Abstract
Inherited aortopathy, which is characterized by a high risk of fatal aortic aneurysms/dissections, can occur secondarily to several syndromes. To identify genetic mutations and help make a precise diagnosis, we designed a gene panel containing 15 genes responsible for inherited aortopathy and tested 248 probands with aortic disease or Marfan syndrome. The results showed that 92 individuals (37.1%) tested positive for a (likely) pathogenic mutation, most of which were FBN1 mutations. We found that patients with a FBN1 truncating or splicing mutation were more prone to developing severe aortic disease or valvular disease. To date, this is the largest reported cohort of Chinese patients with aortic disease who have undergone genetic testing. Therefore, it can serve as a considerable dataset of next generation sequencing data analysis of Chinese population with inherited aortopathy. Additionally, according to the accumulated data, we optimized the analysis pipeline by adding quality control steps and lowering the false positive rate.
Similar content being viewed by others
Introduction
Inherited aortopathy, which is characterized by aortic dilation or aortic aneurysms/dissection, may be syndromic, as occurs in Marfan syndrome (MFS)1, Loeys-Dietz syndrome (LDS)2, Ehlers-Danlos syndrome, vascular type (vEDS)3, and Shprintzen-Goldberg syndrome (SGS)4, or non-syndromic, in which abnormalities are restricted to the aorta5. Although these diseases have their own unique characteristics, they also share some clinical manifestations, which makes the precise diagnosis and treatment strategy difficult. Previous studies demonstrated that the mortality after the rupture of thoracic aortic aneurysms (TAA) was as high as 97%, with a median survival time of 3 days6, and the acute aortic dissection patients had a higher re-intervention rate, even if they survived the initial surgery7. Hence, early diagnosis is important because it provides valuable time for prophylactic measures to be taken. Genetic testing can help to detect the pathogenic genes/mutations involved in the disease and confirm the diagnosis before the full development of symptom, thereby reduce the rate of cardiovascular events.
Several causative genes for syndromic aortopathy have been identified, including FBN1 for Marfan syndrome8, TGFBR1/2, SMAD3, TGFB2 for Loeys-Dietz syndrome9,10,11, COL3A1 for Ehlers-Danlos syndrome, vascular type12, and SLC2A10 for arterial tortuosity syndrome13. Additionally, an increasing number of genes have been implicated in the pathogenesis of thoracic aortic aneurysms, including MYH11, ACTA2, NOTCH1, MYLK, PRKG1, and SKI14.
The clinical utility of genetic testing for heritable aortopathy is now well established15,16, and several commercial panel tests containing different numbers of genes are available. However, due to the lack of a database for Chinese population, it is challenging to determine the pathogenicity of genetic variants for Chinese patients. To identify genetic mutations and make a precise diagnosis and to establish an aortopathy genetic database for Chinese population, we recruited 248 probands with aortic disease or Marfan syndrome in Fuwai hospital and performed gene panel testing involving 15 genes related to inherited aortopathy. Herein, we report the molecular findings from the 248 patients, which, at present, is the largest group of aortic disease patients ever reported in China. Further, we optimized the analysis pipeline by adding quality control steps and lowering the false positive rate.
Results
Aortopathy panel performance
Sequencing of the 15 aortopathy genes (Table 1) in the 248 samples yielded a mean depth of ~350X and coverage of 98.7% (Supp. Figure S1). Exons in FBN1 with low (<20X) or no coverage were subject to Sanger sequencing to obtain 100% coverage. In addition, potential pathogenic mutations and rare variant of unknown significance (VUS) were confirmed using Sanger sequencing.
Automated and optimal analysis pipeline
Initially, we used Ion Torrent Suite and Ion Reporter, which were provided by Life Tech, to accomplish the alignment, variant calling and annotation processes. Based on our growing data and experience, we developed an automated and optimal analysis plugin named iAorta, which allowed us to automatically pick up suspected pathogenic mutations or VUS from polymorphism or false-positive variants, add quality control steps to assess the sequencing quality and indicate possible false-negative variants, and remove frequent false-positive mutations based on our 248 samples. Compared with Ion Torrent Suite, the analysis strategy of iAorta was to relax the filter conditions to avoid false negative variants. Subsequently, according to the accumulated data, false positive variants were removed.
