Abstract
We examined occupational and industrial differences in lung, gastric, and colorectal cancer risk among Japanese men of working age (25–64 years) using the 2010 Japanese national survey data for occupation and industry-specific death rates. Poisson regression models were used to estimate the age-adjusted incident rate ratios by lung, gastric, and colorectal cancers, with manufacturing used as the referent occupation or industry. Unemployed Japanese men and those in manufacturing had an 8–11-fold increased risk of lung, gastric and colorectal cancer. The highest mortality rates for lung and colorectal cancer by occupation were “administrative and managerial” (by occupation) and “mining” (by industry). For gastric cancer, the highest mortality rate was “agriculture” (by occupation) and “mining” (by industry). By occupation; Japanese men in service occupations, those in administrative and managerial positions, those in agriculture, forestry and fisheries, and those in professional and engineering categories had higher relative mortality risks for lung, gastric, and colorectal cancers. By industry; mining, electricity and gas, fisheries, and agriculture and forestry had the higher mortality risks for those cancers. Unemployed men had higher mortality rates than men in any occupation and industry for all three cancers. Overall, this study suggests that for Japanese men, occupations and industries may be a key social determinant of health.
Similar content being viewed by others
Introduction
Lung, gastric, and colorectal cancer have now risen to become the leading three causes of cancer-related deaths among Japanese men1, and the Japanese government has therefore placed a high priority on further improving the cancer screening rate2. In order to maximize cancer prevention, the risk factors for these diseases warrant detailed investigation. Although tobacco use is the greatest risk factor for lung cancer; other factors such as age, radon exposure, environmental pollution, occupational exposure, sex, and pre-existing lung disease are also important contributors3. Risk factors for gastric cancer are known to include age, sex, tobacco smoking, radiation, and family history4; while risk factors for colorectal cancer include dietary and lifestyle factors such as lack of exercise, overeating, and eating red meat, processed meats, and perhaps; the consumption of refined carbohydrates5.
Occupationally-related hazards which contribute to the development of cancer represent an important avoidable cause of mortality6. Considerable evidence suggests that individuals working in coal and tin mining, metal processing (particularly steel and iron), and rubber manufacturing industries have increased risks of gastric cancer7,8. Occupational exposures play a significant role in lung cancer aetiology, and the risk of lung cancer is increased among workers employed in a number of industries and occupations such as aluminum production, coal production, painting and welding9. Previous studies have indicated increased risks of colorectal cancer risk within the Portland cement industry10, wood dust exposed workers11, and firefighters12.
Analysis of national datasets on occupational and industrial mortality contribute significantly to this endeavor because they incorporate data on either occupations or jobs and health outcomes over an entire population13. They are particularly useful in the assessment of diseases and injuries with high fatality rates; and also for diseases where fatality rates are lower. Occupation and industry classifications are commonly used as proxies for occupational exposure (post facto), to help identify and explore issues of worker morbidity and mortality from cancer14,15; particularly when this information is not available through other means.
For this study, we hypothesized that identifying occupations and industries with a higher risk of death due to lung, gastric and colorectal cancer would be a significant first step in elucidating some key social markers of health. In this regard, the Japanese Ministry of Health, Labour and Welfare produces an occupation-specific Vital Statistics Survey every 5 years16. The survey takes place in the same year as the national population census; with the government collecting information on occupations and industries to which deceased persons belonged at their time of death; and also records the cause of death from death certificates. Such data can potentially elucidate the magnitude of occupation and industry effects on health-related outcomes among working-age populations. To date, no studies have addressed occupational and industrial differences in lung, gastric, and colorectal cancer related deaths in Japan. The present study aimed therefore, to examine occupational and industry-related differences in lung, gastric, and colorectal cancer mortality rates among employed Japanese men aged 25 to 64 years.
Methods
Data sources
We obtained the most recent (2010) national dataset titles “Report of Vital Statistics: Occupational and Industrial Aspects” from the Japanese Ministry of Health, Labour, and Welfare. Occupation- and industry-specific death rates were calculated based on the 2010 national population census (also implemented at 5-year intervals on 1 October each year in Japan).
