Abstract
Introduction
Hip–spine syndrome, wherein flexion deformity of the hip might exaggerate normal lumbar lordosis (LL), was first described in 1983. It could result in subluxation of the posterior facets and cause low back pain (LBP). However, the clinical outcomes of total hip arthroplasty (THA) and spinal alignment changes in patients with lumbar hyperlordosis (hyper LL) remain unknown. We aimed to clarify the proportion of patients with hyper LL before THA and compare pre- and post-operative sagittal spinal alignment, LBP, and clinical outcomes between patients with hyper LL and those with normal LL.
Materials and methods
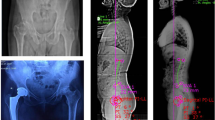
We investigated 278 patients who underwent primary THA between December 2015 and December 2019. Spine radiographs in the standing position were examined preoperatively and 1 year postoperatively. Patients with hyper LL were defined as having a pelvic incidence (PI) minus LL of < − 9° preoperatively. The control group included age- and sex-matched patients with normal LL, defined by a PI minus LL of − 9° to 9°. Clinical outcomes were evaluated using the visual analogue scale (VAS) for LBP, Harris hip score (HHS), Oxford hip score (OHS), and University of California, Los Angeles (UCLA) activity score.
Results
Thirty-eight patients (13.7%) had hyper LL, and they exhibited a lower pelvic tilt, lower sagittal vertical axis, and greater sigmoid curvature than did the controls. Evaluation of changes in the spinal alignment after surgery showed that the pelvis tilted more posteriorly, and LL decreased more in the hyper LL group than in the control group. Pre- and post-operative VAS for LBP, HHS, OHS, and UCLA activity scores were not significantly different between the two groups.
Conclusion
Hyper LL in patients with hip osteoarthritis had no adverse effects on LBP and the clinical outcomes of THA. Hyper LL may partially result from a flexible and adaptable lumbo-pelvic structure.




Similar content being viewed by others
Data availability
The datasets analyzed in this study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Offierski CM, MacNab I (1983) Hip–spine syndrome. Spine (Phila Pa 1976) 8:316–321. https://doi.org/10.1097/00007632-198304000-00014
Ellenrieder M, Bader R, Bergschmidt P, Fröhlich S, Mittelmeier W (2015) Coexistent lumbar spine disorders have a crucial impact on the clinical outcome after total hip replacement. J Orthop Sci 20:1046–1052. https://doi.org/10.1007/s00776-015-0764-y
Prather H, Van Dillen LR, Kymes SM, Armbrecht MA, Stwalley D, Clohisy JC (2012) Impact of coexistent lumbar spine disorders on clinical outcomes and physician charges associated with total hip arthroplasty. Spine J 12:363–369. https://doi.org/10.1016/j.spinee.2011.11.002
Ochi H, Homma Y, Baba T, Nojiri H, Matsumoto M, Kaneko K (2017) Sagittal spinopelvic alignment predicts hip function after total hip arthroplasty. Gait Posture 52:293–300. https://doi.org/10.1016/j.gaitpost.2016.12.010
Di Martino A, Bordini B, Ancarani C, Viceconti M, Faldini C (2021) Does total hip arthroplasty have a higher risk of failure in patients who undergo lumbar spinal fusion? Bone Joint J 103-B:486–491. https://doi.org/10.1302/0301-620X.103B3.BJJ-2020-1209.R1
Schwab F, Lafage V, Patel A, Farcy JP (2009) Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 34:1828–1833. https://doi.org/10.1097/BRS.0b013e3181a13c08
Jentzsch T, Geiger J, König MA, Werner CM (2017) Hyperlordosis is associated with facet joint pathology at the lower lumbar spine. Clin Spine Surg 30:129–135. https://doi.org/10.1097/BSD.0b013e3182aab266
Chun SW, Lim CY, Kim K, Hwang J, Chung SG (2017) The relationships between low back pain and lumbar lordosis: a systematic review and meta-analysis. Spine J 17:1180–1191. https://doi.org/10.1016/j.spinee.2017.04.034
Kim Y, Pour AE, Lazennec JY (2020) How do global sagittal alignment and posture change after total hip arthroplasty? Int Orthop 44:267–273. https://doi.org/10.1007/s00264-019-04363-5
Radcliff KE, Orozco F, Molby N, Delasotta L, Chen E, Post Z, Ong A (2013) Change in spinal alignment after total hip arthroplasty. Orthop Surg 5:261–265. https://doi.org/10.1111/os.12076
Taki N, Mitsugi N, Mochida Y, Akamatsu Y, Saito T (2012) Change in pelvic tilt angle 2 to 4 years after total hip arthroplasty. J Arthroplasty 27:940–944. https://doi.org/10.1016/j.arth.2011.10.003
Suzuki H, Inaba Y, Kobayashi N, Ishida T, Ike H, Saito T (2016) Postural and chronological change in pelvic tilt five years after total hip arthroplasty in patients with developmental dysplasia of the hip: a three-dimensional analysis. J Arthroplasty 31:317–322. https://doi.org/10.1016/j.arth.2015.07.026
Lembeck B, Mueller O, Reize P, Wuelker N (2005) Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop 76:517–523. https://doi.org/10.1080/17453670510041501
Moskal JT, Capps SG (2011) Acetabular component positioning in total hip arthroplasty: an evidence-based analysis. J Arthroplasty 26:1432–1437. https://doi.org/10.1016/j.arth.2010.11.011
Digioia AM 3rd, Jaramaz B, Plakseychuk AY, Moody JE Jr, Nikou C, Labarca RS, Levison TJ, Picard F (2002) Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty 17:359–364. https://doi.org/10.1054/arth.2002.30411
Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60:217–220. https://doi.org/10.2106/00004623-197860020-00014
Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A (2019) Sagittal balance of the spine. Eur Spine J 28:1889–1905. https://doi.org/10.1007/s00586-019-06083-1
Rivière C, Lazennec JY, Van Der Straeten C, Auvinet E, Cobb J, Muirhead-Allwood S (2017) The influence of spine–hip relations on total hip replacement: a systematic review. Orthop Traumatol Surg Res 103:559–568. https://doi.org/10.1016/j.otsr.2017.02.014
Acknowledgements
None.
Funding
This research received a Grant from the Japan Orthopaedics and Traumatology Foundation, Inc. (Grant number 463).
Author information
Authors and Affiliations
Contributions
YO and TM collected and interpreted the patient’s data. YO was a major contributor in writing the manuscript. TM, TK, YK, KG, and SM were involved in report design, critically revised the report, and commented on drafts of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Shuichi Matsuda has received speaker and consultant honoraria from Kyocera. Other authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Kyoto University approved this study.
Consent to participate
Informed consent to use patients’ data for retrospective studies was obtained before surgery.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Okuzu, Y., Miyahara, T., Goto, K. et al. Investigating sagittal spinal alignment, low back pain, and clinical outcomes after total hip arthroplasty for lumbar hyperlordosis: a retrospective study. Arch Orthop Trauma Surg 142, 4007–4013 (2022). https://doi.org/10.1007/s00402-021-04266-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04266-4