Abstract
Background
Lumbar fusion corrects spinal deformities and improves spinal complications. Hip osteoarthritis (OA) is strongly correlated with spinal mobility, and joint space narrowing of the hip after spinal fusion has gained attention. This study aimed to elucidate the effect of spinal fusion on hip joint space narrowing.
Materials and methods
We retrospectively examined 530 hips of 270 patients who underwent spinal surgery. All the patients underwent whole-spine radiography before and at the final follow-up. Patients were divided into three groups (N group: non-spinal fusion, S group: up to three interbody fusions, and L group: more than four interbody fusions). The rates of joint space narrowing, spinal parameters (sagittal vertical axis, thoracic kyphosis, lumbar lordosis, sacral slope, pelvic tilt, and pelvic incidence), and limb length discrepancy at the final follow-up were compared. A multilinear regression analysis was performed to identify the risk factors for the rate of joint space narrowing.
Results
The rate of joint space narrowing was significantly higher in the L group than in the N and S groups (P < 0.001). No significant difference in the rate of joint space narrowing was observed between the N and S groups. Multiple linear regression analysis revealed that the number of fusion levels (p < 0.05) and follow-up period (p < 0.001) were independent risk factors for joint space narrowing. Spinal parameters at the final follow-up were not independent risk factors.
Conclusions
Long spinal fusion (more than four levels) led to significantly greater joint space narrowing of the hip than short (up to three levels) or no fusion. Spinal alignment did not affect joint space narrowing of the hip. Surgeons should be aware that more than four interbody fusions may result in worse joint space narrowing of the hip.
Level of evidence
IV, retrospective study
Similar content being viewed by others
Introduction
Multiple factors have been found to be associated with hip osteoarthritis (OA) [1, 2]. The correlation between spinal alignment and hip OA has received attention since hip–spine syndrome [3] was first reported, the correlation between spinal alignment and hip OA has received attention. Spinal alignment and pelvic inclination changes with aging, and these changes directly affect the hip joint loading. Spinal inclination and tilting affect the load on the hip joints [4, 5]. In addition, a large pelvic tilt (PT) is observed in patients with rapidly destructive coxarthrosis [6, 7]. A large pelvic incidence (PI), sacral slope (SS), and PI minus lumbar lordosis (LL) are associated with hip OA [8]. However, some reports showed that PI was not associated with hip OA [9], and so this relationship remains inconclusive [10]. Therefore, the correlation between spinal alignment and hip OA remains unclear.
Spinal fusion has been performed to fix spinal instability and correct spinal malalignment.
Spinal surgery widely contributes to reducing pain, such as that from myelopathy and hernia, and improves activities of daily living. However, there is a possibility that spinal fusion also affects joint space narrowing of the hip. Some studies reported that long spinal fusion accelerates joint space narrowing of the hip and increases the risk of total hip arthroplasty (THA) [11, 12]. Long spinal fusion was performed to correct sagittal malalignment. Although spinal alignment is improved by spinal fusion, spinal fusion may increase the mechanical load on the adjacent joints. Adjacent segmental degeneration (ASD) after spinal fusion has been reported in 16.5% (5 years after spinal fusion) and 36.1% (10 years after spinal fusion) of patients [13]. Similarly, asymptomatic and symptomatic ASD were reported in 26.6% and 8.5% of patients, respectively [14]. Spinopelvic joints play a crucial role during sitting-to-standing and standing-to-sitting postures. Therefore, spinopelvic fusion restricts mobility and increases the mechanical force on the hip to compensate for the restriction of spinopelvic mobility. Some studies have shown the drawbacks of spinopelvic fusion. Spinopelvic fusion is associated with dislocation after THA due to contact with the femoral neck and the acetabular rim [15, 16]. Other studies showed that lumbosacral fusion affects sacroiliac joint pain [17, 18].
Spinal fusion not only improves spinal alignment, but it also increases the mechanical load on adjacent joints and accelerates joint space narrowing. However, this discrepancy has not yet been fully elucidated. The purpose of this retrospective study was to determine (1) if spinal fusion affects joint space narrowing of the hip; (2) if spinal alignment affects joint space narrowing of the hip; and (3) how non-fusion and short and long spinal fusion affect joint space narrowing.
