Abstract
Gut microbiota regulates various aspects of human physiology by producing metabolites, metabolizing enzymes, and toxins. Many studies have linked microbiota with human health and altered microbiome configurations with the occurrence of several diseases, including cancer. Accumulating evidence suggests that the microbiome can influence the initiation and progression of several cancers. Moreover, some microbiotas of the gut and oral cavity have been reported to infect tumors, initiate metastasis, and promote the spread of cancer to distant organs, thereby influencing the clinical outcome of cancer patients. The gut microbiome has recently been reported to interact with environmental factors such as diet and exposure to environmental toxicants. Exposure to environmental pollutants such as polycyclic aromatic hydrocarbons (PAHs) induces a shift in the gut microbiome metabolic pathways, favoring a proinflammatory microenvironment. In addition, other studies have also correlated cancer incidence with exposure to PAHs. PAHs are known to induce organ carcinogenesis through activating a ligand-activated transcriptional factor termed the aryl hydrocarbon receptor (AhR), which metabolizes PAHs to highly reactive carcinogenic intermediates. However, the crosstalk between AhR and the microbiome in mediating carcinogenesis is poorly reviewed. This review aims to discuss the role of exposure to environmental pollutants and activation of AhR on microbiome-associated cancer progression and explore the underlying molecular mechanisms involved in cancer development.
Similar content being viewed by others
Introduction
The human body is a complex ecosystem hosting trillions of commensal microbes, collectively known as “microbiota” [1, 2]. These microbes represent over 5,000 species, including archaea, bacteria, protists, viruses, and fungi, among which bacteria are the most abundant [3, 4]. The human microbiome refers to the collective genetic makeup and byproducts of these microorganisms that inhabit the human body [3]. Approximately 90% of human cells are associated with microbiota, while only 10% are microbiome-free [5]. Commensal microbes reside in numerous sites within the human body, including the skin, oral cavity, and, most prominently, the gut [3, 6].
The mammalian gut is arguably one of the most advanced and complex communities of commensal microbes and presents the highest concentration of microorganisms in the human body [1, 2, 7]. The gut microbiome has been characterized as “the last undiscovered human organ” due to its significant impact on human health [8]. Gut microbiota was shown to play a profound role in regulating various aspects of human physiology by producing metabolites, metabolizing enzymes, and toxins [9]. Consequently, it helps protect the body from pathogenic invaders, promotes the development of the immune system, aids in food digestion and nutrient uptake, and may even influence mood and behavior [3, 6, 9]. Moreover, through their interaction with epithelial and stromal cells, gut microbiota regulates mucosal immune homeostasis, acts as a barrier, controls pathogen overgrowth, and maintains host–microbiota symbiosis [2, 10,11,12]. Therefore, dysbiosis, an alteration in the composition or function of the gut microbiome in response to environmental or host-related changes in a way such that the balance between beneficial microorganisms and pathogenic microorganisms is lost[13, 14], has been increasingly linked to the emergence of diverse pathological conditions such as obesity [15,16,17], diabetes [18,19,20], cardiovascular diseases [21], neurological disorders [22,23,24], and even psychological disorders [25, 26]. Furthermore, altered gut microbiota contributes to developing autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus [27, 28]. Recently, a growing body of evidence has revealed a link between gut microbiota and cancer [2, 26].
The normal gut microbiota is dominated by four major phyla of bacteria: Bacteroidetes, Firmicutes, Proteobacteria, and Actinomycetes [2]. Firmicutes and Bacteroidetes account for more than 90% of the bacterial population in the gastrointestinal tract (GIT), while Actinobacteria and Proteobacteria are less abundant [29]. Nevertheless, each individual’s exact composition of gut microbiota is distinctive [3]. In 2010, researchers suggested that individuals could be characterized on the basis of the significant constituents of their gut microbiome to possess distinct “enterotypes” which are shaped by factors such as geographical area, diet pattern, genetic features, lifestyle, and environmental factors [30,31,32,33]. For example, transplanting fecal microbes from obese donors to germ-free mice induced higher weight gain than similar mice receiving fecal microbiota from lean donors [33]. These findings highlight the physiological importance of microbiota equilibrium, which appears to be unique for each individual [3, 34]. It has been suggested that once established, the gut microbiome’s composition remains relatively unchanged and resilient throughout adult life. However, factors such as bacterial infections, use of antibiotics, smoking, and disease states may still alter the human gut microbiome’s composition [2, 3, 30,31,32,33].
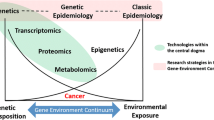
Gut microbiome and cancer
Over the years, several studies have begun to direct focus on the study of gut microbiota and its implications on human health. Advancements in biomedical research have shed light on how disruptions in the gut microbiota could likely contribute to the etiology of disease pathogenesis [35]. Although initial studies were specific to enteric infections [36], over the past decade, microbiome research has rapidly shifted from pathology-related laboratory-based studies toward research that enables the enumeration of specific intestinal bacteria specimens, their genes, and metabolic products [37]. The National Institute of Health in the USA launched the Human Microbiome Project to establish a microbial genome database. This database provided insight into the diversity of microbial organisms, their genomic information, and their interaction across several organ systems, including the GIT, oral cavity, nares, and breast [38]. Extensive advancements in high-throughput techniques such as transcriptomics, sequencing, and metabolomics studies have further facilitated the understanding of the association between gut microbiota and a spectrum of immunological, neuro-psychiatric [39], and allergic disorders [40], atherosclerosis [41], obesity and diabetes [42], Parkinson’s disease [43], autism [44], central nervous system dysfunction [39], and malignancies [41, 45].
An accumulating body of evidence has shown that the microbiome can influence the development, progression, and therapeutic outcomes of cancer patients [4, 6, 8, 26, 46]. Particularly, alteration in the gut microbiota and infection of tumors with the microbiota of the gut and oral cavity have been linked to the initiation and progression of various types of tumors, including gastric cancer [47, 48], colorectal cancer (CRC) [46], and esophageal cancer [49]. Besides, it was found that the effects of gut microbiome extend beyond the GIT, where it can promote carcinogenesis in distant organs such as the liver [50, 51], pancreas [52, 53], breast [54], and brain [55]. Around 20% of the worldwide tumors’ burden is estimated to be triggered or modulated by microbes and their byproducts [9, 56]. Several studies utilizing metagenomic approaches revealed novel pathogens enriched in different types of tumors compared to surrounding tissues or healthy individuals, indicating that the microbiome is now recognized as a prospective hallmark of cancer [57].
While alterations in gut microbiome composition can promote carcinogenesis, they, on the other hand, may reduce the risk of cancer development. Evidence highlights the microbiota’s dual function in maintaining individuals’ overall well-being [3]. Host microbiomes were shown to possess several functions that maintain homeostasis and prevent cancer development, including reinforcing mucosal barrier [58], enhancing antitumor immune responses [59], suppressing inflammation [60], and reducing genotoxicity [61].
On the other hand, the crosstalk among certain microbial species and infection of tumors with bacteria was found to influence cancer pathology by acting on DNA stability, cancer immune responses, and microenvironment composition [62, 63]. Alterations in the gut microbiome increase the risk of GIT malignancies and promote carcinogenesis by inducing chronic inflammation, releasing mutagenic metabolites, and promoting cell proliferation [4, 46, 64]. For instance, the colonization of Helicobacter pylori stimulates immune responses and persistent inflammation, resulting in gastritis and ultimately leading to gastric cancer [65,66,67]. Further analysis revealed that several genes of Helicobacter pylori alter tissue homeostasis, leading to the accumulation of cytokines and activation of other cancer-causing signaling, such as the β-catenin signaling pathway [65, 68]. On the other hand, eradicating Helicobacter pylori reduced the risk of developing gastric cancer, suggesting that it plays a significant role in the early stages of gastric carcinogenesis [69]. Moreover, epigenetic alterations could mediate microbiome effects on carcinogenesis [4]. For example, Helicobacter pylori-induced murine gastric tumor was associated with hypomethylation and reduction of miR-490-3p [70].
A previous study also demonstrated a connection between the gut microbiome and esophageal cancer. In a fluorescence in situ hybridization study with a CY3-labeled Fusobacterium nucleatum (Fn)-specific probe, Fn was significantly more abundant in esophageal squamous cell carcinoma (ESCC) tissues than adjacent non-cancerous tissues. It appeared to correlate with the tumor stage, with Fn DNA levels significantly higher in advanced ESCC (Stage III–IV) than in early-stage ESCC (Stage I–II). The presence of Fn within the deep layers of the tissue indicated that this was not surface-level contamination from the oral cavity. BALB/C nude mice subcutaneously injected with KYSE-450 ESCC cells had significantly higher tumor volumes when the cells were pretreated with Fn compared with the negative control [71].
Similarly, the development of CRC has also been associated with specific types of microbes [46]. The gut microbiota signature analysis between patients with CRC and healthy individuals revealed a statistically significant difference between the two groups [72, 73]. For example, certain bacterial species such as Bacteroides fragilis (Bf), Fn, and Porphyromonas asaccharolytica (Pa) were found to be enriched in fecal metagenomic samples isolated from patients with CRC [74,75,76], suggesting that gut microbiome could serve as a noninvasive diagnostic marker for CRC. Additionally, even within the same patient, significant differences were found in microbiota community arrangements in tumor tissues as compared to surrounding normal tissues, in which Fusobacterium and Lactococcus were overrepresented, whereas Pseudomonas and Escherichia/Shigella were underrepresented [3, 77, 78].
