Abstract
Antimicrobial-resistant bacteria have been an increasing problem in human medicine and animal husbandry since the introduction of antimicrobials on the market in the 1940s. Over the last decades, efforts to reduce antimicrobial usage in animal husbandry have been shown to limit the development of resistant bacteria. Despite this, antimicrobial-resistant bacteria are still commonly detected and isolated worldwide. In this study, we investigated the presence of antimicrobial-resistant bacteria in bovine milk samples using a multiple approach based on culturing and amplicon sequencing. We first enriched milk samples obtained aseptically from bovine udders in the presence of two antimicrobials commonly used to treat mastitis and then described the resistant microbiota by amplicon sequencing and isolate characterization. Our results show that several commensal species and mastitis pathogens harbor antimicrobial resistance and dominate the enriched microbiota in milk in presence of antimicrobial agents. The use of the two different antimicrobials selected for different bacterial taxa and affected the overall microbial composition. These results provide new information on how different antimicrobials can shape the microbiota which is able to survive and reestablish in the udder and point to the fact that antimicrobial resistance is widely spread also in commensal species.
Similar content being viewed by others
Introduction
Mastitis is an inflammation of the udder, often caused by bacteria, with high cost to the dairy industry and a large impact on animal welfare1,2. Bacteria enter the udder through the teat canal during milking or from the cow’s environment, such as bedding materials1. Mastitis can be classified as clinical or subclinical. The clinical cases display signs such as fever, redness, swelling, and pain in addition to an increase of the somatic cell count (SCC) in the milk from 10,000 to 100,000 cells/mL to several million cells/mL. The increased number of somatic cells is due to immune cells that migrate to the udder lumen to fight off the infection and increased shedding of the udder epithelial cells. Subclinical cases are not associated with the abovementioned signs and present a SCC of 100,000 to several million cells/mL depending on the pathogen3,4,5,6. An essential part of combating mastitis is through antimicrobial treatment. However, several studies show that antimicrobial agents have a limited impact on the pathogenic bacteria causing the infection, mainly when the infectious bacterium is Gram-negative7,8,9.
Gram-positive bacteria are the most frequent findings in mastitis in Norway10, and penicillin is currently the first choice for treating bacterial mastitis11. In cases where penicillin resistance is detected, other antimicrobial agents, such as a combination of amoxicillin and clavulanic acid (AMC), are available12. Penicillin and amoxicillin are β-lactams targeting bacterial cell wall synthesis and are widely used in veterinary medicine13. Amoxicillin is typically administered with clavulanic acid, an inhibitor of β-lactamases, enzymes that a bacterium can produce that binds and cleaves β-lactams so that they are no longer harmful to the cell. The treatment for mastitis is commonly a combination of intramammary and systemic injections of the chosen antimicrobial agent in combination with optimal cow comfort and supportive therapy such as fluid therapy14. Dry cow therapy is another way the bacteria in the udder are exposed to antimicrobials15. As the cow has a risk of contracting an infectious bacteria causing mastitis during the dry period, a common practice has been to treat the cow with intramammary antimicrobial agents, often cloxacillin, at dry-off to reduce the risk of developing mastitis during the next lactation cycle1. Preventive treatment at dry-off has not been practiced in Norway, but selective dry cow therapy is increasingly used in Norway and other Nordic countries. This means that only cows with a high SCC and the presence of typical mastitis pathogens are treated before the dry period14.
Inappropriate use and overuse of antimicrobial agents are the main reasons for developing and spreading antimicrobial-resistant bacteria over the last decades. The recent focus on reducing antimicrobial agents in food-producing animals has shown some positive effects. In 2021, the population-weighted mean antimicrobial use in food-producing animals was lower than in humans for the first time16. This starkly contrasts with 2017, when 73% of all antimicrobials used worldwide were in animals17. Penicillin resistance amongst bacteria isolated from cases of mastitis in Norway is low10,18. Even though the usage of antimicrobial agents in Norway has been reduced over the last few decades, we know resistance is a fast-spreading issue worldwide and is considered the next pandemic. The current method used to isolate resistant bacteria in the laboratory is by cultivation on agar. However, it is well known that not all bacteria can grow under these standard laboratory conditions, as they are often optimized for the growth of the most common mastitis pathogens1. High-throughput sequencing of 16S rRNA genes has already been used on bovine milk samples to show the presence of diverse bacterial groups that often go undetected with traditional cultivation methods19,20.
In this study, we aimed to investigate whether resistant isolates were present as part of the mammary microbiome in dairy cows and how the milk microbial composition might be affected by treatment with antimicrobial agents. To answer this question, we selected cows from a farm that has historically had a healthy herd with minimal usage of antimicrobials, in vitro enriched milk samples taken aseptically from healthy udders in milk containing penicillin G or AMC and studied the surviving bacteria. In addition to the traditional cultivation method to isolate and identify antimicrobial-resistant bacteria, we also used amplicon sequencing to investigate which bacteria survived and tolerated the antimicrobial treatment. Utilizing this additional technique allowed us also to detect the genera that did not grow under standard laboratory conditions.
Results
Milk samples and study design
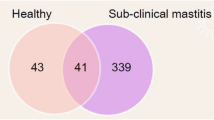
The milk samples used in this study were bovine quarter samples collected from Norwegian Red cows for a study characterizing the microbiota in milk samples from healthy udders with high (> 100,000 cells/mL) and low (< 100,000 cells/mL) somatic cell count (SCC)3. Thus, in these samples, the heightened SCC was not from quarters with clinical mastitis but could indicate subclinical mastitis and showed that quarters with a high SCC generally displayed a less stable and less diverse microbiota than quarters with a low SCC. In addition to the 45 samples from the published study, three fresh samples from three cows from the same farm were included in the current study. One of these had a low SCC (< 100,000 cells/mL), and two had high SCC (> 100,000 cells/mL). The experiment comprised 48 samples, 25 with a high SCC (H01-H25) and 23 with a low SCC (L01-L23). Once the milk samples were thawed, 0.1 mL of each sample was plated on TSA blood agar and incubated overnight (T0). After incubation, the number of colonies and the different morphologies were recorded. The results of this analysis can be found in Table 1. Milk from each sample was then inoculated in UHT milk with penicillin G or the AMC combination. To monitor the growth of the bacteria in the milk over the next three days, 0.1 mL of the milk cultures were plated on TSA blood agar daily. In the cases where an increasing number of colonies were detected over the three days, indicating that the bacteria could grow in the presence of penicillin G or AMC, colonies were inoculated in liquid BHI and kept for further analysis. The concentrations used for penicillin G (0.125 µg/mL) and AMC (0.25 µg/mL) were based on EUCAST breakpoint tables and literature21,22,23. We found bacteria that were able to tolerate one or both antimicrobial agents in 35 of the 48 samples. In total, 92% (23 of 25) of the samples with high SCC harbored resistant bacteria, and 52% (12 of 23) with low SCC harbored resistant bacteria. As amoxicillin is considered a broader spectrum antimicrobial compared to penicillin24, it was surprising that all samples except one where we isolated resistant bacteria had one or more isolates resistant to AMC, while only 20 of the 35 samples with resistant bacteria had isolates resistant to penicillin G.