Measurements
Japanese death certificate data includes the underlying causes of death and is completed by physicians based on the sequences of events leading to death, and coded according to the International Classification of Diseases (ICD), 10th Revision17. Relevant codes for this study included lung cancer: C34.0–34.9, gastric cancer: C16.0–16.9, and colorectal cancer: CI8.0–18.9, C19, C20 and C21.0–C21.8. In the years that these statistics were collected in Japan, family members of deceased individuals were required to report the occupation and industry of the deceased person. Family members were given occupation and industry lists, and corresponding descriptions and definitions, and asked to select one occupational and one industry category. The occupation list included 11 occupations: administrative and managerial; professional; clerical; sales; services; security; agriculture, forestry and fisheries; manufacturing; transport; construction and mining; and carrying, cleaning and packaging. The industry list comprised 19 industries: agriculture; fisheries; mining; construction; manufacturing; electricity and gas; information; transport; wholesale and retail; finance; real estate and rental; research and professional services; accommodation and dining services; amusement services; education; medical and welfare; compound services; other service industries; and government. These categories are based on the International Standard Classification of Occupations18,19 and the International Standard Industrial Classification20,21. Detailed lists of occupations and industries used in Japanese national datasets have been published elsewhere22.
Statistical analysis
We examined data for Japanese men who were aged 25–64 years in 2010, grouped into 5-year age intervals. Death rates for lung, gastric, and colorectal cancer in each age group by the occupation and industry categories defined in the Japanese national census. The numbers of employees from the national census in 201023 was used as the denominator and the number of deaths as the numerator, to provide a Poisson distribution. We aggregated individual patient data in groups of industry and age to calculate the Poisson regression. Separate regression models estimated the incidence rate ratio (IRR) for lung, gastric and colorectal cancers in each occupation or industry category compared with the reference category of “manufacturing.” We then conducted separate regression models to estimate the IRR for lung, gastric, and colorectal cancers in each industry compared with the industry, “manufacturing”. Given that manufacturing has the largest number of categories, is traditionally the most advanced in taking occupational health measures, and also shares commonalities in both industry and occupation; manufacturing was selected as the reference category for this study.
Each occupation or industry model followed the same structure, as shown in the equation below. We included age, and the interaction term between the occupation or industry being tested and age, to allow for possible modifications of occupation or industry related effects at different ages. The logarithm of the expected number of lung, gastric or colorectal cancer deaths (Y) is a linear function of the logarithm of the exposed individuals (N), the occupation (or industry) being tested (Xi), age, and the interaction between age and occupation (or industry). Age was coded as 0 for the reference category “25–29 years”, and then 1, 2, 3, and so on for older age groups. In each occupation category model, Xi was coded as 0 for the “manufacturing” category and 1 for the category being compared in the model. In the industry models, i was coded as 0 for “manufacturing” and 1 for the industry being compared:

In this equation, exp(β0) estimates the rate in the occupation (or industry) reference group at age 25–29 years, exp(β1i) estimates the IRR between the occupation (or industry) being tested and the reference occupation (or industry) at age 25–29 years, exp(β2j) estimates the effect of age in the reference occupation (or industry), exp(β1i + β3i*Agej) estimates the IRR between the occupation (or industry) being tested and the reference occupation (or industry) at a given age group “j”. The interaction coefficient β3i allows modeling of a different effect due to occupation (or industry) by age. If the interaction coefficient was not significant, we re-estimated the model without the interaction term, and the effect of occupation (or industry) was captured by exp (β1i). Data were analyzed using STATA version 14 (StataCorp LP; College Station, TX, USA).
Results
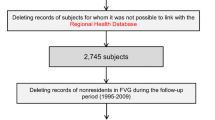
Tables 1 and 2 present the distribution of lung, gastric, and colorectal cancer mortality cases by occupation and industry in Japan. Lung cancer accounted for a total of 8,517 deaths among Japanese men aged 25–64 years during the study period. We excluded 1,269 men of unknown occupation category, and 1,440 men with no industry category; to give 7,248 lung cancer cases analyzed by occupation and 7,077 by industry. Gastric cancer accounted for a total of 6,319 deaths among Japanese men aged 25–64 years, from which we excluded 987 men without an occupation category, and 1,093 men without an industry category; resulting in 5,332 gastric cancer cases analyzed by occupation and 5,226 by industry. Colorectal cancer accounted for a total of 5,546 deaths among Japanese men aged 25–64 years, from which we excluded 838 men without an occupation category, and 908 men without an industry category, resulting in 4,708 colorectal cancer cases analyzed by occupation and 4,638 by industry.
