Abstract
Alveolar bone loss resulting from periodontal disease ultimately leads to tooth loss. Periodontal ligament mesenchymal stem cells (PDLMSCs) are the tissue-specific cells responsible for maintaining and repairing the periodontal ligament, cementum, and alveolar bone. In this study, we explored the role of aldehyde oxidase 1 (AOX1) in regulating the osteoinduction of human periodontal ligament stem cells (hPDLMSCs). hPDLMSCs were isolated from clinically healthy donors, and AOX1 expression was assessed by comparing inducted and non-inducted hPDLMSCs. Remarkably, we observed a significant upregulation of AOX1 expression during osteoinduction, while AOX1 silencing resulted in the enhanced osteogenic potential of hPDLMSCs. Subsequent experiments and analysis unveiled the involvement of retinoid X receptor (RXR) signaling in the inhibition of osteogenesis in hPDLMSCs. Ligands targeting the RXR receptor mirrored the effects of AOX1 on osteogenesis, as evidenced by alterations in alkaline phosphatase (ALP) activity and bone formation levels. Collectively, these findings underscore the potential regulatory role of AOX1 via RXR signaling in the osteogenesis of hPDLMSCs. This elucidation is pivotal for advancing hPDLMSC-based periodontal regeneration strategies and lays the groundwork for the development of targeted therapeutic interventions aimed at enhancing bone formation in the context of periodontal disease.
Similar content being viewed by others
Introduction
Periodontitis is a chronic inflammatory disease affecting the supporting tissues of the teeth, including the gums, periodontal ligament, and alveolar bone. Traditional treatment approaches focus on controlling the infection and inflammation through mechanical debridement and antimicrobial therapy. However, these approaches may not always fully restore the damaged tissues1. Regenerative therapies aim to promote the regeneration of lost periodontal tissues, including the periodontal ligament, cementum, and alveolar bone. These approaches involve the use of various biomaterials, growth factors, and stem cells to stimulate tissue repair and regeneration. Mesenchymal stem cells (MSCs) derived from sources such as the bone marrow, adipose tissue, or periodontal ligament have shown promise in periodontal regeneration due to their ability to differentiate into various cell types involved in tissue repair2,3.
As a type of MSCs found within the periodontal ligament, PDLMSCs play a crucial role in maintaining the health and integrity of the periodontium, which includes the periodontal ligament, cementum, alveolar bone, and gingiva4,5,6. One of the key functions of PDLMSCs is their potential for osteogenesis, which is the process of forming bone tissue. PDLMSCs have the capacity to differentiate into osteoblasts, the cells responsible for bone formation by secreting collagen and other proteins that form the organic matrix of bone, subsequently facilitating the mineralization process7. These functions of PDLMSCs indicate their roles in maintaining periodontal homeostasis or managing periodontal disease. And this differentiation process is regulated by various signaling pathways and molecular factors8,9. This prompts researchers to investigate potential pathways that can be modulated exogenously to augment the osteogenic capacity of target cells.
Recent studies have emphasized the connection between osteogenesis and aldehyde oxidase 1 (AOX1), an enzyme belonging to the molybdenum-containing hydroxylase family. AOX1 is an enzyme involved in the metabolism of various compounds, which plays a role in the conversion of aldehyde into carboxylic acid, therefore taking part in many pathways including retinol metabolism, serotonin metabolism, purine metabolism, etc.10 And some of the pathways, such as retinol11,12 and serotonin13 pathway, have reported to be associated with the osteogenesis and/or adipogenesis of MSCs. AOX1’s relevance in mesenchymal stem cells has garnered attention in current researches, indicating its potential in osteoblastic genes upregulation and alkaline phosphatase (ALP) activity enhancement14,15. These studies found that by inhibiting AOX1 expression by shRNA, osteogenesis or adipogenesis of bone marrow mesenchymal stem cells (BMMSCs) are significantly regulated.
Based on prior research findings, an inquiry arises regarding the potential involvement of AOX1 in hPDLMSCs osteogenesis and its underlying mechanism. In this study, based on previous results about AOX1’s potential functions and our RNA-sequencing data of hPDLMSCs, we aimed to experimentally investigate the role of AOX1 in hPDLMSCs osteogenesis and identify possible pathways responsible for its functions.
