Abstract
Myopia is a growing concern worldwide, especially among adolescents. This study aimed to investigate the prevalence and associated factors of myopia in adolescents aged 12–15 in Shandong Province, China. This cross-sectional study adhered to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines and involved stratified random cluster sampling of 128,678 students from 186 middle schools across 17 cities in Shandong Province. Data collection was conducted from March to April 2024. We excluded students with organic eye diseases, abnormal binocular vision functions, or a history of eye injuries or surgeries. Myopia was assessed using the standard logarithmic visual acuity chart and autorefractor without inducing ciliary muscle paralysis. A comprehensive questionnaire survey was conducted to gather demographic characteristics and daily life behaviors. With the chi-squared test for univariable analysis and multivariable logistic regression for identifying significant factors. This study included 126,375 participants, with a gender distribution of 51.02% male and 48.98% female. The overall prevalence of myopia was 71.34%. Higher prevalence was observed in girls (72.26%) compared to boys (70.45%), and the prevalence increased with age, peaking at 73.12% in 15-year-olds. Urban residents had a higher prevalence (71.86%) than rural (70.39%). Factors such as increased frequency of eye usage while lying down or leaning forward, frequent use of eyes while walking or riding in a car, prolonged screen time, and extended homework duration were associated with higher odds of developing myopia. Conversely, higher frequency of outdoor exercise, maintaining proper posture during reading and writing, greater distance from eyes to screen, and longer sleep duration were associated with lower odds. Additionally, female gender, older age, urban residence, and parental history of myopia increased the risk. The high prevalence of myopia among adolescents in Shandong Province was influenced by a combination of demographic, behavioral, and environmental factors. The study highlighted the importance of lifestyle modifications, such as increasing outdoor activities and maintaining proper visual habits, limiting the duration of screen exposure and homework sessions, and extending sleep duration, to mitigate the risk of developing myopia. These findings underscored the need for targeted public health interventions and educational campaigns to address this significant public health issue.
Similar content being viewed by others
Introduction
With the rapid development of socio-economics, people’s lifestyles have undergone significant changes. The fast-paced life and the emergence of electronic devices have not only brought immense pressure to our daily lives but also provided convenience. However, at the same time, the increased hours spent on work and study have brought about numerous negative effects, especially for adolescents. This has led to a significant rise in myopia among youths, presenting a new challenge to public health and individual well-being. Myopia is a refractive defect of the eye that causes light to focus in front of, rather than on, the retina, usually because the axial length of the eye is too long. As a result,distant objects appear blurred and close objects appear clearly1. Myopia can have its symptoms mitigated through the use of spectacles2, contact lenses3, or through refractive surgeries4. However, regardless of these methods of vision correction, there remains an increased risk of serious eye complications that can lead to blindness. These complications include conditions like retinal detachment5, glaucoma6, and myopic maculopathy7, which are more likely to occur in cases of high myopia due to the elongation of the eye’s axial length. Myopia is one of the leading causes of distance impairment worldwide8, and its prevalence is increasing rapidly9,10,11,12, which has deleterious ramifications for the quality of life and economic health of individuals and nations as a whole13,14. In 2020, it was estimated that approximately 30% of the adult global population was affected by myopia, a significant public health concern11. Moreover, it has been projected that by the year 2050, myopia may afflict nearly half of the global population unless effective intervention strategies are implemented15. Notably, the progression of myopia is most rapid during adolescence16, highlighting this period as crucial for myopia prevention efforts. It is important to note that rapid economic development in East and Southeast Asia has led to significant shifts in ocular and physical activity behaviors, exacerbating the issue of myopia among adolescents in these regions17. In parts of East and Southeast Asia, the prevalence of myopia has been reported to reach approximately 80–90% among senior high school students18, underscoring the urgent need for targeted myopia control measures in these demographic groups.
In summary, it is increasingly evident that in regions like East and Southeast Asia, and indeed globally, we are encountering a mounting public health challenge: the prevalence of myopia among adolescents. This issue represents a critical concern requiring immediate attention and effective action. Prioritizing the eye health of our young population is in line with the third goal of the United Nations’ Sustainable Development Goals for 2030, which aims to ensure healthy lives and promote well-being for all at all ages19. The aim of this study was to explore the prevalence and associated risk factors of myopia in adolescents aged 12–15 in Shandong Province. The findings from this research were expected to deepen our understanding of myopia in this specific age group and geographical area, and would offer valuable insights for the creation of effective prevention and treatment strategies tailored to these young individuals.