Materials and methods
Patients
This retrospective study examined 530 hips of patients (252 hips of 127 males and 278 hips of 143 females) who underwent spinal surgery between May 2010 and May 2019. This study was approved by the Institutional Review Board of the authors (22R118). The inclusion criteria were as follows: (1) age over 50 years, (2) pre- and postoperative whole standing X-rays, and (3) a follow-up period of over 2 years. The exclusion criteria were as follows: (1) a previously operated-on limb, (2) patients with no hip joint space during preoperative radiography, (3) connective tissue disease, (4) the absence of a pre- or postoperative whole standing X-ray, and (5) a follow-up period of less than 2 years. The requirement for informed consent was waived because of the retrospective nature of the study. The patients were divided into three groups (N group with no fusion; S group with up to three interbody fusions; L group with more than four interbody fusions). The number of patients in each group was as follows: N group, 85 patients with 167 hips; S group, 114 patients with 225 hips; L group, 71 patients with 138 hips.
Demographic data for the three groups are shown in Table 1.
Surgical indication
Spinal surgery without fusion was performed in patients with foraminal stenosis and without instability. Short fusions (up to three interbody fusions) were performed to decompress foraminal stenosis or correct segmental instability. Middle or long fusion (more than four interbody fusions) was performed to correct global sagittal malalignment.
Radiographic assessment
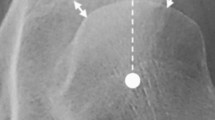
Whole-spine standing radiography was performed preoperatively and more than 2 years after spinal surgery. Sagittal spine radiography was performed in the relaxed standing position. Patients were instructed to look ahead and place their hands on both clavicles [19]. The sagittal vertical axis (SVA), thoracic kyphosis (TK), lumbar lordosis (LL), SS, PT, and PI were evaluated as spinal parameters (Fig. 1) [20, 21]. The center edge (CE) angle [22], Sharp angle, limb length discrepancy [23], and minimum joint width (MJW) of the hip were evaluated as hip parameters (Fig. 2). MJW was measured in 0.1-mm increments between the lateral edge of the acetabulum and fovea (Fig. 2) [24]. The preoperative MJW and postoperative MJW were measured at the same point. The rate of joint space narrowing was calculated using the following formula: {preoperative MJW (mm) − postoperative MJW (mm)}/follow-up years [9].
Measurements of spinal parameters. The SVA was defined as the distance between the vertical line from the center of the seventh vertebral body and the posterior edge of the first sacral vertebra. TK was defined as the angle between the parallel lines drawn along the twelfth inferior thoracic vertebra and the fourth superior thoracic vertebra. LL was defined as the angle between the parallel lines drawn along the first superior lumbar and sacral vertebrae. SS was defined as the angle between the horizontal line and first superior sacral vertebra. PT was defined as the angle between the vertical line and the line connecting the centers of the bilateral femoral heads. PI was defined as the angle between the vertical line from the superior first sacral vertebra and the line connecting the centers of the bilateral femoral heads. SVA sagittal vertical axis, TK thoracic kyphosis, LL lumbar lordosis, SS sacral slope, PT pelvic tilt, PI pelvic incidence
Measurements of hip parameters. The CE angle was defined as the angle between the vertical line and the lateral edge of the acetabulum. The Sharp angle was defined as the line connecting the bilateral teardrops and the lateral edge of the acetabulum. MJS was defined as the narrowest point from the lateral edge of the acetabulum and fovea. Limb length discrepancy was calculated as the perpendicular distance from the line connecting the bilateral teardrops to the center of each lesser trochanter. Limb length discrepancy was defined as the length of the right side (D1) minus that of the left side (D2) and recorded as an absolute value. CE center edge, MJS minimum joint space
All measurements were performed using a picture archiving and communication system (TechMatrix Corporation, Tokyo, Japan). Radiographic evaluation was performed by two orthopedic surgeons. A single surgeon evaluated all radiographic data, and the other orthopedic surgeon evaluated 80 randomly selected radiographic data values. Each surgeon performed the evaluation twice, and the average value was used for the evaluation. The intraclass reliability of the radiographic parameters was as follows: SVA (0.98); TK (0.8); LL (0.91); SS (0.94); PT (0.97); PI (0.92); CE (0.81); Sharp angle (0.83); limb length discrepancy (0.79); and MJW (0.8).