Moreover, unique metagenomic and metabolomic shifts have been noticed in different stages of CRC, starting from polypoid adenomas and intramucosal carcinomas and moving to more advanced and metastatic lesions [79]. Notably, Fn’s relative abundance increased continuously with disease progression from intramucosal carcinomas to more advanced stages [79]. On the other hand, Atopobium parvulum and Actinomyces ondontolyticus were enriched only in multiple polypoid adenomas and intramucosal carcinomas. These findings were derived from multiomics data of a large cohort (n = 616) and suggested that microbiome and metabolome changes start from the early stages of CRC, highlighting its potential etiological and diagnostic relevance [79, 80]. Mechanistically, preclinical studies demonstrated that Fn promotes CRC cell proliferation in vitro and patient-derived CRC xenograft models by modulating the Wnt/β-catenin signaling pathway [81, 82]. Additionally, Fn can suppress immune surveillance by inhibiting the cytotoxic responses of tumor-infiltrating lymphocytes and natural killer cells through binding to the T-cell immunoreceptor with Ig and ITIM domains (TIGIT), an inhibitory immune checkpoint, protecting Fn and surrounding tumor cells from immune-mediated killing [83]. Moreover, additional preclinical studies have further established a direct causative relationship between the microbiome and the development of several types of cancer. For instance, feeding fecal samples from patients with CRC to healthy animals induced higher proinflammatory cytokines, altered immune responses, and initiated procarcinogenic signals and tumorigenesis in both germ-free and conventional mice models compared with feeding control fecal samples from healthy individuals [84].
Nevertheless, the exact underlying mechanisms have not been fully elucidated. Numerous studies have been undertaken to understand the mechanisms behind dysbiosis-mediated carcinogenesis and suggested several potential mechanisms. These mechanisms include the promotion of an inflammatory tumor microenvironment, epithelial–mesenchymal transition, production of reactive oxygen species (ROS), and suppression of tumor immune surveillance [3, 5, 85].
Mechanisms through which the gut microbiome induces cancer
Gut dysbiosis alters the healthy gut microbiome’s composition and function, causing a loss of balance between beneficial and pathogenic microorganisms [13, 14]. Several intestinal microorganisms have been associated with carcinogenesis, including Fn, Escherichia coli, Bf, Streptococcus gallolyticus (Sg), Clostridium septicum, Enterococcus faecalis (Ef), and Pa [14]. Several mechanisms have been proposed regarding how the gut microbiome can contribute to carcinogenesis, including but not limited to genotoxicity, immune tolerance, chronic inflammation, secreting oncogenic metabolites, expressing oncogenic virulence factors, and inducing oxidative stress [13]. Illustrative mechanisms are described in Fig. 1.
Mechanisms through which the gut microbiome contributes to oncogenesis. Fn expresses various virulent factors that activate prooncogenic pathways. FadA adhesin expressed by Fn binds to E-cadherin, leading to activation of Annexin 1 and activation of the Wnt/β-catenin signaling pathway. Activation of TLR4 by LPS activates NF-κB to upregulate the production of miRNA-21, which promotes oncogenesis by inducing the Wnt/β-catenin pathway and inhibiting RASA1, a GTPase activating protein that normally inhibits the Ras/Raf/MAPK pathway. Activation of TLR4 by LPS also upregulates the CYP2J2/12,13-EpOME pathway, promoting tumor migration, invasion, EMT, and metastasis. Microorganisms also secrete different metabolites which activate the AhR pathway, which contributes to oncogenesis through various mechanisms, one of which is through crosstalk with the Wnt/β-catenin signaling pathway. Created with BioRender.com
Fusobacterium nucleatum (Fn)
Several studies have shown the role of Fn in gastrointestinal cancers and have highlighted several mechanisms through which Fn contributes to the development and progression of different cancer types. The effect of Fn on cancer cells appears to depend on the tumor type, as coincubation with Fn significantly stimulated the growth of several in vitro CRC cells, such as AA/C1/SB10C, HCT116, DLD1, SW480, and HT29 CRC cells [82, 86], but did not stimulate the growth of lung cancer (PC-9), prostate cancer (22RV1), bladder cancer (UMUC3), or breast cancer (MCF-7) cells [82]. Furthermore, upon assaying Fn levels in tissue sections from patients with colorectal adenomas and carcinomas, Fn levels were found to significantly increase with disease progression from tubulovillous adenoma to tubular adenoma, high-grade dysplasia, and eventually to CRC, and negatively correlate with overall survival [87]. Recently, Fn infection was reported to have the greatest negative prognostic impact in patients with high-risk, mesenchymal-rich tumors of the consensus molecular subtype 4 (CMS4). By contrast, this correlation is not observed in non-mesenchymal tumors (CMS1-3). Furthermore, the relative abundance of Fn in patients’ tumors was found to be positively associated with tumor proliferation, metastasis, and DNA damage [88]. In addition, several virulence factors expressed by Fn may contribute to these effects.
FadA interaction with Wnt/ β-catenin
Fn binds and invades AA/C1/SB/10C (aka 10C) CRC cells more efficiently than their non-cancerous counterpart AA/C1/SB (aka SB) cells. Annexin 1, a membrane protein previously found to be upregulated in 10C cells [89], seems to play an essential role in the interactions between Fn and cancer cells, as its downregulation in aka 10C cells reduced Fn binding and invasion. Conversely, overexpression of Annexin 1 in non-cancerous aka SB cells significantly increased Fn binding and invasion [82]. The growth stimulation appears to be mediated through FadA, as FadA-deficient Fn strains failed to stimulate CRC cell growth [82, 86]. FadA adhesin, a virulence factor expressed by Fn to mediate attachment and invasion, binds to E-cadherin (CDH1) and upregulates Annexin 1, which in turn activates Wnt/β-catenin signaling, leading to overexpression of oncogenes and inflammatory genes [82, 86].
Fap2 lectin
Fap2 lectin, another virulence factor expressed by Fn, recognizes and binds to d-galactose-β(1–3)-N- acetyl-d-galactosamine (Gal-Gal-NAc), which is overexpressed in CRC cells [90]. In another study, Fap2 was found to bind to the inhibitory TIGIT receptor on tumor-associated T cells and natural killer (NK) cells, leading to immune cells’ inhibition of cancer cell killing [91].
MicroRNA-21
Another mechanism through which Fn contributes to carcinogenesis is microRNA regulation. In HCT116 CRC cells, treatment with Fn followed by microarray analysis identified that Fn stimulates the Toll-like receptor 4 (TLR4) signaling to MYD88, which may be mediated through the binding of Fn lipopolysaccharide (LPS) to TLR4 [92], leading to activation of the nuclear factor κB (NF-κB). In turn, NF-κB upregulates the oncogenic miRNA-21 promoter activity, which reduces the levels of the RAS GTPase-activating protein (RASA1), a tumor suppressor that inactivates the oncoprotein RAS [93], a well-known activator of the Ras/Raf/MAPK pathway [94]. There could also be potential crosstalk between miRNA-21 and the Wnt/β-catenin pathway, as miRNA-21 knockdown in mice was found to significantly decrease tumor size and number, increase E-cadherin level, and decrease the expression of β-catenin, NF-κB, signal transducer and activator of transcription-3 (STAT3), Bcl-2, and SOX-9 [95].
CYP2J2 pathway
Activation of TLR4 by Fn could also contribute to carcinogenesis through upregulation of the cytochrome P450 (CYP) 2J2 (CYP2J2) and its metabolites, 12,13-epoxy octadecenoic acid (12,13-EpOME) production by activating the nuclear factor erythroid 2-related factor 2 (NRF2) pathway. Mechanistically, upon activation, NRF2 liberates from KEAP1 and then translocates to the nucleus and binds to the promoter region of the CYP2J2 to induce its transcriptional expression. A significant correlation was found between Fn level and CYP2J2 expression in human CRC tissues. Knocking down CYP2J2 in LoVo CRC cells significantly reduced the effect of Fn on promoting invasion, migration, epithelial–mesenchymal transition (EMT), and metastasis. These findings were validated in vivo using a model of azoxymethane-induced CRC in mice, where Fn-treated wild-type mice had significantly higher tumor loads than Fn-treated Cyp2j5 knockout mice. This mechanism may contribute to the poor overall survival in patients with a high tumor expression of CYP2J2, as noted in The Cancer Genome Atlas (TCGA) database [96].
Autophagy and modulating chemoresistance
Coculture of the CRC cells, HCT116 and HT29, with Fn increased the expression of several autophagy-regulated markers, such as pAMPK, ULK1, pULK1, ATG7, and LC3-II. Correspondingly, the chemosensitivity of these cells to oxaliplatin and 5-fluorouracil, anticancer drugs, was reduced upon coculture with Fn, an effect that was abolished by treatment with chloroquine, a known autophagy inhibitor [97]. It has been demonstrated that Fn mediates autophagy and chemoresistance through downregulating miRNA-18a and miRNA-4802 expression. In patients with CRC, cancer recurrence was significantly correlated with high Fn levels, high expression of autophagy markers, and low expression of miRNA-18a and miRNA-4802 [97]. Fn was noted to also confer chemoresistance in ESCC cells through the activation of autophagy[98]. Oral treatment with the antibiotic metronidazole in mice with Fn-positive patient-derived CRC xenografts significantly reduced Fn load, tumor growth, and tumor cell proliferation[99].
Numb protein
Numb is a crucial cell fate regulator responsible for cell differentiation, tumor suppression, and rendering stemness onto cancer cells [100]. A recent study has shown that infecting CRC cells with Fn promotes cancer stem cell (CSC) features such as self-renewal through the activation of fatty acid oxidation and triglycerol synthesis. This leads to high lipid droplet production with Numb degradation. The study also showed that the promotion of CSCs by the action of the microbe is attributed to the activation of NF-κB, which led to the upregulation of carnitine palmitoyltransferase 1B, the enzyme that catalyzes the rate-limiting step of fatty acid oxidation, in CSCs [100]. Taken together, this study demonstrated that Fn renders stem cell-like features on CRC and could, therefore, promote cancer cells’ self-renewal ability.