Materials and methods
Design and participants
This study adhered to the guidelines of Strengthening the Reporting of Observational Studies in Epidemiology20. Employing a stratified random cluster sampling approach, we selected students aged 12–15 from 186 middle schools across 17 cities in Shandong Province, China, as our research participants. The study was conducted between March and April 2024. The sampling process involved stratifying students by grade, followed by random selection of entire classes as sampling units. In total, 128,678 students were surveyed.
From this group, we excluded students with organic eye diseases, abnormal binocular vision functions, and those with a history of eye injuries or surgeries. Ultimately, 126,375 students completed the myopia examination and questionnaire, leading to a 98.21% validity rate. The gender distribution among valid respondents was 51.02% male (64,471 individuals) and 48.98% female (61,904 individuals). Age distribution was as follows: 20.64% (26,078 individuals) were 12 years old, 24.99% (31,581 individuals) were 13 years old, 25.53% (32,263 individuals) were 14 years old, and 28.85% (36,453 individuals) were 15 years old. The average age of the participants was 13.63 ± 1.106 years.
Measurement of myopia and questionnaire survey
All participants and investigators received thorough training, guaranteeing precise measurements of visual acuity, as well as a comprehensive understanding of field epidemiological techniques. Prior to the initiation of the survey, students were comprehensively briefed about the study’s objectives and the potential impact of the findings. Following the vision test, students were provided with detailed questionnaires. They were given a full day to discuss these with their parents before submission, ensuring thoughtful and informed responses. Once collected, the questionnaires were systematically organized and the data was quickly entered for in-depth analysis. All procedures strictly adhered to relevant guidelines and regulations, and written informed consent was duly obtained from every participant involved in the study, and for minors (below age 16), informed consent was obtained from their parents and/or legal guardians.
The evaluation of the students’ left and right eyes’ naked eye visual acuity was conducted using the standard logarithmic visual acuity chart in conjunction with autorefractor model HRK-7000A (HUVITZ Corporation, Anshan, the Republic of Korea), performed without inducing ciliary muscle paralysis. The criteria established for identifying myopia stipulated that a standard logarithmic visual acuity below 5.0 in the naked eye, combined with a spherical equivalent of less than − 0.50D as determined by autorefractor under non-ciliary muscle paralysis conditions, would classify an individual as myopic. In this assessment, any student diagnosed with myopia in at least one eye was included in the overall count of myopia cases21. The questionnaire section was conducted anonymously, with the survey content specifically including: Demographic characteristics: gender, age, family annual income (yuan), place of residence (classified according to the hukou system), parents’ education level, parents’ myopia condition; Daily life behaviors: frequency of using eyes while lying down or leaning forward, frequency of using eyes while walking or riding in the car, frequency of outdoor exercise weekly, proper posture for reading and writing, distance from eyes to television screen (meter), distance from eyes to computer screen (centimeter), screen duration on smart phone and computer daily (hour), watching television duration daily (hour), homework duration daily (hour), sleep duration daily (hour).
Statistical analysis
A database was meticulously developed utilizing EpiData version 3.1 (EpiData Association, Odense, the Kingdom of Denmark). Subsequent data analysis was adeptly performed using the Statistical Product and Service Solutions version 27.0 (International Business Machines Corporation, New York, the United States of America). In terms of data representation, continuous variables were precisely detailed as means and standard deviations, while categorical variables were elucidated through the number of cases and their corresponding percentages (%). For the univariable analysis, the chi-squared (χ2) test was employed. Significantly distinguished variables (P < 0.05) from this univariable analysis phase were subsequently integrated into the multivariable logistic regression analysis22. The subsequent stage of our investigation implemented a logistic regression analysis, adeptly yielding results quantified by odds ratios (OR) and further augmented by 95% confidence intervals (CI) to precisely delineate the accuracy of our estimations. In our commitment to uphold the integrity of our findings, we conducted a thorough evaluation of the logistic regression model’s fit, under the guidance of the Hosmer–Lemeshow test. This rigorous approach not only substantiated the validity of our model but also reinforced the robustness of our analytical framework, anchored firmly in the principles of statistical rigor and precision.
Ethics statement
This study received ethical approval from the Ethics Committee of Shandong Institute of Petroleum and Chemical Technology (registration number: KY-2024-006).