Results
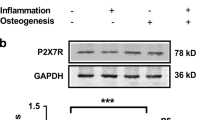
AOX1 expression upregulates in hPDLMSCs osteoinduction
Our RNA-sequencing data16 showed three times increase in AOX1 expression after the transition to osteo-inductive medium over a four-day period. To substantiate these findings, we conducted real-time reverse transcription–polymerase chain reaction (RT-PCR) assays to assess mRNA fold changes in hPDLMSCs after 5 days of induction. Given that our osteoinduction medium incorporates dexamethasone, a potent hormone with broad influence on cellular pathways, mRNA from both AOX1 and the reference gene (ACTB) was extracted from cells cultured in a standard medium as well as various osteo-inductive medium to delineate dexamethasone’s impact. Subsequent rt-PCR analysis demonstrated about two times increase in AOX1 expression following osteoinduction (Fig. 1A).
AOX1 expression under osteo-induction medium and AOX1 knockdown’s effects on ALP activity. Cells were cultivated in basic medium consisting of alpha-minimum essential medium (α-MEM; Thermo Fisher Scientific) supplemented with 10% fetal bovine serum (FBS; Thermo Fisher Scientific), 100 U ml−1 penicillin and 100 μg ml−1 streptomycin (P/S; Thermo Fisher Scientific). Transfections were done 1 day after seeding. And osteoinduction started 2 days after seeding. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001; by Brown–Forsythe and Welch ANOVA test (A), two-way ANOVA test (C) and student’s t-test (D). (A) AOX1 expression under different osteo-induction medium with ascorbic acid (AA), with or without β-glycerophosphate (bGP) and dexamethasone (Dex). (B) Knockdown efficiency of different siRNA product targeting AOX1. (C) Impact of AOX1 knockdown to ALP activity in PDLMSC. (D) Osteogenic genes expression changes under AOX1 knockdown by siRNA. Neg Ctrl Silencer® Select negative control #1 siRNA, ABD osteoinduction with ascorbic acid, β-glycerophosphate and dexamethasone.
Despite observed further enhancements in alkaline phosphatase (ALP) activity upon supplementation with β-glycerophosphate (βGP) and dexamethasone (Dex), the AOX1 fold changes across induction groups remained nonsignificant. This suggests that the upregulation of AOX1 was not closely associated with the addition of βGP and dexamethasone, but rather may be more closely linked to the presence of ascorbic acid as an osteo-inductive component.
siRNA-Mediated knockdown of AOX1 enhances ALP activity and osteogenic gene expression
To elucidate the role of AOX1 in osteoinduction process of hPDLMSCs, small interfering RNA (siRNA) technology was employed to suppress AOX1 expression. A preliminary investigation was conducted to determine the optimal siRNA concentration for efficient knockdown, in accordance with the manufacturer’s recommendations. Experimental findings demonstrated a robust suppression of AOX1 expression after siRNA transfection, with both s33 and s34 siRNA variants exhibiting satisfactory knockdown efficiencies. Concentrations as low as 10 nM yielded approximately 95% inhibition of AOX1 expression (Fig. 1B). Considering the superior stability of knockdown achieved by s33 within the tested concentration range, it was selected for subsequent experimental investigations. This approach enabled the establishment of a reliable model for assessing the functional significance of AOX1 in hPDLMSC osteoinduction, providing a foundation for further mechanistic elucidation of its role in bone regeneration processes.
Next, the impact of siRNA-mediated AOX1 knockdown on ALP activity in hPDLMSCs was assessed. Remarkably, irrespective of osteo-inductive conditions employed, AOX1 knockdown alone significantly upregulated the ALP activity of hPDLMSCs (Fig. 1C). Intriguingly, consistent with the observations regarding AOX1 expression under various osteo-inductive conditions, the addition or omission of βGP and dexamethasone didn’t alter the pattern of AOX1 knockdown effects on ALP activity.
The function of AOX1 in the osteogenesis of hPDLMSCs was further validated by PCR analysis of osteogenic-related genes. The results demonstrated that the expression levels of RUNX2, ALPL, and COL1A1 were significantly upregulated following the knockdown of AOX1 via siRNA (Fig. 1D).