Streptococcus gallolyticus (Sg)
Sg is a strain of bacteria significantly associated with CRC. In vitro, the coincubation of CRC cells, such as HCT116, HT29, and LoVo, with Sg promoted their proliferation. However, this phenomenon was not observed in SW480 and SW116 CRC cells or normal human colon epithelial cells, indicating that the effect may be cell-specific. In an in vivo mouse model of azoxymethane-induced CRC, administration of Sg by oral gavage led to a significantly higher tumor burden compared with mice treated with normal saline [101]. This Sg-induced CRC proliferation in vitro and in vivo was mediated through the activation of β-catenin and its downstream targets c-Myc and cyclin D1, whereas the Sg-induced cell proliferation was abolished by knocking down β-catenin [101].
Bacteroides fragilis (Bf)
Compared with nontoxigenic Bf, enterotoxigenic Bf (ETBF) was found to induce colon tumors in mice heterozygous for the adenomatous polyposis coli (Apc) gene. This effect is mediated through selective induction of STAT3, initiating a Th17-dominant immune response that contributes to carcinogenesis [102]. ETBF also produces an enterotoxin, known as Bf toxin (BFT), which, in addition to causing inflammatory diarrhea, it activates MAPK and NF-κB pathways [103, 104] and cleaves the extracellular domain of E-cadherin, causing the release of β-cateninand and subsequent activation of downstream oncogenic pathways [105].
Escherichia coli
Certain strains of Escherichia coli, namely the phylogenetic group B2, possess a conserved genetic island called “pks island” which codes for non-ribosomal peptide synthetases and polyketide synthetases. These enzymes produce a genotoxin, colibactin, that causes double-strand breaks in DNA and thus possibly contributing to CRC development [106]. These strains were significantly more prevalent in colon specimens from patients with CRC than in patients with diverticulosis as a non-cancer control group [107].
Enterococcus faecalis (Ef)
Ef is a Gram-positive intestinal commensal bacterium that has been linked to CRC through two oxidative stress-mediated mechanisms. First, Ef produces extracellular superoxide, which causes lipid peroxidation leading to the formation of highly reactive electrophilic compounds, such as 4-hydroxy-2-nonenal. These compounds are potent genotoxins that bind with the DNA causing adducts and interfering with microtubule polymerization, thereby interfering with the formation of the mitotic spindle, causing tetraploidy and aneuploidy [108]. Second, Ef contributes to the risk of CRC by producing high levels of highly reactive hydroxyl radicals, causing oxidative stress [109].
Peptostreptococcus anaerobius (Pa)
Pa was found to be more abundant in patients with CRC compared with healthy subjects. Pa promotes tumor cell proliferation by binding to TLR2 and TLR4 on colon cells to induce ROS production [110]. Furthermore, Pa binds to colon cell integrins using its putative cell wall binding repeat 2 (PCWBR2) receptor to activate phosphoinositide 3-kinases (PI3K)/Akt pathway, which stimulates cell proliferation and NF-κB-mediated inflammation [111].
Environmental factors and microbiome-induced cancer
Interaction between the gut microbiome and environmental factors, such as diet, pollutants, and smoking, has recently been reported to contribute to cancers [112]. A strong positive association was found between Fn-positive colorectal tumors and consuming foods rich in red and processed meats [112]. It has been shown that the effect of exposure to environmental toxicants, such as aromatic hydrocarbons, may be dependent on the presence of specific gut microbiome populations [113]. For example, halogenated aromatic hydrocarbons (HAHs), such as 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD), are persistent organic pollutants that bioaccumulate, particularly in fat tissue, through the food chain. As such, in addition to occupational exposure, human exposure to them is also possible through the consumption of meat, eggs, dairy products, and fatty fish [114]. Furthermore, polycyclic aromatic hydrocarbons (PAHs), such as benzo[a]pyrene (BaP), which have been linked to CRC in humans [115], are commonly found in processed meats and have been found to significantly upregulate oncogenes (e.g., KRAS) and downregulate tumor suppressor genes, such as TP53 [116]. In addition to their connection to cancer, exposure to PAHs was also found to induce a shift in the gut microbiome metabolic pathways, favoring a proinflammatory microenvironment [117]. It is well documented that PAHs and HAHs exert their toxicity and carcinogenicity through the interaction with and activation of a transcription factor, the aryl hydrocarbon receptor (AhR) [118]. However, the role of the AhR pathway in microbiome-mediated cancer remains unlocked. The next section of the review will discuss the crosstalk between AhR and microbiome in cancer development and progression.
The aryl hydrocarbon receptor (AhR) pathway and cancer development
AhR is a cytosolic ligand-activated transcription factor that belongs to the bHLH-PAS (basic helix-loop-helix-Per/Arnt/Sim) protein family [119]. AhR is actively involved in the regulation of several transcription genes involved in cell proliferation [120], apoptosis [121], development, and immunomodulation [122]. Over the years, several studies have demonstrated activation of AhR plays a significant role in cancer initiation and promotion. AhR is activated by PAHs, such as BaP, benzoflavones, and benzanthracenes, and HAHs, such as dibenzofurans, biphenyls, and dioxins, the most notable of which is TCDD, the most potent AhR activator [118, 120]. Following ligand binding, AhR undergoes conformational changes and translocates to the nucleus, dimerizing with AhR nuclear translocator (ARNT) [121]. The formed AhR–ARNT complex then binds to specific DNA-responsive elements, the dioxin-responsive elements (DRE), to initiate the transcription expression of the AhR target genes, cytochrome P450 1A1 (CYP1A1) and CYP1B1 [122, 123]. The CYP1A1 and CYP1B1 then bioactivate pollutants into highly reactive and carcinogenic intermediates that initiate cancer [118, 124].
In support of the role of AhR in cancer development, researchers have identified upregulated expression of AhR in human and rodent tumors, such as breast cancer [125,126,127], lung adenocarcinoma [128, 129], and ovarian cancer [130], implicating the role of AhR in tumor progression. Interestingly, AhR also holds a functional role in the molecular mechanisms governing the development of CSCs, which are well-known tumor-initiating cells, along with being targets for several chemical carcinogens. AhR has not only been found to be constitutively expressed in cancer tissues but its activation has also been strongly linked to CSC progression and renewal [131]. Of particular interest, there was a study that explored the mechanistic role of the AhR/CYP1A1 signaling pathway in controlling the progression of breast CSCs. Findings from the study provide significant evidence that activation of the AhR signaling pathway leads to the development and progression of CSCs through inhibiting the tumor suppressor protein PTEN and the activation of the Akt and Wnt/β-Catenin pathways [132].
AhR and microbiome crosstalk in cancer
Several recent studies, summarized in Table 1, have demonstrated a connection between AhR and the prooncogenic bacteria commonly found colonizing the tumor microenvironment. Analysis of the datasets from the TCGA database and the European Genome-phenome Archive (EGA) identified a significant association between AhR signaling and the abundance of Fn in CRC tissues [133]. Coculture of ESCC cell lines, such as KYSE-450 and KYSE-150, with Fn significantly promoted cell proliferation, colony formation, and cell migration compared to the control [71]. Interestingly, a subsequent high-throughput sequencing study on Fn-treated ESCC cells has identified CYP1A1, the major target gene for AhR pathway activation, as the most significantly upregulated gene. Similarly, patient-derived ESCC tissues with a high abundance of Fn had higher CYP1A1 protein levels than those with low Fn. In addition, inhibition of CYP1A1 either genetically using the shRNA lentivirus vector or pharmacologically using CH223191 abolished the effects of Fn on cell proliferation and colony formation in vitro and tumor growth in vivo [71]. In CRC cells, coculture of T18 cells with Fn was found to upregulate AhR, cancer stemness markers, CYP1A1, Wnt signaling, and MAPK signaling [133]. Similar findings were observed in another study, in which incubation of Sg with CRC cell lines, such as HT29, Caco-2, SW480, and HCT116, increased the expression of CYP1A1 and the CSC marker, aldehyde dehydrogenase 1 (ALDH1) in an AhR-dependent manner [134]. Furthermore, pretreatment of HT29 cells with Sg increased the genotoxicity of 3-methylcholanthrene, a PAH and CYP1A1 inducer [134]. These findings highlight the importance of the interaction between environmental toxins and the gut microbiome, as well as the role of the AhR/CYP1A pathway; however, more research is needed to determine whether the effect is due to CYP1A1- and/or AhR-dependent mechanisms.
Mechanisms of AhR and microbiome crosstalk in cancer
The main proposed mechanisms through which the gut microbiome activates AhR within the tumor microenvironment are illustrated in Fig. 2. Several studies have shown that the gut microbiome represents a rich source of AhR ligands, many of which are products of tryptophan metabolism [135]. Tryptophan is an essential amino acid obtained upon proteolysis of dietary protein. While most ingested tryptophan is absorbed into systemic circulation for use by the host in protein synthesis, approximately 10–20% of it undergoes further metabolism in the GIT by either host enzymes or gut microbiota [135]. There are four known competing catabolic pathways by which tryptophan can enter the GIT: kynurenine (Kyn) pathway (90–95%), serotonin pathway (2%), bacterial indoles pathway (5%), and tryptamine pathway (1%) [136].