Table 1 and Table 2 show the crude lung, gastric, and colon cancer mortality rates by occupation and industry, which are not age-adjusted. The largest number of deaths from lung, gastric, and colorectal cancers by occupational group was “professional and engineering”, and by industry; was “manufacturing”. The highest mortality rates for lung and colorectal cancer by occupation were “administrative and managerial” and by industry, “mining”. For gastric cancer, the highest mortality rate by occupation was “agriculture”, and by industry, “mining”. Unemployed men had higher mortality rates than men in any occupation and industry for all three cancers.
Table 3 indicates age-adjusted IRRs for lung, gastric, and colorectal cancers by occupation among Japanese males aged 25–64 years. When compared with the referent group (manufacturing), the unemployed, service, administrative and managerial, agriculture, forestry and fisheries and professional and engineering categories had higher relative mortality risks for these cancers. No interaction was found between age and occupation during this study.
Age-adjusted IRRs by industry for lung, gastric, and colorectal cancers are shown in Table 4. Mining, unemployed, electricity and gas, fisheries, and agriculture and forestry all had high risks for the three cancers. No interaction was found between age and industry.
Discussion
This study examined the risk of premature mortality for lung, gastric, and colorectal cancer by occupation and industry among Japanese men aged 25–64 years. We found that unemployed Japanese men had the highest mortality risk for lung, gastric and colorectal cancer. When compared with manufacturing, occupations and industries with a relatively higher mortality by lung, gastric, and colorectal cancer were: “service”; “administrative and managerial”; “agriculture and fisheries”; “construction and mining”; “electricity and gas”; and “professional and engineering.” Common multiple risk factors for death due to lung, gastric, and colorectal cancer included smoking, work stress, and lifestyle.
Unemployment might incur the highest mortality risk for lung, gastric, and colorectal cancer among Japanese working-aged men in this study. The interaction works both ways, however, and several possible mechanisms may explain the relatively higher unemployment rates among cancer patients when compared to manufacturing workers. One mechanism may be that cancer patients might quit spontaneously following diagnosis or be fired by their employer if they do not meet the worker’s requirement in terms of physical and mental capacity due to the physical and/or mental side effects of their cancer treatment. It has been previously demonstrated that a significant proportion of cancer survivors may continue to experience levels of physical, emotional, and social problems that are elevated relative to the general population, with these issues sometimes persisting after the treatment period has ended24. Because the participants in the current (mortality) study had died from their cancer, it is conceivable that their symptoms might have affected their fitness for work, thereby leading to at least some period of unemployment prior to their death.
Service occupations had the highest mortality risk for lung, gastric, and colorectal cancers (all three) among Japanese working-aged men. One explanation relates to the hypothesis25,26 that nighttime shift work may be associated with an increase in cancer risk. Workers in service occupations are often required to work at night, for example, as these industries have the highest number of night-shift workers in Japan (28.6%) when compared with manufacturing (11.3%)27. Results from two previous mortality studies28,29 among male shift workers provided the first suggestions that an increased cancer risk was probably associated with night-shift work.
In a previous Japanese study, male mortality rates among administrative, and professional and engineering workers (who are usually of a higher social demographic) was shown to increase between 2000 and 2005 - more so than for other occupations that mostly comprised workers from lower social demographics30; a change could be attributed to the economic depression in Japan at that time30. In the current study, we found that the administrative and professional-and-engineering categories had higher risks for lung, gastric, and colorectal cancer in 2010, than categories with lower social class. These results may be explained by high psychological distress of administrative and professional occupations in Japan. Proposed biological mechanisms for the adverse effects of psychological distress on cancer development include neuroendocrine alterations in the hypothalamus-pituitary-adrenal axis regulating glucocorticoid release and the sympathetic nervous system regulating catecholamine levels31,32. In Japan, companies downsized their organizations after the economic recession in the 1990s; and consequently, the share of managers in the labor market decreased from 3.8% in 1990 to 2.6% in 2010 33. These changes in work structure could increase the overall responsibilities and job demands of managers compared with manufacturing30, which may increase the risk of those cancers through high psychological distress rates among male administrative and professional-and-engineering workers.