After re-analyzing the sequencing data from our 248 samples by iAorta, we obtained a false-negative list (Supp. Table S1). We also generated a false-positive list after validation by Sanger sequencing. Most of the false-positive mutation were scattered over the end of amplicon and were likely introduced by degenerate primers and mapping error. For frameshift/non-frameshift indels, we evaluated the confidence based on the coverage depth (>20x), allele frequency (>10%), and strand bias (both forward and reverse allele reads >3, both forward/reverse and reverse/forward >0.7). If any of the three conditions was not satisfied, the sample was classified as a possible false-positive mutation and marked as “DropIndel”. After we removed some frequent false-positive mutations (Supp. Table S2) and modified our analysis pipeline, the false-positive rate decreased from 25.4% to 15.4%.
In addition, all of the bases coding cysteine in FBN1 were assigned as a “hotspot”. When there was a “NoCall” in the position, an alert for a possible false negative region was generated, and the exon was then Sanger sequenced.
Molecular findings of the aortopathy cohort
A total of 248 patients (162 males and 86 females) with Marfan syndrome and its related aortic diseases, were enrolled in our cohort, with a mean age of 46 years (5–60 years). The primary clinical diagnoses of these probands submitted for aortopathy panel testing were summarized in Table 2. Among the 248 individuals, 92 (37.1%) were tested positive for a (likely) pathogenic mutation, 70 (28.2%) had a VUS, and 86 (34.7%) were tested negative using the 15-gene aortopathy panel. Most of the (likely) pathogenic mutations were located in the FBN1 gene, because the cysteine residues in this gene were evolutionarily conserved and had essential functions17. Accordingly, the destruction or generation of a cysteine residue suggested that the mutation was probably pathogenic18. The pathogenicity of missense mutations in other genes was difficult to define due to the lack of functional studies or strong family segregation evidence. (Likely) pathogenic mutations were identified in FBN1, TGFBR1/2, ACTA2, MYH11, COL3A1 and SLC2A10 (Table 3), and VUS were identified in all 15 genes in the panel.
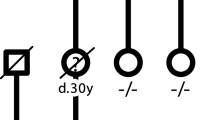
A genotype-phenotype correlation between FBN1 mutation type and aortic events was also investigated. Of all the 248 probands, 82 were tested positive for a (likely) pathogenic FBN1 mutation. Among them, 28 had undergone surgery due to a life-threatening aortic dissection, 21 had undergone prophylactic surgery due to aortic aneurysm, 6 had a valve replacement due to severe valvular disease, 4 had mild aortic dilation and came for genetic testing because of other system manifestations in Marfan syndrome, and the remaining 24 patients had no complete clinical information. We attempted to study the correlation between FBN1 mutation type and severity of aortic events, and the results were listed in Table 4. Among patients with a FBN1 truncating or splicing mutation, 15 suffered from life-threatening aortic dissection, 5 had severe valvular disease, while 9 had aortic aneurysm and therefore underwent prophylactic surgery. Besides, 3 patients with one FBN1 truncating or splicing mutation only showed mild aortic dilation probably due to a young age, therefore they were not excluded to have aortic disease progression in the future. Additionally, in the aneurysm group, patients with a FBN1 truncating or splicing mutation took a prophylactic surgery at a younger age (25.6y vs. 33.4y) than those with a missense mutation. These results suggested that patients with FBN1 truncating or splicing mutation were more prone to developing severe aortic disease or valvular disease.
Variant reclassification
When available, family segregation studies were performed to assist in the variant classification. In this study, 18 variants were reclassified through the family segregation study in our patient cohort (Table 5).
The FBN1, c.1427G>A (p.Cys476Tyr) variant in case AD246, which presented a classic MFS phenotype and a positive family history, was originally classified as likely pathogenic. However, it was downgraded to VUS after familial targeted sequencing revealed that the variant was not present in his affected sibling. Thus, whole exome sequencing (WES) was performed in the proband and his two affected sisters to find other potential pathogenic mutations. Another interesting case was as reported in our previously published paper19. The variant TGFBR2, c.1142G>C (p.Arg381Pro) was detected in a 5 year-old boy, who had a distinctive LDS phenotype of descending pseudoaneurysm, artery tortuosity, bifid uvula, hypertelorism. However, the mutation was also carried by his healthy father, which made its pathogenicity doubtful, although it was once reported as pathogenic in a LDS patient20. Further functional study was necessary to confirm its pathogenicity.
Discussion
Genetic testing is important for the early and accurate diagnosis of diseases. Although patients with Marfan syndrome and its related diseases are all characterized with aortopathy, they may differ in their progress of aortic aneurysm/dissection. It was previously reported that LDS patients had more aggressive arterial disease and rupture, with a median survival time of only 26 years2, compared with 48 years for patients with vEDS3 and 70 years for those with MFS21. However, with early diagnosis and proper management, LDS was particularly amendable to treatment. The incidence of fatal intraoperative or postoperative complications with vascular surgery was only 1.7% in LDS2 compared with approximately 45% in vEDS3.
