Abstract
Background
Resting-state functional connectivity (FC) MRI has widely been used to understand migraine pathophysiology and to identify an imaging marker of the disorder. Here, we review what we have learned from FC studies.
Methods
We performed a literature search on the PubMed website for original articles reporting data obtained from conventional resting-state FC recording in migraine patients compared with healthy controls or during and outside of migraine attacks in the same patients.
Results
We found 219 articles and included 28 in this review after screening for inclusion and exclusion criteria. Twenty-five studies compared migraine patients with healthy controls, whereas three studies investigated migraine patients during and outside of attacks. In the studies of interictal migraine more alterations of more than 20 FC networks (including amygdala, caudate nucleus, central executive, cerebellum, cuneus, dorsal attention network, default mode, executive control, fronto-parietal, hypothalamus, insula, neostriatum, nucleus accumbens, occipital lobe, periaqueductal grey, prefrontal cortex, salience, somatosensory cortex I, thalamus and visual) were reported. We found a poor level of reproducibility and no migraine specific pattern across these studies.
Conclusion
Based on the findings in the present review, it seems very difficult to extract knowledge of migraine pathophysiology or to identify a biomarker of migraine. There is an unmet need of guidelines for resting-state FC studies in migraine, which promote the use of homogenous terminology, public availability of protocol and the a priori hypothesis in line with for instance randomized clinical trial guidelines.
Similar content being viewed by others
Introduction
Pathophysiology of migraine is complex and, so far, no biomarker for any of the phases of this cyclic disease exists. During the last decade, advanced neuroimaging modalities are increasingly used to understand migraine pathophysiology and disease mechanisms in the search for imaging markers of migraine. An often-used imaging technique is the resting-state or the so-called functional connectivity (FC) magnetic resonance imaging (fMRI), which has been applied in increasing number of migraine studies, since the first paper was published in 2011 [1]. Ideally, resting-state FC studies may be used to unveil migraine mechanisms.
The migraine resting-state literature is often analyzed and presented in several different ways, which makes it hard to compare results across studies, and findings are at times difficult to understand and are rarely reproduced. Thus, definitive imaging biomarkers for migraine have still not been identified limiting the usefulness and applicability of FC data.
Still, several well-performed resting-state FC studies and reviews [2] are available but a systematic review of the consistency of findings is missing. In the present review, we wish to provide an overview of all published conventional resting-state FC studies and discuss what we have learned so far based on FC findings.
Methods
Literature search
Two authors (JMH and FMA) performed search on the PubMed.com website to identify all original articles with resting-state FC data in migraine patients. The literature search was finalized on Pubmed.com September 20th, 2018. We used the following search terms: #1 resting state fMRI and migraine, #2 functional connectivity and migraine, and #3 functional connectivity fMRI and migraine. The search was restricted to human studies published in English language within 10 years, up to September 20th, 2018. Reviews, pediatric studies, case-reports, all other headache diagnoses and letters were excluded. We also assessed reference lists of the found articles for additional relevant studies. Moreover, we excluded all studies that did not use conventional resting-state analysis but other modalities, e.g. functional connectivity density, Granger causality, amplitude of low-frequency fluctuations, and regional homogeneity. Articles, in which the method was not properly described or if data on the comparison to a non-headache control group was not available were also excluded (expect if migraine attacks were compared to an interictal phase). Finally, studies testing treatment effect were also excluded. These exclusion criteria were chosen to include comparable studies in this review.
Data extraction
To screen for inclusion and exclusion criteria, the senior authors (JMH and FMA) assessed all abstracts found in the initial search. The selected studies were then sent to the co-authors (KS, WSvH, DD, AP, AS, BMI, EB, IS, LDA, and LF) who then read the text and extracted further information, i.e. origin of study, study population, method and main findings.
Resting-state functional connectivity MRI
The imaging method is based on blood-oxygen-level dependent (BOLD) recordings of the resting brain (i.e. the person lying in the MRI scanner is relaxing with closed eyes, but not sleeping). Every voxel in the obtained image of the brain emits a signal with a specific frequency. The higher the degree of synchronization of signal frequency between two different voxels, the more functional connected are these voxels, and vice versa. Brain areas displaying a particular level of similarity represent a functional connectivity network. Thus, all areas in the brain are more or less functionally connected to each other. The use of this method depends on the change in the functional connectivity between areas in a network, when measured in two different conditions or population samples.