Identification of the resistant isolates using MALDI-TOF MS
To identify the bacteria that survived the antimicrobial treatment, matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) was utilized. Table 1 displays an overview of the bacteria isolated from the two treatments. Seventy-six isolates were identified with MALDI-TOF MS. Six isolates (7%) were not identified. The isolates were found to be both typical mastitis pathogens such as Staphylococcus aureus, E. coli, Enterococcus faecalis, and Corynebacterium bovis, but also S. epidermidis, S. chromogenes and Streptococcus parasanguinis which might be considered to be part of the natural microbiota1,25. As evident in Table 1, many of the bacteria identified as resistant to AMC were staphylococci (69%). These results show a range of bacteria with acquired or innate resistance to both penicillin G and AMC present in the bovine udder.
The minimal inhibitory concentration of the isolates
Milk contains a range of proteins, fat and other components that might influence the effect of the antimicrobial agents. It was, therefore, necessary to investigate the MIC of the 76 isolates identified with matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) under laboratory conditions. For this purpose, the broth microdilution method recommended by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) was used21. The MIC value for each isolate was determined for the antimicrobial agent (penicillin G or AMC) in which the isolate initially proliferated. A 96-well plate with a two-fold dilution series of either penicillin G or AMC was used, and the MIC was recorded as the lowest concentration of the antimicrobial agent that completely inhibited bacterial growth after 20 hours26,27. Some isolates (3%) did not grow under the conditions in the plate reader and were excluded from the analysis. The results of the MIC assays are displayed in Fig. 1. Supplemental Table S1 contains the full overview of the MIC values for all isolates tested. The AMC combination assay showed MIC values ranging from 8 to > 64 µg/mL. The MIC for penicillin G varied from the isolates being able to tolerate low concentrations of penicillin G (< 0.06 µg/mL) up to high concentrations (> 64 µg/mL). S. epidermidis was particularly interesting. Seven out of nine isolates tested against penicillin G had a MIC at or above 64 µg/mL. The susceptibility breakpoint for penicillin G for S. aureus is ≤ 0.125 µg/mL, meaning that the S. aureus (sample H08) is considered susceptible21. Likely, bacteria that were determined to be susceptible to penicillin G in the MIC assay survived in milk with higher concentrations of penicillin G due to the protective effect of milk on the bacteria from the action of the antimicrobial agent.
Scatterplot of the minimal inhibitory concentration (MIC). (A) MIC (µg/mL) for isolates resistant to AMC (B) MIC (µg/mL) for isolates resistant to PEN. Species are separated with different colors in the plots. The asterisk indicates that the specie was isolated from a L sample. Some isolates proliferated in all the concentrations tested in the assay. The MIC was registered as > 64 µg/mL in those cases. The MIC for each isolate was determined for the antimicrobial agent the isolate initially proliferated in. The MIC value was determined as the lowest concentration of the antimicrobial agent required to completely inhibit bacterial growth after 20 h of incubation. AMC amoxicillin/clavulanic acid, PEN penicillin G.
Identification of resistant microbiota using amplicon sequencing
In addition to isolating and identifying the resistant bacteria on the agar plates, a culture-independent analysis was performed to see the overall microbial population that was enriched in milk in the presence of both antimicrobials. This was also done to identify bacteria that potentially survived the antimicrobial treatment but did not grow under our standard laboratory culturing conditions. To make sure we only amplified the 16S rRNA genes from bacteria that survived in the milk with the antimicrobial agents, we treated the samples with propidium monoazide (PMAxx) prior to amplification. This is a nucleic acid intercalating dye that is able to permeate the cell membrane of dead cells and, when activated by photolysis, covalently binds DNA and inhibits amplification by PCR28. We chose the samples where we detected resistant isolates with the traditional cultivation method and performed 16S rRNA sequencing on these samples. The alpha diversity of the amplicon data on genus level was measured as species relative abundance emphasizing species richness estimation (chao1 index, Fig. 2A,C) and evenness and dominance (Shannon diversity, Fig. 2B,D). The average chao1 index was 22.1 for the H samples (SCC > 100,000 cells/mL) and 31.3 for the L samples (SCC < 100,000 cells/mL). The average Shannon diversity was 1.6 for the H samples and 1.9 for the L samples. Statistical testing with the Kruskal-Wallis rank sum test revealed that the difference between the two groups was not significant (p > 0.05). The difference in alpha diversity between the two groups of antimicrobial agents, on the other hand, was significant (p < 0.05). The average chao1 index for samples grown with AMC was 22.0 and for samples grown with penicillin G was 30.2. The average Shannon diversity was 1.5 for samples grown with AMC and 2.18 for samples grown with penicillin G.
Alpha diversity measurements (chao1 index and shannon diversity) based on the 16S rRNA data. (A and B) compare the two diversity measurements between H (SCC > 100,000 cells/mL) and L (SCC < 100,000 cells/mL) samples, while (C and D) compare the diversity measurements between cultures grown with PEN and the AMC combination. The difference in alpha diversity between the H and L samples were not significant (p > 0.05). The difference in alpha diversity between the two treatments were significant (p < 0.05). AMC amoxicillin/clavulanic acid, PEN penicillin G.
