Abstract
The advent of immunotherapy has greatly improved the prognosis of non-small cell lung (NSCLC) patients. However, given its low response rate and high cost of treatment, the search for valuable predictive markers of treatment efficacy is necessary. Considering the complexity and heterogeneity of the tumour and tumour microenvironment, the construction of a multi-dimensional prediction model is necessary. Therefore, we aimed to integrate clinical parameters, radiomic features, and immune signature data from NSCLC patients receiving immunotherapy to construct a multi-dimensional prediction model to better predict the efficacy of immunotherapy. The current study enrolled 137 NSCLC patients who received immunotherapy. We collected baseline clinical information, CT images, and tumour tissue specimens. Using 3D-Slicer software, radiomic features were extracted from patient CT images, and tumor tissue samples obtained before immunotherapy were subjected to immunohistochemical staining. Then, the least absolute shrinkage and selection operator (LASSO) Cox regression analysis was applied to downscale the data, and the radiomic features and immune signatures associated with the prognosis of immunotherapy patients were identified. The modified lung immune predictive index (mLIPI), radiomics score (Radioscore), immune score and multi-dimensional model nomogram were constructed. The C-index and area under the curve (AUC) were applied to evaluate the predictive efficacy of the models. Three radiomic features and three immune signatures that could predict the efficacy of immunotherapy were eventually screened. Multivariate analysis showed that the mLIPI, Radioscore, and immune score were independent predictive factors for PFS and OS (P < 0.05 for all models). The multi-dimensional model combining the three models showed better predictive efficacy than the mLIPI, Radioscore, and immune score (PFS: 0.721 vs. 0.662 vs. 0.610 vs. 0.610; OS: 0.727 vs. 0.661 vs. 0.601 vs. 0.602 respectively). The multi-dimensional model showed the best predictive efficacy, with C-index for PFS and OS higher than mLIPI, radioscore and immune score: 0.721 vs. 0.662 vs. 0.610 vs. 0.610 for PFS and 0.727 vs. 0.661 vs. 0.601 vs. 0.602 for OS, respectively. The AUC for the multi-dimensional model also performed better than those of the individual models: 0.771 vs. 0.684 vs. 0.715 vs. 0.711 for PFS and 0.768 vs. 0.662 vs. 0.661 vs. 0.658 for OS, respectively. The multi-dimensional model combining the three models had better predictive efficacy than any single model and was more likely to help provide patients personalized and precision medicine.
Similar content being viewed by others
Introduction
According to ‘Cancer Statistics, 2024,’ lung cancer is identified as the second most common cancer, accounting for 11% of all diagnoses in U.S. men and 12% in women, and it remains the leading cause of cancer-related deaths both nationally and globally, severely threatening the life and health of all human beings1. The transition from an era dominated by chemotherapy, which targeted tumor cells directly, to the current emphasis on immunotherapy and its focus on altering the tumor microenvironment (TME), marked a significant shift in the approach to cancer therapy2. By offering new avenues for treatment for early to advanced NSCLC, immunotherapy provides renewed hope to patients3,4,5,6,7,8,9. The 5-year OS of patients with unresectable locally advanced NSCLC receiving consolidation therapy with durvalumab has reached approximately 50% 10, and the 5-year OS of patients with advanced NSCLC has also improved from 10% in the chemotherapy era to 20–30% in the immunotherapy era11,12,13. Nevertheless, the data show that more than half of the patients still fail to benefit from immunotherapy. Due to the low response rate and high cost of treatment, it is essential to accurately select patients who might respond to immunotherapy. Programmed death ligand-1 (PD-L1) expression is the most widely used predictive biomarker of immunotherapy efficacy in current clinical practice. The KEYNOTE-024 study demonstrated that patients with a PD-L1 expression ≥ 50% and without EGFR/ALK alterations may receive immunotherapy monotherapy to achieve chemo-free survival14. However, PD-L1 expression has limitations as a predictive marker of efficacy, and some research has shown that even patients with negative PD-L1 expression may benefit from immunotherapy, and vice versa15. Therefore, the development of more reliable prediction schemes remains a top priority.
