters of our patients will be set out retrospectively and successively in the tables and figure below.
We collected 39 patients treated for bladder cancer with a histological variant.
3.1 The clinical characteristics of the patients
The mean age was 62 years, with a male predominance 92% versus 8% of the female.
Hydronephrosis was observed in 33.5% of our patients, 30 (77) patients were smoking and 13 (33.5) patients had an ECOG PS ≥ 2.
Fifty-four percentage of patients had a ≥ cT3 stage with clinical lymph node involvement of 28% and at the initial diagnosis, 23% of patients had distant metastases (Table 1).
No patient received neoadjuvant chemotherapy.
3.2 The therapeutic characteristics of the patients
The surgical procedure corresponded in 36% of the patients to a RC always associated with an extensive pelvic lymph node dissection, including the obturator, external iliac, internal iliac and primitive distal iliac regions going up to the crossing of the ureters.
TURB alone was performed in 3% of our patients, 28% had TURB with systemic chemotherapy such as MVAC (methotrexate, vinblastine, doxorubicin and cisplatin), 23% had TURB with BCG therapy and 10% refused treatment radical (Table 1).
No patient was treated with radiotherapy using a multimodal approach.
3.3 The pathological and oncological results of the patients
The ISC was present in the bladder piece in 21.5% against 38% in the bladder biopsy, lymphovascular invasion (LVI) was present in the bladder piece in 28.5% compared to 46% in the bladder biopsy, and lymph node invasion was 28.5%.
The two predominant histological variants were squamous and micropapillary differentiation between the bladder piece and bladder biopsy 28.5%, 30% and 21.5% and 13%, respectively. The percentage of the micropapillary component ≥ 15% was present in 5% of the patients in the bladder biopsy against 7% in the bladder piece (Table 2).
Mixed differentiations were present in the bladder piece in 21% compared to 15% in the bladder biopsy.
The overall survival at 20 months was 70% and 40% for the patients who had RC and the other therapeutic (TURB alone or a TURB with an adjuvant), respectively; there was no significant difference in survival between the two groups (p = 0.27) (Fig. 1).
4 Discussion
Variants of UC tend to be underdiagnosed or misclassified for several reasons [3].
Tumors are heterogeneous and subsampling can compromise the histological recognition of these entities. This explains the variable agreement rate between the specimen of TURB and radical cystectomy (RC) reported in the literature; while some studies show relatively low agreement [4, 5], others report such high rates 83.6% [10]. In our study was able to show a 36% agreement rate.
However, the histology of these variants is difficult to interpret due to the heterogeneity and the percentage of each variant. In addition, it is not uncommon to have several types of variants in the same tumor.
The therapeutic management of various histological variants remains controversial [11]. It is essentially based on the identification of subtypes responding to non-surgical treatment (systemic therapy, intravesical therapy, radiotherapy, etc.) before radical treatment [12].
The role of neoadjuvant chemotherapy (NAC) in the therapeutic arsenal of these variants has shown an improvement in overall survival mainly in the neuroendocrine component and a decrease in the tumor stage compared to other differentiations.
Vetterlein et al. reported significant overall survival in patients with neuroendocrine bladder tumors who received NAC. In addition, patients with micropapillary differentiation and sarcomatoid differentiation have shown a decrease in the disease stage pT3 and/or pN1 when they received NAC [13]. Neoadjuvant chemotherapy has not been used in our population.
The micropapillary component of these variants does not confer a worse prognosis than pure UC in terms of overall survival after total cystectomy. However, NAC was not significantly associated with better survival outcomes, and it resulted in a significant rate of decline in the stage of the disease [14].
Although there is no clear recommendation in the management of these entities, several studies have proven the place of total cystectomy.
Veskimäe et al. reported that in the majority of these variants, such as the micropapillary and plasmocytoid component, the treatment is mainly NAC and radical cystectomy [15].
A meta-analysis published in 2017 reported that the UC variants did not predict a poor prognosis for patients treated with RC. However, the data have shown patients with these variants who receive RC as soon as possible for better results [16].