A comparison of the effect of the antimicrobial agents on the ability of the enriched microbiota to grow in milk was done by summing up all the relative abundance from the samples within the two antimicrobial groups. Interestingly, some patterns were shown when the data were analyzed at the sequence variance (SV) level (Fig. 3). While some staphylococcal SVs remained more or less the same between the two treatments (e.g., SV_1, SV_3, SV_7, all representing S. epidermidis), some displayed a more noticeable change. In particular, SVs 6 and 8 were more abundant in the AMC cultures. A BLAST search revealed that these SVs were S. xylosus and S. chromogenes, respectively. Additional SVs that were more abundant in the AMC treated cultures included SV_4 and SV_11 corresponding to Corynebacterium bovis and SV_38 corresponding to C. amycolatum. The SVs corresponding to Enterococcus responded differently to the two antimicrobial treatments. SV_17 (E. hirae/E. faecium) and had a higher abundance after penicillin G treatment, while SV_36 (E. faecalis) had a higher abundance after AMC treatment. The SVs corresponding to Streptococcus are interesting as they are considered mastitis pathogens and how they respond to antimicrobials will affect the recovery of the cow after an infection. SV_19 displayed a stable abundance in the two treatments, while SV_22 had a reduced abundance in the AMC-treated samples compared to the penicillin G-treated samples. Taken together, this analysis shows that the AMC combination negatively affects the general microbiota in the milk, leaving Staphylococcus and Corynebacterium to make up the main abundance in these samples. This is also reflected in Table 1, where 69% of the isolates in samples treated with AMC were Staphylococcus. Also worth noting is that SV_5 (Lactococcus lactis/ L. cremoris) was not affected, or was affected equally, by the two treatments. Lactococcus species are important starter cultures in dairy fermentation29, and live suspensions of L. lactis has shown potential as an alternative treatment for antimicrobials in mastitis infections30.
To follow the longitudinal development of growth in the two treatments in the high and low SCC milk, the relative abundance of SVs based on the 16S rRNA sequencing data after 1 and 3 days of incubation with antimicrobial agents is plotted in Fig. 4. It is evident from the bar plots in Fig. 4 that the samples from quarters with a high SCC contain a larger diversity of resistant bacteria compared to the samples from quarters with a low SCC. In some samples, the same bacterial species seems to harbor resistance against both AMC and penicillin G, such as the staphylococcal SVs SV_1, SV_3 and SV_7 in samples H06, H10 and H24. This is also reflected in the alluvial plot in Fig. 3. SV_5 (Lactococcus), although found in low abundance, appears in several samples in both treatments. Some samples harbored species with treatment-dependent resistance patterns. This includes sample H01, which on day 3 displayed a high abundance of SV_1, SV_3, and SV_7 (Staphylococcus) resistant to AMC. Still, these staphylococci were absent when the sample was treated with penicillin G. Here, SV_17 (Enterococcus) was most abundant. The same was true for sample H08, which contained a high amount of SV_25 (Staphylococcus) after three days of AMC treatment, while after treatment with penicillin G SV_19 (Staphylococcus), SV_22 (Streptococcus) and SV_36 (Enterococcus) had a high abundance. In the samples taken from quarters with a low SCC the general trend was a lower diversity of resistant bacteria, specifically for the samples treated with penicillin G. The low SCC samples also contained a higher abundance of Lactococcus than the high SCC samples. This was most likely due to the lower count of resistant bacteria in these samples, allowing the Lactococcus to take up a more significant part of the relative abundance.
The relative abundance of the 20 most abundant genera plotted for each sample. The two bars for each sample represent day 1 and day 3 of antimicrobial treatment. The 16S rRNA sequencing data were rarefied at 1500 sequences and those samples with less sequences were omitted from the analysis. When only one bar was displayed, the other day had too few sequences to be included in the analysis. This was often day 3. The asterisk labels the instances where day 1 was omitted. High SCC refers to the samples with more than 100,000 somatic cells/mL, while low SCC refers to the samples with less than 100,000 somatic cells/mL. AMC amoxicillin/clavulanic acid, PEN penicillin G.
Discussion
In the literature, a common way to detect antimicrobial-resistant bacteria in bovine milk samples has been to plate the samples on agar, identify the isolates, and then test for antimicrobial resistance22,23,31,32,33,34,35. However, it is well known that not all bacteria found in bovine milk can grow with the traditional cultivation methods we use today. In this study, we wanted to use a different approach (i.e., 16S amplicon sequencing of antimicrobial-treated milk) to complement the traditional cultivation-based method. While the exact prevalence of resistance was not determined in this work, our investigation gives new insights into which bacteria survive antimicrobial treatment and demonstrates the power of using non-culture methods to monitor the presence of antimicrobial-resistant or non-susceptible bacteria in bovine milk samples. To isolate bacteria resistant to the commonly used penicillin G and AMC, we enriched milk from bovine quarters with high and low SCC in UHT milk containing penicillin G (0.125 µg/mL) or AMC (0.25 µg/mL). The concentrations used were based on the EUCAST breakpoints and, as the breakpoints are based on bacterial strains isolated from humans, literature regarding resistant strains isolated from bovine milk21,22,23. The growth of bacteria in the milk, or lack thereof, was followed by plating on blood agar daily. The bacteria that survived the treatment were identified with MALDI-TOF MS, and the MIC was determined using the standard broth microdilution method. For the detection of resistant bacteria that did not grow on blood agar and to see the effect of the antimicrobial agents on the growth of bacteria, 16S rRNA sequencing was used. Total bacteria were isolated from day 1 and day 3 of incubation with penicillin G or AMC, and all viable bacteria present in the samples were identified with sequencing. Comparing the results of resistant bacteria isolated with the traditional plating (Table 1) and 16S rRNA sequencing (Fig. 4) showed that the traditional cultivation methods can identify the most abundant species that grew with the two treatments, except Lactococcus.
Altogether, we identified a higher diversity in bacteria resistant to penicillin G than AMC. This is expected, given that AMC has a broader inhibitory spectrum than penicillin G. Still, we cannot exclude the interaction between the antimicrobial agents and the milk which might have had a different impact on the activity of penicillin G compared to AMC. Milk is a complex medium with various components that could bind to and/or sequester the antimicrobial agent and thereby reduce the efficiency. It has been shown that β-lactams bind to milk proteins, which might decrease the antimicrobial activity and spectrum36. However, whether penicillin G is affected differently than AMC in this respect is unknown. In addition, a significant proportion of the milk bacteria is associated with fat globules37,38,39. It could be speculated that the fat globules serve as partial protection against the antimicrobial agent so that the bacteria are not exposed to the concentration required to inhibit or kill. The higher alpha diversity observed for the L samples in Fig. 2A,B, despite not being significant, could be explained by the origin of the samples. The L samples are from udders with a SCC below 100,000 cells/mL and were shown to have a significantly high alpha diversity compared to samples taken from udders with a high SCC (H samples) in our previous study3. It is reasonable to assume that having a more diverse composition of bacteria in these samples would result in a more diverse community resistant to AMC and penicillin G. As amoxicillin is considered a broader spectrum antimicrobial compared to penicillin G, the higher diversity of the community after treatment with penicillin G is in line with the expected result. This also aligns with the results of the MALDI-TOF MS where we observed that a major part (69%) of the isolates resistant to AMC were staphylococci, while the isolates resistant to penicillin G were a more diverse group.
