Abstract
Background
Eptinezumab demonstrated efficacy in adults with migraine and prior preventive treatment failures in the placebo-controlled phase of the DELIVER clinical trial; its long-term effectiveness in this population has not yet been reported. The objective of this study was to evaluate the long-term effectiveness of eptinezumab in a migraine patient population during the 48-week extension phase of DELIVER.
Methods
DELIVER was conducted June 1, 2020 to September 15, 2022. 865 adults with migraine, with documented evidence of 2–4 prior preventive migraine treatment failures and with completion of the 24-week placebo-controlled period of DELIVER received eptinezumab (100 or 300 mg) during the dose-blinded extension, either continuing their randomized dose or, if originally receiving placebo, were randomized 1:1 to an eptinezumab dose (100 or 300 mg). A mixed model for repeated measures was used to evaluate changes from baseline in the number of monthly migraine days (MMDs).
Results
Of 865 patients entering the extension (eptinezumab 100 mg, n = 433; 300 mg, n = 432), 782 (90.4%) completed and 11 (1.3%) discontinued due to an adverse event. Eptinezumab was associated with early and sustained reductions in migraine frequency. Mean MMDs at baseline were approximately 14 days across groups. Mean (standard error) change from baseline in MMDs over the final dosing interval (weeks 61–72) was −6.4 (0.50) with placebo/eptinezumab 100 mg, –7.3 (0.49) with placebo/eptinezumab 300 mg, –7.1 (0.39) with eptinezumab 100 mg, and −7.0 (0.39) with eptinezumab 300 mg. During weeks 61–72, 63–70% of patients demonstrated ≥ 50% reduction in MMDs, and 36–45% demonstrated ≥ 75% reduction. Headache severity and acute medication use reductions, and patient-reported improvements in most bothersome symptom, disease status, quality of life, and work productivity, were observed. Adverse events were generally mild, transient, and similar in frequency/type to previous eptinezumab trials.
Conclusions
The long-term effectiveness and safety/tolerability of eptinezumab in patients with migraine and 2–4 prior preventive treatment failures was demonstrated by high completion rates and migraine-preventive benefits sustained for up to 18 months, implying that eptinezumab is a viable long-term treatment option for patients still seeking successful migraine treatments.
Trial registration
ClinicalTrials.gov (Identifier: NCT04418765; URL: https://www.clinicaltrials.gov/ct2/show/NCT04418765); EudraCT (Identifier: 2019-004497-25; URL: https://www.clinicaltrialsregister.eu/ctr-search/search?query=2019-004497-25).
Graphical Abstract

Similar content being viewed by others
Introduction
Migraine is a chronic neurological disorder that affects an estimated 15% of the global population (over 1 billion people worldwide) [1]. In Europe, the economic consequences of migraine were estimated at €50 billion to €111 billion. Furthermore, direct healthcare costs, which primarily included outpatient care, acute medications and hospitalization, were €1222 per person with migraine in 2011 [2]. Preventive therapy is a crucial aspect of long-term migraine management and could help achieve the goal of reducing utilization of urgent care, outpatient infusions, and inpatient infusions. It is recommended for reducing attack frequency, severity, and duration, as well as for minimizing acute medication use and interictal burden and for enhancing health-related quality of life [3].
Monoclonal antibodies targeting calcitonin gene-related peptide (CGRP) are increasingly used for migraine prevention, particularly in patients who have experienced the failure of older, non-specific oral preventives [4,5,6,7]. Eptinezumab is an intravenously (IV)-administered anti-CGRP monoclonal antibody that has demonstrated efficacy in reducing headache frequency and impact across the migraine spectrum, with a fast onset of effect and sustained improvements throughout treatment [8,9,10,11,12,13,14]. In the phase 3b DELIVER trial, eptinezumab reduced migraine frequency and health-related impact in adults with 2–4 documented prior preventive treatment failures [4, 15, 16]. The objective of this 48-week, dose-blinded extension of the DELIVER trial was to evaluate the long-term effect of eptinezumab in this difficult-to-treat patient population who were unsuccessfully treated with several classes of older, non-specific oral preventive treatments.
Methods
Study design
DELIVER was a multicenter, parallel-group, randomized, double-blind, placebo-controlled phase 3b clinical trial that evaluated the efficacy and safety of eptinezumab for migraine prevention in patients for whom previous preventive treatments failed. The total study duration was 76 weeks, including a screening period of 28‒30 days, a placebo-controlled period of 24 weeks, and a dose-blinded extension period of 48 weeks. The detailed methodology has been published [4], including the protocol and statistical analysis plan; however, key elements are summarized here. The study was conducted in accordance with standards of Good Clinical Practice as defined by the International Conference on Harmonisation and all applicable federal and local regulations. The local review board or a central institutional review board/ethics committee approved all study documentation at each of the 96 study sites. All patients provided written informed consent prior to study participation. Sex and race were self-identified by patients based on fixed categories. DELIVER was registered on ClinicalTrials.gov (NCT04418765) and EudraCT (2019-004497-25).