Results
Our search strategy was finalized September 20th, 2018 and resulted in a total of 219 results, including 94 unique results, from which following were excluded: 15 reviews, 12 stimulation studies, nine non-conventional FC modalities, six examining effect of treatment (acupuncture), five non-migraine studies, five non-FC studies, four non-original articles, one pediatric study, and one study was retracted. Further eight studies were excluded because the method was not properly described or lack of a non-headache control group. One study was subsequently included from the reference lists. We ended up with a total of 28 studies, including 25 during the interictal phase (Table 1) and three during the ictal phase (Table 2) of migraine (Fig. 1). The studies were published between 2011 and 2017 and originated from five different countries, including China = 11; USA = 6; Italy = 6; Denmark = 4; Taiwan = 1.
Interictal migraine versus non-headache controls
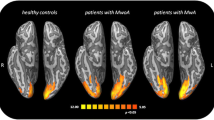
Twenty-five published studies reported data comparing interictal migraine with non-migraine non-headache controls. In 12 studies a migraine without aura (MO) population was examined, while pure migraine with aura (MA) was only investigated in a single study. In four studies, data for both MA and MO groups were reported separately, whereas mixed results were reported in the remaining eight studies.
When comparing migraine patient to controls, the functional connectivity was changed within or with a number of different networks or seed areas: periaqueductal gray network [1, 23], left [3, 7] dorsal [5] and right [3, 25] anterior cingulate cortex, fronto-parietal-network [4], right occipital lobe [5], left medial [5] and bilateral [7] prefrontal cortex, right cerebellum [5], brainstem [5], bilateral central executive network [6, 20], left [16] salience network [6, 20], default mode network [6, 8, 14, 15, 20, 21], right thalamus [7], right [7] and anterior [9] insula, amygdala [9, 10, 24], bilateral caudate [11], right nucleus accumbens [11], hypothalamus [12], right executive control network [13], left dorsal attention network [16], right cuneus [16], visual network [17], marginal division of neostriatum [18], primary visual cortex [19], primary auditory cortex [19] and bilateral primary somatosensory cortex [26]. All areas with abnormal connectivity to the above-mentioned networks are shown in Table 1 and Additional file 1 and Fig. 2.
Ictal migraine versus non-headache controls
Three conventional resting-state FC studies (one MA and two MO) have been published during compared to outside of migraine attacks. Following networks or areas showed altered connectivity during the attack versus outside of the attack: salience network [27], somatosensory network [27], default mode network [27], left pons [28] and right thalamus [29]. All areas with abnormal connectivity to the above-mentioned networks and areas are shown in Table 2.
Discussion
Based on this first systematic review of isolated conventional FC studies in migraine, we report that several areas and networks throughout the brain, brainstem and cerebellum showed altered connectivity in interictal and ictal migraine studies.
The findings are very diverse, with change in FC in many area thought to relevant for migraine as well as several other areas. The fact that almost all published studies report changes to some degree in all areas studied makes it difficult to gather the results into a coherent model, of specific activation patterns of activation in migraine.
All included studies (Tables 1 and 2) shared many characteristics; they used a 3 T MRI scanner, same type of patients (either MA or MO according to the International Classification of Headache Disorders criteria) and controls and in addition analyzed data using almost similar approaches (ICA or seed-based) in either the FSL or MATLAB-based software packages. Seed-based analysis can be affected by the chosen seed. Alterations in the default mode network (DMN) is most frequently reported. However, selection of different seed coordinates for DMN could potentially be the reason why FC changes in the DMN are different across studies. The strength of ICA is that it is independent of seed selection and more reproducible findings should be expected. The ICA-approach has been used in 10 studies and even in these studies different findings were reported.
Migraine is a heterogeneous disorder (with different disease duration, attack frequency, co-morbidity, effect of treatment, presence of aura), which might cause variation in results between studies. We did, however, only include studies where headache was diagnosed according to strict and uniform International Classification of Headache Disorders criteria.
In recent resting-state fMRI studies supplementary analyses like the Granger causality [30,31,32] have been introduced to investigate if FC changes can be linked to migraine phenotypes in the examined populations, but even here findings cannot be reproduced. As it is clear from Additional file 1 the findings are scattered and show very little overlap (Additional file 1). Moreover, none of the reported FC changes may be specific for migraine as other studies reported similar or exact same network changes in several other conditions, including fibromyalgia [33], Parkinsonian syndromes [34, 35] altered consciousness states [36], systemic lupus [37] and chronic hepatitis C virus infection [38]. Thus, it can be suspected that this FC method is at all not reproducible, which may be due to lack of sensitivity and specificity. Furthermore, to the best of our knowledge no sample size or power calculation guidelines are available for resting-state FC, with the consequence that a meaningful sample size for a resting-state FC study remains unknown. To avoid spurious findings, it would be useful to consider either sharing of data or joining patients in multicenter studies to allow for better and more reproducible studies.
