Abstract
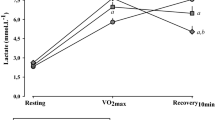
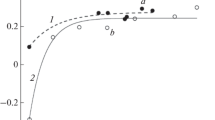
The aim of this work was to study the indicators of heart rate variability (HRV) under conditions of additional respiratory resistance (ARR) as a simulation of climbing to a height in young men with different types of autonomic regulation. The study involved 715 young men aged 19 to 24 years. HRV parameters were assessed by the method of variational pulsometry (BioMouse). Each subject underwent two tests lasting 5 min: background and under ARR conditions. An ETM 2.0 resistive mask was used to simulate climbing (ARR simulation) in three altitudes: 3000, 9000, and 18 000 feet. Each person performed only one test; the height of the lift was not reported to him. Based on the results of background testing, two groups were created: the optimal balance (OB) group—with balanced sympathetic and parasympathetic influences on HRV (stress index 25–100 c.u., VLF above 240 ms2) and the parasympathetic tone (PT) group—with a moderate predominance of parasympathetic (vagal) influences (stress index below 25 c.u., VLF above 500 ms2). During background testing, the OB group was characterized by higher values of the Baevsky indices (the vegetative balance index VBI, vegetative rhythm index VRI, and the indicator of the adequacy of regulatory processes ARPs) reflecting the predominance of sympathetic tone, and the PT group had higher values of the variational range of the duration of R–R intervals, RMSSD, SDNN, and pNN50%, which are considered markers of increased vagal tone, and the total power (TP) of the HRV spectrum. Under ARR conditions, without taking into account the height of the simulated rise, in the OB group, an increase in indicators correlating with vagal activity was revealed: the range of R–R intervals, RMSSD, SDNN, the HF band in the HRV spectrum, with a decrease in the Baevsky indices (VBI, VRI, ARP, and stress index). The increase in spectral measures of HRV associated with sympathetic activity (LF%) and TP reached the statistical significance level only when simulating an ascent to an altitude of 18 000 feet. In the PT group, the changes were oppositely directed: a decrease in correlates of vagal activity and an increase in sympathetic tone, regardless of the height of the lift. However, in both groups, the range of R–R intervals increased most at an altitude of 9000 feet, which is critical for the development of mountain sickness. Differences in the autonomic regulation of the cardiovascular system in young men determine the direction and severity of shifts in HRV indicators when simulating a rise to a height. In the OB group under ARR conditions, the indicators associated with vagal activity increase when a rise to insignificant heights was simulated; with an increase in the rise height, the parameters reflecting the sympathetic tone also increase. In the PT group, an expected increase in sympathetic tone was found at all altitudes.


Similar content being viewed by others
REFERENCES
Raven, P.B., Jackson, A.W., Page, K., et al., The physiological responses of mild pulmonary impaired subjects while using a “demand” respirator during rest and work, Am. Ind. Hyg. Assoc. J., 1981, vol. 42, no. 4, p. 247.
Middleton, J.D. and Lopes, H., Face masks in the Covid-19 crisis: caveats, limits, and priorities, BMJ, 2020, vol. 369, p. m2030.
Özdemir, L., Azizoğlu, M., and Yapıcı, D., Respirators used by healthcare workers due to the COVID-19 outbreak increase end-tidal carbon dioxide and fractional inspired carbon dioxide pressure, J. Clin. Anesth., 2020, vol. 66, p. 109901.
Segizbaeva, M.O. and Aleksandrova, N.P., Effect of the Elevation Training Mask on the functional outcomes of the respiratory muscles, Hum. Physiol., 2018, vol. 44, no. 6, p. 656. https://doi.org/10.1134/S0362119718060117
Porcari, J.P., Probst, L., Forrester, K., et al., Effect of wearing the Elevation Training Mask on aerobic capacity, lung function and hematological variables, J. Sports Sci. Med., 2016, vol. 15, p. 379.
Granados, J., Gillum, T.L., Castillo, W., et al., “Functional” respiratory muscle training during endurance exercise causes modest hypoxemia but overall is well tolerated, J. Strength Cond. Res., 2016, vol. 30, no. 3, p. 755.
Romero-Arenas, S., López-Pérez, E., Colomer-Poveda, D., and Márquez, G., Oxygenation responses while wearing the elevation training mask during an incremental cycling test, J. Strength Cond. Res., 2021, vol. 35, no. 7, p. 1897.
Gáspari, A.F., Carvalho, L., Teodoro, C.L., et al, Is Elevation Training Mask a strategy to increase lactate clearance through respiratory muscle loading? J. Strength Cond. Res., 2018, vol. 32, no. 9. e12
Breslav, I.S. and Nozdrachev, A.D., Respiration: visceral and behavioral aspects, Usp. Fiziol. Nauk, 2007, vol. 38, no. 2, p. 26.
Erkudov, V.O. and Pugovkin, A.P., Effects of additional respiratory resistance in adolescents with increased sympathetic tone, Patogenez, 2019, vol. 17, no. 1, p. 82.
Pankova, N.B., Functional tests for the assessment of the healthy people state using heart rate variability, Ross. Fiziol. Zh. im. I. M. Sechenova, 2013, vol. 99, no. 6, p. 682.
Jung, H.C., Lee, N.H., John, S.D., and Lee, S., The elevation training mask induces modest hypoxaemia but does not affect heart rate variability during cycling in healthy adults, Biol. Sport, 2019, vol. 36, no. 2, p. 105.
Byalovsky, Yu.Yu. and Bulatetsky, S.V., The mechanisms of general adaptation syndrome: influence of increased respiratory resistance, Sport. Med.: Nauka Prakt., 2016, vol. 6, no. 3, p. 29.