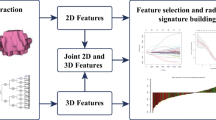
Peripheral blood inflammatory factors have been shown to a certain extent to predict the efficacy of immunotherapy to a certain extent. Additionally, these methods are noninvasive16. Previously, we performed external validation of three prediction models based on clinical and peripheral blood inflammation parameters and identified the modified lung immune predictive index (mLIPI) score as the most suitable prediction model for the Chinese population17. As a prominent research method, radiomics has successfully transformed image information into very large amounts of data that can be used for statistical analyses. Thus, our traditional perception of images has been updated, and further exploration of the intrinsic mechanism related to tumour development and treatment is possible. After years of development, radiomics has stood out in the fields of early cancer detection and treatment efficacy prediction18,19. In this study, we collected enhanced CT images of patients before immunotherapy, extracted radiomic features, screened out features with prognostic significance, and constructed a radiomic score (Radioscore).
Previous studies have demonstrated that tumor-infiltrating immune cells, including tumor-infiltrating lymphocytes (TILs), macrophages, and natural killer (NK) cells, all exhibit predictive power for the efficacy of immunotherapy20,21,22,23,24,25,26,27,28,29. In this study, we obtained tumour tissue specimens from NSCLC patients and performed immunohistochemistry (IHC) staining to detect surface markers of T lymphocytes, B lymphocytes, NK cells, macrophages, and PD-L1 expression levels on the tumour cell surface at the protein level.
In this study, we aimed to integrate the clinical parameters, radiomic features, and immune signature data of NSCLC patients receiving immunotherapy to construct a multi-dimensional prediction model, and then, a nomogram was constructed to visualize the model. This model is expected to provide clinicians with the most comprehensive patient information possible and better guide the clinical application of immunotherapy.
Materials and methods
Patients
We retrospectively collected baseline clinical data from 137 NSCLC patients who received immunotherapy at Shandong Cancer Hospital between March 2019 and June 2020. The inclusion criteria were as follows: (1) stage IIIB to IV NSCLC confirmed by imaging and pathology; (2) age ≥ 18 years; (3) Eastern Cooperative Oncology Group performance status (ECOG PS) ≤ 2; (4) having received at least 2 cycles of immune checkpoint inhibitor (ICI); (5) CT scans available within 28 days before starting immunotherapy; (6) blood markers available within 1 week before starting immunotherapy; and (7) pretreatment tumor specimens available. The exclusion criteria were as follows: (1) concomitant infection, including human immunodeficiency virus or hepatitis; (2) use of systemic steroids; (3) concomitant radiotherapy; and (4) previous or ongoing autoimmune disorders. Experiments using clinical specimens were approved by the ethics committee of Shandong Cancer Hospital and Institute (Approval number: 2023003151). All methods were carried out in accordance with relevant guidelines and regulations. The ethics committee of Shandong Cancer Hospital and Institute approved the waiver of informed consent.
After initial treatment with ICIs, patients received CT scans every 8–12 weeks for efficacy assessment, which was performed according to the Response Evaluation Criteria in Solid Tumours (RECIST, version 1.1). Progression-free survival (PFS) was defined as the period from the initiation of ICIs to disease progression or death, and overall survival (OS) was defined as the period from the initiation of ICIs to death from any cause or to the last follow-up. For those patients who did not show disease progression after the initial treatment with ICIs, we treated these cases as censored data. In our survival analysis, we documented the date of the last effective follow-up as the endpoint for their progression-free survival (PFS) or overall survival (OS).
Data collection
We reviewed the medical records system and extracted baseline clinical information and haematological inflammatory parameters, such as the Eastern Cooperative Oncology Group (ECOG) score, smoking status, lactate dehydrogenase (LDH) level, and the neutrophil-to-lymphocyte ratio (NLR) from the patients who met the inclusion criteria. We collected the contrast-enhanced CT images of the patients before ICI treatment.
We applied 3D-slicer software to segment the region of interest (ROI) that covered the gross tumour volume (GTV), and then extracted 117 radiomics features from the ROI of each patient using the open-source package PyRadiomics in the software. The main types of features include first-order features, shape features (3D), shape features (2D), grey level co-occurrence matrix (GLCM) features, grey level size zone matrix (GLSZM) features, grey level run length matrix (GLRLM) features, neighbouring grey tone difference matrix (NGTDM) features, and grey level dependence matrix (GLDM) features.
Immunohistochemistry and evaluation
We used CD3, CD8, CD20, CD56, and CD68, which are known to be the most widely utilized cell surface markers for the detection of T lymphocytes, B lymphocytes, NK cells, and macrophages, for immunohistochemical (IHC) staining of immune cells in the TME30.