While osteo-inductive stimuli led to an upregulation in the expression of AOX1, its silencing enhanced ALP activity. This observation raises the hypothesis that AOX1 may regulate the osteogenic differentiation of hPDLMSCs in a negative feedback manner, suggesting a nuanced interplay between AOX1 expression and ALP activity in the context of hPDLMSCs.
Retinaldehyde exhibits a close relationship with AOX1’s inhibitory effect
AOX1 has broad substrate specificity, contributing to various pathways. To gain deeper insights into the mechanisms underlying AOX1-mediated inhibition of osteogenesis in hPDLMSCs, an extensive investigation was undertaken to identify the pathways in which AOX1 is implicated and could be related to the osteogenic process. Among all direct substrates for AOX1, retinaldehyde and hydroxyindoleacetaldehyde (a metabolite of retinol and serotonin metabolism) emerged as particularly promising candidates. Previous research has indicated their close association with the osteogenesis or adipogenesis of MSCs11,12,13.
To explore how AOX1 functions in hPDLMSCs osteoinduction, retinaldehyde (all trans-retinaldehyde, R2500, Sigma–Aldrich), retinoic acid (retinoic acid, R2625, Sigma-Aldrich), and serotonin (serotonin hydrochloride, H9523, Sigma–Aldrich) were selected as potential substrates for AOX1. Experimental findings revealed that all three substrates could inhibit ALP activity at physiological concentration (Fig. 2A–C). Considering that AOX1 knockout may prevent the metabolism of these substrates, the observed inhibitory effect of retinal, retinoic acid, and serotonin on ALP activity in hPDLMSCs suggests their involvement in mediating AOX1’s inhibitory effect on osteogenesis, underscores the sophisticated interplay between AOX1 activity and the metabolic pathways regulated by its substrates.
Impact of different substrates on ALP activity and their interplay with siRNA of AOX1. Cells were cultivated in basic medium consisting of alpha-minimum essential medium (α-MEM; Thermo Fisher Scientific) supplemented with 10% fetal bovine serum (FBS; Thermo Fisher Scientific), 100 U ml−1 penicillin and 100 μg ml−1 streptomycin (P/S; Thermo Fisher Scientific). Transfections were done 1 day after seeding. And osteoinduction started 2 days after seeding with the addition of 5 nM retinal, 5 nM ATRA or 100 μM serotonin. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001; by two-way ANOVA test (A–C) and Brown–Forsythe and Welch ANOVA test (D–F). (A–C) Impact of retinal, retinoic acid (ATRA) and serotonin on ALP activity of PDLMSCs. (D–F) Interaction of retinal, ATRA and serotonin with siRNA of AOX1 on ALP activity of PDLMSCs (osteoinduction medium is ascorbic acid only). ABD osteoinduction with ascorbic acid, β-glycerophosphate and dexamethasone.
Subsequent experiments investigated the interplay between all three substrates—retinaldehyde, retinoic acid, and serotonin—and siRNA targeting AOX1 (Fig. 2D–F). 5 nM retinal, 5 nM ATRA, or 100 μM serotonin were added separately into the osteoinduction medium (ascorbic acid only). Interestingly, as the substrate and product of AOX1, retinaldehyde and retinoic acid yielded contrasting outcomes. While the inhibitory effect of retinaldehyde on ALP activity could be entirely reversed by AOX1 siRNA, retinoic acid’s effect remained unaffected by siRNA intervention.
In contrast, the inhibitory effect of serotonin on ALP activity could be partially mitigated by AOX1 siRNA. Considering that siRNA yielded about 95% inhibition of AOX1 expression, the observed partial mitigation does not conclusively establish a direct causal relationship between serotonin and AOX1’s inhibitory effect. Consequently, our subsequent experimental endeavors primarily focused on retinaldehyde metabolism and its potential role in mediating AOX1’s inhibitory effect on osteogenesis.