Patients
DELIVER enrolled adults (18‒75 years [inclusive]) with migraine and documented evidence of 2–4 previous preventive treatment failures in the prior 10 years. Key inclusion criteria included: onset of migraine (International Classification of Headache Disorders 3rd edition [ICHD-3] [17]) at or before 50 years of age; a history of migraine for ≥ 12 months prior to the screening visit; criteria met for chronic migraine (migraine occurring on ≥ 8 days and headache occurring on > 14 days) or episodic migraine (migraine occurring on ≥ 4 days/month and headache occurring on ≤ 14 days/month) during the screening period; a history of 2–4 previous preventives failing due to inadequate efficacy, safety/tolerability reasons, or contraindications (≥ 1 of the failures had to be due to inadequate efficacy following ≥ 3 months of treatment with the locally recommended dose); and compliance demonstrated with the headache eDiary by data entry for ≥ 24 of the 28 days prior to randomization.
Key exclusion criteria included: failure on a previous treatment targeting the CGRP pathway; confounding and clinically significant pain syndromes; diagnosis of temporomandibular disorder; history or diagnosis of other primary headache types; history of clinically significant cardiovascular disease; uncontrolled and/or untreated psychiatric condition; and use of preventive migraine medication within 1 week prior to the screening visit. Patients with concurrent diagnosis of medication-overuse headache (defined by clinical ICHD-3 criteria [17]) were allowed. Use of acute migraine treatments was allowed provided the dose had been stable for ≥ 12 weeks prior to the screening visit. Medications constituting 2–4 prior preventive treatment failures (beta-blockers: propranolol, metoprolol; anticonvulsants: topiramate, valproate, or divalproex; tricyclic antidepressants: amitriptyline; calcium channel blocker: flunarizine; angiotensin II receptor antagonist: candesartan; medications locally approved for prevention of migraine) were disallowed; however, medications within the same classes as the disallowed preventive migraine medications could be used for other comorbidities.
Interventions
For the 24-week, placebo-controlled treatment period, patients were randomized to eptinezumab 100 mg, eptinezumab 300 mg, or placebo IV every 12 weeks in a 1:1:1 fashion, with randomization stratified by monthly headache days (MHDs) at baseline (≤ 14 MHDs or > 14 MHDs) and by country. For the 48-week dose-blinded extension, patients who had received eptinezumab in the double-blind phase continued at their randomized dose (100 mg or 300 mg); patients who had received placebo were randomized 1:1 to eptinezumab 100 mg or 300 mg. Codes for randomization in the extension period were assigned at the start of the study. Eptinezumab was administered intravenously once every 3 months for 4 additional doses.
Throughout the study, patients kept a headache eDiary, which comprised evening reports (completed daily regardless of the presence or absence of headaches) and headache reports (completed for each headache that occurred). The latter were used to document headache start and stop times, characteristics, symptoms, severity (mild, moderate, or severe), and acute medication intake in connection with the headache.
Outcomes
Changes from baseline in the number of monthly migraine days (MMDs) and the percentages of patients achieving ≥ 50% reduction in MMDs (≥ 50% response) and ≥ 75% reduction in MMDs (≥ 75% response) during Weeks 25–36, 37–48, 49–60, and 61–72 were predefined secondary study endpoints. These endpoints were derived from data collected via the eDiary. The change from baseline in the 6-item Headache Impact Test (HIT-6) total score at Weeks 36, 48, 60, and 72 was also a predefined secondary endpoint.
Predefined exploratory endpoints included the change from baseline in the percentage of migraine attacks of severe intensity (Weeks 25–36, 37–48, 49–60, and 61–72); change from baseline in monthly acute migraine medication use; patient-identified most bothersome symptom (PI-MBS) score (Weeks 36, 48, 60, and 72); Patient Global Impression of Change (PGIC) score (Weeks 36, 48, 60, and 72); change from baseline in Migraine-Specific Quality of Life questionnaire (MSQ) subscores (Weeks 36, 48, 60, and 72); change from baseline in EQ-5D-5L visual analog scale (VAS) score (Weeks 36, 48, 60, and 72); and change from baseline in Work Productivity and Impairment, adapted for Migraine (WPAI:M) subscores for absenteeism, presenteeism, work productivity loss, and activity impairment (Weeks 36, 48, 60, and 72). Patient-reported outcomes are described in the Supplemental Methods.
The safety/tolerability of long-term eptinezumab treatment was assessed identically to the primary report and included adverse event monitoring, clinical laboratory testing, physical examinations, electrocardiograms, the Columbia–Suicide Severity Rating Scale, and blood sampling for anti-drug antibody assessment [18].