As is already the norm for clinical trials, FC studies should be based on publically available protocols. It is also noteworthy that since very few studies report “negative results” or no changes in FC, primary endpoints should be chosen before initiating studies, as is already the case for randomized clinical trials (RCT). The fact that few (if any) results are reproducible, strongly suggest that stricter methodological guidelines for FC studies are warranted.
Almost half of the presented studies included only MO patients which gives a total sum of 348 MO patients, where 120 MA patients can be calculated in our tables. The FC method may be useful for the study of specific sub-types of migraine if these are clearly selected beforehand, preferable based on a calculation of the necessary number of patients, and with a clear hypothesis to be tested.
The FC method is very versatile and may potentially help improve our understanding of underlying disease mechanisms and even define biomarkers or migraine. Based on this systematic review, we suggest that the current lack of uniform study design, a priori hypothesis and diverse analyses and terminology makes it difficult to apply the available data for a coherent understanding of migraine.
Conclusions
Imaging, including FC studies could potentially help improve our understanding of underlying disease mechanisms, but so far no reproducible biomarkers of migraine have been identified. Future FC studies should either pool existing data to extract information about sub-phenotypes of migraine patients or follow guidelines similar to RCT guidelines in case of design of new FC studies.
Availability of data and materials
All included references in the present review article are available on the Internet.
Abbreviations
- ACC:
-
Anterior cingulate cortex
- CEN:
-
Central executive network
- DAN:
-
Dorsal attention network
- DMN:
-
Default mode network
- ECN:
-
Executive control network
- FC:
-
Functional connectivity
- fMRI:
-
Functional magnetic resonance imaging
- FPN:
-
Fronto-parietal cortex
- FSL:
-
FMRIB Software Library
- ICA:
-
Independent component analysis
- MA:
-
Migraine with aura
- MdNS:
-
Marginal division of neostriatum
- MO:
-
Migraine without aura
- MOH:
-
Medication overuse headache
- PAG:
-
Periaqueductal gray
- PFC:
-
Prefrontal cortex
- RCT:
-
Randomized clinical trials
- S1:
-
Primary somatosensory cortex
- SMN:
-
Sensorimotor network
- SN:
-
Salience network
- VN:
-
Visual network
References
Mainero C, Boshyan J, Hadjikhani N (2011) Altered functional magnetic resonance imaging resting-state connectivity in periaqueductal gray networks in migraine. Ann Neurol 70:838–845
Schwedt TJ, Chiang CC, Chong CD, Dodick DW (2015) Functional MRI of migraine. Lancet Neurol 14:81–91
Yuan K, Qin W, Liu P, Zhao L, Yu D, Zhao L, Dong M, Liu J, Yang X, von Deneen KM, Liang F, Tian J (2012) Reduced fractional anisotropy of corpus callosum modulates inter-hemispheric resting state functional connectivity in migraine patients without aura. PLoS One 7:e45476
Russo A, Tessitore A, Giordano A, Corbo D, Marcuccio L, De Stefano M, Salemi F, Conforti R, Esposito F, Tedeschi G (2012) Executive resting-state network connectivity in migraine without aura. Cephalalgia 32:1041–1048
Jin C, Yuan K, Zhao L, Zhao L, Yu D, von Deneen KM, Zhang M, Qin W, Sun W, Tian J (2013) Structural and functional abnormalities in migraine patients without aura. NMR Biomed 26:58–64
Xue T, Yuan K, Zhao L, Yu D, Zhao L, Dong T, Cheng P, von Deneen KM, Qin W, Tian J (2012) Intrinsic brain network abnormalities in migraines without aura revealed in resting-state fMRI. PLoS One 7:e52927
Xue T, Yuan K, Cheng P, Zhao L, Zhao L, Yu D, Dong T, von Deneen KM, Gong Q, Qin W, Tian J (2013) Alterations of regional spontaneous neuronal activity and corresponding brain circuit changes during resting state in migraine without aura. NMR Biomed 26:1051–1058
Tessitore A, Russo A, Giordano A, Conte F, Corbo D, De Stefano M, Cirillo S, Cirillo M, Esposito F, Tedeschi G (2013) Disrupted default mode network connectivity in migraine without aura. J Headache Pain 14:89