Statistical analysis
Power analysis was performed to calculate the minimum sample sizes needed to perform linear multiple regression (effect size = 0.25, alpha = 0.05, power = 0.95, number of predictors = 15) and one-way analysis of variance (ANOVA) (effect size = 0.25, alpha = 0.05, power = 0.95, number of groups = 3). The calculated sample sizes were 125 and 252, respectively. The G-Power software (version 3.1.9.2, Germany) was used to calculate the sample size.
One-way ANOVA followed by the Bonferroni test were performed to compare the three groups. Multiple regression analyses were performed to identify the independent predictors of the rate of joint space narrowing. Independent variables were as follows: age, sex, body mass index, CE angle, Sharp angle, postoperative limb length discrepancy, postoperative SVA, postoperative TK, postoperative LL, postoperative SS, postoperative PT, postoperative PI, sacral fusion, number of lumbar fusion levels, and follow-up period. Statistical significance was set at a P value of < 0.05. SPSS software (version 26 IBM Corp., Armonk, NY, USA) was used to perform statistical analyses.
Results
One-way ANOVA followed by Bonferroni revealed that the rate of joint space narrowing of the L group (0.10 ± 0.14 mm/year) was significantly higher than those of the other groups (N group; 0.07 ± 0.1 mm/year, S group; 0.06 ± 0.09 mm/year) (P < 0.001). Regarding the rate of joint space narrowing, no statistically significant difference was observed between the N and S groups. As for spinal parameters, the postoperative SVA of the L group (83 ± 63.7 mm) was significantly higher than that of the N group (52.9 ± 55.8 mm). The postoperative SVA of the S group (71.2 ± 53.2 mm) was significantly higher than that of the N group. The postoperative TK in the L group (45.4 ± 16.3°) was significantly higher than those in the other two groups (N: 31.8 ± 11.7°, S: 28.1 ± 12.2°). The postoperative LL of the S group (30.6 ± 15.8°) was significantly lower than those of the other two groups (L: 37.5 ± 18.5°, N: 36 ± 17.2°). The postoperative SS of the L group (23.4 ± 12.8°) was significantly lower than those of the other two groups (N: 28.4 ± 10.7°, S: 27 ± 11.1°). The postoperative PT of the N group (18.5 ± 10.5°) was significantly lower than those of the other two groups (L: 23.6 ± 11.6°, S: 22.7 ± 9.2°) (Table 2). Multiple regression analysis revealed that the number of fusion levels (P < 0.05) and follow-up period (P < 0.001) were independent risk factors for joint space narrowing (Table 3).
Discussion
This study revealed that the rate of joint space narrowing of the L group was significantly higher than those of the other two groups. No significant difference in the rate of joint space narrowing was observed between the N and S groups. The number of fusion levels and the follow-up period were independent risk factors for the rate of joint space narrowing.
The reported percentage of patients with adjacent segmental degeneration after spinal fusion ranges between 5% and 43% [13, 25,26,27]. This percentage is highly dependent on the follow-up period and the number of fusion levels. Some studies have reported the effects of long spinal fusion on joint space narrowing of the hip. Kawai et al. reported that more than seven spinal fusions accelerate joint space narrowing of the hip [11]. Other authors have reported that female patients with more than seven spinal fusions are more likely to develop THA [12]. However, these reports only included patients who underwent spinal fusion, and there are no reports that elucidate the effect of non-fusion and spinal fusion on joint space narrowing. Our results showed no significant difference in the rate of joint space narrowing between the N and S groups. This result indicates that a short fusion (less than three fusions) does not accelerate joint space narrowing of the hip, at least during a short follow-up period. In contrast, the L group had a higher rate of joint space narrowing than the other two groups. The mobility of the thoracolumbar spine in patients with hip OA was lower than that in healthy individuals [28]. In addition, lower spinal mobility has been reported to be a predictor of hip OA progression [4]. The mechanical overload of the hip increases after spinal fusion because hip motion is affected by spinal motion [29, 30], and restriction of the spinopelvic joint mobility compensates for excessive hip motion. This overload causes dislocation after THA [16] and may affect joint space narrowing of the hip. We consider that the hip overload was compensated for by the remaining spinal motion in short fusion and non-fusion. However, compensation does not work in long fusion because most of the lumbar or thoracolumbar joints are fixed. Hence, the rate of joint space narrowing increased only in the L group. Therefore, surgeons should pay attention to accelerated joint space narrowing of the hip, especially after a long fusion.