The NGS (next generation sequencing)-based assays for screening inherited aortopathy genes have been well established and utilized in some laboratories15,16. Sequencing data processing and analysis is the key point, and validating the candidate causal variants via Sanger sequencing is the most time-consuming step. Therefore, how to optimize the algorithms to lower the false-positive rate without raising the false-negative rate is extremely important. In our study, we developed an automated and optimized pipeline named iAorta that automatically accomplished read mapping, recalibration, quality control, alignment, variant calling, annotation and variant filtering. Compared to the Ion Torrent Suite and Ion Reporter software, which were provided by Life Tech, iAorta was used more flexibly, which allowed us to automatically pick up suspected pathogenic mutations and VUS from polymorphism or false-positive variants, add quality control steps to assess the sequencing quality and to indicate possible false-negative variants, remove frequent false-positive mutations based our existing data and drop the low confidence indel variants to reduce the false-positive rate.
In addition to data processing and analysis, the classification of variant pathogenicity is challenging. Novel variants should be subjected to functional studies, but these are costly, time consuming, and often impractical in the clinical setting. Therefore, classification is largely dependent on database knowledge, which is extremely deficient in Chinese populations. The aim of our study was to build the largest shared database for Chinese aortopathy patients. In our cohort, 92 patients (37.1%) tested positive for a (likely) pathogenic mutation, including 84 Marfan patients, as well as 3 LDS, 3 TAAD (thoracic aortic aneurysms and aortic dissection), 1 vEDS and 1 arterial tortuosity syndrome case. Additionally, the results of the patients’ family members were helpful for pathogenicity classification. Specifically, in our study, 18 variants were reclassified based on family segregation studies. After screening by the current gene panel testing, some cases remained negative, although they presented classical clinical phenotypes or family histories. As a follow-up, we intend to perform MLPA (Multiplex Ligation-dependent Probe Amplification) or WES on these samples to find large deletion/duplication or new potential causative genes. Besides, in more than one third of the patients, no suspected mutation was identified, which suggested that additional aortopathy genes might exist. We anticipate that clinical sensitivity will rise as additional genes are identified and included in the panel and that VUS can be reclassified with increasing numbers of samples and family segregation studies. Several recently identified TAA genes, such as TGFB322, MFAP523, MAT2A24 and LOX25, can be added to the gene list.
A genotype-phenotype correlation between FBN1 mutation type and aortic events was investigated. Interestingly, we found that patients with a FBN1 truncating or splicing mutation were more prone to developing severe aortic disease or valvular disease than the patients with a FBN1 missense mutation. Similarly, Baudhuin et al. once reported that a higher frequency of truncating or splicing FBN1 variants was observed in MFS patients with an aortic event than in those without a reported aortic event26. However, the mechanism whereby FBN1 truncating or splicing mutations exert their effect on aneurysm progression and severity is not clear, which deserves our further investigation.
In summary, our data further expands the FBN1 mutation spectrum and offer evidence for the genotype-phenotype correlation given that Marfan patients with a FBN1 truncating or splicing mutation are more prone to developing severe aortic disease or valvular disease. The aortopathy panel assay undoubtedly presents a highly valuable clinical tool and lays the foundation for further study. We are dedicated to constructing the largest Chinese aortopathy genetic database and continually improving our testing quality.
Materials and Methods
Patients and consent
The study was approved by the ethics committee of Fuwai hospital and adhered to the Declaration of Helsinki. All experimental protocols were approved by the ethics committee of Fuwai hospital, and were carried out in accordance with the approved guidelines. All of the patients enrolled in this study were referred by the center of vascular surgery in Fuwai hospital. Each individual accepting the genetic test was adequately informed regarding the benefits and risks of the test and signed the consent form.
Between Feb 2014 and Apr 2016, we tested a total of 248 patients with various aortic phenotypes, such as early onset aortopathy patients with no apparent secondary causes and (suspected) Marfan patients. The follow-up study was carried out in subsequent clinic visits to the outpatient department and by telephone interviews.
Gene panel testing
A custom-designed gene panel containing 15 genes known to be associated with Marfan syndrome and its related aortic diseases was ordered from Life Tech, USA. The size of the panel was 168.67 kb, with coverage of 99.39% of the target regions.