RXR receptor demonstrates a strong correlation with AOX1 catalyzed retinaldehyde inhibitory effect
Considering AOX1’s enzymatic role in catalyzing the oxidation of retinaldehyde into retinoic acid, the contrasting responses of these substrates hint at retinol metabolism stand as a possible answer for AOX1’s inhibitory effect on osteogenesis. And this highlighted the need for further elucidation of the molecular mechanisms underlying this regulatory pathway. In search of receptors related to retinaldehyde and retinoic acid, we searched online database10 combined with recently published papers17,18. Two notable receptors for retinoic acid, retinoic acid receptor (RAR) and retinoid X receptor (RXR) have been implicated in the osteogenesis or adipogenesis of hMSCs. Research focusing on these two proteins has yielded diverse findings concerning their impact on osteogenesis and adipogenesis19,20,21. Leveraging insights from previous studies, popular agonists and antagonists of RAR and RXR were selected to examine their impact on the osteoinduction of hPDLMSCs. Within the concentration used in previous researches19,22, LG100268 (RXR agonist) (SML0279, Sigma–Aldrich) and AGN194310 (RAR antagonist) (SML2665, Sigma–Aldrich) exhibited inhibitory effects on ALP activity. Conversely, HX531 (RXR antagonist) (SML2170, Sigma–Aldrich) showed contrasting results (Fig. 3A–C).
Impact of different RXR and RAR ligands on ALP activity and their interplay with siRNA of AOX1. Cells were cultivated in basic medium consisting of alpha-minimum essential medium (α-MEM; Thermo Fisher Scientific) supplemented with 10% fetal bovine serum (FBS; Thermo Fisher Scientific), 100 U ml−1 penicillin and 100 μg ml−1 streptomycin (P/S; Thermo Fisher Scientific). Transfections were done 1 day after seeding. And osteoinduction started 2 days after seeding with the addition of 100 nM LG268 or 5 nM HX531. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001; by two-way ANOVA test (A–C) and Brown–Forsythe and Welch ANOVA test (D–E). (A–C) LG100268, HX531 and AGN194310’s effects on ALP activity of PDLMSCs. (D–E) RXR ligands’ cross reaction with siRNA of AOX1 on ALP activity of PDLMSCs (osteoinduction medium is ascorbic acid only). ABD osteoinduction with ascorbic acid, β-glycerophosphate and dexamethasone.
The comparative analysis between RAR and RXR ligands’ osteogenic impacts revealed striking similarities in HX531’s (RXR antagonist) effects with siRNA targeting AOX1 on hPDLMSCs. As RXR receptor inhibition elicited a comparable osteogenic response to AOX1 knockdown, suggesting a potential functional convergence between RXR signaling and AOX1-mediated pathways in regulating hPDLMSCs osteogenesis. In contrast, the retinoic acid receptor (RAR) antagonist AGN194310 yielded divergent outcomes, exhibiting a suppressive effect on ALP activity and downregulating osteogenesis in hPDLMSCs.
This disparity in the effects of RXR and RAR receptor inhibition underscores the regulatory mechanisms of retinoic acid signaling in the context of osteogenic differentiation. In light of our findings implicating RXR signaling in negatively modulating osteogenesis, subsequent experimental investigations were directed toward elucidating the interplay between RXR and AOX1. This focused exploration aims to unravel the crosstalk between RXR-mediated signaling pathways and AOX1 function, thereby providing deeper insights into the regulatory networks governing hPDLMSCs osteogenesis.
ALP assay results revealed that both LG268 and HX531 attenuated the effect of siRNA targeting AOX1 (Fig. 3D, E). 100 nM LG268 or 5 nM HX531 were added separately into the osteoinduction medium (ascorbic acid only). Intriguingly, the introduction of siRNA targeting AOX1 failed to elicit a significant upregulation in ALP activity of hPDLMSCs in the presence of RXR ligands.
These interesting findings shed light on the potential regulatory role of AOX1 in hPDLMSC osteogenesis within the context of RXR-mediated signaling pathways. The observed attenuation of AOX1-mediated effects in the presence of RXR antagonists suggests a functional interplay between AOX1 and RXR signaling cascades in modulating hPDLMSCs osteogenic differentiation.
Alizarin red and oil red O staining results of PDLMSCs
To comprehensively evaluate the osteo-inductive effects of siRNA targeting AOX1 and RXR ligands (HX531 and LG100268), we conducted alizarin red staining and oil red O staining. In alizarin red staining, both HX531 and siRNA demonstrated noticeably stronger staining results compared to control groups (Fig. 4A, B). After 14 day induction, the difference between siRNA group and control group seems more significant comparing with ALP assay results at day 5. These staining results compellingly confirmed the inhibitory effects of AOX1 and RXR pathway inhibition on osteogenic differentiation in hPDLMSCs. Importantly, the observed enhancement in calcium accumulation, as evidenced by the intensified staining, occurred without compromising the viability of hPDLMSCs. This unequivocally supports the notion that AOX1-mediated activation of the RXR signaling pathway exerts inhibitory effects on osteogenic differentiation in hPDLMSCs, as hypothesized.