Limb length discrepancy is observed in hip OA as well as scoliosis patients [31, 32]. It may increase the load on the ipsilateral or contralateral limb and be associated with joint space narrowing of the hip. However, we found no significant differences in our ANOVA and multiple regression analysis. Therefore, we believe that limb length discrepancy does not affect short-term joint space narrowing of the hip.
Some authors have reported that spinal parameters affect the load on the hip joints and hip OA [8]. It has been reported that spinal anterior inclination and a larger SVA increase the load on the hip joint [4]. The load axis may shift anteriorly as SVA increases. Spinal anterior inclination can increase the internal hip extension moment and mechanical load of the hip [4]. The SVA of the L group was higher than that of the N group, but there was no significant difference between the two groups. From this result, we consider that the SVA may not affect the acceleration of the rate of joint space narrowing. LL has also been correlated with hip OA [33]. Pelvic retroversion occurs following lumbar spondylolisthesis and may progress to joint space narrowing of the hip. In this study, the LL in the N and L groups was larger than that in the S group because most of the N group patients did not have severe spinal deformity and the S group patients could not be corrected for sagittal alignment. However, the rate of joint space narrowing in the S group was not significantly different from that in the N group. Thus, other factors may be more affected than LL. PT is consistent with PI, and a higher PI is associated with hip OA. PI is a peculiar pelvic anatomy that remains unchanged even after 10 years [34, 35], and PI, SS, and PT change simultaneously. As PT increases, SS conversely decreases and the pelvis tilts posteriorly. Pelvic posterior tilt is observed in the aging population and is correlated with rapidly destructive coxarthrosis [36]. These spinal parameters may accelerate the rate of narrowing of the joint space. However, these parameters were not independent risk factors for joint space narrowing. Although spinal parameters were different among the three groups, we considered that the spinal fusion level affected the rate of joint space narrowing more than the spinal parameters.
This study has several limitations. First, this was a retrospective study, and several factors affected hip OA. Thus, we could not eliminate all the confounding factors. However, we calculated the sample size and analyzed adequate samples. In addition, we performed linear multiple regression analysis to eliminate the effects of confounding factors. Second, joint space narrowing progresses over a long period, and our average follow-up period was 2.98 years. Thus, a longer follow-up period is needed to elucidate a more detailed analysis. Third, we could not evaluate hip pain because of the retrospective study design. Hip pain is a chief symptom of hip OA; however, the precise association between hip OA and pain remains unclear [37,38,39,40], and most individuals with hip pain do not have radiographic hip OA [38, 41]. Thus, we believe that the evaluation of hip pain is not relevant to this study. Fourth, several methods have been used for the diagnosis of OA. The Kellgren–Laurence grade is commonly used with X-rays for hip OA [42,43,44]. However, there are only four possible grades, and joint space narrowing progresses gradually. Hence, it is difficult to evaluate slight changes in Kellgren–Lawrence grade. We measured MJS directly. This method has already been used to evaluate the rate of joint space narrowing [8, 11, 45], and our intraclass reliability was high. Sixth, we only measured joint space narrowing in this study, even though other findings, such as cartilage thickness, intra-articular fluid, and bone signal intensity changes, are also important. Thus, we plan to evaluate the correlation between spine fusion and these findings in the next study.