Stroman et al. reported a decrease in overall survival in patients with histological variants at 14% at 2 years and 23% at 5 years after RC compared to pure UC. Patients should be informed about the high risk and unpredictable nature of these entities and the recommendation for the first RC performed for this indication [17].
The overall survival at 20 months in our study was 70% and 40% for the patients who had RC and the other therapeutic (TURB alone or a TURB with an adjuvant), respectively.
Regarding BCG immunotherapy, Gofrit et al. reported that patients treated with BCG intravesical immunotherapy did not show efficacy even when confirmation of diagnosis with re-evaluation TURB and rigorous follow-up. The progression rate of these patients is high (40% at 5 years compared to 17.5% pure high grade UC). Patients treated with BCG intravesical immunotherapy have a 27% chance of dying from this disease within 5 years, compared with 7.5% chance of high grade UC. As such, these patients should be informed of this adverse clinical course and considerations for cystectomy are strongly recommended [9].
A recent study of 114 phase 2 patients (PURE-01) administered to patients with impure UC three cycles of 200 mg of pembrolizumab preceding a RC. The preliminary results of this study confirm the activity of pembrolizumab in neoadjuvant the treatment of UC infiltrating the muscle with a histological variant [18].
The limitations of this study were mainly the reduced number of patients and the selection bias by default of randomization. Finally, the heterogeneity of both histological variants of urothelial carcinoma of the bladder and also the use of curative therapies are important limits to emphasize. These results are well worth investigating in multicentric prospective studies with a larger sample.
5 Conclusion
UCVs are heterogeneous groups of tumors which are increasingly identified due to their distinct morphological characteristics with variable clinical prognosis.
Therapeutic management is not in favor of cystectomy in our study. However, a prospective study using a larger cohort is still necessary to validate our results.
Future studies are needed to assess the reactivity of different histological variants to new immunotherapy agents.
Abbreviations
- UBC:
-
urothelial bladder carcinoma
- UC:
-
urothelial carcinoma
- TURB:
-
transurethral resection of bladder
- RC:
-
radical cystectomy
- BCG:
-
Bacilli Calmette and Guerin
- ECOG PS:
-
The Eastern Cooperative Oncology Group performance status
- ISC:
-
in situ carcinoma
- LVI:
-
lymphovascular invasion
- NAC:
-
neoadjuvant chemotherapy
References
Moch H, Cubilla AL, Humphrey PA et al (2016) The 2016 who classification of tumours of the urinary system and male genital organs—part A: renal, penile, and testicular tumours. Eur Urol 70:93–105
Kaimakliotis HZ, Monn MF, Cary KC et al (2014) Plasmacytoid variant urothelial bladder cancer: is it time to update the treatment paradigm? Urol Oncol 32:833–838
Porten SP, Willis D, Kamat AM (2014) Variant histology: role in management and prognosis of nonmuscle invasive bladder cancer. Curr Opin Urol 24:517–523
Xylinas E, Rink M, Robinson BD et al (2013) Impact of histological variants on oncological outcomes of patients with urothelial carcinoma of the bladder treated with radical cystectomy. Eur J Cancer 49:1889–1897
Monn MF, Kaimakliotis HZ, Pedrosa JA et al (2015) Contemporary bladder cancer: variant histology may be a significant driver of disease. Urol Oncol 33(18):e15–2
Shah RB, Montgomery JS, Montie JE, Kunju LP (2013) Variant (divergent) histologic differentiation in urothelial carcinoma is under-recognized in community practice: impact of mandatory central pathology review at a large referral hospital. Urol Oncol 31:1650–1655
Lobo N, Shariat SF, Guo CC, Fernandez MI, Kassouf W, Choudhury A, Gao J, Williams SB, Galsky MD, Taylor JA 3rd, Roupret M, Kamat AM (2020) What is the significance of variant histology in urothelial carcinoma? Eur Urol Focus 6(4):653–663