Alizarin red staining and oil red O staining results of siRNA and RXR ligands in PDLMSCs. (A) siRNA’s impact on alizarin red staining results of PDLMSCs. (B) RXR ligand’s impact on alizarin red staining results of PDLMSCs. (C) RXR ligand’s impact on oil red O staining results of PDLMSCs. (D) Mechanism of AOX1’s inhibition to the osteo-induction of PDLMSCs.
In the oil red O staining assay, it was observed that the LG100268 group exhibited relatively stronger staining results. However, the control group, HX531 group, and siAOX1 group exhibited similarly weak staining results, making it difficult to discern any significant differences between these groups (Fig. 4C). However, the differences between the staining intensities were not deemed significantly notable, likely due to the overall modest lipid accumulation observed in hPDLMSCs. This observation is evident when considering the staining intensity in the control group, which was relatively weak. Despite the visible enhancement in staining intensity in the LG100268 group, the overall lipid accumulation in hPDLMSCs appeared to be relatively limited across all experimental conditions.
Discussion
Periodontitis is a chronic inflammatory condition that leads to the destruction of the supporting structures of the teeth, including the periodontal ligament and alveolar bone. A key feature of periodontitis is bone resorption, where the inflammatory process triggers the breakdown of bone tissue, resulting in tooth instability and potential loss. To counteract this destructive process, bone regeneration is essential, and one promising approach is through regenerative therapy. This involves the use of various techniques and materials to promote the formation of new bone. Central to bone regeneration is the differentiation of MSCs into osteoblasts, the cells responsible for new bone formation. By enhancing osteoblastogenesis, regenerative therapies aim to restore the lost bone and improve periodontal health, offering a potential solution for patients suffering from the detrimental effects of periodontitis.
Recently, researches about AOX1’s function in MSCs came out, suggesting its function in the regulation and induction of MSCs towards osteogenesis and adipogenesis. Firstly, recent bioinformatic analysis suggested its potential in osteogenic differentiation in hMSCs, and identified AOX1 as a potential regulator of osteogenic differentiation in bone marrow-derived mesenchymal stem cells (BMSCs)14. Furthermore, research in hMSCs revealed that AOX1 silencing induced by miR-513a-5p enhances osteogenic proliferation and differentiation15.
Our experimental findings elucidate the involvement of AOX1 in the osteogenic differentiation of hPDLMSCs through the retinoic acid-retinoid X receptor (RA-RXR) pathway. Initially, AOX1 catalyzes the oxidation of retinaldehyde into retinoic acid, a pivotal product with significant implications in MSCs researches. While retinaldehyde has wide functions in cell differentiation like neurogenesis23, it also serves as the chromophore of rod and cone visual pigments24. In our research, we mainly focused on its effects in osteogenesis. Also, the functional role of retinoic acid in MSCs remains a subject of considerable debate, characterized by divergent findings across different studies, particularly concerning its effects on osteogenesis and adipogenesis25,26.
According to our observations, retinoic acid demonstrates a negative impact on osteogenic differentiation in hPDLMSCs. Subsequent experiments aimed at elucidating the specific receptor-mediated signaling pathways involved revealed that, between the two receptors—RAR and RXR—RXR receptor is predominantly associated with the inhibitory effects exerted by retinoic acid. Suggesting a plausible pathway wherein retinoic acid, oxidized by AOX127,28, binds to RXR receptors to suppress osteogenesis in hPDLMSCs (Fig. 4D). This novel insight underscores the complexity of the molecular mechanisms governing bone formation processes and highlights the need for further elucidation of the regulatory interactions between AOX1 and RXR-mediated pathways. Such endeavors hold promise for advancing our understanding of periodontal tissue regeneration and may pave the way for the development of targeted therapeutic strategies aimed at enhancing bone formation and regeneration in periodontal disease contexts. Our results are in accordance with previous research about AOX1’s function in BMSCs14,15, that AOX1 inhibition leads to enhancement of osteogenesis. As for RXR signaling, there wasn’t much study about its relation with osteogenesis. However, some researches reported that RXR signaling is related to the adipogenesis of MSCs29,30.