In conclusion, the rate of joint space narrowing after long fusions (more than four levels) was significantly higher than that after short fusions (up to three levels) and no fusion. Although spinal parameters were different among the three groups, they were not risk factors for acceleration of the rate of joint space narrowing. Therefore, surgeons should pay attention to the fact that more than four interbody fusions worsen joint space narrowing of the hip.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASD:
-
Adjacent segmental degeneration
- OA:
-
Osteoarthritis
- THA:
-
Total hip arthroplasty
- SVA:
-
Sagittal vertical axis
- TK:
-
Thoracic kyphosis
- LL:
-
Lumbar lordosis
- SS:
-
Sacral slope
- PT:
-
Pelvic tilt
- PI:
-
Pelvic incidence
- CE:
-
Center edge
- MJW:
-
Minimum joint width
References
Lievense AM, Bierma-Zeinstra SMA, Verhagen AP, Verhaar JA, Koes BW (2002) Prognostic factors of progress of hip osteoarthritis: a systematic review. Arthritis Rheum 47:556–562. https://doi.org/10.1002/art.10660
Cheung PP, Gossec L, Dougados M (2010) What are the best markers for disease progression in osteoarthritis (OA)? Best Pract Res Clin Rheumatol 24:81–92. https://doi.org/10.1016/j.berh.2009.08.009
Offierski CM, MacNab I (1983) Hip-spine syndrome. Spine (Phila Pa 1976) 8:316–321. https://doi.org/10.1097/00007632-198304000-00014
Tateuchi H, Akiyama H, Goto K, So K, Kuroda Y, Ichihashi N (2018) Sagittal alignment and mobility of the thoracolumbar spine are associated with radiographic progression of secondary hip osteoarthritis. Osteoarthritis Cartilage 26:397–404. https://doi.org/10.1016/j.joca.2017.12.005
Damm P, Reitmaier S, Hahn S, Waldheim V, Firouzabadi A, Schmidt H (2020) In vivo hip and lumbar spine implant loads during activities in forward bent postures. J Biomech 102:109517. https://doi.org/10.1016/j.jbiomech.2019.109517
Yasuda T, Matsunaga K, Hashimura T, Tsukamoto Y, Sueyoshi T, Ota S et al (2020) Characterization of rapidly progressive osteoarthritis of the hip in its early stage. Eur J Rheumatol 7:130–134. https://doi.org/10.5152/eurjrheum.2020.19159
Morimoto T, Kitajima M, Tsukamoto M, Yoshihara T, Sonohata M, Mawatari M (2018) Sagittal spino-pelvic alignment in rapidly destructive coxarthrosis. Eur Spine J 27:475–481. https://doi.org/10.1007/s00586-017-5282-5
Kawai T, Shimizu T, Goto K, Kuroda Y, Okuzu Y, Otsuki B et al (2022) The impact of spinopelvic parameters on hip degeneration after spinal fusion. Spine 47:1093–1102. https://doi.org/10.1097/BRS.0000000000004340
Raphael IJ, Rasouli MR, Kepler CK, Restrepo S, Albert TJ, Radcliff KE (2016) Pelvic incidence in patients with hip osteoarthritis. Arch Bone Jt Surg 4:132–136
Saltychev M, Pernaa K, Seppänen M, Mäkelä K, Laimi K (2018) Pelvic incidence and hip disorders. Acta Orthop 89:66–70. https://doi.org/10.1080/17453674.2017.1377017
Kawai T, Shimizu T, Goto K, Kuroda Y, Okuzu Y, Fujibayashi S, Matsuda S (2021) Number of levels of spinal fusion associated with the rate of joint-space narrowing in the hip. J Bone Joint Surg Am 103:953–960. https://doi.org/10.2106/JBJS.20.01578
Lum ZC, Klineberg EO, Danielsen B, Giordani M, Meehan JP (2019) Female sex and longer fusion constructs significantly increase the risk of total hip arthroplasty following spinal fusion. J Bone Joint Surg Am 101:675–681. https://doi.org/10.2106/JBJS.18.00667
Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG (2004) Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 86:1497–1503. https://doi.org/10.2106/00004623-200407000-00020
Hashimoto K, Aizawa T, Kanno H, Itoi E (2019) Adjacent segment degeneration after fusion spinal surgery- a systematic review. Int Orthop 43:987–993. https://doi.org/10.1007/s00264-018-4241-z
Haffer H, Adl Amini D, Perka C, Pumberger M (2020) The impact of spinopelvic mobility on arthroplasty: implications for hip and spine surgeons. J Clin Med 9:2569. https://doi.org/10.3390/jcm9082569