Schwedt TJ, Schlaggar BL, Mar S, Nolan T, Coalson RS, Nardos B, Benzinger T, Larson-Prior LJ (2013) Atypical resting-state functional connectivity of affective pain regions in chronic migraine. Headache 53:737–751
Hadjikhani N, Ward N, Boshyan J, Napadow V, Maeda Y, Truini A, Caramia F, Tinelli E, Mainero C (2013) The missing link: enhanced functional connectivity between amygdala and visceroceptive cortex in migraine. Cephalalgia 33:1264–1268
Yuan K, Zhao L, Cheng P, Yu D, Zhao L, Dong T, Xing L, Bi Y, Yang X, von Deneen KM, Liang F, Gong Q, Qin W, Tian J (2013) Altered structure and resting-state functional connectivity of the basal ganglia in migraine patients without aura. J Pain 14:836–844
Moulton EA, Becerra L, Johnson A, Burstein R, Borsook D (2014) Altered hypothalamic functional connectivity with autonomic circuits and the locus coeruleus in migraine. PLoS One 9:e95508
Tessitore A, Russo A, Conte F, Giordano A, De Stefano M, Lavorgna L, Corbo D, Caiazzo G, Esposito F, Tedeschi G (2015) Abnormal connectivity within executive resting-state network in migraine with aura. Headache 55:794–805
Zhang J, Su J, Wang M, Zhao Y, Yao Q, Zhang Q, Lu H, Zhang H, Wang S, Li GF, Wu YL, Liu FD, Shi YH, Li J, Liu JR, Du X (2016) Increased default mode network connectivity and increased regional homogeneity in migraineurs without aura. J Headache Pain 17:98
Coppola G, Di Renzo A, Tinelli E, Lepre C, Di Lorenzo C, Di Lorenzo G, Scapeccia M, Parisi V, Serrao M, Colonnese C, Schoenen J, Pierelli F (2016) Thalamo-cortical network activity between migraine attacks: insights from MRI-based microstructural and functional resting-state network correlation analysis. J Headache Pain 17:100
Niddam DM, Lai KL, Fuh JL, Chuang CY, Chen WT, Wang SJ (2016) Reduced functional connectivity between salience and visual networks in migraine with aura. Cephalalgia 36:53–66
Tedeschi G, Russo A, Conte F, Corbo D, Caiazzo G, Giordano A, Conforti R, Esposito F, Tessitore A (2016) Increased interictal visual network connectivity in patients with migraine with aura. Cephalalgia 36:139–147
Chen Z, Chen X, Liu M, Liu S, Shu S, Ma L, Yu S (2016) Altered functional connectivity of the marginal division in migraine: a resting-state fMRI study. J Headache Pain 17(1):89 Epub 2016 Sep 26. PubMed PMID: 27670428; PubMed Central PMCID: PMC5037100
Hodkinson DJ, Veggeberg R, Kucyi A, van Dijk KR, Wilcox SL, Scrivani SJ, Burstein R, Becerra L, Borsook D (2017) Cortico-cortical connections of primary sensory areas and associated symptoms in migraine. eNeuro 3. https://doi.org/10.1523/ENEURO.0163-16.2016
Androulakis XM, Krebs K, Peterlin BL, Zhang T, Maleki N, Sen S, Rorden C, Herath P (2017) Modulation of intrinsic resting-state fMRI networks in women with chronic migraine. Neurology 8(9):163–169
Lo Buono V, Bonanno L, Corallo F, Pisani LR, Lo Presti R, Grugno R, Di Lorenzo G, Bramanti P, Marino S (2017) Functional connectivity and cognitive impairment in migraine with and without aura. J Headache Pain 18:72
Hougaard A, Amin FM, Magon S, Sprenger T, Rostrup E, Ashina M (2015) No abnormalities of intrinsic brain connectivity in the interictal phase of migraine with aura. Eur J Neurol 22:702–e46
Chen Z, Chen X, Liu M, Liu S, Ma L, Yu S (2017) Disrupted functional connectivity of periaqueductal gray subregions in episodic migraine. J Headache Pain 18:36
Chen Z, Chen X, Liu M, Dong Z, Ma L, Yu S (2017) Altered functional connectivity of amygdala underlying the neuromechanism of migraine pathogenesis. J Headache Pain 18:7
Yu D, Yuan K, Luo L, Zhai J, Bi Y, Xue T, Ren X, Zhang M, Ren G, Lu X (2017) Abnormal functional integration across core brain networks in migraine without aura. Mol Pain 13:1744806917737461
Zhang J, Su J, Wang M, Zhao Y, Zhang QT, Yao Q, Lu H, Zhang H, Li GF, Wu YL, Liu YS, Liu FD, Zhuang MT, Shi YH, Hou TY, Zhao R, Qiao Y, Li J, Liu JR, Du X (2017) The sensorimotor network dysfunction in migraineurs without aura: a resting-state fMRI study. J Neurol 264:654–663