In some studies, RXR activation has been shown to direct mesenchymal stem cells toward an adipogenic lineage19,31. However, our experiments yielded different results. The administration of LG100268 did induce some lipid accumulation in hPDLMSCs, but the overall magnitude of this effect was modest. Additionally, the weak staining intensity observed in the control group suggests that the current adipogenic induction medium may not be fully optimized. Further investigation is warranted to elucidate the specific mechanisms underlying lipid metabolism in hPDLMSCs and to understand the potential implications of RXR pathway modulation on this process.
In this experimental setup, we explored the osteogenic outcomes of two osteoinduction media formulations. Alongside the standard formulation comprising ascorbic acid, βGP and dexamethasone32, a simplified formula containing solely ascorbic acid was employed. Initially, this comparative approach aimed to elucidate the individual contributions of each component to the upregulation of AOX1. Subsequent PCR analysis revealed no significant differences in AOX1 expression levels between the osteo-inductive groups, mitigated any potential confounding effects arising from βGP and dexamethasone, such as proliferation, apoptosis, and tissue remodeling33,34.
Encouragingly, our subsequent experiments using both osteoinduction formulas yielded consistent results, as evidenced by the congruent patterns observed in the data (Supplementary Figs. S1, S2). This internal consistency provided robust justification for excluding the potential influence of βGP and dexamethasone on our experimental outcomes, thus suggesting specific effects of ascorbic acid on AOX1 expression and osteogenic differentiation in our model system. As there is no previous research reporting the relationship between AOX1 and ascorbic acid, the underlying mechanism remains unclear and warrants further investigation.
Ascorbic acid, commonly known as vitamin C, plays a crucial role in osteogenesis32. It acts as a cofactor for the enzyme prolyl hydroxylase, which catalyzes the hydroxylation of proline residues in procollagen, a precursor to collagen35. Moreover, ascorbic acid plays a pivotal role in the regulation of osteoblast differentiation and function. Research has demonstrated that ascorbic acid augments the expression of genes critical for osteogenesis, such as alkaline phosphatase and osteocalcin. Recent investigations have further elucidated its involvement in epigenetically orchestrating osteogenic differentiation and function36.
Ascorbic acid-induced AOX1 upregulation may also be linked to these multifaceted functions of ascorbic acid in osteogenesis, particularly its involvement in epigenetic regulation of osteogenic genes by modulating chromatin structure and transcriptional activity. This suggests a potential mechanism through which AOX1 upregulation in hPDLMSCs may be linked to the epigenetic control of osteogenic gene expression by ascorbic acid.
Further investigations into these aspects could yield valuable insights into the regulatory mechanisms and functional significance of AOX1 in hPDLMSCs. By elucidating the interplay between AOX1, ascorbic acid-mediated epigenetic regulation, and osteogenic gene expression, we may uncover novel targets in AOX1/RXR pathway for bone tissue regeneration and repair. Ultimately, such insights could inform the development of targeted therapeutic strategies aimed at enhancing bone regeneration and accelerating the healing process in various clinical contexts.
Conclusion
In summary, this study highlights the potential therapeutic application of PDLMSCs in the treatment of periodontal diseases. Our findings demonstrate that AOX1 expression in PDLMSCs can enhance the RXR pathway, thereby inhibiting osteogenesis. This pathway could be leveraged in PDLMSC-based products for clinical treatment. Further research is needed to elucidate the mechanisms behind AOX1 upregulation in osteoinductive environments, as well as the role of ascorbic acid in this regulation. This may enhance our understanding of AOX1’s role in PDLMSC osteogenesis and further improve PDLMSC-based products.
Methods
Cell culture
This study was conducted in accordance with the principles expressed in the Declaration of Helsinki. It received approval from the Institutional Review Board of Tokyo Medical and Dental University Human Subjects Research (D2020-077). All patients or their guardians were fully informed about the study’s purpose and procedures, and provided written consent for the donation of their teeth and their subsequent use in this research project. hPDLMSCs were isolated from healthy patients as previously reported4 and were cultured in each T-225 flask with a density of 1 × 105 cells. A basic medium consisting of alpha-minimum essential medium (α-MEM; Thermo Fisher Scientific) supplemented with 10% fetal bovine serum (FBS; Thermo Fisher Scientific), 100 U ml−1 penicillin and 100 μg ml−1 streptomycin (P/S; Thermo Fisher Scientific), was utilized for hPDLMSCs maintenance. Weekly cell passaging was followed. Cells were detached with 0.25% Trypsin–EDTA (Thermo Fisher Scientific) and then re-seeded in a new T-225 flask. Medium change was performed every 3 days. Data shown in this study was from one cell line of one patient, and the reproducibility was confirmed with two other cell lines of two other patients.