Furuhashi H, Yamato Y, Hoshino H, Shimizu Y, Hasegawa T, Yoshida G et al (2021) Dislocation rate and its risk factors in total hip arthroplasty with concurrent extensive spinal corrective fusion with pelvic fixation for adult spinal deformity. Eur J Orthop Surg Traumatol 31:283–290. https://doi.org/10.1007/s00590-020-02764-6
Kim KT, Lee SH, Lee YH, Bae SC, Suk KS (2006) Clinical outcomes of 3 fusion methods through the posterior approach in the lumbar spine. Spine 31:1351–1358. https://doi.org/10.1097/01.brs.0000218635.14571.55
Onsel C, Collier BD, Kir KM, Larson SJ, Meyer GA, Krasnow AZ et al (1992) Increased sacroiliac joint uptake after lumbar fusion and/or laminectomy. Clin Nucl Med 17:283–287. https://doi.org/10.1097/00003072-199204000-00004
Hiyama A, Katoh H, Sakai D, Tanaka M, Sato M, Watanabe M (2019) The correlation analysis between sagittal alignment and cross-sectional area of paraspinal muscle in patients with lumbar spinal stenosis and degenerative spondylolisthesis. BMC Musculoskelet Disord 20:352. https://doi.org/10.1186/s12891-019-2733-7
Ames CP, Smith JS, Scheer JK, Bess S, Bederman SS, Deviren V et al (2012) Impact of spinopelvic alignment on decision making in deformity surgery in adults: a review. J Neurosurg Spine 16:547–564. https://doi.org/10.3171/2012.2.SPINE11320
Hiyama A, Katoh H, Sakai D, Sato M, Tanaka M, Nukaga T, Watanabe M (2018) Correlation analysis of sagittal alignment and skeletal muscle mass in patients with spinal degenerative disease. Sci Rep Sci Rep 8:15492. https://doi.org/10.1038/s41598-018-33867-0
Hanson JA, Kapron AL, Swenson KM, MaarK TG, Peters CL, Aoki SK (2015) Discrepancies in measuring acetabular coverage revisiting the anterior and lateral center edge angles. J Hip Preserv Surg 2:280–286. https://doi.org/10.1093/jhps/hnv041
Lim YW, Huddleston JI 3rd, Goodman SB, Maloney WJ, Amanatullar DF (2018) Proximal femoral shape changes the risk of a leg length discrepancy after primary total hip arthroplasty. J Arthroplasty 33:3699–3703. https://doi.org/10.1016/j.arth.2018.08.008
Tateuchi H, Koyama Y, Akiyama H, Goto K, So K, Kuroda Y, Ichihashi N (2017) Daily cumulative hip moment is associated with radiographic progression of secondary hip osteoarthritis. Osteoarthritis Cartilage 25:1291–1298
Frymoyer JW, Hanley E, Howe J, Kuhlmann D, Matteri R (1978) Disc excision and spine fusion in the management of lumbar disc disease. A minimum ten-year followup. Spine 3:1–6. https://doi.org/10.1097/00007632-197803000-00001
Lehmann TR, Spratt KF, Tozzi JE, Weinstein JN, Reinarz SJ, El-Khoury GY, Colby H (1987) Long-term follow-up of lower lumbar fusion patients. Spine 12:97–104. https://doi.org/10.1097/00007632-198703000-00004
Penta M, Sandhu A, Fraser RD (1995) Magnetic resonance imaging assessment of disc degeneration 10 years after anterior lumbar interbody fusion. Spine 20:743–747. https://doi.org/10.1097/00007632-199503150-00018
Mannion AF, Knecht K, Balaban G, Dvorak J, Grob D (2004) A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine: reliability of measurements and comparison with data reviewed from the literature. Eur Spine J 13:122–136. https://doi.org/10.1007/s00586-003-0618-8
Tafazzol A, Arjmand N, Shirazi-Adl A, Parnianpour M (2014) Lumbopelvic rhythm during forward and backward sagittal trunk rotations: combined in vivo measurement with inertial tracking device and biomechanical modeling. Clin Biomech (Bristol Avon) 29:7–13. https://doi.org/10.1016/j.clinbiomech.2013.10.021
Shum GLK, Crosbie J, Lee RYW (2005) Effect of low back pain on the kinematics and joint coordination of the lumbar spine and hip during sit-to-stand and stand-to-sit. Spine 30:1998–2004. https://doi.org/10.1097/01.brs.0000176195.16128.27
Murray KJ, Azari MF (2015) Leg length discrepancy and osteoarthritis in the knee, hip and lumbar spine. J Can Chiropr Assoc 59:226–237
Buyukaslan A, Abul K, Berk H, Yilmaz H (2022) Leg length discrepancy and adolescent idiopathic scoliosis: clinical and radiological characteristics. Spine Deform 10:307–3014. https://doi.org/10.1007/s43390-021-00442-z