Sample size
Sample size calculations were made for the placebo-controlled period and no power calculations were made for the extension period. Based on simulations, an estimated 280 patients per treatment arm (eptinezumab 100 mg, 300 mg, and placebo) provided ≥ 90% power for the primary endpoint and ≥ 68% power for the individual key secondary endpoints [4].
Statistical analysis
All patients who received ≥ 1 infusion and had a visit in the extension period were included in the safety analyses. All patients who had a valid baseline assessment and a valid assessment of MMDs in the extension period were included in the efficacy analyses. Baseline was the 28-day screening period that occurred before the placebo-controlled treatment period.
A mixed model for repeated measures similar to the one used for the primary endpoint (2-sided; 95% CI) [4] was used to evaluate changes from baseline in the number of MMDs as well as changes from baseline in HIT-6 score. For migraine responder rates, counts and proportions are presented. All exploratory endpoints were analyzed similarly to the secondary endpoints. The eDiary endpoints were derived using prorating if data were captured for ≥ 14 of the 28 days in a 4-week period. Analyses were conducted using SAS software (SAS Institute, Inc., Cary, NC, USA) v9.4 or later.
Results
Patients
Of 892 patients randomized in the 24-week placebo-controlled period, 865 (97.0%) completed that portion of the study, enrolled in this dose-blinded extension period, and comprised the safety analysis set (eptinezumab 100 mg, n = 433; eptinezumab 300 mg, n = 432). The efficacy analysis set included 858 patients. Of the 865 patients entering the extension period, 782 (90.4%) completed it (Fig. 1). Key baseline characteristics are summarized in Table 1; as the extension population comprised 97% of the entire study population, it seems reasonable to expect that additional parameters not listed here would be similar to those described in the primary report [4].
CONSORT diagram of patient disposition. Safety analyses were conducted in the all-patients-treated set, which included all randomized patients who received ≥ 1 infusion of double-blind study drug and had a visit in the extension period. Efficacy analyses were conducted in the full analysis set, which included all randomized patients who received ≥ 1 infusion of double-blind study drug, had a valid baseline assessment, and had ≥ 1 valid assessment of monthly migraine days in the extension period
There was a high level of compliance with the eDiary. The mean rate of missing eDiary data was ~ 10% (mean [SE]: 10.1% [0.65], 100 mg; 9.0% [0.56], 300 mg) during Weeks 25–28, and only increased to ~ 18% during Weeks 69–72 (17.5% [1.04], 100 mg; 18.3% [0.99], 300 mg). The proportion of patients with ≥ 14 days of compliance was 98.5% during Weeks 25–28 and gradually declined to 92.9% at Weeks 69–72.
Migraine frequency
Migraine frequency was similar across treatment groups at baseline (~ 14 MMDs). Over the final 4 weeks of the double-blind treatment period (Weeks 21–24), mean (SE) reductions in MMDs were greater in patients that received eptinezumab (−5.6 [0.39] MMDs, 100 mg; −5.7 [0.39] MMDs, 300 mg) than in patients that received placebo (−2.3 [0.50] MMDs, placebo/100 mg and −2.8 [0.50] MMDs, placebo/300 mg) (Supplemental Table 1). For those patients randomized to placebo during the placebo-controlled period, that were only starting treatment with eptinezumab in the long-term extension, the first dose of eptinezumab on average resulted in a steep decrease in MMDs relative to baseline (Weeks 25–28: −5.8 [0.50] MMDs, placebo/100 mg; −7.2 [0.50] MMDs, placebo/300 mg), similar to what was observed with the first eptinezumab treatment in the placebo-controlled period. In all groups, mean reductions in MMDs were sustained through the final assessment (Fig. 2).
Migraine responder rates are depicted in Fig. 3. For patients who switched from placebo to eptinezumab, the first eptinezumab dose (Weeks 25–36) resulted in a more than doubling of ≥ 50% responder rates and an approximate tripling of ≥ 75% responder rates relative to the preceding dosing interval (Weeks 13–24).
Headache impact
Mean HIT-6 total scores were similar across treatment groups at baseline (66.0–66.6), indicating a population with severe headache-related life impact. Improvement was observed at the first assessment after the first eptinezumab infusion for those initially treated with eptinezumab and for those switching from placebo to eptinezumab for the extension period (Fig. 4). HIT-6 total score was reduced by a mean (SE) of −7.3 (0.56) and −7.6 (0.55) points at Week 4 in patients that received eptinezumab 100 mg and 300 mg, respectively, from the start of the study, and by −9.7 (0.83) and −11.5 (0.83) at Week 28 in patients that were switched to eptinezumab 100 mg and 300 mg, respectively. By the end of the extension, mean HIT-6 total scores were reduced by a similar extent across groups (−11.0 to −14.0 points); this represents a change in headache-related life impact from severe impact (mean HIT-6 total score was ~ 66.4 at baseline across groups; total score range 60–78 = severe) to some impact (mean HIT-6 total score was ~ 52–55 over Weeks 69–72 across groups; total score range 50–55 = some) for these participants.