Tumour biopsy specimens from 137 NSCLC patients were fixed overnight in 10% formalin, paraffin-embedded, and sectioned to obtain 4 micrometre-thick sequential tumour samples for IHC staining. The sections were deparaffinized in xylene. Then, they were incubated in 100, 95, and 70% alcohol for 5 min and rehydrated in water. Subsequently, high-pressure thermal repair method was applied to complete the antigen retrieval. Then, primary antibodies, including anti-CD3 antibody, anti-CD8 antibody, anti-CD68 antibody, anti-CD56 antibody (Abcam company), anti-PD-L1 antibody (Beijing Zhongshan Jinqiao Biotechnology Company), and anti-CD20 antibody (Cell Signaling Technology company) were stained for 1 h at room temperature. After that, HRP-labelled goat anti-rabbit secondary antibody was added and stained for half an hour at room temperature. Finally, DAB was added for 60 s and then counterstained with haematoxylin for 5 min. Examples of low and high expression of CD3, CD8, CD20, CD56, CD68, and PD-L1 are shown in Fig. 1.
CD3, CD8, CD20, and CD68 expression was first evaluated in a low power field (LPF). Then, five representative areas where the stained cells were clustered at higher density were selected for counting of positive cells by high power, after which the average value was calculated. CD56 expression was assessed by randomly selecting 10 high-power fields (HPFs) and counting. The presence of more than 5 NK cells in each field, it was scored as 1, and the absence of more than 5 cells was scored as 0, and the remaining was scored as 0.5. PD-L1 status was determined from the tumour proportion score (TPS). The TPS was calculated as the percentage of positive tumour cells divided by the number of all tumour cells31.
Construction of the mLIPI, Radioscore, and Immune score
The calculation of the mLIPI score model was performed based on previously reported literature17,32. Details are shown in the Supplementary Table 1.
Features dimension reduction and screening were performed using the least absolute shrinkage and selection operator (LASSO) Cox regression method for both the Radioscore and immune scores. The most predictive features and weight coefficients for the efficacy of ICIs were selected and linearly combined to construct the Radioscore and immune score. The C-index was applied to evaluate the predictive efficacy of the models.
Statistical analysis
SPSS 23.0 statistical software was applied for data analysis. ROC curves were plotted, and the point with the maximized Youden’s index on the curve was selected as the cut-off value of the Radioscore and immune score. The area under the curve (AUC) was applied to evaluate the predictive efficacy of the models. For the analysis and plotting of PFS and OS, we utilized the Kaplan-Meier method along with the log-rank test to compare the survival curves. Furthermore, cox proportional hazards regression models were applied to assess the independence of risk factors associated with PFS and OS. Variables with P < 0.05 in the univariate analysis were included in the subsequent multivariate analysis. We utilized the glmnet package in R version 3.6.0 software to perform the LASSO Cox regression algorithm. Additionally, the rms package was employed to construct the nomogram. Furthermore, we conducted internal validation of the nomogram using ten-fold cross-validation. Finally, the clinical application of the model was assessed through decision curve analysis (DCA).
Results
Patient characteristics
A total of 137 patients with NSCLC who met the enrolment criteria were included in the present study. The basic characteristics of the patients are summarized in Table 1. The majority of patients were male (72.3%), and the median age was 62 years (range 30–81 years). Nearly half of the patients had a history of smoking (45.3%). The majority of recruited patients had a histological diagnosis of adenocarcinoma (62.8%), and the disease stage was mostly stage IV (79.6%). Eighty-four patients (61.3%) received ICIs as first-line or second-line therapy. After a median follow-up period of 35.8 months, the mPFS and mOS were 5.4 (95% CI:4.5–6.4) and 13.4 months (95% CI:10.9–15.9), respectively.
Construction of the Radioscore and immune score
We extracted 112 radiomic features from the pretreatment CT images of each patient. Then, we performed dimensionality reduction of the data and eventually screened three radiomic features associated with the prognosis of patients receiving immunotherapy by the LASSO Cox regression analysis to construct Radioscore (Supplementary Fig. 1). The calculation formula was as follows: Radioscore = 0.0034772*Large Dependence Low Gray Level Emphasis + 0.0013238*Maximum_A + 0.0000002*Maximum_B. The immune score was constructed in the same manner and ultimately screened out three immune signatures associated with treatment prognosis were ultimately screened out (Supplementary Fig. 2). The calculation formula was as follows: immune score = 0.4*PD-L1 + 0.008*CD8-0.038*CD56. Furthermore, multivariate analysis revealed that the Radioscore and immune score were independent predictive factors for PFS and OS, respectively (Table 2).