Men who work directly with natural resources in environments that contain dusty air (e.g., mining, and electricity and gas), have been shown to have higher risks of these cancers in Western countries7,34, similar to the current study. One possible explanation is the continuous exposure to higher levels of dust and chemical substances faced by workers in these occupations when compared to manufacturing. In Japan, the rate of dusty workplace environments has been shown to be higher in mining (50.1%) than in manufacturing (21.5%)35. The rate of workplaces with carcinogenic chemical substances is also known to be higher (24.4%) than in manufacturing (12.5%)35. The International Agency for Research on Cancer for example, has reported that there is an association with exposure to silica, some silicates, coal dust and lung, stomach, and colorectal cancer36. Further research on the role of responsible agents in these environments is necessary.
Workers in primary industries and occupations (e.g., agriculture and fisheries) had the higher mortality risk for lung, gastric, and colorectal cancers (all three) compared to manufacturing workers. The smoking rates, cancer screening rates and implementation rates of no smoking policies in the workplace do not differ between agriculture and fisheries and manufacturing27. Small-scale and family businesses are more common in primary industry than in manufacturing. It is reasonable to assume that small sized and family companies may have insufficient human resources for health activities when compared with large companies. It is important to note that Japanese companies with 50 or more employees are required by the Occupational Health and Safety Law to employ an occupational health physician. Therefore, a lack of physician supervision may be one reason why Japanese workers in primary industries are at a higher risk than their counterparts in manufacturing.
The current study may have incurred some limitations which should be considered. Firstly, the Japanese dataset only contains aggregate data by occupation (industry) and age category rather than individual-level data, and could not therefore adjust for individual-level variables (such as smoking or other lifestyle factors) that might confound the results. Secondly, for the vital statistics for death (numerator), families of the deceased persons selected their occupations and industries, which could have potentially led to misclassification in this regard. Thirdly, “Manufacturing” is a broad category and does not specify what types of exposures these workers actually incurred. Fourth, because we could not obtain actual work histories, we could not exclude the possibility that some workers developed the disease which ultimately killed them in their first job, but were not diagnosed at the time. Fifth, because this study was based on 2010 data only, we could not confirm the changes between 2010 and earlier years. Sixth, as census data was collected by self-administered questionnaires, numerator-denominator bias might also have occurred, considering the different information sources for the numbers of deaths, occupations and industries37. Such bias may occur if the distribution of populations across industries and occupations differs between the two data sources. Finally, in our analysis we have not compared the rates of cancer in working men with the rates in the general population. Although such a method might provide some interesting results, the research question of our current study was to compare cancer rates between industries in Japan, and not with the general population. It should be noted that working aged men are a subgroup that probably differ from the general population in many substantial ways (other than age). Crucially this data was collected within the limitations explained above that could introduce some biased comparisons with the general population. However, these biases would have occurred equally across all industries studied, therefore limiting its overall effect.
Conclusion
In the current study, we identified differences of risks in mortality among lung, gastric, and colorectal cancer in Japanese working-age men, based on their occupations and industries. For Japanese men, occupations and industries may therefore be a key social determinant of health.
Additional Information
How to cite this article: Eguchi, H. et al. Lung, gastric and colorectal cancer mortality by occupation and industry among working-aged men in Japan. Sci. Rep. 7, 43204; doi: 10.1038/srep43204 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Foundation for Promotion of Cancer Research. Cancer statistics in Japan-2015 Available at: http://ganjoho.jp/reg_stat/statistics/stat/summary.html (Accessed: 18 Jan 2017). (in Japanese) (2016).
Ministry of Health, Labour and Welfare. Annual Health, Labour and Welfare Report Available at: http://www.mhlw.go.jp/english/wp/wp-hw9/index.html (Accessed: 18 Jan 2017) (2015).
de Groot, P. & Munden, R. F. Lung cancer epidemiology, risk factors, and prevention. Radiol Clin North Am 50, 863–876 doi: 10.1016/j.rcl.2012.06.006 (2012).
Karimi, P., Islami, F., Anandasabapathy, S., Freedman, N. D. & Kamangar, F. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomarkers Prev 23, 700–713 doi: 10.1158/1055-9965.EPI-13-1057 (2014).