Farfan HF (1980) The pathological anatomy of degenerative spondylolisthesis. A cadaver study. Spine 5:412–418. https://doi.org/10.1097/00007632-198009000-00004
Mac-Thiong JM, Berthonnaud E, Dimar JR 2nd, Betz RR, Labelle H (2004) Sagittal alignment of the spine and pelvis during growth. Spine (Phila Pa 1976) 29:1642–1647. https://doi.org/10.1097/01.brs.0000132312.78469.7b
Mangione P, Gomez D, Senegas J (1997) Study of the course of the incidence angle during growth. Eur Spine J 6:163–167. https://doi.org/10.1007/BF01301430
Onishi E, Ota S, Fujita S, Tsukamoto Y, Yamashita S, Hashimura T et al (2022) Association between sagittal spinopelvic alignment and femoral head destruction in the early stage of rapidly destructive coxopathy. Bone Jt Open Bone Jt Open 3:77–84. https://doi.org/10.1302/2633-1462.31.BJO-2021-0175.R1
Iidaka T, Muraki S, Akune T, Oka H, Kodama R, Tanaka S et al (2016) Prevalence of radiographic hip osteoarthritis and its association with hip pain in Japanese men and women: the ROAD study. Osteoarthritis Cartilage 24:117–123. https://doi.org/10.1016/j.joca.2015.07.017
Park JH, Lee JS, Lee SJ, Kim YH (2021) Low prevalence of radiographic hip osteoarthritis and its discordance with hip pain: a nationwide study in Korea. Geriatr Gerontol Int 21:20–26. https://doi.org/10.1111/ggi.14085
Jacobsen S, Sonne-Holm S, Søballe K, Gebuhr P, Lund B (2004) Radiographic case definitions and prevalence of osteoarthrosis of the hip: a survey of 4151 subjects in the Osteoarthritis Substudy of the Copenhagen City Heart Study. Acta Orthop Scand 75:713–720. https://doi.org/10.1080/00016470410004085
Birrell F, Lunt M, Macfarlane G, Silman A (2005) Association between pain in the hip region and radiographic changes of osteoarthritis: results from a population based study. Rheumatology 44:337–341. https://doi.org/10.1093/rheumatology/keh458
Rondas GAM, Macri EM, Oei EHG, Bierma-Zeinstra SMA, Rijkels-Otters HBM et al (2022) Association between hip pain and radiographic hip osteoarthritis in primary care. Br J Gen Pract 72:e722–e728. https://doi.org/10.3399/BJGP.2021.0547
Reijman M, Hazes JMW, Koes BW, Verhagen AP, Bierma-Zeinstra SM (2004) Validity, reliability, and applicability of seven definitions of hip osteoarthritis used in epidemiological studies: a systematic appraisal. Ann Rheum Dis 63:226–232. https://doi.org/10.1136/ard.2003.010348
Bergink AP, Zillikens MC, Van Leeuwen JPTM, Hofman A, Uitterlinden AG, van Meurs JBJ (2016) 25-Hydroxyvitamin D and osteoarthritis: a meta-analysis including new data. Semin Arthritis Rheum 45:539–546. https://doi.org/10.1016/j.semarthrit.2015.09.010
Bouyer B, Mazieres B, Guillemin F, Bouttier R, Fautrel B, Morvan J et al (2016) Association between hip morphology and prevalence, clinical severity and progression of hip osteoarthritis over 3 years: the knee and hip osteoarthritis long-term assessment cohort results. Jt Bone Spine 83:432–438. https://doi.org/10.1016/j.jbspin.2015.09.005
Kozaki T, Hashizume H, Nishiyama D, Iwasaki H, Tsutsui S, Takami M et al (2021) Adjacent segment disease on hip joint as a complication of spinal fusion surgery including sacroiliac joint fixation. Eur Spine J 30:1314–1319. https://doi.org/10.1007/s00586-020-06700-4
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
TU conceptualized and designed this study; TU and KY acquired and analyzed the data; TU drafted the article; HK, KY, SM, and MW critically revised the important intellectual content of the manuscript; all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the Declaration of Helsinki and after the authors had received ethical committee approval (approval number: 22R118).
Consent for publication
Not applicable.
Competing interests
The authors have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ukai, T., Katoh, H., Yokoyama, K. et al. Effect of spinal fusion on joint space narrowing of the hip: comparison among non-fusion, short fusion, and middle or long fusion. J Orthop Traumatol 24, 1 (2023). https://doi.org/10.1186/s10195-022-00682-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-022-00682-3