Survival analysis based on mLIPI, Radioscore, and immune score
Patients were divided into two subgroups according to their mLIPI score: those with a good prognosis (mLIPI ≤ 1) and poor prognosis (mLIPI ≥ 2). The mPFS and mOS in the good prognosis group were 7.0 months (95% CI: 6.0–8.0) and 15.9 months (95% CI: 10.7–21.1), respectively. The 6-month PFS rate and 1-year OS rate were 60.6% and 63.6%, respectively (Figs. 2 and 3). In the poor prognosis group, the mPFS and mOS were 3.8 months (95% CI: 2.7–4.8) and 6.9 months (95% CI: 4.5–9.3), respectively. The optimal cut-off value for Radioscore was determined by plotting the ROC curve, which was 0.391. As shown in Figs. 2 and 3, patients with lower scores had a better prognosis than those with higher scores. The mPFS and mOS of the lower-scoring group were 7.3 months (95% CI: 6.4–8.3) and 15.9 months (95% CI: 11.4–20.3), respectively. The 6-month PFS rate and 1-year OS rate were 70.8% and 72.9%, respectively. In the higher-scoring group, mPFS and mOS were 4.6 months (95% CI: 4.4–4.9) and 11.0 months (95% CI: 8.0–14.0), respectively. The 6-month PFS rate and 1-year OS rate were 35.9% and 46.0%, respectively. The optimal cut-off value for the immune score was selected in the same manner, and was 0.0831. As shown in Figs. 2 and 3, patients with higher scores had a better prognosis than those with higher scores. The mPFS and mOS of the higher-scoring group were 7.1 months (95% CI: 6.4–7.8) and 17.1 months (95% CI: 8.7–25.5), respectively. The 6-month PFS rate and 1-year OS rate were 66.6% and 64.9%, respectively. In the lower score group, the mPFS and mOS were 4.7 months (95% CI: 4.2–5.2) and 10.6 months (95% CI: 6.9–14.3), respectively. The 6-month PFS rate and 1-year OS rate were 35.0% and 48.7%, respectively.
Predictive effects of mLIPI, Radioscore, immune score, and multi-dimensional prediction model
The C-index was applied to compare the predictive ability of these models. The results showed that the multi-dimensional model incorporating mLIPI, Radioscore, and immune score showed the best predictive efficacy compared to the TNM staging system, mLIPI, Radioscore, and immune score (PFS: 0.721 vs. 0.568 vs. 0.662 vs. 0.610 vs. 0.610; OS 0.727 vs. 0.534 vs. 0.661 vs. 0.601 vs. 0.602 respectively) (Fig. 4). To provide oncologists with a quantitative method to predict the 6-month PFS and 1-year OS of patients receiving immunotherapy, we built nomogram based on the multi-dimensional prediction model containing the above three models (Fig. 4). In addition, the calibration curves of the multi-dimensional prediction nomogram showed a favourable agreement between predictions and actual observations (Fig. 5). Additionally, the decision curve analysis (DCA) results indicated that the integrated model-based nomogram yielded favorable net benefits across a range of reasonable thresholds, especially within the OS threshold range of 0.1–0.8 and the PFS threshold range of 0.2–0.8 (Fig. 6). The AUC for the nomogram also performed better than mLIPI, radioscore and immune score: 0.771 vs. 0.684 vs. 0.715 vs. 0.711 for PFS and 0.768 vs. 0.662 vs. 0.661 vs. 0.658 for OS, respectively (Fig. 7).
Discussion
Lung cancer currently has the highest mortality rate worldwide33. Although the advent of immunotherapy has brought significant survival benefits to NSCLC patients, our ability to accurately identify patients who will benefit from immunotherapy remains very limited. Considering the high medical costs of immunotherapy, it is particularly crucial to construct an effective predictive model. Previous parametric prediction models mostly focused on a single dimension. However, considering that the therapeutic efficacy of ICIs is influenced by the internal characteristics of the tumour and the immune state of the body, it is obvious that a single-dimensional parametric prediction model cannot be used to accurately predict curative effects.