Hermand, E., Lhuissier, F.J., Pichon, A., et al., Exercising in hypoxia and other stimuli: heart rate variability and ventilatory oscillations, Life (Basel). 2021, vol. 11, no. 7, p. 625.
Baevsky, R.M., Bennett, B.S., Bungo, M.W., et al., Adaptive responses of the cardiovascular system to prolonged spaceflight conditions: assessment with Holter monitoring, J. Cardiovasc. Diagn. Proced., 1997, vol. 14, no. 2, p. 53.
Shlyk, N.I., Standards for variation range in RR-intervals at rest and in orthostasis in training of racing skiers with different types of regulatiion, Nauka Sport: Sovrem. Tendentsii, 2021, vol. 9, no. 4, p. 35.
Maksimov, A.L. and Averyanova, I.V., Informative markers of cardiohemodynamic state in young men with different types of autonomic regulation during submaximal bicycle exercise test, Hum. Physiol., 2019, vol. 45, no. 3, p. 283. https://doi.org/10.1134/S0362119719020051
Natarajan, A., Pantelopoulos, A., Emir-Farinas, H., and Natarajan, P., Heart rate variability with photoplethysmography in 8 million individuals: a cross-sectional study, Lancet Digit. Health, 2020, vol. 2, no. 12. e650
Baevsky, R.M., Kirillov, O.I., and Kletskin, S.Z., Matematicheskii analiz izmenenii serdechnogo ritma pri stresse (Mathematical Analysis of Changes in Heart Rate during Stress), Moscow: Nauka, 1984.
Heart rate variability: standards of measurement, physiological interpretation, and clinical use, Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology, Eur. Heart J., 1996, vol. 17, no. 3, p. 354.
Shaffer, F. and Ginsberg, J.P., An overview of heart rate variability metrics and norms, Front. Public Health, 2017, vol. 5, p. 258.
Shlyk, N.I., Sapozhnikova, E.N., Kirillova, T.G., and Semenov, V.G., Typological characteristics of the functional state of regulatory systems in schoolchildren and young athletes (according to heart rate variability data), Hum. Physiol. 2009, vol. 35, no. 6, p. 730.
Shlyk, N.I. and Zufarova, E.I., Normative values of heart rate variability for trial subjects between 16 and 21 years old with different prevalent types of autonomic heart regulation, Vestn. Udmurt. Univ., Ser. Biol. Nauki Zemle, 2013, no. 4, p. 96.
Billman, G.E., The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance, Front. Physio-l., 2013, vol. 4, p. 26.
Perini, R. and Veicsteinas, A., Heart rate variability and autonomic activity at rest and during exercise in various physiological conditions, Eur. J. Appl. Physiol., 2003, vol. 90, no. 3–4, p. 317.
La Rovere, M.T., Porta, A., Schwartz, P.J., Autonomic control of the heart and its clinical impact: a personal perspective, Front. Physiol., 2020, vol. 11, p. 582.
Ruffle, J.K., Hyare, H., Howard, M.A., et al., The autonomic brain: multi-dimensional generative hierarchical modelling of the autonomic connectome, Cortex, 2021, vol. 143, p. 164.
Valenza, G., Sclocco, R., Duggento, A., et al., The central autonomic network at rest: uncovering functional MRI correlates of time-varying autonomic outflow, NeuroImage, 2019, vol. 197, p. 383.
Usui, H. and Nishida, Y., The very low-frequency band of heart rate variability represents the slow recovery component after a mental stress task, PLoS One, 2017, vol. 12, no. 8, p. e0182611
Pankova, N.B., Arkhipova, E.N., and Alchinova, I.B., et al., Comparative analysis of methods for rapid assessment of the functional state of the cardiovascular system, Vestn. Vosstanov. Med., 2011, no. 6(46), p. 60.
Stuckless, T.J.R., Vermeulen, T.D., Brown, C.V., et al., Acute intermittent hypercapnic hypoxia and sympathetic neurovascular transduction in men, J. Physiol., 2020, vol. 598, no. 3, p. 473.
Mellor, A., Bakker-Dyos, J., OʼHara, J., et al., Smartphone-enabled heart rate variability and acute mountain sickness, Clin. J. Sport. Med., 2018, vol. 28, no. 1, p. 76.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
COMPLIANCE WITH ETHICAL STANDARDS
All procedures performed in studies involving human participants were in accordance with the biomedical ethics principles formulated in the 1964 Helsinki Declaration and its later amendments and approved by the local Ethics Committee of the Research Institute of General Pathology and Pathophysiology (Moscow), protocol no. 4 of September 2, 2019.
CONFLICT OF INTERESTS
The authors declare that they have no conflicts of interest.
INFORMED CONSENT
Each study participant provided a signed voluntary written informed consent after explanation of the potential risks and benefits, as well as the nature of the upcoming study, to him.
AUTHOR CONTRIBUTION
V.O. Erkudov, K.U. Rozumbetov, A.P. Pugovkin, and A.T. Matchanov developed the concept and design of the study and prepared the original text of the article. K.U. Rozumbetov and A.T. Matchanov collected the data. V.O. Erkudov, K.U. Rozumbetov, A.P. Pugovkin, A.T. Matchanov, and N.B. Pankova analyzed and interpreted the results. V.O. Erkudov and N.B. Pankova edited and approved the final version of the article.
Additional information
Translated by E. Babchenko
Rights and permissions
About this article
Cite this article
Erkudov, V.O., Rozumbetov, K.U., Pugovkin, A.P. et al. Typological Features of Autonomic Heart Rate Regulation during Imitation of a Rise to Altitude by Using Additional Respiratory Resistance. Hum Physiol 49, 393–401 (2023). https://doi.org/10.1134/S0362119723600078
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0362119723600078