Results
The epidemiological characteristics of myopia prevalence among adolescents in Shandong Province
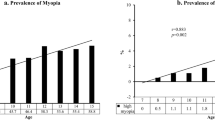
According to a myopia prevalence survey conducted in 2023 among adolescents aged 12–15 in Shandong Province, the overall prevalence of myopia was found to be 71.34%. When analyzed by gender, the data revealed a slightly higher incidence in girls at 72.26%, compared to 70.45% in boys, a difference that was statistically significant (P < 0.05). Age also appeared to be a contributing factor. The highest myopia prevalence was observed in 15-year-olds at 73.12%, followed by 14-year-olds at 72.10%, 13-year-olds at 70.46%, and 12-year-olds at 68.97%. This variation across different age groups was statistically significant (P < 0.05). Place of residence was another determinant. Adolescents living in urban areas had a higher myopia prevalence (71.86%) than those in rural areas (70.39%), with this difference also being statistically significant (P < 0.05). Additionally, parents’ myopia condition influenced the prevalence in children. The prevalence was 69.95% when neither parent had myopia, increased to 72.02% if one parent was affected, and rose further to 73.46% if both parents were myopic, with this difference also being statistically significant (P < 0.05) (Table 1).
Univariable analysis of myopia prevalence in adolescents from Shandong Province
The univariable analysis revealed that a range of factors were closely associated with the prevalence of myopia in adolescents aged 12–15. These factors included frequency of using eyes while lying down or leaning forward, frequency of using eyes while walking or riding in the car, frequency of outdoor exercise weekly, proper posture for reading and writing, distance from eyes to television screen (meter), distance from eyes to computer screen (centimeter), screen duration on smart phone and computer daily (hour), homework duration daily (hour), sleep duration daily (hour) (P < 0.05) (Table 2).
Multivariable analysis of myopia prevalence in adolescents from Shandong Province
Using the results of the students’ visual condition (0 = normal vision, 1 = myopia) as the dependent variable, and according to the inclusion and exclusion criteria (P = 0.05), a total of 13 independent variables were included in the multivariable logistic regression analysis: gender, age, place of residence, parents’ myopia condition, frequency of using eyes while lying down or leaning forward, frequency of using eyes while walking or riding in the car, frequency of outdoor exercise weekly, proper posture for reading and writing, distance from eyes to television screen (meter), distance from eyes to computer screen (centimeter), screen duration on smart phone and computer daily (hour), homework duration daily (hour), sleep duration daily (hour). Subsequent to the analytical rigour imparted by the Hosmer–Lemeshow test, the logistic regression model exhibited a commendable degree of fit (P > 0.05). Several determinants have been identified that decreased the odds of developing myopia. Adolescents who engaged in outdoor exercise 3–5 times weekly (OR 0.928, 95% CI 0.898–0.958) and more than five times weekly (OR 0.927, 95% CI 0.882–0.975) had shown reduced odds compared to those engaging less than three times. Proper posture for reading and writing also contributed to lower odds (OR 0.959, 95% CI 0.922–0.998) than not maintaining proper posture. Keeping a distance of 50 centimeters or more from the computer screen (OR 0.970, 95% CI 0.945–0.996) was associated with lower odds than a distance of less than 50 centimeters. Sleep duration of 6–8 h (OR 0.921, 95% CI 0.885–0.958) and over 8 h (OR 0.896, 95% CI 0.860–0.933) both resulted in decreased odds compared with sleeping less than 6 h. Conversely, some factors have been identified that increased the odds of myopia. Female adolescents presented higher odds (OR 1.093, 95% CI 1.066–1.120) compared with males. Ages of 13 (OR 1.072, 95% CI 1.035–1.111), 14 (OR 1.163, 95% CI 1.122–1.205), and 15 years (OR 1.222, 95% CI 1.180–1.265) showed increased odds compared with 12-year-olds. Urban living was associated with increased odds (OR 1.076, 95% CI:1.049–1.103) compared with rural living. The risk further escalated when one parent had myopia (OR 1.105, 95% CI 1.075–1.136) and even more when both parents were myopic (OR 1.191, 95% CI:1.151–1.231). Using eyes while lying down or leaning forward often (OR 1.043, 95% CI 1.009–1.077) and always (OR 1.066, 95% CI 1.017–1.118) increased the odds compared with never doing so. Similarly, using eyes while walking or riding in the car often (OR 1.044, 95% CI 1.009–1.080) and always (OR 1.105, 95% CI 1.062–1.150) was associated with higher odds compared with never. Screen duration of more than 3 h daily on smart phone and computer (OR 1.061, 95% CI 1.019–1.104) resulted in higher odds compared with less than an hour. Finally, engaging in homework for more than 3 h daily increased the odds (OR 1.043, 95% CI 1.011–1.077) compared with less than an hour (Table 3).
