Abstract
Background
Spermatic cord malignant mesotheliomas (SCM) are extremely rare tumours arising from the tunica vaginalis of the spermatic cord (only 18 cases reported—worldwide in the literature). Paratesticular malignant mesotheliomas (PMM) account for about 0.3–1.4% of all mesotheliomas, while those from the spermatic cord account for less than 10% of paratesticular tumours. Spermatic cord mesotheliomas may be overlooked commonly owing to its unique ability to mimic benign disorders associated with a thickened cord, leading to loss of timely management in many cases. Hence, this case report hence serves to provide pointers to the urologist/surgeon and alerts them towards timely diagnosis and early management of SCM’s besides adding to its limited literature.
Case presentation
We present a case of spermatic cord mesothelioma (SCM) in a 39-year-old male presenting to our clinic with persistentcomplaints of left inguinoscrotal swelling with a vague dull-aching, poorly localising pain sensation over the inguinoscrotal region associated with a persistent dragging sensation for more than a year. Initial evaluation suggested and inclined us towards the diagnosis a benign pathology (spermatocele); however, the persistence of symptoms (pain and swelling) despite prior therapeutic measures initiated elsewhere prompted us to consider an FNAC (which was benign) and surgical exploration which surprisingly revealed the diagnosis of SCM. Owing to the wide spread nature of the disease, the patient was started on palliative chemotherapy. He is currently is doing clinically well on a 1-year follow-up.
Conclusion
Spermatic cord malignant mesothelioma is an extremely rare tumour with an unique tendency to masquerade and mimic cord thickening also associated with several other benign groin/inguinoscrotal swellings. In all such cases, a high index of suspicion should be entertained by the urologist, even in the absence of classical risk factors for SCM like prior asbestos exposure while evaluating patients presenting with persistent expanding inguinoscrotal swellings associated with non-resolving symptoms.
Similar content being viewed by others
1 Background
Paratesticular malignant mesothelioma (PMM) is a rare disease accounting for 0.3–1.4% of all malignant mesotheliomas (malignancy of the mesothelial cells lining the serosal surfaces in the body) with a peculiar but an inconsistent association with asbestos exposure [1]. The rare nature of mesothelioma arising from the peritoneal covering of spermatic cord is suggested by the literature search revealing only 18 reported cases till date.
2 Case presentation
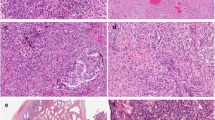
A 39-year-old male presented with complaints of persistent left inguinoscrotal swelling with a vague dull-aching, poorly localising pain over the region of the swelling with a persistent dragging sensation for more than a year with no significant past, family/medical history. The patient had approached several practitioners elsewhere owing to chronicity of condition with no relief obtained by variety of their treatment modalities like multiple antibiotic courses, analgesics, scrotal support and local anaesthetic injections. The patient also gave history of anti-tubercular drug therapy prescribed empirically by one of the practitioners that attended him but unfortunately had no formal records of same. Focussed examination revealed a non-tender, firm, and non-reducible left inguinoscrotal swelling with separate palpable normal bilateral testis, no significant inguinal adenopathy and normal external genitalia/abdominal examination. The blood biochemistry/urinalysis was unremarkable. Scrotal ultrasonography revealed a bulky heteroechoic left spermatic cord interspersed with hypoechoic areas/ectatic lymphatic channels suggestive of a left spermatocele. Hence owing to the mismatch/dicrepancy between clinical (smooth, firm, enlarged inguinoscrotal swelling that suggested probable benign epididymal enlargement) and ultrasonographic findings (that suggested a spermatocele) and the thought that both these conditions would not usually cause such persistent symptoms, a fine needle aspiration cytology (FNAC) evaluation was executed under image guidance which revealed the presence of numerous sperms amidst the clear background of no inflammation/foreign-body giant cells that suggested a spermatocele. Thus, considering the non-relieving nature of patient’s persistent painful symptoms despite prior multiple treatment courses/options executed elsewhere over the past year, an inguinoscrotal exploration was considered with the primary intent of spermatocelectomy to relieve the persistent patient symptoms. However contrary to the preoperative clinical diagnosis, intraoperative findings revealed a diffusely thickened firm spermatic cord with an apparent normal testis (Fig. 1). Due to non-availability of frozen section services at the odd hour and an intraoperative suspicion of a spermatic cord neoplasm, an uneventful high inguinal orchiectomy was performed. Post-operative histopathology and immuno-histochemistry (IHC) revealed normal testicular architecture and a 5–10% Ki67 index (indicating mild to moderate proliferation capacity) suggested a spermatic cord mesothelioma
(Fig. 2a–e). Follow-up PET-CT scan suggested fluorodeoxyglucose (FDG) avid peritoneal deposits in the gastrohepatic, gastrocolic ligaments, peripancreatic region and greater omentum with foci of residual disease in the left inguinal region probably from the orchiectomy stump (Fig. 3). Considering the widespread nature of disease, he was referred to oncology department and is currently doing well on cisplatin-based palliative chemotherapy with three monthly follow-up in the outpatient clinic for the past 1 year.