In the present study, we collected clinical parameters, CT images, and immune characteristics of a relatively large number of NSCLC patients before immunotherapy and combined all these indicators to construct a multi-dimensional prediction model. Compared to unidimensional prediction models, this approach could overcome the deficiencies of a single marker and fully utilize of the advantages of each marker while accounting for the scientific basis and accessibility of each marker34. Ultimately, by visualizing the model by plotting the nomogram, we expect patients to obtain the full benefit from these transformative treatments and assist clinicians in their clinical decision-making. The results demonstrate that the C-index of the multi-dimensional prediction model was 0.72, which is superior to the prediction performance of other single-dimensional models.
Numerous studies have demonstrated that peripheral blood inflammatory factors can predict the efficacy of immunotherapy35,36,37,38. Notably, peripheral blood is readily available and can be obtained repeatedly. Based on our previous findings, the score of peripheral blood inflammation parameters included in the current multi-dimensional model was mLIPI17, which included pretreatment NLR, LDH, and ECOG PS. The NLR has been shown to reflect the state of chronic inflammation in patients, and chronic inflammation can suppress the body’s immune response to tumours and exert protumour effects in a variety of ways39,40. Serum LDH concentrations could reflect the tumour burden and the hypoxic condition of the TME in patients with solid tumours. Elevated serum levels of LDH generally correlate with poor prognosis41. In sum, the mLIPI contains a subset of clinical parameters that could reflect the immunological competence of NSCLC patients, and a higher score indicates a poorer disease outcome. In this study, the c-index for predicting the efficacy of immunotherapy PFS and OS was 0.610 and 0.602, respectively. Compared to traditional medical images, radiomics not only provides anatomical information such as changes in tumour volume, lesion density, or degree of enhancement, but also extracts mineable data from the images, providing additional information about tumour phenotype, gene and protein expression, etc. Thus imaging histology can be considered a “virtual biopsy” that can elucidate the association between imaging features and tumour biological or clinical characteristics42. Radiomics has been widely used in lung cancer, either for benign and malignant identification of lung nodules or for patient prognosis prediction, all of which have shown promising applications43. Tian et al. collected computed tomography (CT) images of 117 patients with stage IV EGFR mutated NSCLC and extracted 1032 radiomics features. Ultimately, screening 12 features associated with the efficacy of tyrosine kinase inhibitors (TKIs) were screened to construct a prediction model, the AUC of which predicted PFS at 6 months was 0.71144. In the present study, we applied 3D-slicer software to extract radiomics features and screened three features associated with prognosis by the LASSO Cox regression model, namely LargeDependenceLowGrayLevelEmphasis, Maximum_A, and Maximum_B. Radioscore was constructed, and the C-index of the predictive accuracy of PFS and OS was 0.610 and 0.621, respectively. Large Dependence Low Gray Level Emphasis measures the joint distribution of large dependence with lower gray-level values. The ‘Maximum’ refers to the maximum gray level intensity within the ROI. A higher value of these indicators correlates with poorer outcomes in immunotherapy. Immune cell infiltration in the TME was significantly correlated with the efficacy of immunotherapy in lung cancer. However, a single immune signature cannot comprehensively reflect the immune status of the TME; therefore, it is necessary to establish a reliable and feasible scoring system related to the immune microenvironment. In this study, we screened three markers that were predictive for the prognosis of NSCLC treated with ICIs by a LASSO Cox regression model and constructed an immune score. The calculation was as follows: immune score = 0.038*CD56-0.4*PD-L1-0.008*CD8. The expression of PD-L1 and CD8 was positively correlated with the efficacy of ICIs, and the expression of CD56 was negatively correlated with efficacy. Targeting the PD-1/PD-L1 axis is a significant breakthrough in cancer therapy, and the PD-L1 expression level often correlates positively with treatment efficacy45,46,47,48. The National Comprehensive Cancer Network (NCCN) guidelines also recommend different immunotherapy regimens for NSCLC patients depending on their PD-L1 expression levels49. CD8 + T lymphocytes exert antitumour effects by secreting granzyme B (GzmB) and interferon-γ (IFN-γ), and are also the main effector cells of ICIs50. Therefore, the infiltration density of CD8 + T lymphocytes in the TME is also an important biomarker for predicting the efficacy of ICIs51.