Disussion
In the Shandong Province, a significant proportion of adolescents aged 12–15 are affected by myopia, with specific lifestyle factors contributing to its prevalence. Our study revealed that frequent engagement in outdoor exercise significantly reduced the odds of developing myopia. Proper posture for reading and writing, maintaining an appropriate distance from computer screen, and ensuring adequate sleep duration also decreased the risk. Conversely, female adolescents, those older adolescents, urban residents, and adolescents with myopic parents faced higher odds of developing myopia. Frequent improper use of eyes, such as lying down or leaning forward, walking or riding in the car, and prolonged exposure to screen on smartphone and computer, as well as extensive periods of doing homework further elevated the risk. These findings underscore the importance of targeted preventive measures and early interventions tailored to these identified risk factors to mitigate the rising incidence of myopia among adolescents.
The present study uncovered gender disparities in the prevalence of myopia, observing a marginally higher incidence in female adolescents compared to their male counterparts, a finding that aligned with previous research23. This discrepancy may be attributed to differences in physiological changes experienced during adolescence between genders. Notably, significant choroidal thinning, which is linked to the rapid progression of myopia, has been reported to be more pronounced in females24. Furthermore, the correlation between serum sex hormone levels and the onset and progression of myopia in adolescents has been established. Studies have shown that levels of follicle-stimulating hormone and luteinizing hormone were higher in females than in males, potentially contributing to the observed variations in myopia rates between the sexes25. In addition, a specific form of severe myopia, which is exclusive to females and characterized by central macula dysfunction, has been identified as a monogenic genetic disorder caused by mutations in the ARR3 gene26. This emerging evidence underscored the importance of considering gender-specific factors in the study and management of myopia.
This study identified age as a critical determinant in the prevalence of myopia among adolescents. Consistent with prior findings27, our data indicated that the rate of myopia tended to increase with age in adolescents. The adolescent period is characterized by rapid growth and significant developmental changes in the human body28, which include physiological transformations impacting vision. This phase is particularly vital for the development of the visual system, marking adolescence as a period of increased susceptibility29. During this time, the ocular structure undergoes continued development, becoming more receptive to external environmental influences. As adolescents age, their increased engagement in activities and environments conducive to myopia can exacerbate the risk. This heightened exposure, combined with the eye’s enhanced sensitivity during this phase, is associated with the elongation of the eyeball30, potentially accelerating the onset and progression of myopia.
In the current study, a significant variation in myopia risk was identified based on family location, with urban areas exhibiting a higher prevalence compared to rural regions. This observation aligned with similar findings demonstrating elevated rates of myopia among urban adolescents relative to their rural counterparts31. The disparity in myopia incidence between urban and rural settings is complex and may be attributed to differences in population densities. Nevertheless, it is essential to recognize that the etiology of myopia extends beyond mere geographical factors. It encompasses a combination of environmental and behavioral influences32,33. Children in urban areas often have the advantage of better economic conditions compared to rural areas. This economic disparity allows urban children access to environments that might inadvertently increase their risk of developing myopia16. Such environments often promote extended periods of ocular exertion, which may significantly contribute to the observed variance in myopia prevalence between urban and rural children.
This study highlighted the significant role of parental myopia in the development of myopia among adolescents. Corresponding with similar research, it was noted that children with one or both parents affected by myopia were at a greater risk of developing the condition themselves34. The influence of genetics on adolescent myopia is indisputably substantial35. Further investigations have identified specific genetic markers that correlated with an increased risk of myopia36. A history of myopia in parents or other family members is indicative of an elevated likelihood of adolescents inheriting these genetic predispositions. Although these genetic factors do not inevitably lead to the development of myopia, they significantly increase the susceptibility to this condition in adolescents.
The current study identified the use of eyes in positions such as lying down or leaning forward as a contributing factor to myopia in adolescents. This aligned with recent research indicating that frequently adopting such postures was a risk factor for adolescent myopia37. These postures necessitate extra effort to control eye movements for focusing, resulting in continuous strain on ocular muscles. This sustained tension can lead to visual fatigue and potentially precipitate the onset of nearsightedness.
This research highlighted that engaging in visual tasks while walking or riding in the car, a behavior frequently observed among adolescents, played a significant role in the onset and progression of myopia. Parallel findings have identified this practice as a risk factor for adolescent myopia38. This practice is characterized by the challenge of maintaining a stable visual focus. The eyes are required to continuously adapt to varying distances and shifting focal points, leading to an increased demand for ocular adjustments.