Mechanisms of AhR activation by microbiome in the tumor microenvironment. The microbiome within the tumor microenvironment secretes a variety of metabolites, including SCFAs, formate, and tryptophan-derive indoles, which promote immune tolerance and metastasis through activation of the AhR pathway. Furthermore, the release of TNF-⍺ and IL-6 in response to LPS in tumor-associated macrophages and dendritic cells (antigen-presenting cells; APCs) upregulates IDO activity in the resident APCs and tumor cells, leading to local overproduction of Kyn from tryptophan, which activates AhR to further promote immune tolerance. Created with BioRender.com
Kynurenine (Kyn)
One of the proposed theories regarding how the gut microbiome activates AhR to promote carcinogenesis is through the upregulation of the Kyn pathway. The Kyn pathway is a metabolic pathway that produces nicotinamide adenine dinucleotide (NAD) and is responsible for approximately 95% of total tryptophan catabolism [136, 137]. Kyn is synthesized mainly in the liver and brain by the enzyme tryptophan 2,3-dioxygenase (TDO) and by indoleamine 2,3-dioxygenase (IDO) in many tissues in inflammatory stimuli. TDO and IDO are overexpressed by tumor cells as have immune and neuroactive functions, in addition to the production of NAD+ and ATP in host cells [136, 137]. It has been reported that tumor-associated macrophages and dendritic cells (DCs) express high levels of IDO1, leading to local depletion of tryptophan and Kyn overproduction. Kyn is a weak AhR agonist and at high concentrations constitutively activates AhR to boost regulatory T-cell activity, leading to suppressing the activities of T helper cells (Th1, Th2), NK, and DCs. Such effects promote self-tolerance, immune evasion, and subsequently tumor survival [120, 136,137,138,139]. An in vivo study has demonstrated that administration of LPS upregulated TDO2 and IDO in mice, which was associated with increased serum Kyn and AhR activation [140], suggesting that carcinogenic microbes could activate AhR through a similar mechanism. Furthermore, infection of THP-1-derived macrophages with live/heat-killed Fn induced IDO expression in a time- and dose-dependent manner through LPS-mediated induction of the tumor necrosis factor (TNF-α) and IL-6, which are both IDO inducers [141].
Bacterial indoles
The bacterial indole pathway in tryptophan catabolism may also play a role in activating AhR to induce cancer. This is evidenced by the observations that in pancreatic ductal adenocarcinoma patients, activation of AhR was found to positively correlate with the enrichment of indole-producing bacteria, while negatively correlates with overall survival [142]. Mechanistically, activation of the AhR in tumor-associated macrophages by tryptophan-derived bacterial indoles alters the cells polarization toward a protumor alternative antiinflammatory M2 phenotype and suppresses antitumor immunity. In this context, it has been shown that removal of dietary tryptophan, which cause AhR inhibition, and administration of ampicillin, an antibiotic that eradicates indole-producing Lactobacilli, all restored cytotoxic IFNγ + TNF⍺ + CD8 + T-cell function, increased tumor-associated macrophages expression of PD-L1 and MHC class II molecules, and reduced the expression of Cyp1a1, Cyp1b1, and Cyp1a2 genes [142]. This reduced tumor growth and improved the efficacy of immune checkpoint blockade by PD-L1 inhibition. Importantly, knockdown of AhR in mice eliminated the effect of ampicillin on tumor growth, suggesting an AhR-mediated pathway [142]. Nevertheless, given the wide variety and bioactivity of indole compounds produced by different bacterial species, further studies are required to identify which specific indoles are produced by cancer-associated bacteria and could contribute to carcinogenesis.
Short-chain fatty acids (SCFA)
Short-chain fatty acids (SCFAs), such as butyrate, acetate, and propionate, are produced from dietary fiber fermentation by microbiota and act as histone deacetylase (HDAC) inhibitors. HDAC inhibition increases the recruitment of AhR to its target gene CYP1A1’ promoter through the reshaping of chromatin and enhancing the expression of AhR-responsive genes CYP1A1, CYP1B1, AhR repressor in Caco-2 CRC cells and YAMC mouse colonic epithelial cells [143, 144]. Interestingly, in addition to enhancing the basal expression of AhR and its downstream genes, butyrate also synergistically enhanced TCDD-induced AhR activation [143], further highlighting the potential role of crosstalk between the gut microbiome and environmental toxins in carcinogenesis. Butyrate also enhanced AhR activation by microbiota-derived tryptophan metabolites, including indoles. Hence, rather than directly acting as AhR ligands, SCFAs synergize with bacterial-derived AhR agonists to facilitate the binding of the activated AhR complex to its target genes [143].
Formate
Formate is a bacterial fermentation product that is known to play a role in cancer, but its role in the crosstalk between gut microbiome and AhR is still unexplored. Coculture with T18 CRC cells increases the Fn secretion of fermentation products, such as acetate, propionate, butyrate, and formate four-fold, with formate being the predominant fermentation product across different Fn strains [133]. Interestingly, AhR was the most significantly activated pathway following formate treatment. Incubation with Fn and formate-induced AhR nuclear translocation increased the invasion and migration of CRC cells, upregulated cancer stemness markers (ALDH1A1, CD44, OCT4, SOX2, CD133, and CD24), enhanced metastatic dissemination, and induced Wnt signaling. These effects were all reversed by AhR pharmacological inhibition by CH223191 [133]. However, the exact mechanisms through which formate activates AhR were not investigated, and further studies are required.
Paradoxical modulation of AhR by microbiome and its effect on cancer (MR)
In the absence of cancer, AhR activation by the healthy gut microbiome has an important regulatory role in maintaining intestinal homeostasis and gut barrier integrity [145]. Patients with celiac disease have reduced levels of endogenous AhR ligands and consequently less intestinal AhR activity [146], and AhR knockout mice were found to be more susceptible to dextran sulfate sodium -induced colitis. Conversely, supplementation with β-napthoflavone, an AhR agonist, accelerated recovery from colitis [147]. These protective effects may be due to the AhR-mediated release of IL-10 and IL-22, which promote mucosal healing and inflammation resolution in inflammatory bowel disease [148,149,150].
The consequences of AhR activation hence appear to be ligand-specific, as while some AhR ligands that possess short half-lives and bind to AhR only transiently have been reported to be protective against colitis, other ligands have been reported to induce a proinflammatory response. The toxicities observed with carcinogens such as TCDD may hence be attributed to the persistent and potent occupation of the AhR [137] or to targeting different binding sites on the receptor [151, 152].
Conclusions and remarks
In the last decade, valuable insights have been poured into identifying the role and involvement of the gut microbiome in modulating human physiology and disease. Due to the increased occurrence and higher mortality rate of cancer, the crosstalk between gut microbiota and cancer incidence has been well studied. Though reports have successfully proven their role in promoting tumorigenesis via altering the physiology and microenvironment and favoring tumorigenic environment, cancer development, progression, and altering treatment responsiveness, the role of other factors remains unexplored. As a significant pathway mediating gut homeostasis and as a sensor for several microbial metabolites, AhR could have a role in microbe-mediated tumorigenesis. Although studies are limited in this context, this could be a better endpoint for cancer maintenance and therapy. More studies identifying and testing the level of microbial metabolites activating AhR and their potential involvement in mediating cancer would shed new insights into managing cancer in a targeted therapy scenario. Furthermore, since most studies have focused on Fn, further research is required on the possible crosstalk between AhR and other bacterial species implicated in CRC, such as Sg, ETBF, Escherichia coli B2, Enterococcus faecalis, and Peptostreptococcus anaerobius. Additionally, the role of the microbiome in promoting immune responses and responsiveness to immunotherapy and the relevance of possible future investigations in light of the role of AhR need further investigation.
In this review, we attempted to highlight recent developments that point to a possible crosstalk between the AhR pathway and the microbiome in cancer initiation, promotion, and progression. Furthermore, revealing the mechanisms governing this crosstalk will provide future insights into disease understanding and pave the way for the revolutionization of targeted pharmaceuticals and therapeutics.
Availability of data and materials
Not applicable.
Abbreviations
- Apc:
-
Adenomatous polyposis coli
- AhR:
-
Aryl hydrocarbon receptor
- BaP:
-
Benzo[a]pyrene
- BFT:
-
Fragilis toxin
- CRC:
-
Colorectal cancer
- CSCs:
-
Cancer stem cells
- CYP:
-
Cytochrome P450 proteins
- CYP1A1:
-
Cytochrome P450 1A1
- CYP1B1:
-
Cytochrome P450 1B1
- CYP2J2:
-
Cytochrome P450 2J2
- DRE:
-
Dioxin-responsive elements
- EMT:
-
Epithelial–mesenchymal transition
- ETBF:
-
Enterotoxigenic Bacteroides fragilis
- Fn:
-
Fusobacterium nucleatum
- HDAC:
-
Histone deacetylase
- Kyn:
-
Kynurenine
- LPS:
-
Lipopolysaccharide
- NRF2:
-
Nuclear factor erythroid 2-related factor 2
- NF-κB:
-
Nuclear factor κB
- PDAC:
-
Pancreatic ductal adenocarcinoma
- Sg:
-
Streptococcus gallolyticus
- Stat3:
-
Signal transducer and activator of transcription-3
- TCDD:
-
2,3,7,8-tetrachlorodibenzo-p-dioxin
- TDO:
-
Tryptophan 2,3-dioxygenase
- TIGIT:
-
T cell immunoglobulin, and ITIM domain
- TLR4:
-
Toll-like receptor 4
References
Akbar N, Khan NA, Muhammad JS, Siddiqui R. The role of gut microbiome in cancer genesis and cancer prevention. Health Sci Rev. 2022;2: 100010.
Rahman MM, Islam MR, Shohag S, Ahasan MT, Sarkar N, Khan H, Hasan AM, Cavalu S, Rauf A. Microbiome in cancer: role in carcinogenesis and impact in therapeutic strategies. Biomed Pharmacother. 2022;149: 112898.
Bagheri Z, Moeinzadeh L, Razmkhah M. Roles of microbiota in cancer: from tumor development to treatment. J Oncol. 2022;2022: e3845104.
Sadrekarimi H, Gardanova ZR, Bakhshesh M, Ebrahimzadeh F, Yaseri AF, Thangavelu L, Hasanpoor Z, Zadeh FA, Kahrizi MS. Emerging role of human microbiome in cancer development and response to therapy: special focus on intestinal microflora. J Transl Med. 2022;20(1):301.
Gupta I, Pedersen S, Vranic S, Al Moustafa A-E. Implications of gut microbiota in epithelial-mesenchymal transition and cancer progression: a concise review. Cancers. 2022;14(12):2964.