The relationship between NK cell infiltration in the TME and the cancer prognosis has been a controversial topic. A study by Yang et al. that included 378 patients with advanced pancreatic cancer revealed that the number of NK cell infiltrates in the tumour microenvironment was negatively correlated with the prognosis. This may be due to the reduced secretion of IL-2, IFN-γ, and TNF-α in the TME, resulting in impaired activation of NK cells and an inability to kill tumour cells52. The relationship between NK cells in NSCLC and prognosis has also been controversial53. Russick J, et al. reported that total NK cell density in the TME of lung cancer patients was not associated with prognosis, whereas in patients with high intratumour CD8 + T-cell density, the density of NK cells was associated with poorer prognosis. Immunohistochemistry and transcriptome sequencing revealed that the number of CD8 T cells was positively correlated with CTLA4 gene expression in NK cells, suggesting that the inhibitory effect on NK cells might be limited to a subset of NK cells expressing CTLA454. In this study, we observed that the density of intratumoural NK cells was negatively correlated with the efficacy of immunotherapy. This might be because NK cells in the TME are influenced by tumour cells to form a unique subset that was more conducive to tumour cell growth.
Our study also has several potential limitations. First, this was a retrospective study with unavoidable selection bias, and only patients who met the inclusion criteria were enrolled in the analysis. Second, this is a single-centre study; however, given that radiomics involves the acquisition of information from CT images, there might be machine parameters and operational errors in collecting images between multiple centres. Third, we retrospectively collected specimens from 2018 to 2020, so the storage time of the specimens may affect the accuracy of the IHC analysis. Additionally, the majority of the specimens were biopsy specimens with less tissue and therefore limited immune signatures that could be analysed. Furthermore, current research indicates that driver gene mutations and tumor mutation burden (TMB) may affect the efficacy of immunotherapy. However, our study did not include an analysis of these factors. Moreover, the limited number of cases in our study could affect the statistical power and generalizability of our findings. Future research involving larger cohorts is required to validate and potentially expand upon our conclusions.
Conclusion
Clinical parameters, radiomics features, and immune signatures are all independent predictive factors for NSCLC patients treated with immunotherapy. The multi-dimensional prediction model combining the three models had better predictive efficacy than any single model and was more likely to help patients achieve personalized and precision medicine.
Data availability
The data that support the findings of this study are available from the corresponding author, Linlin Wang, upon reasonable request.
References
Siegel, R. L., Giaquinto, A. N. & Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin.74, 12–49 (2024).
Pardoll, D. M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer. 12, 252–264 (2012).
Brahmer, J. et al. Nivolumab versus Docetaxel in advanced squamous-cell non–small-cell lung cancer. N. Engl. J. Med.373, 123–135 (2015).
Herbst, R. S. et al. Pembrolizumab versus Docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 387, 1540–1550 (2016).
Rittmeyer, A. et al. Atezolizumab versus Docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 389, 255–265 (2017).
O’Brien, M. et al. Pembrolizumab versus placebo as adjuvant therapy for completely resected stage IB–IIIA non-small-cell lung cancer (PEARLS/KEYNOTE-091): an interim analysis of a randomised, triple-blind, phase 3 trial. Lancet Oncol.23, 1274–1286 (2022).
Felip, E. et al. Adjuvant atezolizumab after adjuvant chemotherapy in resected stage IB–IIIA non-small-cell lung cancer (IMpower010): a randomised, multicentre, open-label, phase 3 trial. Lancet. 398, 1344–1357 (2021).
Forde, P. M. et al. Neoadjuvant nivolumab plus chemotherapy in resectable lung cancer. N. Engl. J. Med.386, 1973–1985 (2022).
Wakelee, H. et al. Perioperative pembrolizumab for early-stage non–small-cell lung cancer. N. Engl. J. Med.389, 491–503 (2023).
Spigel, D. R. et al. Five-year survival outcomes from the PACIFIC trial: Durvalumab after chemoradiotherapy in stage III non–small-cell lung cancer. J. Clin. Oncol.40, 1301 (2022).
Brahmer, J. R. et al. Health-related quality-of-life results for pembrolizumab versus chemotherapy in advanced, PD-L1-positive NSCLC (KEYNOTE-024): a multicentre, international, randomised, open-label phase 3 trial. Lancet Oncol.18, 1600–1609 (2017).