The identification of resistant bacteria from both culture-dependent and culture-independent analysis shows that the commensal species, such as S. chromogenes and S. parasanguinis, can harbor innate resistance to antimicrobial agents and/or develop resistance to the antimicrobials they are exposed to. Non-aureus staphylococci (NAS), such as S. chromogenes, are commonly found in bovine milk and cause subclinical mastitis40,41. It is a well-known phenomenon that these NAS can carry multiple resistance genes such as ampA, ermC, blaZ, and tetK making them resistant to ampicillin, erythromycin, penicillin and tetracycline42,43. Multi-resistance in these species is of particular concern as they are potentially pathogenic for humans through enterotoxin production44,45,46. It is also apparent from the results that there is a range of bacteria (labeled “other” in Fig. 4) in the milk that could tolerate the antimicrobial agents used in the study or were somehow protected from these antimicrobials by the properties of the milk. Although not surprising, this is potentially concerning as these commensal and less abundant species can become a pool of resistance genes that the pathogens can acquire when they breach the udder defenses, making an infection such as mastitis complicated to treat. If commensals and pathogens alike harbor resistance to antimicrobial agents and are protected against their activity by the milk, it might be necessary to evaluate traditional treatments against mastitis. Alternatives to the commonly used antimicrobials have been reported, including bacteriophages, antimicrobial peptides, and herbal antimicrobial substances47,48,49.
During the treatment of mastitis, most bacteria in the udder are exposed to and affected by the antimicrobial agent administered. The species that are less or not at all affected by the treatment have an ecological advantage to reestablish and dominate the microbial community and potentially affect the general udder health50,51. To date, no clinical studies have proven that the milk microbiota is beneficial for the cow’s protection against mastitis or the general health of the udder. There are, however, several studies reporting on the correlation between the bacteria commonly found in milk samples. Some commensal species can prevent the growth of mastitis pathogens by producing antimicrobial materials52,53,54. In contrast, others can modulate the host production of anti-inflammatory cytokines55. Some studies have shown that dysbiosis in the udder microbiota caused by an intramammary infection or cephalosporin treatment is reversed after the infection ends or the antimicrobial is cleared from the udder1,50. The rate of clearance and how fast the initial microbial community is reestablished are also greatly affected by the genetic composition of the cow1. However, the microbial community in the udder goes through a disruption during an infection and the following treatment, and the species less affected will be necessary for shaping the microbial community in the udder, at least for a while.
No Lactococcus were isolated with the traditional culture-dependent methods, while the 16S rRNA sequencing detected Lactococcus (SV_5) as part of the 20 most abundant genera. In the literature, Lactococcus is often isolated from bovine milk on MRS agar on 30 ℃ and not the blood TSA agar and 37 ℃ used in this project56,57. This shows that the chosen culturing method dramatically affects the isolates one finds in such experiments. In Fig. 4, SV_5 can be found in several samples from both high and low SCC quarters. The alluvial plot in Fig. 3 reveals that the relative abundance of the Lactococcus does not seem to be affected differently by the two treatments. A BLAST search revealed that SV_5 is L. lactis or L. cremoris. These are important species in dairy starter cultures, can be important in probiotics and L. lactis can produce bacteriocins that could potentially be beneficial for mastitis control30,58. As L. lactis has a positive effect on preventing mastitis development in the udder and dairy production, it seems valuable to have it survive antimicrobial treatment. As no Lactococcus were isolated using the culture-dependent method, we cannot test the MIC for this genus. Whether Lactococcus was resistant to penicillin G and AMC or protected by the milk is hence unknown. In the literature, L. lactis displays low levels of resistance to penicillin G and AMC59,60. Still, having this beneficial genus surviving in the udder despite the presence of antimicrobial agents could be beneficial for reestablishing the commensal microbiota after an infection.
S. epidermidis is, together with the other NAS species, a common cause of subclinical mastitis. As the NAS species are frequently isolated from bovine milk samples and considered to be opportunistic pathogens, S. epidermidis might be a common part of the milk microbiome51. It has been shown that S. epidermidis can produce bacteriocins that efficiently inhibit some S. agalactiae strains isolated from bovine mastitis61. This would make this species beneficial in the udder after antimicrobial treatment to modulate the growth of pathogens. SV_1, SV_3 and SV_7 all corresponded to S. epidermidis, and it was particularly interesting that these were equally affected by the two treatments. It could thus be speculated that these have a selective advantage after antimicrobial treatment and are likely part of shaping the udder microbiota after an infection.
As observed for Lactococcus, not all species will grow under the conditions in the laboratory. Culturing milk samples on blood agar before antimicrobial treatment (T0, Table 1) often resulted in growth from milk samples with high SCC and no or little growth from samples with low SCC. However, some samples displayed the opposite trend. It is possible that for samples with low SCC, the colonies that grew on blood agar were part of the contamination from the barn environment or teat skin. Even though this is unfortunate, finding antimicrobial resistance amongst bacteria that are part of the cow’s environment is interesting. These species can gain access to the udder and cause an infection, or their resistance genes can be transferred to pathogens through horizontal gene transfer. High SCC is not only an indication of bacterial infection but can also result from viral or yeast infections or trauma to the udder1. This can explain the culture negative results from samples with high SCC.
We detected several species of Staphylococcus in the AMC-treated cultures. In AMC, clavulanic acid acts as a β-lactamase inhibitor, allowing amoxicillin to retain its activity against β-lactamase expressing strains, one of staphylococci’s main β-lactam resistance mechanisms. Another major resistance mechanism against β-lactams in this family is through target modulation. These strains have been able to acquire a gene (mecA) encoding an alternative penicillin-binding protein (PBP), i.e. one of the enzymes responsible for building the cell wall and the target of β-lactams62. This means that the staphylococci do not necessarily utilize β-lactamases (which are inhibited by clavulanic acid) to confer β-lactam resistance, and clavulanic acid would thus not have the enhancing effect when administered with amoxicillin against such strains63. Furthermore, there is also evidence for the presence of so-called mec-independent oxacillin non-susceptible S. aureus (MIONSA) or borderline oxacillin resistance S. aureus (BORSA), which display phenotypic β-lactam resistance without the presence of β-lactamases or mecA64,65,66. In these cases, the non-susceptibility is normally due to mutations affecting cell wall synthesis and metabolism. We did not investigate the molecular mechanism underlying the non-susceptibility to β-lactams in the current work, but this would be of interest for future studies.