Genomic DNA (deoxyribonucleic acid) was extracted from EDTA (eathylene diamine tetraacetic acid)–anticoagulated whole blood, and checked to assure the quality and quantity before processing. Library preparation was performed according to the manufacturer’s instructions (Ion AmpliSeqTM library kit 2.0, Life Technologies, Inc.). Pooled libraries (up to 12–15 samples per chip) were sequenced on the Ion 318TM Chip on Life PGMTM instrument.
Suspected pathogenic variants and VUS were confirmed using Sanger sequencing. Exons in FBN1 with low (<20X) or no coverage were also subjected to Sanger sequencing to obtain 100% coverage.
Bioinformatics analysis
To perform the analysis automatically, the iAorta plugin was developed based on the sequencing platform for ion torrent PGM™. The pipeline consisted of read mapping, recalibration, quality control, variant calling, annotation and variant filtering. The annotation included genetic reference sequences, genomic and cDNA positions, amino acid changes, and related information available from public databases, such as 1000 Genomes, dbSNP142 (National Center for Biotechnology Information, http://www.ncbi.nlm.nih.gov/SNP/), NHLBI Grand Opportunity Exome Sequencing Project (ESP6500) (https://esp.gs.washington.edu/drupal/), ExAC03 (http://exac.broadinstitute.org), ClinVar, DrugBank, Online Mendelian Inheritance in Man (OMIM), Uniprot (http://www.uniprot.org), and the Human Gene Mutation Database (HGMD), Pfam (http://pfam.xfam.org). The in-silico based computation analysis was carried out using a suite of bioinformatics tools, including SIFT, Polyphen2, MutationTaster, Grantham, and PolyP.
Because most of the heritable aortopathies were autosomal-inherited rare Mendelian disease, the variants with a minor allele frequency (MAF) > 1% in the following databases were filtered out: the 1000 Genomes, ESP6500, ExAC03.
Variant classification
Variants were analyzed for pathogenicity according to the recommendations from the American College of Medical Genetics (ACMG). Specifically, the analysis was based on the following criteria: (i) whether they were previously reported by functional study or family segregation study; (ii) the nature of the variant (e.g., nonsense, frameshift indel, or splicing mutations (intron ±1 or ±2)); (iii) variant frequency in the 1000 Genomes, Exome Sequencing Project (ESP6500) and ExAC03; (iv) conservation of the altered residue; (v) in-silico based computational prediction (SIFT, PholyPhen2, or MutationTaster); (vi) de novo mutation; and (vii) family segregation studies. Based on this information, a variant was classified into one of the 5 following categories: benign, likely benign, unknown significance, likely pathogenic or pathogenic27.
Additional Information
How to cite this article: Yang, H. et al. Genetic testing of 248 Chinese aortopathy patients using a panel assay. Sci. Rep. 6, 33002; doi: 10.1038/srep33002 (2016).
References
Sinha, K. P. & Goldberg, H. Marfan’s syndrome: a case with complete dissection of the aorta. Am Heart J 56, 890–897 (1958).
Loeys, B. L. et al. Aneurysm syndromes caused by mutations in the TGF-beta receptor. N Engl J Med 355, 788–798 (2006).
Pepin, M., Schwarze, U., Superti-Furga, A. & Byers, P. H. Clinical and genetic features of Ehlers-Danlos syndrome type IV, the vascular type. N Engl J Med 342, 673–680 (2000).
Doyle, A. J. et al. Mutations in the TGF-beta repressor SKI cause Shprintzen-Goldberg syndrome with aortic aneurysm. Nat Genet 44, 1249–1254 (2012).
Nicod, P. et al. Familial aortic dissecting aneurysm. J Am Coll Cardiol 13, 811–819 (1989).
Johansson, G., Markstrom, U. & Swedenborg, J. Ruptured thoracic aortic aneurysms: a study of incidence and mortality rates. J Vasc Surg 21, 985–988 (1995).
Schoenhoff, F. S. et al. Acute aortic dissection determines the fate of initially untreated aortic segments in Marfan syndrome. Circulation 127, 1569–1575 (2013).
Dietz, H. C. et al. Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 352, 337–339 (1991).
Loeys, B. L. et al. A syndrome of altered cardiovascular, craniofacial, neurocognitive and skeletal development caused by mutations in TGFBR1 or TGFBR2. Nat Genet 37, 275–281 (2005).
Regalado, E. S. et al. Exome sequencing identifies SMAD3 mutations as a cause of familial thoracic aortic aneurysm and dissection with intracranial and other arterial aneurysms. Circ Res 109, 680–686 (2011).
Lindsay, M. E. et al. Loss-of-function mutations in TGFB2 cause a syndromic presentation of thoracic aortic aneurysm. Nat Genet 44, 922–927 (2012).