This study underscored the potential of outdoor exercise in mitigating myopia risk. Similar research supported the protective role of outdoor physical activities against the development of myopia in adolescents39. This preventive effect is likely attributed to the enhancement of blood circulation within the eye due to physical activities, which in turn inhibits the excessive elongation of the eyeball, a key factor in the development of myopia in children and adolescents23. Furthermore, increased exposure to sunlight aids in the synthesis of Vitamin D in the human body40, offering a protective effect in maintaining normal vision41. Additionally, it is proposed that outdoor exposure contributes to myopia prevention through the photostimulation of retinal dopamine release. The increase in dopamine levels is believed to impede the axial elongation of the eye, which constitutes the fundamental structural change in myopia42. Moreover, outdoor activities provide opportunities for distant viewing, which is beneficial for the regulation and relaxation of the eyes43. The intensity of outdoor illumination significantly surpasses that of indoor environments. Under the influence of high ambient light, the pupil constricts and depth of field increases, which collectively serves to decelerate the onset and progression of myopia44.
This study identified maintaining proper reading and writing postures as a key factor in preventing myopia. Supporting research has indicated that not maintaining good postures during these activities constituted a risk factor for the development of myopia in adolescents45. The posture adopted during reading and writing influences not only the pleasure and effectiveness of these activities but also impacts retinal image quality, convergence and accommodation demands, and binocular comfort, all of which can contribute to the incidence of myopia46.
This study revealed that prolonged near-vision activities were a significant risk factor for myopia in adolescents. Similar studies have shown that extended use of computers47 and smartphones48, as well as prolonged reading periods49, especially when the eyes were too close to screens or books, can accelerate the progression of myopia50. These activities impose greater demands on accommodation and vergence due to the axial elongating effects of excessive accommodative convergence and peripheral defocus. Additionally, the small screens and font size on smart devices encourage closer viewing distances than conventional print materials, exacerbating these effects51.
This study found that adequate sleep duration was associated with myopia prevention in adolescents. Research supported that sufficient sleep served as a protective factor against myopia52. The beneficial effect of sleep on myopia might be attributed to the relief or rest it provides to the ciliary muscle, thereby helping to prevent or alleviate myopic progression53. Sleep is regulated by circadian and homeostatic mechanisms and may also contribute to ocular growth and emmetropization54. Recent studies have reported that myopic children tend to exhibit delays in sleep onset and wake-up time, aligning with delays in dim light melatonin onset55, and experience reduced sleep quality compared to their emmetropic peers56. However, current evidence linking sleep disorders with the incidence and progression of myopia remained inconclusive57. This ambiguity is primarily due to limitations in the sensitivity of outcome measures, variations in the definition of studied variables and participant demographics57, the absence of cycloplegic refraction leading to overestimation of myopia, and recall bias from questionnaires assessing sleep characteristics53.
Nevertheless, it was imperative to approach the insights gleaned from this investigation with a discerning perspective, acknowledging the inherent limitations of the study. This cautious interpretation is vital for the accurate contextualization and application of the research outcomes in broader epidemiological and clinical settings. Despite employing a stratified random cluster sampling method, the study was confined to Shandong Province, China, which might limit the generalizability of the findings to other regions or populations with different socioeconomic or environmental backgrounds. As a cross-sectional study, it only provided a snapshot of myopia prevalence and its associated factors at a single point in time, limiting the ability to establish causality or track changes in myopia progression over time. The questionnaire relied on self-reported data regarding daily life behaviors, which might be subject to recall bias or social desirability bias, meaning the accuracy of reported habits might not fully reflect actual behavior patterns. Although the study used multivariable logistic regression analysis to adjust for several variables, there might still be unmeasured confounding factors that could affect the results. Additionally, the measurement of non-cycloplegic autorefraction and not measuring axial length/choroid thickness were limitations of this study.
Conclusion
This research highlighted the multifactorial nature of myopia development among adolescents, revealing significant demographic, genetic, behavioral, and environmental determinants. Our findings emphasized the importance of holistic strategies to combat the rising incidence of myopia. Regular outdoor exercise, maintaining good visual habits, keeping a safe distance from screens, reducing screen time and homework duration, and ensuring adequate sleep were critical preventive measures. Additionally, targeted interventions should focus on higher-risk groups such as female adolescents, older youths, urban residents, and those with myopic parents. These comprehensive strategies could help reduce myopia rates and safeguard the long-term vision health of adolescents.
The clinical implications of this study suggested that an integrated approach, focusing on both preventive measures and targeted interventions for high-risk groups, was essential. Healthcare providers should advocate for regular eye exams in schools and community settings to detect early signs of myopia. Moreover, public health campaigns should promote healthy visual habits and environments. This holistic strategy will not only help in controlling the rise of myopia but also contribute to the overall ocular and systemic health of adolescents.
Data availability
The data used during the current study are included in this published article and its supplementary information files.