Our results show that despite being part of a healthy herd with little antimicrobial treatment, resistance against the commonly used penicillin G and AMC still occurs among strains in the mammary microbiota. Both methods used to identify resistant bacteria suggested that the major player that might have a selective advantage in reestablishing itself in the udder after antimicrobial treatment is S. epidermidis (SV_1, SV_3, and SV_7). The culture-independent method also included Lactococcus (SV_5) in this group. The study revealed that more knowledge on the effect of other antimicrobial agents and in vivo experiments are necessary to confirm these results.
Materials and methods
Study animals and sample collection
The milk samples used in this study were quarter samples collected from Norwegian Red cows selected from “The Livestock Production Research Centre” at the Norwegian University of Life Sciences with regards to a different project3. Left over milk thawed from − 80 ℃ were used in the current study. In addition, three fresh samples were taken from three different cows from the same farm. All samples included in the study were taken from healthy animals and grouped into “high” (H) or “low” (L) based on SCC below or above 100,000 cells/mL on quarter level. The total amount of samples processed were 48. The farm operates under the regulations of the Norwegian Food Safety Authority regarding food production and animal care. Permission for sample collection and use of information regarding the samples was given by the farm owners. No invasive procedures were used in this study. The cattle enrolled in the study were housed in freestalls with cubicles containing bedding materials of rubber mats with raw wood chips. Their diet consisted of silage, continuously available, and supplemented with pelleted feed based on milk production of the individual cow. The herd level SCC remained consistent from 2018 to 2023, fluctuating between a minimum of 91,000 cells/mL and a maximum of 124,000 cells/mL. Throughout this period, the herd experienced a low incidence of mastitis cases, ranging from 0.077 to 0.211. This calculation is derived by dividing the number of mastitis treatments with at least 4 days in between by the total number of year cows in the herd. Samples were collected following the “Procedure for Collecting Milk Samples” of the National Mastitis Council (NMC, www.nmconline.org) at the end of the regular milking routine as previously described51. The milking apparatus was removed, the teats were washed with iodine and then alcohol, and 200 mL of milk were collected manually in sterile glass bottles. All the operators changed gloves between samples. The samples were kept on ice and immediately transported to the laboratory, aliquoted into 50 mL falcon tubes, and stored at − 80 ℃.
Procedure used to screen milk for antimicrobial resistant isolates
The antimicrobial agent penicillin G and the antimicrobial agent/β-lactamase inhibitor combination amoxicillin/clavulanic acid (AMC) were chosen for this project as they are clinically relevant drugs67,68,69. The concentrations utilized were based on literature and EUCAST standards and were 0.125 µg/mL (penicillin G) and 0.25 µg/mL (amoxicillin/clavulanic acid)21,22,23. Upon arrival in the laboratory, 100 µl of each milk sample were plated on TSA blood agar plates (ThermoFischer Scientific, Massachusetts, United States) and incubated at 37 ℃ overnight (T0). The number of colonies on each plate and the different types of morphology were recorded. To screen for bacteria resistant to penicillin G or AMC, one mL of each milk sample was inoculated in 9 mL of UHT milk in six parallels. Three contained penicillin G with the concentration indicated above and three contained AMC. The three parallels with each antimicrobial agent were incubated at 37 ℃ for one, two, and three days. After each incubation period was finalized, 100 µl of each parallel was plated on TSA blood agar plates. When the number of colonies on TSA blood agar plates increased from day one to day three, isolates of different morphology were picked, grown in BHI broth (Oxoid), and kept for further analysis. The remaining milk from each parallel was prepared for DNA extraction and amplicon sequencing as described below.
DNA extraction and amplicon sequencing
For the identification of resistant bacteria that grew in the milk but did not appear on the blood agar plates, 16S amplicon sequencing was utilized as described previously51. In brief, the milk samples were centrifuged at 8000 × g for 5 min, and the fat layer was removed with a sterile cotton swab. After removal of the supernatant, the pellet was washed twice with 2% citrate water, dissolved in 500 µl H2O, and treated with PMAxx (Biotium) according to the manufacturer’s protocol. Finally, the DNA was extracted from each pellet using the DNeasy PowerFood Microbial Kit (Qiagen, Düsseldorf, Germany) starting from step 3 in the detailed protocol of DNeasy Powerfood Microbial Kit Handbook. To prepare the library for amplicon sequencing the V3 and V4 regions of the 16S rRNA gene were amplified with the primers Uni340F (CCTACGGGRBGCASCAG) and Bac806R (GGACTACYVGGGTATCTAAT) and reagents and conditions as previously described51. The first PCR reaction contained 1 × Q5 Hot Start High-Fidelity, 2 × Master Mix (New England Biolabs, Massachusetts, United States), 1 × EvaGreen Dye 20 × in water (Biotium, California, United States), 0.5 µM of each primer, and 3 µl of DNA in a final volume of 20 µL. In the amplification process, initial denaturation was performed at 98 ℃ for 30 s, followed by 35 cycles of denaturation at 98 ℃ for 15 s, annealing at 53 ℃ for 30 s and elongation at 72 ℃ for 20 s. The final elongation was performed at 72 ℃ for 10 min. The PCR product was purified with Agencourt AMPure XP beads (Beckman Coulter, Inc, Brea, CA, USA) according to the manufacturer’s instructions. The second PCR was performed with 4 µL of the purified PCR product to incorporate the adapters and the P5 and P7 Nextera indexes (Illumina, San Diego, CA, USA). The conditions for the second PCR were the same as above, except that the annealing temperature was 55 ℃, and 10 cycles were used. Libraries were cleaned and normalized using the SequalPrep Normalization Plate (96) Kit (ThermoFischer Scientific) and pooled together. Negative controls were included in the DNA extraction process (using only extraction kit reagents) and during library preparation (PCR-grade water). The library concentration was measured using Qubit 2 with the dsDNA HS kit (ThermoFischer Scientific), and the final sequencing was performed by Novogene on an Illumina NovaSeq platform with read lengths of 2 × 250 bp.