Chen Y, Wu F-H, Wu P-Q, Xing H-Y, Ma T. The role of the tumor microbiome in tumor development and its treatment. Front Immunol. 2022; 13.
Meng C, Bai C, Brown TD, Hood LE, Tian Q. Human gut microbiota and gastrointestinal cancer. Genomics Proteomics Bioinformatics. 2018;16(1):33–49.
Lee KA, Luong MK, Shaw H, Nathan P, Bataille V, Spector TD. The gut microbiome: what the oncologist ought to know. Br J Cancer. 2021;125(9):1197–209.
Zitvogel L, Daillère R, Roberti MP, Routy B, Kroemer G. Anticancer effects of the microbiome and its products. Nat Rev Microbiol. 2017;15(8):465–78.
Chung WSF, Walker AW, Louis P, Parkhill J, Vermeiren J, Bosscher D, Duncan SH, Flint HJ. Modulation of the human gut microbiota by dietary fibres occurs at the species level. BMC Biol. 2016;14(1):3.
Vaishnava S, Behrendt CL, Ismail AS, Eckmann L, Hooper LV. Paneth cells directly sense gut commensals and maintain homeostasis at the intestinal host-microbial interface. Proc Natl Acad Sci. 2008;105(52):20858–63.
Peterson LW, Artis D. Intestinal epithelial cells: regulators of barrier function and immune homeostasis. Nat Rev Immunol. 2014;14(3):141–53.
Abu-Ghazaleh N, Chua WJ, Gopalan V. Intestinal microbiota and its association with colon cancer and red/processed meat consumption. J Gastroenterol Hepatol. 2021;36(1):75–88.
Pandey H, Tang DWT, Wong SH, Lal D. Gut microbiota in colorectal cancer: biological role and therapeutic opportunities. Cancers (Basel). 2023;15(3):866.
Virtue AT, McCright SJ, Wright JM, Jimenez MT, Mowel WK, Kotzin JJ, Joannas L, Basavappa MG, Spencer SP, Clark ML, et al. The gut microbiota regulates white adipose tissue inflammation and obesity via a family of microRNAs. Sci Transl Med. 2019;11(496):eaav1892.
Foley KP, Zlitni S, Denou E, Duggan BM, Chan RW, Stearns JC, Schertzer JD. Long term but not short term exposure to obesity related microbiota promotes host insulin resistance. Nat Commun. 2018;9(1):4681.
Sun L, Ma L, Ma Y, Zhang F, Zhao C, Nie Y. Insights into the role of gut microbiota in obesity: pathogenesis, mechanisms, and therapeutic perspectives. Protein Cell. 2018;9(5):397–403.
Brown K, Godovannyi A, Ma C, Zhang Y, Ahmadi-Vand Z, Dai C, Gorzelak MA, Chan Y, Chan JM, Lochner A, et al. Prolonged antibiotic treatment induces a diabetogenic intestinal microbiome that accelerates diabetes in NOD mice. ISME J. 2016;10(2):321–32.
Livanos AE, Greiner TU, Vangay P, Pathmasiri W, Stewart D, McRitchie S, Li H, Chung J, Sohn J, Kim S, et al. Antibiotic-mediated gut microbiome perturbation accelerates development of type 1 diabetes in mice. Nat Microbiol. 2016;1(11):1–13.
Koh A, Molinaro A, Ståhlman M, Khan MT, Schmidt C, Mannerås-Holm L, Wu H, Carreras A, Jeong H, Olofsson LE, et al. Microbially produced imidazole propionate impairs insulin signaling through mTORC1. Cell. 2018;175(4):947-961.e917.
Czesnikiewicz-Guzik M, Müller DN. Scientists on the Spot: salt, the microbiome, and cardiovascular diseases. Cardiovasc Res. 2018;114(10):e72–3.
Erny D, Hrabě de Angelis AL, Jaitin D, Wieghofer P, Staszewski O, David E, Keren-Shaul H, Mahlakoiv T, Jakobshagen K, Buch T, et al. Host microbiota constantly control maturation and function of microglia in the CNS. Nat Neurosci. 2015;18(7):965–77.
Jangi S, Gandhi R, Cox LM, Li N, von Glehn F, Yan R, Patel B, Mazzola MA, Liu S, Glanz BL, et al. Alterations of the human gut microbiome in multiple sclerosis. Nat Commun. 2016;7(1):12015.
Maini Rekdal V, Bess EN, Bisanz JE, Turnbaugh PJ, Balskus EP. Discovery and inhibition of an interspecies gut bacterial pathway for Levodopa metabolism. Science (New York, NY). 2019;364(6445):eaau6323.
Kelly JR, Kennedy PJ, Cryan JF, Dinan TG, Clarke G, Hyland NP. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392.
Cheng WY, Wu C-Y, Yu J. The role of gut microbiota in cancer treatment: friend or foe? Gut. 2020;69(10):1867–76.
De Luca F, Shoenfeld Y. The microbiome in autoimmune diseases. Clin Exp Immunol. 2019;195(1):74–85.
Jiao Y, Wu L, Huntington ND, Zhang X. Crosstalk between gut microbiota and innate immunity and its implication in autoimmune diseases. Front Immunol. 2020; 11.
Kim S, Covington A, Pamer EG. The intestinal microbiota: antibiotics, colonization resistance, and enteric pathogens. Immunol Rev. 2017;279(1):90–105.
Arumugam M, Raes J, Pelletier E, Le Paslier D, Yamada T, Mende DR, Fernandes GR, Tap J, Bruls T, Batto J-M, et al. Enterotypes of the human gut microbiome. Nature. 2011;473(7346):174–80.
Dominguez-Bello MG, Blaser MJ, Ley RE, Knight R. Development of the human gastrointestinal microbiota and insights from high-throughput sequencing. Gastroenterology. 2011;140(6):1713–9.
Lee SM, Donaldson GP, Mikulski Z, Boyajian S, Ley K, Mazmanian SK. Bacterial colonization factors control specificity and stability of the gut microbiota. Nature. 2013;501(7467):426–9.
Goodrich JK, Waters JL, Poole AC, Sutter JL, Koren O, Blekhman R, Beaumont M, Van Treuren W, Knight R, Bell JT, et al. Human genetics shape the gut microbiome. Cell. 2014;159(4):789–99.
Sommer F, Anderson JM, Bharti R, Raes J, Rosenstiel P. The resilience of the intestinal microbiota influences health and disease. Nat Rev Microbiol. 2017;15(10):630–8.
Blaser MJ. The microbiome revolution. J Clin Invest. 2014;124(10):4162–5.
Iqbal S, Quigley EM. Progress in our understanding of the gut microbiome: implications for the clinician. Curr Gastroenterol Rep. 2016;18(9):49.
O’Toole PW, Flemer B. From culture to high-throughput sequencing and beyond: a Layperson’s guide to the “omics” and diagnostic potential of the microbiome. Gastroenterol Clin North Am. 2017;46(1):9–17.
Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI. The human microbiome project. Nature. 2007;449(7164):804–10.
Cryan JF, Dinan TG. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci. 2012;13(10):701–12.
Nicolaro M, Portal DE, Shinder B, Patel HV, Singer EA. The human microbiome and genitourinary malignancies. Ann Transl Med. 2020;8(19):1245.
Miyake M, Tatsumi Y, Ohnishi K, Fujii T, Nakai Y, Tanaka N, Fujimoto K. Prostate diseases and microbiome in the prostate, gut, and urine. Prostate Int. 2022;10(2):96–107.
Devaraj S, Hemarajata P, Versalovic J. The human gut microbiome and body metabolism: implications for obesity and diabetes. Clin Chem. 2013;59(4):617–28.
Parashar A, Udayabanu M. Gut microbiota: implications in Parkinson’s disease. Parkinsonism Relat Disord. 2017;38:1–7.
Vuong HE, Hsiao EY. Emerging roles for the gut microbiome in autism spectrum disorder. Biol Psychiatry. 2017;81(5):411–23.
Purcell RV, Visnovska M, Biggs PJ, Schmeier S, Frizelle FA. Distinct gut microbiome patterns associate with consensus molecular subtypes of colorectal cancer. Sci Rep. 2017;7(1):11590.
Pleguezuelos-Manzano C, Puschhof J, Clevers H. Gut microbiota in colorectal cancer: associations, mechanisms, and clinical approaches. Annu Rev Cancer Biol. 2022;6(1):65–84.
Murata-Kamiya N, Kurashima Y, Teishikata Y, Yamahashi Y, Saito Y, Higashi H, Aburatani H, Akiyama T, Peek RM, Azuma T, et al. Helicobacter pylori CagA interacts with E-cadherin and deregulates the β-catenin signal that promotes intestinal transdifferentiation in gastric epithelial cells. Oncogene. 2007;26(32):4617–26.
Nasrollahzadeh D, Malekzadeh R, Ploner A, Shakeri R, Sotoudeh M, Fahimi S, Nasseri-Moghaddam S, Kamangar F, Abnet CC, Winckler B, et al. Variations of gastric corpus microbiota are associated with early esophageal squamous cell carcinoma and squamous dysplasia. Sci Rep. 2015;5(1):8820.
Yang L, Lu X, Nossa CW, Francois F, Peek RM, Pei Z. Inflammation and intestinal metaplasia of the distal esophagus are associated with alterations in the microbiome. Gastroenterology. 2009;137(2):588–97.
Yoshimoto S, Loo TM, Atarashi K, Kanda H, Sato S, Oyadomari S, Iwakura Y, Oshima K, Morita H, Hattori M, et al. Obesity-induced gut microbial metabolite promotes liver cancer through senescence secretome. Nature. 2013;499(7456):97–101.
Ma C, Han M, Heinrich B, Fu Q, Zhang Q, Sandhu M, Agdashian D, Terabe M, Berzofsky JA, Fako V, et al. Gut microbiome-mediated bile acid metabolism regulates liver cancer via NKT cells. Science (New York, NY). 2018;360(6391):eaan5931.