Abbreviations
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Mountjoy, E. et al. Education and myopia: Assessing the direction of causality by Mendelian randomisation. BMJ 361, k2022. https://doi.org/10.1136/bmj.k2022 (2018).
Naik, A. et al. An insight into knowledge, perspective, and practices of Indian optometrists towards childhood myopia. Vision (Basel) 8(2), 22. https://doi.org/10.3390/vision8020022 (2024).
Sankaridurg, P. Contact lenses to slow progression of myopia. Clin. Exp. Optom. 100, 432–437. https://doi.org/10.1111/cxo.12584 (2017).
Gomel, N. et al. Predictive factors for efficacy and safety in refractive surgery for myopia. PLoS One 13, e0208608. https://doi.org/10.1371/journal.pone.0208608 (2018).
Lakawicz, J. M., Bottega, W. J., Fine, H. F. & Prenner, J. L. On the mechanics of myopia and its influence on retinal detachment. Biomech. Model Mechanobiol. 19, 603–620. https://doi.org/10.1007/s10237-019-01234-1 (2020).
Chong, R. S. et al. Mendelian randomization implicates bidirectional association between myopia and primary open-angle glaucoma or intraocular pressure. Ophthalmology 130, 394–403. https://doi.org/10.1016/j.ophtha.2022.11.030 (2023).
Haarman, A. E. G. et al. The complications of myopia: A review and meta-analysis. Invest Ophthalmol. Vis. Sci. 61, 49. https://doi.org/10.1167/iovs.61.4.49 (2020).
Holden, B. et al. Myopia, an underrated global challenge to vision: Where the current data takes us on myopia control. Eye 28, 142–146. https://doi.org/10.1038/eye.2013.256 (2014).
Wang, T. J., Chiang, T. H., Wang, T. H., Lin, L. L. & Shih, Y. F. Changes of the ocular refraction among freshmen in National Taiwan University between 1988 and 2005. Eye 23, 1168–1169. https://doi.org/10.1038/eye.2008.184 (2009).
Vitale, S., Sperduto, R. D. & Ferris, F. L. III. Increased prevalence of myopia in the United States between 1971–1972 and 1999–2004. Arch. Ophthalmol. 127, 1632–1639. https://doi.org/10.1001/archophthalmol.2009.303 (2009).
Craig, J. P. et al. TFOS DEWS II definition and classification report. Ocul. Surf. 15, 276–283. https://doi.org/10.1016/j.jtos.2017.05.008 (2017).
Fricke, T. R. et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: Systematic review, meta-analysis and modelling. Br. J. Ophthalmol. 102, 855–862. https://doi.org/10.1136/bjophthalmol-2017-311266 (2018).
Dutheil, F. et al. Myopia and near work: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 20, 875. https://doi.org/10.3390/ijerph20010875 (2023).
Ramamurthy, D., Lin Chua, S. Y. & Saw, S. M. A review of environmental risk factors for myopia during early life, childhood and adolescence. Clin. Exp. Optom. 98, 497–506. https://doi.org/10.1111/cxo.12346 (2015).
Muralidharan, A. R. et al. Light and myopia: From epidemiological studies to neurobiological mechanisms. Ther. Adv. Ophthalmol. 13, 25158414211059250. https://doi.org/10.1177/25158414211059246 (2021).
Chen, S. et al. Establishment and validation of a risk assessment model for myopia among Chinese primary school students during the COVID-19 pandemic: A lasso regression approach. Heliyon 9, e20638. https://doi.org/10.1016/j.heliyon.2023.e20638 (2023).
Morgan, I. G., Ohno-Matsui, K. & Saw, S. M. Myopia. Lancet 379, 1739–1748. https://doi.org/10.1016/S0140-6736(12)60272-4 (2012).
Jonas, J. B. et al. IMI prevention of myopia and its progression. Invest Ophthalmol. Vis. Sci. 62, 6. https://doi.org/10.1167/iovs.62.5.6 (2021).
Huang, Y. K. & Chang, Y. C. Oral health: The first step to sustainable development goal 3. J. Formos. Med. Assoc. 121, 1348–1350. https://doi.org/10.1016/j.jfma.2021.10.018 (2022).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology—STROBE Statement: guidelines for reporting observational studies. Int. J. Surg. 12, 1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013 (2014).
Zhang, D. et al. Prevalence and associated factors of myopia among school students in Shenyang, China: A cross-sectional study. Front. Public Health 11, 1239158. https://doi.org/10.3389/fpubh.2023.1239158 (2023).
Bzovsky, S. et al. The clinician’s guide to interpreting a regression analysis. Eye 36, 1715–1717. https://doi.org/10.1038/s41433-022-01949-z (2022).