Amin FM, Hougaard A, Magon S, Asghar MS, Ahmad NN, Rostrup E, Sprenger T, Ashina M (2016) Change in brain network connectivity during PACAP38-induced migraine attacks: a resting-state functional MRI study. Neurology 86:180–187
Hougaard A, Amin FM, Larsson HB, Rostrup E, Ashina M (2017) Increased intrinsic brain connectivity between pons and somatosensory cortex during attacks of migraine with aura. Hum Brain Mapp 3(8):2635–2642
Amin FM, Hougaard A, Magon S, Sprenger T, Wolfram F, Rostrup E, Ashina M (2018) Altered thalamic connectivity during spontaneous attacks of migraine without aura: a resting-state fMRI study. Cephalalgia 38:1237–1244
Wang T, Zhan W, Chen Q, Chen N, Zhang J, Liu Q, He L, Zhang J, Huang H, Gong Q (2016) Altered resting-state ascending/descending pathways associated with the posterior thalamus in migraine without aura. Neuroreport 27:257–263
Ning Y, Zheng R, Li K, Zhang Y, Lyu D, Jia H, Ren Y, Zou Y (2018) The altered Granger causality connection among pain-related brain networks in migraine. Medicine (Baltimore) 97:e0102
Wang T, Chen N, Zhan W, Liu J, Zhang J, Liu Q, Huang H, He L, Zhang J, Gong Q (2015) Altered effective connectivity of posterior thalamus in migraine with cutaneous allodynia: a resting-state fMRI study with granger causality analysis. J Headache Pain 17:17
Napadow V, Harris RE (2014) What has functional connectivity and chemical neuroimaging in fibromyalgia taught us about the mechanisms and management of ‘centralized’ pain? Arthritis Res Ther 16:425
Wolters AF, van de Weijer SCF, Leentjens AFG, Duits AA, Jacobs HIL, Kuijf ML (2018) Resting-state fMRI in Parkinson’s disease patients with cognitive impairment: a meta-analysis. Parkinsonism Relat Disord S1353-8020(18):30550–30559
Filippi M, Sarasso E, Agosta F (2019) Resting-state functional MRI in Parkinsonian syndromes. Mov Disord Clin Pract 6:104–117
Heine L, Soddu A, Gömez F, Vanhaudenhuyse A, Tshibanda L, Thonnard M, Charland-Verville V, Kirsch M, Laureys S, Demertzi A (2012) Resting state networks and consciousness: alterations of multiple resting state networks connectivity in physiological, pharmacological, and pathological consciousness states. Front Psychol 3:295
Mikdashi JA (2016) Altered functional neuronal activity in neuropsychiatric lupus: a systematic review of the fMRI investigations. Semin Arthritis Rheum 45:455–462
Kharabian Masouleh S, Herzig S, Klose L, Roggenhofer E, Tenckhoff H, Kaiser T, Thöne-Otto A, Wiese M, Berg T, Schroeter ML, Margulies DS, Villringer A (2017) Functional connectivity alterations in patients with chronic hepatitis C virus infection: a multimodal MRI study. J Viral Hepat 24:216–225
Acknowledgements
Authors thank Prof. Paolo Martelletti for organizing this EHF-SAS working group.
Funding
The article-processing charges for the article has been sponsored by the European Headache Federation.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed equally. KS, WSvH, DD, AP, AS, BMI, EB, IS, LDA, and LF are junior fellows, while SS, JMH and FMA are senior fellows of EHF-SAS. All authors contributed with data interpretation, drafting, revision of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
KS has received personal fees, honoraria for lecturing or travel grants from TEVA, Novartis, Alder, Roche, and Allergan. SS has received personal fees, honoraria for lecturing or travel grants from Allergan, Eli Lilly, TEVA, and Novartis. FMA has participated in advisory boards and/or received personal fees, honoraria for lecturing or travel grants from Eli Lilly, TEVA, and Novartis. All authors (WSvH, DD, AP, AS, BMI, EB, IS, LDA, LF, and JMH) reports no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S2.
Schematic overview of regions with an altered functional connectivity to the examined networks throughout 25 studies of interictal migraine compared with healthy volunteers
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Skorobogatykh, K., van Hoogstraten, W.S., Degan, D. et al. Functional connectivity studies in migraine: what have we learned?. J Headache Pain 20, 108 (2019). https://doi.org/10.1186/s10194-019-1047-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-019-1047-3