Pushalkar S, Hundeyin M, Daley D, Zambirinis CP, Kurz E, Mishra A, Mohan N, Aykut B, Usyk M, Torres LE, et al. The pancreatic cancer microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer Discov. 2018;8(4):403–16.
Riquelme E, Zhang Y, Zhang L, Montiel M, Zoltan M, Dong W, Quesada P, Sahin I, Chandra V, Lucas AS, et al. Tumor microbiome diversity and composition influence pancreatic cancer outcomes. Cell. 2019;178(4):795-806.e712.
Ruo SW, Alkayyali T, Win M, Tara A, Joseph C, Kannan A, Srivastava K, Ochuba O, Sandhu JK, Went TR, et al. Role of gut microbiota dysbiosis in breast cancer and novel approaches in prevention, diagnosis, and treatment. Cureus. 2021;13(8): e17472.
Li Y, Jiang H, Wang X, Liu X, Huang Y, Wang Z, Ma Q, Dong L, Qi Y, Zhang H, et al. Crosstalk between the gut and brain: importance of the fecal microbiota in patient with brain tumors. Front Cell Infect Microbiol. 2022;12: 881071.
Pevsner-Fischer M, Tuganbaev T, Meijer M, Zhang S-H, Zeng Z-R, Chen M-H, Elinav E. Role of the microbiome in non-gastrointestinal cancers. World J Clin Oncol. 2016;7(2):200–13.
Villemin C, Six A, Neville BA, Lawley TD, Robinson MJ, Bakdash G. The heightened importance of the microbiome in cancer immunotherapy. Trends Immunol. 2023;44(1):44–59.
Johansson MEV, Hansson GC. Immunological aspects of intestinal mucus and mucins. Nat Rev Immunol. 2016;16(10):639–49.
McCoy KD, Geuking MB. Microbiota regulates intratumoral monocytes to promote anti-tumor immune responses. Cell. 2021;184(21):5301–3.
Sokol H, Pigneur B, Watterlot L, Lakhdari O, Bermúdez-Humarán LG, Gratadoux J-J, Blugeon S, Bridonneau C, Furet J-P, Corthier G, et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc Natl Acad Sci USA. 2008;105(43):16731–6.
Rosshart SP, Vassallo BG, Angeletti D, Hutchinson DS, Morgan AP, Takeda K, Hickman HD, McCulloch JA, Badger JH, Ajami NJ, et al. Wild mouse gut microbiota promotes host fitness and improves disease resistance. Cell. 2017;171(5):1015-1028.e1013.
Dzutsev A, Badger JH, Perez-Chanona E, Roy S, Salcedo R, Smith CK, Trinchieri G. Microbes and cancer. Annu Rev Immunol. 2017;35:199–228.
Fernandes MR, Aggarwal P, Costa RGF, Cole AM, Trinchieri G. Targeting the gut microbiota for cancer therapy. Nat Rev Cancer. 2022;22(12):703–22.
Abreu MT, Peek RM. Gastrointestinal malignancy and the microbiome. Gastroenterology. 2014;146(6):1534-1546.e1533.
Odenbreit S, Püls J, Sedlmaier B, Gerland E, Fischer W, Haas R. Translocation of Helicobacter pylori CagA into gastric epithelial cells by type IV secretion. Science (New York, NY). 2000;287(5457):1497–500.
Kim SS, Ruiz VE, Carroll JD, Moss SF. Helicobacter pylori in the pathogenesis of gastric cancer and gastric lymphoma. Cancer Lett. 2011;305(2):228–38.
Hatakeyama M. Malignant Helicobacter pylori-associated diseases: gastric cancer and MALT lymphoma. In: Kamiya S, Backert S, editors. Helicobacter pylori in human diseases: advances in microbiology, infectious diseases and public health, vol. 11. Cham: Springer International Publishing; 2019. p. 135–49.
Polk DB, Peek RM. Helicobacter pylori: gastric cancer and beyond. Nat Rev Cancer. 2010;10(6):403–14.
Doorakkers E, Lagergren J, Engstrand L, Brusselaers N. Eradication of Helicobacter pylori and gastric cancer: a systematic review and meta-analysis of cohort studies. JNCI J Natl Cancer Inst. 2016;108(9):djw132.
Shen J, Xiao Z, Wu WKK, Wang MH, To KF, Chen Y, Yang W, Li MSM, Shin VY, Tong JH, et al. Epigenetic silencing of miR-490-3p reactivates the chromatin remodeler SMARCD1 to promote Helicobacter pylori-induced gastric carcinogenesis. Can Res. 2015;75(4):754–65.
Yin H, Zhang J, Zhang H, Li Q, Qiu H, Hong K, Wang W, Xiao Y, Yu B. Fusobacterium nucleatum promotes proliferation in oesophageal squamous cell carcinoma via AHR/CYP1A1 signalling. FEBS J. 2023;290(3):837–54.
Poore GD, Kopylova E, Zhu Q, Carpenter C, Fraraccio S, Wandro S, Kosciolek T, Janssen S, Metcalf J, Song SJ, et al. Microbiome analyses of blood and tissues suggest cancer diagnostic approach. Nature. 2020;579(7800):567–74.
Zhang Y-K, Zhang Q, Wang Y-L, Zhang W-Y, Hu H-Q, Wu H-Y, Sheng X-Z, Luo K-J, Zhang H, Wang M, et al. A comparison study of age and colorectal cancer-related gut bacteria. Front Cell Infect Microbiol. 2021;11: 606490.
Dai Z, Coker OO, Nakatsu G, Wu WKK, Zhao L, Chen Z, Chan FKL, Kristiansen K, Sung JJY, Wong SH, et al. Multi-cohort analysis of colorectal cancer metagenome identified altered bacteria across populations and universal bacterial markers. Microbiome. 2018;6(1):70.
Wirbel J, Pyl PT, Kartal E, Zych K, Kashani A, Milanese A, Fleck JS, Voigt AY, Palleja A, Ponnudurai R, et al. Meta-analysis of fecal metagenomes reveals global microbial signatures that are specific for colorectal cancer. Nat Med. 2019;25(4):679–89.
Silva M, Brunner V, Tschurtschenthaler M. Microbiota and colorectal cancer: from gut to bedside. Front Pharmacol. 2021;12: 760280.
Lu Y, Chen J, Zheng J, Hu G, Wang J, Huang C, Lou L, Wang X, Zeng Y. Mucosal adherent bacterial dysbiosis in patients with colorectal adenomas. Sci Rep. 2016;6:26337.
Fan X, Jin Y, Chen G, Ma X, Zhang L. Gut microbiota dysbiosis drives the development of colorectal cancer. Gastroenterologia. 2020;102(4):508–15.
Yachida S, Mizutani S, Shiroma H, Shiba S, Nakajima T, Sakamoto T, Watanabe H, Masuda K, Nishimoto Y, Kubo M, et al. Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat Med. 2019;25(6):968–76.
Nakatsu G, Li X, Zhou H, Sheng J, Wong SH, Wu WKK, Ng SC, Tsoi H, Dong Y, Zhang N, et al. Gut mucosal microbiome across stages of colorectal carcinogenesis. Nat Commun. 2015;6:8727.
Bullman S, Pedamallu CS, Sicinska E, Clancy TE, Zhang X, Cai D, Neuberg D, Huang K, Guevara F, Nelson T, et al. Analysis of Fusobacterium persistence and antibiotic response in colorectal cancer. Science (New York, NY). 2017;358(6369):1443–8.
Rubinstein MR, Baik JE, Lagana SM, Han RP, Raab WJ, Sahoo D, Dalerba P, Wang TC, Han YW. Fusobacterium nucleatum promotes colorectal cancer by inducing Wnt/β-catenin modulator Annexin A1. EMBO Rep. 2019; 20(4).
Brennan CA, Garrett WS. Fusobacterium nucleatum—symbiont, opportunist and oncobacterium. Nat Rev Microbiol. 2019;17(3):156–66.
Wong SH, Zhao L, Zhang X, Nakatsu G, Han J, Xu W, Xiao X, Kwong TNY, Tsoi H, Wu WKK, et al. Gavage of fecal samples from patients with colorectal cancer promotes intestinal carcinogenesis in germ-free and conventional mice. Gastroenterology. 2017;153(6):1621-1633.e1626.
Mangerich A, Knutson CG, Parry NM, Muthupalani S, Ye W, Prestwich E, Cui L, McFaline JL, Mobley M, Ge Z, et al. Infection-induced colitis in mice causes dynamic and tissue-specific changes in stress response and DNA damage leading to colon cancer. Proc Natl Acad Sci. 2012;109(27):E1820–9.
Rubinstein MR, Wang X, Liu W, Hao Y, Cai G, Han YW. Fusobacterium nucleatum promotes colorectal carcinogenesis by modulating E-cadherin/β-catenin signaling via its FadA adhesin. Cell Host Microbe. 2013;14(2):195–206.
Flanagan L, Schmid J, Ebert M, Soucek P, Kunicka T, Liska V, Bruha J, Neary P, Dezeeuw N, Tommasino M, et al. Fusobacterium nucleatum associates with stages of colorectal neoplasia development, colorectal cancer and disease outcome. Eur J Clin Microbiol Infect Dis. 2014;33(8):1381–90.
Salvucci M, Crawford N, Stott K, Bullman S, Longley D, Prehn J. Patients with mesenchymal tumours and high Fusobacteriales prevalence have worse prognosis in colorectal cancer (CRC). Gut. 2022;71(8):4307.
Roth U, Razawi H, Hommer J, Engelmann K, Schwientek T, Müller S, Baldus SE, Patsos G, Corfield AP, Paraskeva C, et al. Differential expression proteomics of human colorectal cancer based on a syngeneic cellular model for the progression of adenoma to carcinoma. Proteomics. 2010;10(2):194–202.