Mandel, Y. et al. Season of birth, natural light, and myopia. Ophthalmology 115, 686–692. https://doi.org/10.1016/j.ophtha.2007.05.040 (2008).
Xu, M. et al. Two-year longitudinal change in choroidal and retinal thickness in school-aged myopic children: Exploratory analysis of clinical trials for myopia progression. Eye Vis. 9, 5. https://doi.org/10.1186/s40662-022-00276-4 (2022).
Xie, H. et al. Analysis on the relationship between adolescent myopia and serum sex hormone. Natl. Med. J. China 94, 1294–1297. https://doi.org/10.3760/cma.j.issn.0376-2491.2014.17.004 (2014).
Széll, N. et al. Myopia-26, the female-limited form of early-onset high myopia, occurring in a European family. Orphanet. J. Rare Dis. 16, 45. https://doi.org/10.1186/s13023-021-01673-z (2021).
Lin, T., Hu, J., Lin, J., Chen, J. & Wen, Q. Epidemiological investigation of the status of myopia in children and adolescents in Fujian Province in 2020. Jpn. J. Ophthalmol. 67, 335–345. https://doi.org/10.1007/s10384-023-00991-y (2023).
Desalegn, B. B., Diddana, T. Z., Daba, A. K. & Tafese, T. A. Overnutrition in adolescents and its associated factors in Dale district schools in Ethiopia: A cross-sectional study. PeerJ 11, e16229. https://doi.org/10.7717/peerj.16229 (2023).
Jian, W., Shen, Y., Chen, Y., Tian, M. & Zhou, X. Ocular dimensions of the Chinese adolescents with keratoconus. BMC Ophthalmol. 18, 43. https://doi.org/10.1186/s12886-018-0713-6 (2018).
Fu, J., Zhu, H. & Sun, Y. Effect of peripheral retinal defocus caused by pupil diameter on myopia progression in adolescents. J. Clin. Ophthalmol. 28, 434–437. https://doi.org/10.3969/j.issn.1006-8422.2020.05.012 (2020).
Wang, Y. et al. Rural-urban differences in prevalence of and risk factors for refractive errors among school children and adolescents aged 6–18 years in Dalian, China. Front. Public Health 10, 917781. https://doi.org/10.3389/fpubh.2022.917781 (2022).
Ip, J. M., Rose, K. A., Morgan, I. G., Burlutsky, G. & Mitchell, P. Myopia and the urban environment: findings in a sample of 12-year-old Australian school children. Invest. Ophthalmol. Vis. Sci. 49, 3858–3863. https://doi.org/10.1167/iovs.07-1451 (2008).
Zhang, M. et al. Population density and refractive error among Chinese children. Invest. Ophthalmol. Vis. Sci. 51, 4969–4976. https://doi.org/10.1167/iovs.10-5424 (2010).
O’Donoghue, L. et al. Risk factors for childhood myopia: Findings from the NICER study. Invest. Ophthalmol. Vis. Sci. 56, 1524–1530. https://doi.org/10.1167/iovs.14-15549 (2015).
Yu, M. et al. Global risk factor analysis of myopia onset in children: A systematic review and meta-analysis. PLoS One 18(9), e0291470. https://doi.org/10.1371/journal.pone.0291470 (2023).
Yang, L., Xu, Y., Zhou, P. & Wan, G. The SNTB1 and ZFHX1B gene have susceptibility in northern Han Chinese populations with high myopia. Exp. Eye Res. 237, 109694. https://doi.org/10.1016/j.exer.2023.109694 (2023).
Yang, X. et al. Prediction of myopia in adolescents through machine learning methods. Int. J. Environ. Res. Public Health 17(2), 463. https://doi.org/10.3390/ijerph17020463 (2020).
Shi, H. et al. Influence of the interaction between parental myopia and poor eye habits when reading and writing and poor reading posture on prevalence of myopia in school students in Urumqi, China. BMC Ophthalmol. 21(1), 299. https://doi.org/10.1186/s12886-021-02058-3 (2021).
Jin, J. X. et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: The Sujiatun eye care study. BMC Ophthalmol. 15, 73. https://doi.org/10.1186/s12886-015-0052-9 (2015).
Biswas, S. et al. The influence of the environment and lifestyle on myopia. J. Physiol. Anthropol. 43(1), 7. https://doi.org/10.1186/s40101-024-00354-7 (2024).
Liang, R. et al. Effect of exogenous calcitriol on myopia development and axial length in guinea pigs with form deprivation myopia. Sci. Rep. 14(1), 11382. https://doi.org/10.1038/s41598-024-62131-x (2024).