At baseline, the proportion of migraine attacks with severe intensity ranged 37.6–47.3% across treatment groups. Reductions in severe migraine attacks with eptinezumab were sustained or further improved with continued treatment (Fig. 5). Improvement was observed soon after the start of eptinezumab treatment, with mean (SE) reductions of 18.4% (1.89) and 19.9% (1.89) over Weeks 1–4 in patients initially receiving eptinezumab 100 mg and 300 mg, respectively, and mean (SE) reductions of 21.3% (2.66) and 23.9% (2.67) over Weeks 25–28 in patients switched from placebo to eptinezumab 100 mg and 300 mg, respectively. Over the final 4 weeks (Weeks 69–72), the proportion of migraine attacks reported as severe was reduced by 22.1‒25.3% across treatment groups relative to baseline.
Acute migraine medication use
At baseline, patients across treatment groups were using acute migraine medications for ~ 11 days/month, generally above the ICHD-3 threshold for acute medication overuse, depending on type of acute medication used. In all groups, patients used ~ 5 fewer acute migraine medication days/month during the first eptinezumab dosing interval compared to baseline (Weeks 1–12 for patients initially treated with eptinezumab and Weeks 25–36 for patients switched from placebo to eptinezumab). Thus, the population mean for acute medication use was reduced to below ICHD-3 thresholds for acute medication overuse. Use remained at similarly reduced levels for the remainder of eptinezumab treatment (Fig. 6).
Mean changes from baseline in acute migraine medication days/month (MMRM; efficacy analysis set). Acute migraine medication types included ergotamine, triptan, simple analgesic, combination analgesic, and opioid. BL, baseline; Epti, eptinezumab; LS, least squares; MMRM, mixed model for repeated measures
Other patient-reported outcomes
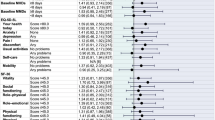
The impact of treatment on other patient-reported outcomes was also positive, demonstrating consistency with each additional dose, and with the placebo-to-active arms achieving similar outcomes to the active-to-active arms over time (Supplemental Table 1). By the end of the study, mean PI-MBS and PGIC scores reflected “much improvement” in patients’ most bothersome symptom and disease status, respectively (Supplemental Figs. 1 and 2). Mean MSQ role function‒restrictive subscores had improved by 32 to 40 points and role function‒preventive and emotional function subscores by 26–33 points each (Supplemental Table 1). Mean EQ-5D-5L scores had improved by 6–9 points (Supplemental Fig. 3). Working patients reported 3.5‒7.4 fewer days missed (WPAI:M absenteeism), and reductions in WPAI:M presenteeism, work productivity loss, and activity impairment subscores were consistent with greater ability to function at work when present (Supplemental Table 1).
Safety
Treatment-emergent adverse events (TEAEs) were reported with similar frequency across groups (Table 2); the most commonly reported TEAEs were COVID-19, nasopharyngitis, and upper respiratory tract infection. The proportions of patients with serious adverse events, TEAEs leading to withdrawal, and TEAEs leading to infusion interruption were low.
Discussion
The long-term extension phase of the DELIVER trial shows that the benefits of eptinezumab treatment in reducing migraine frequency and impact are sustained for up to 18 months in patients with migraine and 2–4 prior preventive treatment failures. Patients who were originally randomized to placebo during the double-blind phase experienced an immediate decrease in MMDs with the first dose of eptinezumab in the extension phase that was a similar level of MMDs experienced by those who received eptinezumab during the placebo-controlled phase. The improvements observed over time with each additional infusion suggests a sustained or potentially additive effect of continued treatment, possibly justifying continuing eptinezumab beyond current stopping rules. This is especially important in consideration that a sizable portion of the DELIVER population may meet criteria for resistant or refractory migraine [19], which are frequently encountered in clinical practice and for which less than half of healthcare providers are highly confident in treating [20]. Intravenous eptinezumab has also been suggested as a rescue treatment in the emergency department to be then continued as preventative, attesting to long-term benefits [21]. The dose regimens used in DELIVER (100 or 300 mg every 12 weeks) are those currently approved by the US Food and Drug Administration [22] and the European Medicines Agency [23], among other regulatory authorities.