Garassino, M. C. et al. Patient-reported outcomes following pembrolizumab or placebo plus pemetrexed and platinum in patients with previously untreated, metastatic, non-squamous non-small-cell lung cancer (KEYNOTE-189): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol.21, 387–397 (2020).
Paz-Ares, L. et al. A randomized, placebo-controlled trial of pembrolizumab plus chemotherapy in patients with metastatic squamous NSCLC: protocol-specified final analysis of KEYNOTE-407. J. Thorac. Oncol.15, 1657–1669 (2020).
Reck, M. et al. Updated analysis of KEYNOTE-024: pembrolizumab versus platinum-based chemotherapy for advanced non-small-cell lung cancer with PD-L1 tumor proportion score of 50% or greater. (2019).
Bagchi, S., Yuan, R. & Engleman, E. G. Immune checkpoint inhibitors for the treatment of cancer: clinical impact and mechanisms of response and resistance. Annu. Rev. Pathol.16, 223–249 (2021).
Mezquita, L. et al. Association of the lung immune prognostic index with immune checkpoint inhibitor outcomes in patients with advanced non–small cell lung cancer. JAMA Oncol.4, 351–357 (2018).
Zhao, Q. et al. Three models that predict the efficacy of immunotherapy in Chinese patients with advanced non-small cell lung cancer. Cancer Med.10, 6291–6303 (2021).
Zhang, L. et al. The progress of multimodal imaging combination and subregion based radiomics research of cancers. Int. J. Biol. Sci.18, 3458 (2022).
Barabino, E. et al. Exploring response to immunotherapy in non-small cell lung cancer using delta-radiomics. Cancers. 14, 350 (2022).
Yu, X. et al. Immune modulation of liver sinusoidal endothelial cells by melittin nanoparticles suppresses liver metastasis. Nat. Commun.10, 574 (2019).
Tang, H. et al. Facilitating T cell infiltration in tumor microenvironment overcomes resistance to PD-L1 blockade. Cancer cell.29, 285–296 (2016).
Al-Shibli, K. I. et al. Prognostic effect of epithelial and stromal lymphocyte infiltration in non–small cell lung cancer. Clin. Cancer Res.14, 5220–5227 (2008).
Schalper, K. A. et al. Objective measurement and clinical significance of TILs in non–small cell lung cancer. J. Natl Cancer Inst.107, dju435 (2015).
Kinoshita, T. et al. Prognostic value of tumor-infiltrating lymphocytes differs depending on histological type and smoking habit in completely resected non-small-cell lung cancer. Ann. Oncol.27, 2117–2123 (2016).
Germain, C. et al. Presence of B cells in tertiary lymphoid structures is associated with a protective immunity in patients with lung cancer. Am. J. Respir. Crit Care Med.189, 832–844 (2014).
Myers, J. A. & Miller, J. S. Exploring the NK cell platform for cancer immunotherapy. Nat. Reviews Clin. Oncol.18, 85–100 (2021).
Ghaedrahmati, F., Esmaeil, N. & Abbaspour, M. Targeting immune checkpoints: how to use natural killer cells for fighting against solid tumors. Cancer Commun.43, 177–213 (2023).
Xiang, X., Wang, J., Lu, D. & Xu, X. Targeting tumor-associated macrophages to synergize tumor immunotherapy. Signal. Transduct. Target. Therapy. 6, 75 (2021).
Zhang, E. et al. Roles and mechanisms of tumour-infiltrating B cells in human cancer: a new force in immunotherapy. Biomark. Res.11, 28 (2023).
Amoueian, S., Attaranzadeh, A. & Montazer, M. Intratumoral CD68-, CD117-, CD56-, and CD1a-positive immune cells and the survival of Iranian patients with non-metastatic intestinal-type gastric carcinoma. Pathology-Research Pract.211, 326–331 (2015).
Saito, Y. et al. Inter-tumor heterogeneity of PD-L1 expression in non-small cell lung cancer. J. Thorac. Disease. 11, 4982 (2019).
Moor, R., O’Byrne, K. & Roberts, K. Modified lung Immune Predictive Index (mLIPI) as a predictive tool of nivolumab outcomes and immune related adverse events in advanced non-small cell lung cancer (NSCLC) patients. Lung Cancer. 127, S67–S68 (2019).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J. Clin.71, 209–249 (2021).