Giovannucci, E. Modifiable risk factors for colon cancer. Gastroenterol Clin North Am 31, 925–943 (2002).
Takala, J. Eliminating occupational cancer. Ind Health 53, 307 doi: 10.2486/indhealth.53–307 (2015).
Raj, A., Mayberry, J. F. & Podas, T. Occupation and gastric cancer. Postgrad Med J 79, 252–258 (2003).
Uthman, O. A., Jadidi, E. & Moradi, T. Socioeconomic position and incidence of gastric cancer: a systematic review and meta-analysis. J Epidemiol Community Health 67, 854–860 doi: 10.1136/jech-2012-201108 (2013).
Cogliano, V. J. et al. Preventable exposures associated with human cancers. J Natl Cancer Inst 103, 1827–1839 doi: 10.1093/jnci/djr483 (2011).
Cohen, S. S., Sadoff, M. M., Jiang, X., Fryzek, J. P. & Garabrant, D. H. A review and meta-analysis of cancer risks in relation to Portland cement exposure. Occup Environ Med 71, 796–802 doi: 10.1136/oemed-2014-102193 (2014).
Llorente, J. L., Pérez-Escuredo, J., Alvarez-Marcos, C., Suárez, C. & Hermsen, M. Genetic and clinical aspects of wood dust related intestinal-type sinonasal adenocarcinoma: a review. Eur Arch Otorhinolaryngol 266, 1–7 doi: 10.1007/s00405-008-0749-y (2008)
Youakim, S. Risk of Cancer among Firefighters: A Quantitative Review of Selected Malignancies. Arch Environ Occup Health 61, 223–231 (2006).
Harris, E. C. et al. Trends in mortality from occupational hazards among men in England and Wales during 1979–2010. Occup Environ Med 73, 385–393 doi: 10.1136/oemed-2015-103336 (2016).
‘t Mannetje, A. & Pearce, N. Occupational mortality studies: still relevant in the 21st century. Occup Environ Med 67, 802–803 doi: 10.1136/oemed-2015-103336 (2010).
Robinson, C. F. et al. Overview of the National Occupational Mortality Surveillance (NOMS) system: Leukemia and acute myocardial infarction risk by industry and occupation in 30 US states 1985–1999, 2003–2004, and 2007. Am J Ind Med 58, 123–137 doi: 10.1002/ajim.22408 (2015).
Ministry of Health, Labour and Welfare. Report of Vital Statistics: Occupational and Industrial Aspects. Available at: http://www.mhlw.go.jp/english/database/db-hw/orvf/2010.html (Accessed: 18 Jan 2017) (2010).
World Health Organization. Manual of the International Statistical Classification of Diseases and Related Health Problems. Tenth Revision. Geneva, Switzerland: World Health Organization Available at: http://apps.who.int/classifications/icd10/browse/2016/en (Accessed: 18 Jan 2017) (1992).
International Labour Organization. International Standard Classification of Occupations. Available at: http://www.ilo.org/public/english/bureau/stat/isco/index.htm (Accessed: 18 Jan 2017) (2010).
Ministry of Internal Affairs and Communications. Standard Occupational Classification for Japan. Available at: http://www.soumu.go.jp/toukei_toukatsu/index/seido/shokgyou/kou_h21.htm (Accessed: 18 Jan 2017). (in Japanese) (2009).
Ministry of Internal Affairs and Communications. Japan Standard Industry Classification. Available at: http://www.soumu.go.jp/toukei_toukatsu/index/seido/sangyo/19index.htm (Accessed: 18 Jan 2017). (in Japanese) (2007).
United Nations, Statistics Division. International Standard Industrial Classification of All Economic Activities (ISIC) Revision 4. Available at: http://unstats.un.org/unsd/cr/registry/regcst.asp?Cl=27 (Accessed: 18 Jan 2017) (2008).
Wada, K., Eguchi, H., Prieto-Merino, D. & Smith, D. Occupational differences in suicide mortality among Japanese men of working age. J Affect Disord 190, 316–321, doi: 10.1016/j.jad.2015.10.032 (2016).
Statistics Bureau, Ministry of Internal Affaires and Communications. Population Census 2010. Available at: http://www.stat.go.jp/english/data/kokusei/2010/summary.htm (Accessed: 18 Jan 2017) (2010).