While the migraine responder rates tended to favor the higher eptinezumab dose (300 mg) in the placebo-controlled phase of the study, the effectiveness of the 100-mg dose approached that of the 300-mg dose with longer-term treatment. The proportion of patients experiencing a ≥ 50% reduction in MMDs during the final 12 weeks of the long-term extension was similar across all 4 treatment groups. The ≥ 75% migraine responder rates, however, continued to favor the higher dose at this timepoint. At present, long-term data beyond 1 year in similar patient populations are available for only one other anti-CGRP monoclonal antibody (erenumab) [24]; data from other agents are limited to 3–6 months [1, 7]. The proportions of patients achieving a ≥ 50% reduction in MMDs in the 2-year LIBERTY study were 47% over Weeks 61–64 and 57% over Weeks 109–112; ≥75% responder rates were 23% and 31% over Weeks 61–64 and 109–112, respectively [24].
Following eptinezumab initiation, patients used ~ 5 fewer days/month of acute migraine medications use when compared to baseline, bringing the average to below thresholds for medication overuse [17]. The change from baseline in patients switching from placebo to eptinezumab was similar in magnitude to that observed in patients initially randomized to eptinezumab, and across groups, acute medication use remained at a similarly reduced level for the remainder of eptinezumab treatment. This decrease in the amount of acute migraine medication needed signifies the long-term effectiveness of eptinezumab and its potential to revert and/or prevent medication overuse in a refractory patient population [25].
Improvements in patient-reported outcomes indicate that patients perceived benefits beyond reduced migraine frequency and acute medication use with eptinezumab therapy. Across measures of disease-related functioning, impact, quality of life, and work productivity, patients treated with eptinezumab experienced improvements following the first administration, which demonstrated consistency or further improvement with each subsequent administration. By the end of study, scores indicated that the average patient in DELIVER shifted from experiencing severe headache-related life impact to moderate impact (HIT-6 total score), had clinically meaningful improvement in health-related quality of life (MSQ subscores), experienced much improvement in their most bothersome symptom (PI-MBS) and overall disease state (PGIC), and reported increased work productivity (WPAI:M). These findings are consistent with those of previous eptinezumab studies, which have demonstrated long-term reductions in disability and improvements in functioning and quality of life over periods of up to 2 years (PROMISE-1 [9], PROMISE-2 [11], PREVAIL [26]).
In this long-term study of eptinezumab, there was a low dropout rate, indicating tolerability, and TEAEs with an incidence of ≥ 1.5% were of similar nature to those most commonly reported in previous studies [4, 8,9,10,11,12,13]. Other phase 3b studies with anti-CGRP monoclonal antibodies in similar populations have also demonstrated high completion rates over shorter open-label extension studies. The completion rate in this study was 90.4% and consistent with findings from the LIBERTY study, in which 85% of patients completed 13 months of an open-label extension of the original 3-month double-blind study and 75% completed 25 months [24, 27]. Long-term treatment with eptinezumab in the real-world may improve persistence/adherence to a preventive medication and thereby lower burden/disability, improve function, and reduce presenteeism/absenteeism.
Limitations
The extension phase of the DELIVER trial lacked a placebo or active comparator arm, which may limit the interpretation of the results; however, dose-blinding was maintained for patients and investigators (but not for the sponsor) throughout the extension phase. Although the study was primarily conducted in Europe, the results are likely applicable to the US. Enrolled patients were predominantly White and female, limiting generalizability. Additional studies in broader patient populations are needed to confirm that observed benefits extend to these populations. DELIVER did, however, include older participants (up to and including 75 years of age) and those with comorbidities that were excluded in previous trials. The inclusion of these patients did not appear to be associated with any new safety concerns. Lastly, DELIVER did not allow for dose escalation or reduction; thus, the effects of changing dose levels during long-term treatment cannot be evaluated.
Conclusion
This long-term extension study highlights eptinezumab as an effective and well-tolerated long-term preventive migraine treatment option for adults with a history of 2–4 prior preventive treatment failures. This study had high completion rates and demonstrated tolerability and benefits sustained for up to 18 months across migraine endpoints, including reductions in frequency and severity of migraine, reductions in acute medication use, high responder rates, and patient-reported improvements in functioning, disease status, and health-related quality of life.
Availability of data and materials
In accordance with EFPIA’s and PhRMA’s “Principles for Responsible Clinical Trial Data Sharing” guidelines, Lundbeck is committed to responsible sharing of clinical trial data in a manner that is consistent with safeguarding the privacy of patients, respecting the integrity of national regulatory systems, and protecting the intellectual property of the sponsor. The protection of intellectual property ensures continued research and innovation in the pharmaceutical industry. Deidentified data are available to those whose request has been reviewed and approved through an application submitted to https://www.lundbeck.com/global/our-science/clinical-data-sharing.