Abed J, Emgård JE, Zamir G, Faroja M, Almogy G, Grenov A, Sol A, Naor R, Pikarsky E, Atlan KA, et al. Fap2 mediates Fusobacterium nucleatum colorectal adenocarcinoma enrichment by binding to tumor-expressed gal-GalNAc. Cell Host Microbe. 2016;20(2):215–25.
Gur C, Ibrahim Y, Isaacson B, Yamin R, Abed J, Gamliel M, Enk J, Bar-On Y, Stanietsky-Kaynan N, Coppenhagen-Glazer S, et al. Binding of the Fap2 protein of Fusobacterium nucleatum to human inhibitory receptor TIGIT protects tumors from immune cell attack. Immunity. 2015;42(2):344–55.
To TT, Gümüş P, Nizam N, Buduneli N, Darveau RP. Subgingival plaque in periodontal health antagonizes at toll-like receptor 4 and inhibits E-selectin expression on endothelial cells. Infect Immun. 2016;84(1):120–6.
Yang Y, Weng W, Peng J, Hong L, Yang L, Toiyama Y, Gao R, Liu M, Yin M, Pan C, et al. Fusobacterium nucleatum increases proliferation of colorectal cancer cells and tumor development in mice by activating toll-like receptor 4 signaling to nuclear factor-κB, and up-regulating expression of MicroRNA-21. Gastroenterology. 2017;152(4):851-866.e824.
Molina JR, Adjei AA. The Ras/Raf/MAPK pathway. J Thorac Oncol. 2006;1(1):7–9.
Shi C, Yang Y, Xia Y, Okugawa Y, Yang J, Liang Y, Chen H, Zhang P, Wang F, Han H, et al. Novel evidence for an oncogenic role of microRNA-21 in colitis-associated colorectal cancer. Gut. 2016;65(9):1470–81.
Kong C, Yan X, Zhu Y, Zhu H, Luo Y, Liu P, Ferrandon S, Kalady MF, Gao R, He J, et al. Fusobacterium nucleatum promotes the development of colorectal cancer by activating a cytochrome P450/epoxyoctadecenoic acid axis via TLR4/Keap1/NRF2 signaling. Cancer Res. 2021;81(17):4485–98.
Yu T, Guo F, Yu Y, Sun T, Ma D, Han J, Qian Y, Kryczek I, Sun D, Nagarsheth N, et al. Fusobacterium nucleatum promotes chemoresistance to colorectal cancer by modulating autophagy. Cell. 2017;170(3):548-563.e516.
Liu Y, Baba Y, Ishimoto T, Tsutsuki H, Zhang T, Nomoto D, Okadome K, Yamamura K, Harada K, Eto K, et al. Fusobacterium nucleatum confers chemoresistance by modulating autophagy in oesophageal squamous cell carcinoma. Br J Cancer. 2021;124(5):963–74.
Bullman S, Pedamallu CS, Sicinska E, Clancy TE, Zhang X, Cai D, Neuberg D, Huang K, Guevara F, Nelson T, et al. Analysis of Fusobacterium persistence and antibiotic response in colorectal cancer. Science. 2017;358(6369):1443–8.
Liu H, Du J, Chao S, Li S, Cai H, Zhang H, Chen G, Liu P, Bu P. Fusobacterium nucleatum promotes colorectal cancer cell to acquire stem cell-like features by manipulating lipid droplet-mediated numb degradation. Adv Sci. 2022;9(12):2105222.
Kumar R, Herold JL, Schady D, Davis J, Kopetz S, Martinez-Moczygemba M, Murray BE, Han F, Li Y, Callaway E, et al. Streptococcus gallolyticus subsp. gallolyticus promotes colorectal tumor development. PLoS Pathog. 2017;13(7):e1006440.
Wu S, Rhee KJ, Albesiano E, Rabizadeh S, Wu X, Yen HR, Huso DL, Brancati FL, Wick E, McAllister F, et al. A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses. Nat Med. 2009;15(9):1016–22.
Kim JM, Jung HY, Lee JY, Youn J, Lee CH, Kim KH. Mitogen-activated protein kinase and activator protein-1 dependent signals are essential for Bacteroides fragilis enterotoxin-induced enteritis. Eur J Immunol. 2005;35(9):2648–57.
Wu S, Powell J, Mathioudakis N, Kane S, Fernandez E, Sears CL. Bacteroides fragilis enterotoxin induces intestinal epithelial cell secretion of interleukin-8 through mitogen-activated protein kinases and a tyrosine kinase-regulated nuclear factor-kappaB pathway. Infect Immun. 2004;72(10):5832–9.
Wu S, Lim KC, Huang J, Saidi RF, Sears CL. Bacteroides fragilis enterotoxin cleaves the zonula adherens protein, E-cadherin. Proc Natl Acad Sci U S A. 1998;95(25):14979–84.
Cuevas-Ramos G, Petit CR, Marcq I, Boury M, Oswald E, Nougayrède JP. Escherichia coli induces DNA damage in vivo and triggers genomic instability in mammalian cells. Proc Natl Acad Sci U S A. 2010;107(25):11537–42.
Buc E, Dubois D, Sauvanet P, Raisch J, Delmas J, Darfeuille-Michaud A, Pezet D, Bonnet R. High prevalence of mucosa-associated E. coli producing cyclomodulin and genotoxin in colon cancer. PLoS ONE. 2013;8(2):e56964.
Wang X, Yang Y, Moore DR, Nimmo SL, Lightfoot SA, Huycke MM. 4-hydroxy-2-nonenal mediates genotoxicity and bystander effects caused by Enterococcus faecalis-infected macrophages. Gastroenterology. 2012;142(3):543-551.e547.
Huycke MM, Moore DR. In vivo production of hydroxyl radical by Enterococcus faecalis colonizing the intestinal tract using aromatic hydroxylation. Free Radic Biol Med. 2002;33(6):818–26.
Tsoi H, Chu ESH, Zhang X, Sheng J, Nakatsu G, Ng SC, Chan AWH, Chan FKL, Sung JJY, Yu J. Peptostreptococcus anaerobius induces intracellular cholesterol biosynthesis in colon cells to induce proliferation and causes dysplasia in mice. Gastroenterology. 2017;152(6):1419-1433.e1415.
Long X, Wong CC, Tong L, Chu ESH, Ho Szeto C, Go MYY, Coker OO, Chan AWH, Chan FKL, Sung JJY, et al. Peptostreptococcus anaerobius promotes colorectal carcinogenesis and modulates tumour immunity. Nat Microbiol. 2019;4(12):2319–30.
Liu L, Tabung FK, Zhang X, Nowak JA, Qian ZR, Hamada T, Nevo D, Bullman S, Mima K, Kosumi K, et al. Diets that promote colon inflammation associate with risk of colorectal carcinomas that contain Fusobacterium nucleatum. Clin Gastroenterol Hepatol. 2018;16(10):1622-1631.e1623.
Williams MR, Stedtfeld RD, Stedtfeld TM, Crawford RB, Kuwahara T, Kaminski NE, Tiedje JM, Hashsham SA. MicroRNA-based host response to toxicant exposure is influenced by the presence of gut microbial populations. Sci Total Environ. 2021;797: 149130.
Pelclová D, Urban P, Preiss J, Lukás E, Fenclová Z, Navrátil T, Dubská Z, Senholdová Z. Adverse health effects in humans exposed to 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD). Rev Environ Health. 2006;21(2):119–38.
Diakité MT, Diakité B, Koné A, Balam S, Fofana D, Diallo D, Kassogué Y, Traoré CB, Kamaté B, Ba D et al. Relationships between gut microbiota, red meat consumption and colorectal cancer. J Carcinog Mutagen. 2022; 13(3).
Cheng T, Chaousis S, Madhurika S, Kodagoda G, Lam A, Gopalan V. Polycyclic aromatic hydrocarbons detected in processed meats cause genetic changes in colorectal cancers. Int J Mol Sci. 2021;22(20):10959.
Defois C, Ratel J, Garrait G, Denis S, Le Goff O, Talvas J, Mosoni P, Engel E, Peyret P. Food chemicals disrupt human gut microbiota activity and impact intestinal homeostasis as revealed by in vitro systems. Sci Rep. 2018;8(1):11006.
Bohonowych JE, Denison MS. Persistent binding of ligands to the aryl hydrocarbon receptor. Toxicol Sci. 2007;98(1):99–109.
Kolluri SK, Jin UH, Safe S. Role of the aryl hydrocarbon receptor in carcinogenesis and potential as an anti-cancer drug target. Arch Toxicol. 2017;91(7):2497–513.
Murray IA, Patterson AD, Perdew GH. Aryl hydrocarbon receptor ligands in cancer: friend and foe. Nat Rev Cancer. 2014;14(12):801–14.
Hord NG, Perdew GH. Physicochemical and immunocytochemical analysis of the aryl hydrocarbon receptor nuclear translocator: characterization of two monoclonal antibodies to the aryl hydrocarbon receptor nuclear translocator. Mol Pharmacol. 1994;46(4):618–26.
Perdew GH. Association of the Ah receptor with the 90-kDa heat shock protein. J Biol Chem. 1988;263(27):13802–5.
Nair SC, Toran EJ, Rimerman RA, Hjermstad S, Smithgall TE, Smith DF. A pathway of multi-chaperone interactions common to diverse regulatory proteins: estrogen receptor, Fes tyrosine kinase, heat shock transcription factor Hsf1, and the aryl hydrocarbon receptor. Cell Stress Chaperones. 1996;1(4):237–50.
Sayed TS, Maayah ZH, Zeidan HA, Agouni A, Korashy HM. Insight into the physiological and pathological roles of the aryl hydrocarbon receptor pathway in glucose homeostasis, insulin resistance, and diabetes development. Cell Mol Biol Lett. 2022;27(1):103.