Smith, T. et al. The rationale, design, and implementation of the American Cancer Society’s studies of cancer survivors. Cancer 109, 1–12 (2007).
Blask, D. E. et al. Melatonin-depleted blood from premenopausal women exposed to light at night stimulates growth of human breast cancer xenografts in nude rats. Cancer Res 65, 11174–11184 (2005).
Pandi‐Perumal, S. R. et al. Melatonin. FEBS Journal 273, 2813–2838 (2006).
Ministry of Health, Labour and Welfare. Survey on State of Employees’ Health in 2012. Available at: http://www.mhlw.go.jp/toukei/list/h24-46-50.html (Accessed: 30 Nov 2016). (in Japanese) (2013).
Taylor, P. & Pocock, S. Mortality of shift and day workers 1956–68. Br J Ind Med 29, 201–207 (1972).
Rafnsson, V. & Gunnarsdottir, H. Mortality study of fertiliser manufacturers in Iceland. Br J Ind Med 47, 721–725 (1990).
Wada, K. et al. Trends in cause specific mortality across occupations in Japanese men of working age during period of economic stagnation, 1980-2005: retrospective cohort study. BMJ 344, e1191, doi: 10.1136/bmj.e1191 (2012).
Ross, K. Mapping pathways from stress to cancer progression. J Natl Cancer Inst 100, 914–917 doi: 10.1093/jnci/djn229 (2008).
McEwen, B. S., Gray, J. D. & Nasca, C. 60 years of neuroendocrinology: redefining neuroendocrinology: stress, sex and cognitive and emotional regulation. J Endocrinol 226, T67–T83 doi: 10.1530/JOE-15-0121 (2015).
Statistics Bureau, Ministry of Internal Affairs and Communications. Labour Force Survey 2016 Available at: http://www.stat.go.jp/data/roudou/longtime/03roudou.htm (Accessed: 18 Jan 2017). (in Japanese) (2016).
Burns, P. B. & Swanson, G. M. The Occupational Cancer Incidence Surveillance Study (OCISS): risk of lung cancer by usual occupation and industry in the Detroit metropolitan area. Am J Ind Med 19, 655–671 (1991).
Ministry of Health, Labour and Welfare. Survey on Labour Environment in 2013. Available at: http://www.mhlw.go.jp/toukei/list/h26-46-50.html (Accessed: 18 Jan 2017). (in Japanese) (2014).
International Agency for Research on Cancer. Silica, Some Silicates, Coal Dust and para-Aramid Fibrils. IARC monographs on the evaluation of carcinogenic risks to humans. Volume 68 Available at: http://monographs.iarc.fr/ENG/Monographs/vol68/ (Accessed: 30 Nov 2016) (1997).
Williams, G. M., Najman, J. M. & Clavarino, A. Correcting for numerator/denominator bias when assessing changing inequalities in occupational class mortality, Australia 1981–2002. Bull World Health Organ 84 (2006).
Acknowledgements
This work was supported by the Japan Society for the Promotion of Science, KAKENHI Grant-in-Aid for Scientific Research C, Grant no. 25460812. The funders had no role in the study design, data collection or analysis, the decision to publish or manuscript preparation.
Author information
Authors and Affiliations
Contributions
K.W. conceived and coordinated the project. K.W. and D.P.M. completed the data analysis. H.E., K.W., D.P.M. and D.S. wrote the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Eguchi, H., Wada, K., Prieto-Merino, D. et al. Lung, gastric and colorectal cancer mortality by occupation and industry among working-aged men in Japan. Sci Rep 7, 43204 (2017). https://doi.org/10.1038/srep43204
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep43204
- Springer Nature Limited
This article is cited by
-
Exposome and unhealthy aging: environmental drivers from air pollution to occupational exposures
GeroScience (2023)
-
Occupation- and industry-specific cancer mortality among Japanese women from 1980 to 2015
BMC Public Health (2022)
-
Evaluation of CSTB and DMBT1 expression in saliva of gastric cancer patients and controls
BMC Cancer (2022)
-
Mortality by occupation and industry among Japanese men in the 2015 fiscal year
Environmental Health and Preventive Medicine (2020)