Abbreviations
- CGRP:
-
Calcitonin gene-related peptide
- HIT-6:
-
6-item Headache Impact Test
- MHDs:
-
Monthly headache days
- MMDs:
-
Monthly migraine days
- MSQ:
-
Migraine-Specific Quality of Life questionnaire
- PGIC:
-
Patient Global Impression of Change
- PI-MBS:
-
Patient-identified most bothersome symptom
- TEAEs:
-
Treatment-emergent adverse events
- WPAI:M:
-
Work Productivity and Impairment, adapted for Migraine
References
Ashina M, Katsarava Z, Do TP, Buse DC, Pozo-Rosich P, Ozge A et al (2021) Migraine: epidemiology and systems of care. Lancet 397(10283):1485–1495. https://doi.org/10.1016/S0140-6736(20)32160-7
Linde M, Gustavsson A, Stovner LJ, Steiner TJ, Barre J, Katsarava Z et al (2012) The cost of headache disorders in Europe: the Eurolight project. Eur J Neurol 19(5):703–711. https://doi.org/10.1111/j.1468-1331.2011.03612.x
Eigenbrodt AK, Ashina H, Khan S, Diener HC, Mitsikostas DD, Sinclair AJ et al (2021) Diagnosis and management of migraine in ten steps. Nat Rev Neurol 17(8):501–514. https://doi.org/10.1038/s41582-021-00509-5
Ashina M, Lanteri-Minet M, Pozo-Rosich P, Ettrup A, Christoffersen CL, Josiassen MK et al (2022) Safety and efficacy of eptinezumab for migraine prevention in patients with two-to-four previous preventive treatment failures (DELIVER): a multi-arm, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol 21(7):597–607. https://doi.org/10.1016/S1474-4422(22)00185-5
Reuter U, Goadsby P, Lanteri-Minet M, Wen S, Hours-Zesiger P, Ferrari M et al (2018) Efficacy and tolerability of erenumab in patients with episodic migraine in whom two-to-four previous preventive treatments were unsuccessful: a randomised, double-blind, placebo-controlled, phase 3b study. Lancet 392(10161):2280–2287
Ferrari MD, Diener HC, Ning X, Galic M, Cohen JM, Yang R et al (2019) Fremanezumab versus placebo for migraine prevention in patients with documented failure to up to four migraine preventive medication classes (FOCUS): a randomised, double-blind, placebo-controlled, phase 3b trial. Lancet 394(10203):1030–1040. https://doi.org/10.1016/S0140-6736(19)31946-4
Mulleners WM, Kim BK, Lainez MJA, Lanteri-Minet M, Pozo-Rosich P, Wang S et al (2020) Safety and efficacy of galcanezumab in patients for whom previous migraine preventive medication from two to four categories had failed (CONQUER): a multicentre, randomised, double-blind, placebo-controlled, phase 3b trial. Lancet Neurol 19(10):814–825. https://doi.org/10.1016/S1474-4422(20)30279-9
Ashina M, Saper J, Cady R, Schaeffler BA, Biondi DM, Hirman J et al (2020) Eptinezumab in episodic migraine: a randomized, double-blind, placebo-controlled study (PROMISE-1). Cephalalgia 40(3):241–254. https://doi.org/10.1177/0333102420905132
Smith TR, Janelidze M, Chakhava G, Cady R, Hirman J, Allan B et al (2020) Eptinezumab for the Prevention of episodic migraine: sustained Effect through 1 year of treatment in the PROMISE-1 study. Clin Ther. 42(12):2254–65e3. https://doi.org/10.1016/j.clinthera.2020.11.007
Lipton RB, Goadsby PJ, Smith J, Schaeffler BA, Biondi DM, Hirman J et al (2020) Efficacy and safety of eptinezumab in patients with chronic migraine: PROMISE-2. Neurology 94(13):e1365–e1377. https://doi.org/10.1212/WNL.0000000000009169
Silberstein S, Diamond M, Hindiyeh NA, Biondi DM, Cady R, Hirman J et al (2020) Eptinezumab for the prevention of chronic migraine: efficacy and safety through 24 weeks of treatment in the phase 3 PROMISE-2 (Prevention of migraine via intravenous ALD403 safety and efficacy-2) study. J Headache Pain 21(1):120. https://doi.org/10.1186/s10194-020-01186-3
Dodick DW, Lipton RB, Silberstein S, Goadsby PJ, Biondi D, Hirman J et al (2019) Eptinezumab for prevention of chronic migraine: a randomized phase 2b clinical trial. Cephalalgia 39(9):1075–1085. https://doi.org/10.1177/0333102419858355
Kudrow D, Cady RK, Allan B, Pederson SM, Hirman J, Mehta LR et al (2021) Long-term safety and tolerability of eptinezumab in patients with chronic migraine: a 2-year, open-label, phase 3 trial. BMC Neurol 21(1):126. https://doi.org/10.1186/s12883-021-02123-w
Baker B, Shen V, Cady R, Ettrup A, Larsen F (2022) Eptinezumab administered intravenously, subcutaneously, or intramuscularly in healthy subjects and/or patients with migraine: early development studies. Cephalalgia Rep 5:25158163221131330. https://doi.org/10.1177/25158163221131326