Sequence analysis and statistical testing
Reads were quality filtered and trimmed using the Dada2 package using truncating of forward reads set to 260 bases and reverse reads set to 240 bases70. The error model in Dada2 was created using 1 million random filtered reads. Sequence variants (SV) were inferred using the Dada2 algorithm, and the removal of chimeras was performed using the function “removeBimeraDenovo” in the Dada2 R package. Sequence variants shorter than 375 base pairs were removed from the final table. Taxonomy was assigned using the Decipher R package71 against the SILVA SSU database72. Samples with less than 1500 reads and SVs with less than 10 sequences were removed from the table. For a few of the main interesting SVs, a search against the rRNA/ITS database at NCBI was performed using BLAST tool73. The name of the species with the highest % similarity was then retrieved and, in case two or more species had the same % similarity, all the species names were used. Alpha diversity was calculated using the Vegan package in R as described previously3,74. A pairwise comparison of the alpha diversity indexes between group levels was performed using the Kruskal–Wallis rank sum test. The alluvial plot was created with the Alluvial package in R.
Identification of isolated bacteria with MALDI-TOF MS
The isolates that grew on TSA blood agar after inoculating milk samples in UHT milk with antimicrobial agents were identified using MALDI-TOF MS75. For this purpose, a colony of the isolate to be identified was transferred from TSA blood agar to a VITEK MS-DS slide (BioMerieux) and 1 µl VITEK MS CHCA matrix was applied on top. Ionization and mass analysis were done in the VITEK MS instrument with E. coli ATCC 8739 as a reference strain. The resulting peptide mass fingerprints were compared to the VITEK MS Expanded V3.2 Database and the results with a confidence value > 98% were considered identified.
Minimal inhibitory concentration assays
Determination of MIC was performed on the isolates that were identified using MALDI-TOF MS. For this purpose, the broth microdilution method was utilized21. Briefly, a two-fold dilution series of penicillin G and AMC in 96 well microtiter plates with Hinton-Mueller broth were used. The dilutions used for both antimicrobial agents were (in µg/mL) 64, 32, 16, 8, 4, 2, 1, 0.5, 0.25, 0.125, 0.062. Wells without antimicrobial agents were included for each isolate. The microtiter plates were incubated at 37 ℃ in a Synergy H1 hybrid reader (BioTek) and OD600 was recorded every 10 min for 20 h. The MIC was recorded as the first well with severely reduced growth after 20 hours22,23.
Data availability
The 16S amplicon data is available in the EBI repository, https://www.ebi.ac.uk/, with accession number PRJEB70316.
References
Derakhshani, H. et al. Invited review: Microbiota of the bovine udder: Contributing factors and potential implications for udder health and mastitis susceptibility. J. Dairy Sci. 101, 10605–10625 (2018).
Sharun, K. et al. Advances in therapeutic and managemental approaches of bovine mastitis: A comprehensive review. Vet. Q. 41, 107–136 (2021).
Winther, A. R. et al. Longitudinal dynamics of the bovine udder microbiota. Animal Microbiome 4, 1–10 (2022).
Wang, N. et al. Mechanisms by which mastitis affects reproduction in dairy cow: A review. Reprod. Domest. Anim. 56, 1165–1175 (2021).
Niedziela, D. A., Murphy, M. P., Grant, J., Keane, O. M. & Leonard, F. C. Clinical presentation and immune characteristics in first-lactation Holstein-Friesian cows following intramammary infection with genotypically distinct Staphylococcus aureus strains. J. Dairy Sci. 103, 8453–8466 (2020).
Yang, W. et al. Bovine TLR2 and TLR4 properly transduce signals from Staphylococcus aureus and E. coli, but S. aureus fails to both activate NF-κB in mammary epithelial cells and to quickly induce TNFα and interleukin-8 (CXCL8) expression in the udder. Mol. Immunol. 45, 1385–1397 (2008).
Suojala, L., Kaartinen, L. & Pyörälä, S. Treatment for bovine Escherichia coli mastitis–an evidence-based approach. J. Vet. Pharmacol. Ther. 36, 521–531 (2013).
Oliveira, L. & Ruegg, P. Treatments of clinical mastitis occurring in cows on 51 large dairy herds in Wisconsin. J. Dairy Sci. 97, 5426–5436 (2014).
Ganda, E. K. et al. Normal milk microbiome is reestablished following experimental infection with Escherichia coli independent of intramammary antibiotic treatment with a third-generation cephalosporin in bovines. Microbiome 5, 1–17 (2017).
Smistad, M., Bakka, H. C., Sølverød, L., Jørgensen, H. J. & Wolff, C. Prevalence of udder pathogens in milk samples from Norwegian dairy cows recorded in a national database in 2019 and 2020. Acta Vet. Scand. 65, 19 (2023).
Statens Legemiddelverk. Terapianbefaling - bruk av antibakterielle midler til matproduserende dyr. <https://legemiddelverket.no/veterinermedisin/terapianbefalinger/bruk-av-antibakterielle-midler-til-matproduserende-dyr/terapianbefalinger-for-storfe> (2022).
Gruet, P., Maincent, P., Berthelot, X. & Kaltsatos, V. Bovine mastitis and intramammary drug delivery: Review and perspectives. Adv. Drug Deliv. Rev. 50, 245–259 (2001).
Belmar-Liberato, R., Gonzalez-Canga, A., Tamame-Martin, P. & Escribano-Salazar, M. Amoxicillin and amoxicillin-clavulanic acid resistance in veterinary medicine–the situation in Europe: A review. Vet. Med. 56, 473 (2011).
Rajala-Schultz, P., Nødtvedt, A., Halasa, T. & Persson Waller, K. Prudent use of antibiotics in dairy cows: The Nordic approach to udder health. Front. Vet. Sci. 8, 623998 (2021).
Hillerton, E., Bryan, M., Biggs, A., Berry, E. & Edmondson, P. Time to standardise dry cow therapy terminology. Vet. Record 180, 301–302 (2017).
European Centre for Disease Prevention and Control (ECDC), European Food Safety Authority (EFSA) and European Medicines Agency (EMA). Third joint inter-agency report on integrated analysis of consumption of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from humans and food-producing animals in the EU/EEA, JIACRA III. 2016–2018. (2021).
Mulchandani, R., Wang, Y., Gilbert, M. & Van Boeckel, T. P. Global trends in antimicrobial use in food-producing animals: 2020 to 2030. PLoS Global Public Health 3, e0001305 (2023).
Østerås, O. Helsekortordningen Storfe 2018 - Statistikksamling. https://www.animalia.no/contentassets/36db1ac2b4f14ec9acc74eea3457ce0e/arsrapport_helsekortordningen_-2018.pdf (2019).