Yamashita N, Saito N, Zhao S, Terai K, Hiruta N, Park Y, Bujo H, Nemoto K, Kanno Y. Heregulin-induced cell migration is promoted by aryl hydrocarbon receptor in HER2-overexpressing breast cancer cells. Exp Cell Res. 2018;366(1):34–40.
Al-Dhfyan A, Alaiya A, Al-Mohanna F, Attwa MW, AlAsmari AF, Bakheet SA, Korashy HM. Crosstalk between aryl hydrocarbon receptor (AhR) and BCL-2 pathways suggests the use of AhR antagonist to maintain normal differentiation state of mammary epithelial cells during BCL-2 inhibition therapy. J Adv Res. 2022;50:177.
Al-Dhfyan A, Alhoshani A, Korashy HM. Aryl hydrocarbon receptor/cytochrome P450 1A1 pathway mediates breast cancer stem cells expansion through PTEN inhibition and beta-Catenin and Akt activation. Mol Cancer. 2017;16(1):14.
Williams TD, Lee JS, Sheader DL, Chipman JK. The cytochrome P450 1A gene (CYP1A) from European flounder (Platichthys flesus), analysis of regulatory regions and development of a dual luciferase reporter gene system. Mar Environ Res. 2000;50(1–5):1–6.
Buters JT, Sakai S, Richter T, Pineau T, Alexander DL, Savas U, Doehmer J, Ward JM, Jefcoate CR, Gonzalez FJ. Cytochrome P450 CYP1B1 determines susceptibility to 7, 12-dimethylbenz[a]anthracene-induced lymphomas. Proc Natl Acad Sci U S A. 1999;96(5):1977–82.
Therachiyil L, Krishnankutty R, Ahmad F, Mateo JM, Uddin S, Korashy HM. Aryl hydrocarbon receptor promotes cell growth, stemness like characteristics, and metastasis in human ovarian cancer via activation of PI3K/Akt, beta-catenin, and epithelial to mesenchymal transition pathways. Int J Mol Sci. 2022;23(12):6395.
Jung JW, Park SB, Lee SJ, Seo MS, Trosko JE, Kang KS. Metformin represses self-renewal of the human breast carcinoma stem cells via inhibition of estrogen receptor-mediated OCT4 expression. PLoS ONE. 2011;6(11): e28068.
Al-Dhfyan A, Alhoshani A, Korashy HM. Aryl hydrocarbon receptor/cytochrome P450 1A1 pathway mediates breast cancer stem cells expansion through PTEN inhibition and β-Catenin and Akt activation. Mol Cancer. 2017;16(1):14.
Ternes D, Tsenkova M, Pozdeev VI, Meyers M, Koncina E, Atatri S, Schmitz M, Karta J, Schmoetten M, Heinken A, et al. The gut microbial metabolite formate exacerbates colorectal cancer progression. Nat Metab. 2022;4(4):458–75.
Taddese R, Roelofs R, Draper D, Wu X, Wu S, Swinkels DW, Tjalsma H, Boleij A. Streptococcus gallolyticus increases expression and activity of aryl hydrocarbon receptor-dependent CYP1 biotransformation capacity in colorectal epithelial cells. Front Cell Infect Microbiol. 2021;11: 740704.
Dong F, Perdew GH. The aryl hydrocarbon receptor as a mediator of host-microbiota interplay. Gut Microbes. 2020;12(1):1859812.
Wyatt M, Greathouse KL. Targeting dietary and microbial tryptophan-indole metabolism as therapeutic approaches to colon cancer. Nutrients. 2021;13(4):1189.
Han H, Safe S, Jayaraman A, Chapkin RS. Diet-host-microbiota interactions shape aryl hydrocarbon receptor ligand production to modulate intestinal homeostasis. Annu Rev Nutr. 2021;41:455–78.
Pilotte L, Larrieu P, Stroobant V, Colau D, Dolusic E, Frédérick R, De Plaen E, Uyttenhove C, Wouters J, Masereel B, et al. Reversal of tumoral immune resistance by inhibition of tryptophan 2,3-dioxygenase. Proc Natl Acad Sci U S A. 2012;109(7):2497–502.
Stone TW, Stoy N, Darlington LG. An expanding range of targets for kynurenine metabolites of tryptophan. Trends Pharmacol Sci. 2013;34(2):136–43.
Bessede A, Gargaro M, Pallotta MT, Matino D, Servillo G, Brunacci C, Bicciato S, Mazza EM, Macchiarulo A, Vacca C, et al. Aryl hydrocarbon receptor control of a disease tolerance defence pathway. Nature. 2014;511(7508):184–90.
Xue Y, Xiao H, Guo S, Xu B, Liao Y, Wu Y, Zhang G. Indoleamine 2,3-dioxygenase expression regulates the survival and proliferation of Fusobacterium nucleatum in THP-1-derived macrophages. Cell Death Dis. 2018;9(3):355.
Hezaveh K, Shinde RS, Klötgen A, Halaby MJ, Lamorte S, Ciudad MT, Quevedo R, Neufeld L, Liu ZQ, Jin R, et al. Tryptophan-derived microbial metabolites activate the aryl hydrocarbon receptor in tumor-associated macrophages to suppress anti-tumor immunity. Immunity. 2022;55(2):324-340.e328.
Jin UH, Cheng Y, Park H, Davidson LA, Callaway ES, Chapkin RS, Jayaraman A, Asante A, Allred C, Weaver EA, et al. Short chain fatty acids enhance aryl hydrocarbon (Ah) responsiveness in mouse colonocytes and caco-2 human colon cancer cells. Sci Rep. 2017;7(1):10163.
Modoux M, Rolhion N, Lefevre JH, Oeuvray C, Nádvorník P, Illes P, Emond P, Parc Y, Mani S, Dvorak Z, et al. Butyrate acts through HDAC inhibition to enhance aryl hydrocarbon receptor activation by gut microbiota-derived ligands. Gut Microbes. 2022;14(1):2105637.
Lamas B, Richard ML, Leducq V, Pham H-P, Michel M-L, Da Costa G, Bridonneau C, Jegou S, Hoffmann TW, Natividad JM, et al. CARD9 impacts colitis by altering gut microbiota metabolism of tryptophan into aryl hydrocarbon receptor ligands. Nat Med. 2016;22(6):598–605.
Lamas B, Hernandez-Galan L, Galipeau HJ, Constante M, Clarizio A, Jury J, Breyner NM, Caminero A, Rueda G, Hayes CL et al. Aryl hydrocarbon receptor ligand production by the gut microbiota is decreased in celiac disease leading to intestinal inflammation. Sci Transl Med. 2020; 12(566).
Furumatsu K, Nishiumi S, Kawano Y, Ooi M, Yoshie T, Shiomi Y, Kutsumi H, Ashida H, Fujii-Kuriyama Y, Azuma T, et al. A role of the aryl hydrocarbon receptor in attenuation of colitis. Dig Dis Sci. 2011;56(9):2532–44.
Mizoguchi A, Yano A, Himuro H, Ezaki Y, Sadanaga T, Mizoguchi E. Clinical importance of IL-22 cascade in IBD. J Gastroenterol. 2018;53(4):465–74.
Kawai S, Iijima H, Shinzaki S, Hiyama S, Yamaguchi T, Araki M, Iwatani S, Shiraishi E, Mukai A, Inoue T, et al. Indigo Naturalis ameliorates murine dextran sodium sulfate-induced colitis via aryl hydrocarbon receptor activation. J Gastroenterol. 2017;52(8):904–19.
Monteleone I, Rizzo A, Sarra M, Sica G, Sileri P, Biancone L, MacDonald TT, Pallone F, Monteleone G. Aryl hydrocarbon receptor-induced signals up-regulate IL-22 production and inhibit inflammation in the gastrointestinal tract. Gastroenterology. 2011;141(1):237-248.e231.
Smith S, McHale K, Creech K, Rickard D, Jayawickreme C, Wu D, Rastinejad F, Rubenstein D. 595 Differential ligand binding distinguishes therapeutic from pathologic Aryl Hydrocarbon Receptor (AhR) modulating agents: implications for inflammatory skin disease. J Investig Dermatol. 2020;140(7):S81.
Hwang J, Newton EM, Hsiao J, Shi VY. Aryl hydrocarbon receptor/nuclear factor E2-related factor 2 (AHR/NRF2) signalling: a novel therapeutic target for atopic dermatitis. Exp Dermatol. 2022;31(4):485–97.
Acknowledgements
This study was supported by Qatar University Internal grant numbers IRCC-2022-484 and QUCG-CPH-23/24-154 to H.M.K., Qatar University–Royal College of Surgeons of Ireland PhD dual degree scholarship to M.R., and Qatar Foundation Graduate Studies Research Assistantship number GSRA8-L-1-0506-21033 to O.J.H. Open Access funding provided by the Qatar National Library.
Funding
Open Access funding provided by the Qatar National Library. This study was supported by Qatar University Internal grant nos. IRCC-2022-484 and QUCG-CPH-23/24-154.
Author information
Authors and Affiliations
Contributions
M.R. carried out the writing—original draft, preparation, and editing; T.S.S., O.J.H., and L.T. carried out the writing—original draft preparation; Z.M.: writing—reviewing and editing; S.U., C.M., and J.H.M.P. carried out the supervision and writing—reviewing and editing. H.M.K. carried out the conceptualization and supervision, and writing—reviewing and Editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
There are no financial or other interests in this review that might be construed as a conflict of interest. All the authors are aware of and agree to the content of the review and their being listed as authors on the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rayan, M., Sayed, T.S., Hussein, O.J. et al. Unlocking the secrets: exploring the influence of the aryl hydrocarbon receptor and microbiome on cancer development. Cell Mol Biol Lett 29, 33 (2024). https://doi.org/10.1186/s11658-024-00538-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11658-024-00538-0