Goadsby PJ, Barbanti P, Lambru G, Ettrup A, Christoffersen CL, Josiassen MK et al (2023) Eptinezumab improved patient-reported outcomes and quality of life in patients with migraine and prior preventive treatment failures. Eur J Neurol 30(4):1089–1098. https://doi.org/10.1111/ene.15670
Barbanti P, Goadsby PJ, Lambru G, Ettrup A, Christoffersen CL, Josiassen MK et al (2022) Effects of eptinezumab on self-reported work productivity in adults with migraine and prior preventive treatment failure in the randomized, double-blind, placebo-controlled DELIVER study. J Headache Pain 23(1):153. https://doi.org/10.1186/s10194-022-01521-w
Arnold M (2018) Headache classification committee of the international headache society (IHS) the international classification of headache disorders. Cephalalgia 38(1):1–211. https://doi.org/10.1177/0333102417738202
Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA et al (2011) The Columbia-suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 168(12):1266–1277. https://doi.org/10.1176/appi.ajp.2011.10111704
Sacco S, Amin F, Ashina M, Bendtsen L, Deligianni C, Gil-Gouveia R et al. (2022) European Headache Federation guideline on the use of monoclonal antibodies targeting the calcitonin gene related peptide pathway for migraine prevention – 2022 update. J Headache Pain. 23(1). https://doi.org/10.1186/s10194-022-01431-x
Sacco S, Lampl C, van den Maassen A, Caponnetto V, Braschinsky M, Ducros A et al (2021) Burden and attitude to resistant and refractory migraine: a survey from the European Headache Federation with the endorsement of the European Migraine and Headache Alliance. J Headache Pain 22:39. https://doi.org/10.1186/s10194-021-01252-4
Benemei S, Bentivegna E, Martelletti P (2022) Positioning the new drugs for migraine. Expert Opin Drug Metab Toxicol 18(1):1–3. https://doi.org/10.1080/17425255.2022.2049236
(2022) Vyepti [package insert]. Bothell, WA, United States, Lundbeck Seattle BioPharmaceuticals, Inc. https://www.lundbeck.com/content/dam/lundbeck-com/americas/unitedstates/products/neurology/vyepti_pi_us_en.pdf.
(2021) Vyepti [information for the patient]. Copenhagen, Denmark, Lundbeck H/S. https://www.medicines.org.uk/emc/files/pil.13243.pdf.
Ferrari MD, Reuter U, Goadsby PJ, Paiva da Silva Lima G, Mondal S, Wen S et al (2022) Two-year efficacy and safety of erenumab in participants with episodic migraine and 2–4 prior preventive treatment failures: results from the LIBERTY study. J Neurol Neurosurg Psychiatry 93(3):254–262. https://doi.org/10.1136/jnnp-2021-327480
Schwedt TJ, Buse DC, Argoff CE, Reed ML, Fanning KM, Hussar CR et al (2021) Medication overuse and headache burden: results from the CaMEO study. Neurol Clin Pract 11(3):216–226. https://doi.org/10.1212/CPJ.0000000000001037
Blumenfeld A, Ettrup A, Hirman J, Ebert B, Cady R (2022) Long-term reductions in disease impact in patients with chronic migraine following preventive treatment with eptinezumab. BMC Neurol 22(1):251. https://doi.org/10.1186/s12883-022-02774-3
Goadsby PJ, Reuter U, Lanteri-Minet M, Paiva da Silva Lima G, Hours-Zesiger P, Fernandes C et al (2021) Long-term efficacy and safety of Erenumab: results from 64 weeks of the LIBERTY Study. Neurology 96(22):e2724–e2735. https://doi.org/10.1212/WNL.0000000000012029
Acknowledgements
The authors thank participating patients, families, and study sites. Medical writing support was provided by Mary Tom, PharmD, Julia L. Jones, PhD, and Nicole Coolbaugh, CMPP, of The Medicine Group, LLC (New Hope, PA, United States) in accordance with Good Publication Practice guidelines.
Funding
The clinical trial and publication support were funded by H. Lundbeck A/S, Copenhagen, Denmark. In collaboration with the academic authors, the sponsor participated in the design and conduct of the study and in the collection, management, analysis, and interpretation of the data. The preparation, review, and approval of the manuscript was undertaken by all authors and by a professional medical writer and editor funded by the sponsor. Statistical analyses were performed by Cecilie Laurberg Christoffersen, an employee of H. Lundbeck A/S, with oversight by MKJ. All authors and H. Lundbeck A/S prepared, reviewed, and approved the final version of the manuscript and made the decision to submit the manuscript for publication. The sponsor did not have the right to veto publication or to control the decision regarding to which journal the paper was submitted.