Kuehn, J. S. et al. Bacterial community profiling of milk samples as a means to understand culture-negative bovine clinical mastitis. PloS ONE 8, e61959 (2013).
Oikonomou, G. et al. Microbiota of cow’s milk; distinguishing healthy, sub-clinically and clinically diseased quarters. PloS ONE 9, e85904 (2014).
The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 13.0,. http://www.eucast.org. (2023).
Bolte, J., Zhang, Y., Wente, N. & Krömker, V. In vitro susceptibility of mastitis pathogens isolated from clinical mastitis cases on northern German dairy farms. Vet. Sci. 7, 10 (2020).
McDougall, S., Hussein, H. & Petrovski, K. Antimicrobial resistance in Staphylococcus aureus, Streptococcus uberis and Streptococcus dysgalactiae from dairy cows with mastitis. N. Z. Vet. J. 62, 68–76 (2014).
Soares, G. M. S. et al. Mechanisms of action of systemic antibiotics used in periodontal treatment and mechanisms of bacterial resistance to these drugs. J. Appl. Oral Sci. 20, 295–309 (2012).
De Buck, J. et al. Non-aureus staphylococci and bovine udder health: Current understanding and knowledge gaps. Front. Vet. Sci. 8, 658031 (2021).
Andrews, J. M. Determination of minimum inhibitory concentrations. J. Antimicrob. Chemother. 48, 5–16 (2001).
EUCAST. Reading Guide for Broth Microdilution, version 4.0. (Eucast.org, 2022).
Nocker, A., Cheung, C.-Y. & Camper, A. K. Comparison of propidium monoazide with ethidium monoazide for differentiation of live vs. dead bacteria by selective removal of DNA from dead cells. J. Microbiol. Methods 67, 310–320 (2006).
Casalta, E. & Montel, M.-C. Safety assessment of dairy microorganisms: The Lactococcus genus. Int. J. Food Microbiol. 126, 271–273 (2008).
Klostermann, K. et al. Intramammary infusion of a live culture of Lactococcus lactis for treatment of bovine mastitis: Comparison with antibiotic treatment in field trials. J. Dairy Res. 75, 365–373 (2008).
Abdi, R. D. et al. Antimicrobial resistance of Staphylococcus aureus isolates from dairy cows and genetic diversity of resistant isolates. Foodborne Pathog. Dis. 15, 449–458 (2018).
Cheng, J. et al. Antimicrobial resistance profiles of 5 common bovine mastitis pathogens in large Chinese dairy herds. J. Dairy Sci. 102, 2416–2426 (2019).
Denamiel, G., Llorente, P., Carabella, M., Rebuelto, M. & Gentilini, E. Anti-microbial susceptibility of Streptococcus spp. isolated from bovine mastitis in Argentina. J. Vet. Med. Ser. B 52, 125–128 (2005).
Kalayu, A. A. et al. Burden and antimicrobial resistance of S. aureus in dairy farms in Mekelle Northern Ethiopia. BMC Vet. Res. 16, 1–8 (2020).
Thomas, V. et al. Antimicrobial susceptibility monitoring of mastitis pathogens isolated from acute cases of clinical mastitis in dairy cows across Europe: VetPath results. Int. J. Antimicrob. Agents 46, 13–20 (2015).
Grunwald, L. & Petz, M. Food processing effects on residues: Penicillins in milk and yoghurt. Anal. Chim. Acta 483, 73–79 (2003).
Jiménez-Flores, R. & Brisson, G. The milk fat globule membrane as an ingredient: Why, how, when?. Dairy Sci. Technol. 88, 5–18 (2008).
Ly, M., Vo, N., Le, T., Belin, J.-M. & Waché, Y. Diversity of the surface properties of Lactococci and consequences on adhesion to food components. Colloids Surf. B Biointerfaces 52, 149–153 (2006).
Brisson, G., Payken, H. F., Sharpe, J. P. & Jiménez-Flores, R. Characterization of Lactobacillus reuteri interaction with milk fat globule membrane components in dairy products. J. Agric. Food Chem. 58, 5612–5619 (2010).
Bertelloni, F. et al. Detection of genes encoding for enterotoxins, TSST-1, and biofilm production in coagulase-negative staphylococci from bovine bulk tank milk. Dairy Sci. Technol. 95, 341–352 (2015).
Turchi, B. et al. Coagulase negative staphylococci from ovine milk: Genotypic and phenotypic characterization of susceptibility to antibiotics, disinfectants and biofilm production. Small Rumin. Res. 183, 106030 (2020).
Fišarová, L., Pantůček, R., Botka, T. & Doškař, J. Variability of resistance plasmids in coagulase-negative staphylococci and their importance as a reservoir of antimicrobial resistance. Res. Microbiol. 170, 105–111 (2019).
Argudín, M. A., Vanderhaeghen, W. & Butaye, P. Diversity of antimicrobial resistance and virulence genes in methicillin-resistant non-Staphylococcus aureus staphylococci from veal calves. Res. Vet. Sci. 99, 10–16 (2015).
Balaban, N. & Rasooly, A. Analytical chromatography for recovery of small amounts of staphylococcal enterotoxins from food. Int. J. Food Microbiol. 64, 33–40 (2001).
Chen, M. et al. Molecular Mechanism of Staphylococcus xylosus resistance against tylosin and florfenicol. Infect. Drug Resist. https://doi.org/10.2147/IDR.S379264 (2022).
Raspanti, C. G. et al. Prevalence and antibiotic susceptibility of coagulase-negative Staphylococcus species from bovine subclinical mastitis in dairy herds in the central region of Argentina. Rev. Argent. de Microbiol. 48, 50–56 (2016).
Shin, B. & Park, W. Zoonotic diseases and phytochemical medicines for microbial infections in veterinary science: Current state and future perspective. Front. Vet. Sci. 5, 166 (2018).
Cao, L., Wu, J., Xie, F., Hu, S. & Mo, Y. Efficacy of nisin in treatment of clinical mastitis in lactating dairy cows. J. Dairy Sci. 90, 3980–3985 (2007).
Ngassam-Tchamba, C. et al. In vitro and in vivo assessment of phage therapy against Staphylococcus aureus causing bovine mastitis. J. Global Antimicrob. Resist. 22, 762–770 (2020).
Ganda, E. K. et al. Longitudinal metagenomic profiling of bovine milk to assess the impact of intramammary treatment using a third-generation cephalosporin. Sci. Rep. 6, 37565 (2016).