Superti-Furga, A., Steinmann, B., Ramirez, F. & Byers, P. H. Molecular defects of type III procollagen in Ehlers-Danlos syndrome type IV. Hum Genet 82, 104–108 (1989).
Drera, B. et al. Two novel SLC2A10/GLUT10 mutations in a patient with arterial tortuosity syndrome. Am J Med Genet A 143A, 216–218 (2007).
Milewicz, D. M. & Regalado, E. S. Use of genetics for personalized management of heritable thoracic aortic disease: how do we get there? J Thorac Cardiovasc Surg 149, S3–S5 (2015).
Wooderchak-Donahue, W. et al. Clinical utility of a next generation sequencing panel assay for Marfan and Marfan-like syndromes featuring aortopathy. Am J Med Genet A 167A, 1747–1757 (2015).
Proost, D. et al. Performant Mutation Identification Using Targeted Next-Generation Sequencing of 14 Thoracic Aortic Aneurysm Genes. Hum Mutat 36, 808–814 (2015).
Schrijver, I., Liu, W., Brenn, T., Furthmayr, H. & Francke, U. Cysteine substitutions in epidermal growth factor-like domains of fibrillin-1: distinct effects on biochemical and clinical phenotypes. Am J Hum Genet 65, 1007–1020 (1999).
Arslan-Kirchner, M. et al. Clinical utility gene card for: Marfan syndrome type 1 and related phenotypes [FBN1]. Eur J Hum Genet 18 (2010).
Luo, M. et al. Genetic testing of 10 patients with features of loeys-dietz syndrome. Clin Chim Acta 456, 144–148 (2016).
Uike, K. et al. Systemic vascular phenotypes of Loeys-Dietz syndrome in a child carrying a de novo R381P mutation in TGFBR2: a case report. BMC Res Notes 6, 456 (2013).
Silverman, D. I. et al. Life expectancy in the Marfan syndrome. Am J Cardiol 75, 157–160 (1995).
Bertoli-Avella, A. M. et al. Mutations in a TGF-beta ligand, TGFB3, cause syndromic aortic aneurysms and dissections. J Am Coll Cardiol 65, 1324–1336 (2015).
Barbier, M. et al. MFAP5 loss-of-function mutations underscore the involvement of matrix alteration in the pathogenesis of familial thoracic aortic aneurysms and dissections. Am J Hum Genet 95, 736–743 (2014).
Guo, D. C. et al. MAT2A mutations predispose individuals to thoracic aortic aneurysms. Am J Hum Genet 96, 170–177 (2015).
Guo, D. C. et al. LOX Mutations Predispose to Thoracic Aortic Aneurysms and Dissections. Circ Res 118, 928–934 (2016).
Baudhuin, L. M., Kotzer, K. E. & Lagerstedt, S. A. Increased frequency of FBN1 truncating and splicing variants in Marfan syndrome patients with aortic events. Genet Med 17, 177–187 (2015).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17, 405–424 (2015).
Acknowledgements
We thanked all subjects who participated in this study. This work was supported by the grant of China 1000 Young Talents Program.
Author information
Authors and Affiliations
Contributions
H.Y. performed the majority of the data analysis and wrote the manuscript. M.L. was charge of patient recruitment, sample and clinical information collection. Y.F. was in charge of communication with the clinicians. Y.C. and W.L. analyzed the sequencing data. K.Y., C.M. and Y.M. performed the NGS sequencing and Sanger validation. J.Z. collected samples and communicated with patients. Y.F. gave a direction on the experiment, data analysis and interpretation. C.S. and Q.C. were in charge of the clinical evaluation and sample management. Z.Z. was in charge of the project design and revised the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Yang, H., Luo, M., Fu, Y. et al. Genetic testing of 248 Chinese aortopathy patients using a panel assay. Sci Rep 6, 33002 (2016). https://doi.org/10.1038/srep33002
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep33002
- Springer Nature Limited
This article is cited by
-
A population-based survey of FBN1 variants in Iceland reveals underdiagnosis of Marfan syndrome
European Journal of Human Genetics (2024)
-
Novel LTBP3 mutations associated with thoracic aortic aneurysms and dissections
Orphanet Journal of Rare Diseases (2021)
-
Genetic profiling and cardiovascular phenotypic spectrum in a Chinese cohort of Loeys-Dietz syndrome patients
Orphanet Journal of Rare Diseases (2020)
-
Human aortic aneurysm genomic dictionary: is it possible?
Indian Journal of Thoracic and Cardiovascular Surgery (2019)
-
Identification of gross deletions in FBN1 gene by MLPA
Human Genomics (2018)