Black PC, Brown GA, Dinney CP (2009) The impact of variant histology on the outcome of bladder cancer treated with curative intent. Urol Oncol 27(1):3–7
Gofrit Ofer N, Yutkin Vladimir, Shapiro Amos, Pizov Galina, Zorn Kevin C, Hidas Guy, Gielchinsky Ilan, Duvdevani Mordechai, Landau Ezekiel H, Pode Dov (2016) The response of variant histology bladder cancer to intravesical immunotherapy compared to conventional cancer. Front Oncol 15(6):43
Sahin AA, Myhre M, Ro JY et al (1991) Plasmacytoid transitional cell carcinoma. Report of a case with initial presentation mimicking multiple myeloma. Acta Cytol 35:277–280
Keck B, Wach S, Stoehr R et al (2013) Plasmacytoid variant of bladder cancer defines patients with poor prognosis if treated with cystectomy and adjuvant cisplatin-based chemotherapy. BMC Cancer 13:71
Li Q, Assel M, Benfante NE, Pietzak EJ, Herr HW, Donat M, Cha EK, Donahue TF, Bochner BH, Dalbagni G (2019) The impact of plasmacytoid variant histology on the survival of patients with urothelial carcinoma of bladder after radical cystectomy. Eur Urol Focus 5(1):104–108
Vetterlein MW, Wankowicz SAM, Seisen T, Lander R, Löppenberg B, Chun FK, Menon M, Sun M, Barletta JA, Choueiri TK, Bellmunt J, Trinh QD, Preston MA (2017) Neoadjuvant chemotherapy prior to radical cystectomy for muscle-invasive bladder cancer with variant histology. Cancer 123(22):4346–4355
Abufaraj M, Foerster B, Schernhammer E, Moschini M, Kimura S, Hassler MR, Preston MA, Karakiewicz PI, Remzi M, Shariat SF (2019) Micropapillary urothelial carcinoma of the bladder: a systematic review and meta-analysis of disease characteristics and treatment outcomes. Eur Urol 75(4):649–658
Veskimäe E, Espinos EL, Bruins HM, Yuan Y, Sylvester R, Kamat AM, Shariat SF, Witjes JA, Compérat EM (2019) What Is the prognostic and clinical importance of urothelial and nonurothelial histological variants of bladder cancer in predicting oncological outcomes in patients with muscle-invasive and metastatic bladder cancer? A European Association of Urology Muscle Invasive and Metastatic Bladder Cancer Guidelines Panel systematic review. Eur Urol Oncol 2(6):625–642
Chen Q, Li L, Wang G, Hu J, Sun T, Fu B (2017) Do histological variants in urothelial carcinoma of the bladder portend poor prognosis? A systematic review and meta-analysis. Oncotarget 8:48263–48271
Stroman L, Nair R, Russell B, Malik N, Desai A, Chandra A, Thurairaja R, Dasgupta P, Khan MS, Malde S (2019) The impact of non-urothelial variant histology on oncological outcomes following radical cystectomy. BJU Int 124(3):418–423
Necchi A, Raggi D, Gallina A, Madison R, Colecchia M, Lucianò R, Montironi R, Giannatempo P, Farè E, Pederzoli F, Bandini M, Bianchi M, Colombo R, Gandaglia G, Fossati N, Marandino L, Capitanio U, Dehò F, Ali SM, Chung JH, Ross JS, Salonia A, Briganti A, Montorsi F (2020) Updated results of PURE-01 with preliminary activity of neoadjuvant pembrolizumab in patients with muscle-invasive bladder carcinoma with variant histologies. Eur Urol 77(4):439–446
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
A.S wrote the article, K.T, K.E, A.K and A.I corrected the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Ibn Sina Hospital in Mohamed V University. The patients provided verbal consent to participate in this study.
Consent for publication
The patient gave his informed and free consent for the publication of this study.
Competing interests
The authors declare that they have no conflicts of interest in connection with this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Saouli, A., Karmouni, T., El Khader, K. et al. Histology of variants of urothelial carcinoma of the bladder: a Moroccan series of 39 cases. Afr J Urol 27, 1 (2021). https://doi.org/10.1186/s12301-020-00106-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-020-00106-w