Porcellato, D., Meisal, R., Bombelli, A. & Narvhus, J. A. A core microbiota dominates a rich microbial diversity in the bovine udder and may indicate presence of dysbiosis. Sci. Rep. 10, 1–14 (2020).
Braem, G. et al. Antibacterial activities of coagulase-negative staphylococci from bovine teat apex skin and their inhibitory effect on mastitis-related pathogens. J. Appl. Microbiol. 116, 1084–1093 (2014).
Woodward, W., Besser, T., Ward, A. & Corbeil, L. In vitro growth inhibition of mastitis pathogens by bovine teat skin normal flora. Can. J. Vet. Res. 51, 27 (1987).
Isaac, P. et al. Commensal coagulase-negative Staphylococcus from the udder of healthy cows inhibits biofilm formation of mastitis-related pathogens. Vet. Microbiol. 207, 259–266 (2017).
Bouchard, D. S. et al. Lactic acid bacteria isolated from bovine mammary microbiota: Potential allies against bovine mastitis. PloS ONE 10, e0144831 (2015).
Alharbi, K. N. & Alsaloom, A. N. Characterization of lactic bacteria isolated from raw milk and their antibacterial activity against bacteria as the cause of clinical bovine mastitis. J. Food Qual. 2021, 1–8 (2021).
Taye, Y., Degu, T., Fesseha, H. & Mathewos, M. Isolation and identification of lactic acid bacteria from cow milk and milk products. Sci. World J. https://doi.org/10.1155/2021/4697445 (2021).
Furtado, D. N., Todorov, S. D., Landgraf, M., Destro, M. T. & Franco, B. D. Bacteriocinogenic Lactococcus lactis subsp. lactis DF04Mi isolated from goat milk: Characterization of the bacteriocin. Braz. J. Microbiol. 45, 1541–1550 (2014).
Sorge, U. S., Huber-Schlenstedt, R. & Schierling, K. In vitro antimicrobial resistance profiles of Streptococcus uberis, Lactococcus spp., and Enterococcus spp. from quarter milk samples of cows between 2015 and 2019 in Southern Germany. J. Dairy Sci. 104, 5998–6012 (2021).
Plumed-Ferrer, C. et al. Antimicrobial susceptibilities and random amplified polymorphic DNA-PCR fingerprint characterization of Lactococcus lactis ssp. lactis and Lactococcus garvieae isolated from bovine intramammary infections. J. Dairy Sci. 98, 6216–6225 (2015).
dos Santos Nascimento, J., Fagundes, P. C., de Paiva Brito, M. A. V., Dos Santos, K. R. N. & de Freire Bastos, Md. C. Production of bacteriocins by coagulase-negative staphylococci involved in bovine mastitis. Vet. Microbiol. 106, 61–71 (2005).
Fuda, C., Fisher, J. & Mobashery, S. β-Lactam resistance in Staphylococcus aureus: The adaptive resistance of a plastic genome. Cell. Mol. Life Sci. 62, 2617–2633 (2005).
Chambers, H. F. Solving staphylococcal resistance to β-lactams. Trends Microbiol. 11, 145–148 (2003).
Giulieri, S. G. Case commentary: The hidden side of oxacillin resistance in Staphylococcus aureus. Antimicrob. Agents Chemother. 67, e00716-00723 (2023).
Hess, K. A. et al. Failure of mecA/mecC PCR testing to accurately predict oxacillin resistance in a patient with Staphylococcus aureus infective endocarditis. Antimicrob. Agents Chemother. 67, e00437-00423 (2023).
Hryniewicz, M. M. & Garbacz, K. Borderline oxacillin-resistant Staphylococcus aureus (BORSA)–a more common problem than expected?. J. Med. Microbiol. 66, 1367–1373 (2017).
McDougall, S., Clausen, L., Hintukainen, J. & Hunnam, J. Randomized, controlled, superiority study of extended duration of therapy with an intramammary antibiotic for treatment of clinical mastitis. J. Dairy Sci. 102, 4376–4386 (2019).
MacDiarmid, S. Antibacterial drugs used against mastitis in cattle by the systemic route. N. Z. Vet. J. 26, 290–295 (1978).
Ajose, D. J. et al. Combating bovine mastitis in the dairy sector in an era of antimicrobial resistance: Ethno-veterinary medicinal option as a viable alternative approach. Front. Vet. Sci. 9, 287 (2022).
Callahan, B. J. et al. DADA2: High-resolution sample inference from Illumina amplicon data. Nat. Methods 13, 581–583 (2016).
Murali, A., Bhargava, A. & Wright, E. S. IDTAXA: A novel approach for accurate taxonomic classification of microbiome sequences. Microbiome 6, 1–14 (2018).
Quast, C. et al. The SILVA ribosomal RNA gene database project: Improved data processing and web-based tools. Nucleic Acids Res. 41, D590–D596 (2012).
Camacho, C. et al. BLAST+: Architecture and applications. BMC Bioinform. 10, 1–9 (2009).
Dixon, P. VEGAN, a package of R functions for community ecology. J. Veg. Sci. 14, 927–930 (2003).
Singhal, N., Kumar, M., Kanaujia, P. K. & Virdi, J. S. MALDI-TOF mass spectrometry: An emerging technology for microbial identification and diagnosis. Front. Microbiol. 6, 791 (2015).
Acknowledgements
Thanks to the Centre for Livestock Production at the Norwegian University of Life Sciences for sampling. Thanks to Tine SA for delivering the individual cow data obtained from the Norwegian Cattle Health Recording System.
Funding
This work received financial contributions from the Norwegian Foundation for Research Levy on Agricultural Products (FFL) and the Norwegian Agricultural Agreement Research Fund (JA) (Grant No. 267623), the Norwegian Research Council (Grant No. 314733), JPI-AMR grant from the Research Council of Norway (Grant No. 296906), and the Faculty of Chemistry, Biotechnology and Food Science at the Norwegian University of Life Sciences.
Author information
Authors and Affiliations
Contributions
Anja Ruud Winther: planned project, collected data, laboratory work, analysis of data, wrote the paper. Aurelie Perrin: collected data, laboratory work. Anne O. O. Nordraak: collected data, laboratory work. Morten Kjos: planned project, wrote the paper. Davide Porcellato: planned project, analysis of data, wrote the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Winther, A.R., Perrin, A., Nordraak, A.O.O. et al. An in vitro evaluation of the effect of antimicrobial treatment on bovine mammary microbiota. Sci Rep 14, 18333 (2024). https://doi.org/10.1038/s41598-024-69273-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69273-y
- Springer Nature Limited