Author information
Authors and Affiliations
Contributions
All authors had full access to the study data and take responsibility for the integrity of the data. BS and MKJ contributed to the conception or design of the study. BS and MKJ contributed to obtaining funding. AG and MA were study investigators, contributing to the acquisition of data. MKJ provided oversight for the statistical analyses. All authors contributed to the interpretation of data, were involved in drafting the manuscript, and critically reviewed the manuscript for important intellectual content. All authors provided final approval of the manuscript content for submission and had final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved at each study site by the corresponding ethics committee or institutional review board. All clinical work was conducted in compliance with current Good Clinical Practices as defined in the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use guidelines, local regulatory requirements, and the Declaration of Helsinki policy statement. All patients enrolled in the trial provided written informed consent prior to trial participation.
Consent for publication
Not applicable.
Competing interests
Messoud Ashina reports receiving personal fees from AbbVie, Amgen, Eli Lilly, GlaxoSmithKline, Lundbeck, Novartis, Pfizer, and Teva Pharmaceuticals during the conduct of the study. He reported serving as associate editor of Cephalalgia, associate editor of The Journal of Headache and Pain, and associate editor of Brain.
Stewart J. Tepper reports grants for research (no personal compensation): Allergan/AbbVie, Amgen, Eli Lilly, Lundbeck, Neurolief, Novartis, Satsuma, Zosano. Consultant and/or Advisory Boards (honoraria): Aeon, Allergan/AbbVie, Alphasights, Amgen, Aruene, Atheneum, Axsome Therapeutics, Becker Pharmaceutical Consulting, BioDelivery Sciences International, Biohaven, ClearView Healthcare Partners, ClickTherapeutics, CoolTech, CRG, Decision Resources, Defined Health, DRG, Eli Lilly, ExpertConnect, FCB Health, Fenix, GLG, Guidepoint Global, Health Advances, Health Science Communications, HMP Communications, Impel, Initiatior Pharma, InteractiveForums, Keyquest, Ki Health Partners, Krog and Partners, Lundbeck, M3 Global Research, Magnolia Innovation, MJH Holdings, Miravo Healthcare, Neurofront Therapeutics, Neurolief, Novartis, P Value Communications, Pain Insights, Inc., Palion Medical, Pfizer, Pulmatrix, Putnam Associates, Rehaler, SAI MedPartners, Satsuma, Slingshot Insights, Spherix Global Insights, Strategy Inc., Synapse Medical Communication, System Analytic, Taylor and Francis, Tegus, Teva, Theranica, Tremeau, Trinity Partners, Unity HA, Vial, XOC, Zosano. Salary: Dartmouth-Hitchcock Medical Center and Thomas Jefferson University. CME honoraria: American Academy of Neurology, American Headache Society, Annenberg Center for Health Sciences, Catamount Medical Education, Diamond Headache Clinic, Forefront Collaborative, Haymarket Medical Education, HMP Global, Medical Education Speakers Network, Medical Learning Institute Peerview, Migraine Association of Ireland, Miller Medical Education, National Association for Continuing Education, North American Center for CME, The Ohio State University, Physicians’ Education Resource, PlatformQ Education, Primed, Vindico Medical Education, and WebMD/Medscape.
Astrid Gendolla has received honoraria for advisory boards and lectures from Novartis, Lilly, TEVA, Allergan/AbbVie, Mundipharma, Stada Arzneimittel, Grünenthal, Hormosan Pharma, Perfood, Lundbeck, and Pfizer within the past 3 years.
Bjørn Sperling, Anders Ettrup and Mette Krog Josiassen are current employees of H. Lundbeck A/S. Bjørn Sperling and Mette Krog Josiassen own stock in H. Lundbeck A/S.
Amaal J. Starling has received consulting fees from AbbVie, Allergan, Amgen, Axsome Therapeutics, eNeura, Everyday Health, Lundbeck, Med-IQ, Medscape, Miller Medical, Satsuma, and WebMD within the past 3 years.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Methods.
Patient-reported outcomes. Supplemental Table 1. Monthly migraine days and patient-reported outcomes (MMRM; efficacy analysis set). Supplemental Figure 1. Mean PI-MBS score (MMRM; efficacy analysis set). Supplemental Figure 2. Mean PGIC score (MMRM; efficacy analysis set). Supplemental Figure 3. Mean change from baseline in EQ-5D-5L VAS score (MMRM; efficacy analysis set).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ashina, M., Tepper, S.J., Gendolla, A. et al. Long-term effectiveness of eptinezumab in patients with migraine and prior preventive treatment failures: extension of a randomized controlled trial. J Headache Pain 24, 155 (2023). https://doi.org/10.1186/s10194-023-01688-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-023-01688-w