Bai, R., Lv, Z., Xu, D. & Cui, J. Predictive biomarkers for cancer immunotherapy with immune checkpoint inhibitors. Biomark. Res.8, 1–17 (2020).
Kazandjian, D., Gong, Y., Keegan, P., Pazdur, R. & Blumenthal, G. M. Prognostic value of the lung immune prognostic index for patients treated for metastatic non–small cell lung cancer. JAMA Oncol.5, 1481–1485 (2019).
Prelaj, A. et al. Predictive biomarkers of response for immune checkpoint inhibitors in non–small-cell lung cancer. Eur. J. Cancer. 106, 144–159 (2019).
Hwang, M. et al. Peripheral blood immune cell dynamics reflect antitumor immune responses and predict clinical response to immunotherapy. J. Immunother. Cancer10 (2022).
Du, X. et al. Peripheral blood lymphocytes differentiation patterns in responses/outcomes to immune checkpoint blockade therapies in non-small cell lung cancer: a retrospective study. BMC cancer. 23, 83 (2023).
Elinav, E. et al. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nat. Rev. Cancer. 13, 759–771 (2013).
Russo, A. et al. Neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and outcomes with nivolumab in pretreated non-small cell lung cancer (NSCLC): a large retrospective multicenter study. Adv. Therapy. 37, 1145–1155 (2020).
Brand, A. et al. LDHA-associated lactic acid production blunts tumor immunosurveillance by T and NK cells. Cell Metabol.24, 657–671 (2016).
Limkin, E. J. et al. Promises and challenges for the implementation of computational medical imaging (radiomics) in oncology. Ann. Oncol.28, 1191–1206 (2017).
Digumarthy, S. R. et al. Predicting malignant potential of subsolid nodules: can radiomics preempt longitudinal follow up CT? Cancer Imaging. 19, 1–8 (2019).
Song, J. et al. A New Approach to predict progression-free survival in Stage IV EGFR-mutant NSCLC patients with EGFR-TKI TherapyPrediction of EGFR-TKI Treatment Outcome in Stage IV NSCLC. Clin. Cancer Res.24, 3583–3592 (2018).
Munari, E. et al. PD-1/PD-L1 in cancer: pathophysiological, diagnostic and therapeutic aspects. Int. J. Mol. Sci.22, 5123 (2021).
Reck, M. et al. Pembrolizumab versus chemotherapy for PD-L1–positive non–small-cell lung cancer. N engl. J. med.375, 1823–1833 (2016).
Aguilar, E. et al. Outcomes to first-line pembrolizumab in patients with non-small-cell lung cancer and very high PD-L1 expression. Ann. Oncol.30, 1653–1659 (2019).
Ricciuti, B. et al. Association of high tumor mutation burden in non–small cell lung cancers with increased immune infiltration and improved clinical outcomes of PD-L1 blockade across PD-L1 expression levels. JAMA Oncol.8, 1160–1168 (2022).
Ettinger, D. S. et al. Non–small cell lung cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Canc. Netw.20, 497–530 (2022).
An, H. J., Chon, H. J. & Kim, C. Peripheral blood-based biomarkers for immune checkpoint inhibitors. Int. J. Mol. Sci.22, 9414 (2021).
Chen, D. S. & Mellman, I. Oncology meets immunology: the cancer-immunity cycle. immunity39, 1–10 (2013).
Yang, C. et al. Anergic natural killer cells educated by tumor cells are associated with a poor prognosis in patients with advanced pancreatic ductal adenocarcinoma. Cancer Immunol. Immunother.67, 1815–1823 (2018).
Picard, E. et al. Circulating NKp46 + natural killer cells have a potential regulatory property and predict distinct survival in Non-small Cell Lung Cancer. Oncoimmunology. 8, e1527498 (2019).
Russick, J. et al. Natural killer cells in the human lung tumor microenvironment display immune inhibitory functions. J. Immunother. Cancer8 (2020).
Author information
Authors and Affiliations
Contributions
J.Y. and L.W.—conception and design. X.Z., X.W., B.L., and Q.Z.—data acquisition and analysis. Q.Z. and Y.X.—draft revision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, Q., Zhong, X., Wang, X. et al. Clinical multi-dimensional prognostic nomogram for predicting the efficacy of immunotherapy in NSCLC. Sci Rep 14, 21380 (2024). https://doi.org/10.1038/s41598-024-72760-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72760-x
- Springer Nature Limited