Panel images a, b showing H&E staining revealing stromal invasive neoplasm with papillary and glandular configuration (10×) with cuboidal lining cells with scant to moderate amount of eosinophilic cytoplasm and bland nuclear features (40×). IHC analysis (section c–f) showed Cytokeratin 7 and Calretinin positivity with Cytokeratin 20 negativity. The Ki67 index of the tumour was 5–10% indicating mild to moderate proliferation capacity
3 Discussion
Paratesticular malignant mesotheliomas are rare tumours arising from the tunica vaginalis of the spermatic cord that in 30–55% may clinically present as scrotal masses/expanding hydrocele [2, 3]. The present case was similar in mimicking benign conditions of spermatic cord like filariasis, epididymorchitis, funiculitis, spermatocele, cord lipoma and inguinal hernia. Spermatic cord mesotheliomas usually present in 6–8th decade with the exception of those associated with classical history of childhood asbestos exposure which present at an earlier age [3]. Other etiological risk factors believed to be associated with SCM include trauma, prior herniorrhaphy and long-standing expanding hydroceles [2]. Paratesticular malignant mesotheliomas are extremely rare and aggressive neoplasms capable of a silent widespread lymphatic and haematogenous metastasis at the time of presentation/diagnosis [4].
The present case of inguinoscrotal swelling was initially evaluated in terms of benign conditions such as chronic epididymitis, tubercular epididymitis and extrascrotal spermatoceles as the presentation of the current case mimicked these benign aetiologies which incidence wise also vastly outnumber malignant spermatic cord swellings. The younger age of the patient (39 years), good nutritional status and a chronic inguinoscrotal swelling in the absence of classical risk factors of spermatic cord malignancies (asbestos exposure) inclined us towards consideration of a benign pathology. Thus our initial line of management was primarily an ultrasound imaging followed by an ultrasound guided FNAC due to the clinico-investigational mismatch. FNAC, revealed a benign diagnosis (spermatocele) coupled with reasons mentioned previously prevented us from further considering a trucut biopsy/preoperative CECT evaluation.
A definite preoperative diagnosis is seldom feasible and a combination of CT/MRI with PET imaging and post-operative histopathology/IHC usually offers the confirmatorydefinitive diagnosis. According to Ahmed et al. [5], confirmation is possible with IHCrevealing cytokeratin positivity for (CKAE1/AE3, CK7, CK5/6, EMA, K2-40, thrombomodulin, Calretinin and WT1) and negative for (CK20, BerEP4, B72’3, MOC-31 and Leu M1).
Considering the scarce amount of literature available on SCM, unsurprisingly there is no established protocol for evaluation and management at present. Surgical clearance with a high inguinal orchiectomy and retroperitoneal lymphadenectomy with adjunctive cisplatin based chemotherapy or radiotherapy appears to be the only potential curative option in localised cases though according to one review the same may be associated with a 60% high rate of local recurrence within 2 years with mortality approaching 30% after a median survival of 2 years [4].
The evaluating practitioner hence should endeavour to initiate early focussed treatment in all such cases as age at the time of presentation is the single most vital prognostic factor in paratesticular malignant mesothelioma [3, 4, 6]. This report serves to alert the urologist/practitioner to refrain from dismissing spermatic cord swellings as benign especially in the setting of a persistent swelling with resistance to usual treatment modalities with sinister conditions like the spermatic cord mesothelioma that may present without classical risk factors and masquerade as benign pathologies leading to infrequent diagnoses at an advanced stage of the disease.
4 Conclusion
Spermatic cord malignant mesothelioma is a rare tumour with a sinister tendency to closely mimic several benign groin masses. A high index of suspicion should be entertained in patients presenting with an expanding inguinoscrotal swelling even in the absence of classical risk factors. Early diagnosis and timely management form the primary pillars of successful management of spermatic cord mesotheliomas.
Availability of data and material
Not applicable.
Abbreviations
- SCM:
-
apermatic cord mesothelioma
- PMM:
-
paratesticular malignant mesotheliomas
- IHC:
-
immunohistochemistry
- PET/CT:
-
positron emission tomography/computerised tomography
- FDG:
-
fluorodeoxyglucose
- FNAC:
-
fine needle aspiration cytology
References
Park YJ, Kong HJ, Jang HC, Shin HS, Oh HK, Park JS (2011) Malignant mesothelioma of the spermatic cord. Korean J Urol 52(3):225–229
Plas E, Riedl CR, Pflüger H (1998) Malignant mesothelioma of the tunica vaginalis testis: review of the literature and assessment of prognostic parameters. Cancer 83(12):2437–2446
Bisceglia M, Dor DB, Carosi I, Vairo M, Pasquinelli G (2010) Paratesticular mesothelioma. Report of a case with comprehensive review of literature. AdvAnatPathol 17(1):53–70
de Jalón AG, Gil P, Azúa-Romeo J et al (2003) Malignant mesothelioma of the tunica vaginalis. Report of a case without risk factors and review of the literature. Int UrolNephrol 35:59–62
Ahmed I, Ahmed Tipu S (2013) IshtiaqS. Malignant mesothelioma. Pak J Med Sci 29(6):1433–1438
Hassan R, Alexander R (2005) Nonpleural mesotheliomas: mesothelioma of the peritoneum, tunica vaginalis, and pericardium. Hematol Oncol Clin N Am 19(6):1067–1087
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
IS was the responsible consultant surgeon in-charge of the overall care of the patient and on whom the final decision on the patient management rested. IS and ATK composed the first draft of the manuscript. ATK and DPB were involved in day-to-day patient care and follow-up. DJ was responsible for providing histopathology workup and immune-histochemistry pictures. NP provided insight and valuable inputs to the manuscript, collected references and was responsible for typography of final manuscript draft. All authors have read and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed signed consent to publish executed. Personal identifiers have been removed to preserve anonymity. Written informed consent has been executed/signed by the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Singh, I., Aravind, T.K., Behera, D.P. et al. Malignant mesothelioma of the spermatic cord mimicking a benign inguinoscrotal swelling: case report with review of literature. Afr J Urol 26, 87 (2020). https://doi.org/10.1186/s12301-020-00095-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-020-00095-w