Feldkaemper, M. & Schaeffel, F. An updated view on the role of dopamine in myopia. Exp. Eye Res. 114, 106–119. https://doi.org/10.1016/j.exer.2013.02.007 (2013).
Flitcroft, D. I. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog. Retin. Eye Res. 31, 622–660. https://doi.org/10.1016/j.preteyeres.2012.06.004 (2012).
Norton, T. T. & Siegwart, J. T. Jr. Light levels, refractive development, and myopia-a speculative review. Exp. Eye Res. 114, 48–57. https://doi.org/10.1016/j.exer.2013.05.004 (2013).
Charman, W. N. Myopia, posture and the visual environment. Ophthalmic Physiol. Opt. 31, 494–501. https://doi.org/10.1111/j.1475-1313.2011.00825.x (2011).
Jiang, D. et al. Associations between reading and writing postures and myopia among school students in Ningbo, China. Front. Public Health 10, 713377. https://doi.org/10.3389/fpubh.2022.713377 (2022).
Paudel, P. et al. Prevalence of vision impairment and refractive error in school children in Ba Ria–Vung Tau province. Vietnam. Clin. Exp. Ophthalmol. 42, 217–226. https://doi.org/10.1111/ceo.12273 (2014).
Foreman, J. et al. Association between digital smart device use and myopia: A systematic review and meta-analysis. Lancet Digit. Health 3(12), e806–e818. https://doi.org/10.1016/S2589-7500(21)00135-7 (2021).
Karthikeyan, S. K., Ashwini, D. L., Priyanka, M., Nayak, A. & Biswas, S. Physical activity, time spent outdoors, and near work in relation to myopia prevalence, incidence, and progression: An overview of systematic reviews and meta-analyses. Indian J. Ophthalmol. 70(3), 728–739. https://doi.org/10.4103/ijo.IJO_1564_21 (2022).
Yu, H. et al. Variability of accommodative microfluctuations in myopic and emmetropic juveniles during sustained near work. Int. J. Environ. Res. Public Health 19, 7066. https://doi.org/10.3390/ijerph19127066 (2022).
Mccrann, S., Loughman, J., Butler, J. S., Paudel, N. & Flitcroft, D. I. Smartphone use as a possible risk factor for myopia. Clin. Exp. Optom. 104, 35–41. https://doi.org/10.1111/cxo.13092 (2021).
Xu, S. et al. Association between sleep-wake schedules and myopia among Chinese school-aged children and adolescents: A cross-sectional study. BMC Ophthalmol. 23, 135. https://doi.org/10.1186/s12886-023-02874-9 (2023).
Li, M. et al. Sleep patterns and myopia among school-aged children in Singapore. Front. Public Health 10, 828298. https://doi.org/10.3389/fpubh.2022.828298 (2022).
Chakraborty, R. et al. Circadian rhythms, refractive development, and myopia. Ophthalmic Physiol. Opt. 38, 217–245. https://doi.org/10.1111/opo.12453 (2018).
Chakraborty, R. et al. Delayed melatonin circadian timing, lower melatonin output, and sleep disruptions in myopic, or short-sighted, children. Sleep 47(1), zsad265. https://doi.org/10.1093/sleep/zsad265 (2024).
Xu, S. et al. Association between sleep-wake schedules and myopia among Chinese school-aged children and adolescents: A cross-sectional study. BMC Ophthalmol. 23(1), 135. https://doi.org/10.1186/s12886-023-02874-9 (2023).
Liu, X. N., Naduvilath, T. J. & Sankaridurg, P. R. Myopia and sleep in children—A systematic review. Sleep 46(11), zsad162. https://doi.org/10.1093/sleep/zsad162 (2023).
Funding
This research was funded by the Social Sciences Planning Project of Dongying (DYSK2024 No.1113) and the Scientific Developmental Foundation Project of Dongying (DJB2023016).
Author information
Authors and Affiliations
Contributions
Zhihao Huang: conceptualization, formal analysis, methodology, project administration, software, supervision, writing—original draft, writing—review and editing. Ding Song: conceptualization, formal analysis, investigation, supervision, visualization, writing—original draft, writing—review and editing. Zhiqi Tian: conceptualization, Visualization, writing—review and editing. Yongming Wang: methodology, writing—review and editing. Kunzong Tian: formal analysis, writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, Z., Song, D., Tian, Z. et al. Prevalence and associated factors of myopia among adolescents aged 12–15 in Shandong Province, China: a cross-sectional study. Sci Rep 14, 17289 (2024). https://doi.org/10.1038/s41598-024-68076-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68076-5
- Springer Nature Limited