Differentiation assay
In osteogenesis studies, 15,000 cells were initially plated in 12-well plates and cultured for 2 days, following a previously established protocol. Subsequently, the medium was switched to a calcification medium, comprising complete medium supplemented with 100 µM ascorbic acid, 10 mM β-glycerophosphate (βGP), and 10 nM dexamethasone (Dex) (osteo-inductive medium)10, and maintained for an additional 14 days. Additional reagents, such as retinal, ATRA, or serotonin, as well as ligands like LG268, HX531, or AGN194310, were incorporated into the osteoinduction medium starting from the first day of induction. The medium was subsequently changed every three days. The resulting cell cultures were then subjected to staining with a 1% alizarin red solution. All experiments were done with biological triplicates.
In adipogenesis experiments, 15,000 cells were initially plated in 12-well plates and cultured for 2 days. Subsequently, the medium was changed to adipogenetic medium, comprising complete medium supplemented with 100 nM DEX, 0.5 mM isobutyl-1-methyl xanthine (Sigma–Aldrich), and 50 mM indomethacin (Wako Pure Chemical), and maintained for an additional 21 days. The resulting adipogenetic cultures were fixed with 4% paraformaldehyde and stained with a fresh oil red O solution. All experiments were done with biological triplicates.
Isolation of RNA and polymerase chain reaction (PCR)
Total RNA extraction was carried out using a QIA shredder and RNeasy mini kit (Qiagen, Valencia, CA, USA) following the manufacturer’s instructions. Subsequently, cDNA was synthesized from 500 ng of the total RNA using the Superscript VILO cDNA synthesis kit (Invitrogen). β-actin was selected as the internal control gene.
For quantitative analysis of mRNA expression levels, real-time PCR (QuantStudio 3 real-time pcr system, Applied Biosystems) was performed using sequence-specific primers. The primers used included aldehyde oxidase 1 (AOX1, Hs00154079_m1), Runt-related transcription factor 2 (RUNX2, Hs01047973_m1), alkaline phosphatase (ALPL, Hs01029144), collagen type I alpha 1 (COL1A1, Hs00164004_m1) and β-actin (ACTB, Hs99999903_m1). All samples were analyzed in biological triplicates and technical duplicates. The mRNA expression levels, relative to β-actin, were determined, and in some cases, fold changes were calculated using the values obtained through the 2−ΔΔCt method at each time point37.
Transfection of small interfering RNA (siRNA)
Pre-designed siRNAs (Silencer® Select Predesigned siRNA) (Thermo Fisher Scientific) for AOX1 (s33 and s34; 4,427,038) were utilized to facilitate the knockdown of the target gene expression. Concurrently, a non-targeting control (Neg Ctrl) (Silencer® Select Negative Control #1 siRNA; 4390843) was employed to assess the impact of gene silencing. Prior to experimentation, the siRNAs were reconstituted in RNase-free water following the manufacturer’s instructions. After siRNA performance test, all later transfection experiments were performed under the concentration of 10 nM. All experiments were done one day after seeding with biological triplicates.
Alkaline phosphatase (ALP) activity
Cells were plated into a 96-well plate at a density of 1 × 104 cells/well. The cells were cultured in complete medium for 48 h, after which the medium was changed to complete medium with or without osteo-inductive supplements. If siRNA transfection was done before, medium without antibiotics was used. All experiments were done with biological triplicates. Following an additional 5 day culture period, cells were washed once with PBS, and the alkaline phosphatase (ALP) activity of the cells was assessed using lab assay ALP (Wako Pure Chemical). The enzyme activity was measured optically at a wavelength of 405 nM using a microplate reader (SpectraMax ABS Plus, Molecular Devices, Sunnyvale, CA).
Data analysis
All experiments were conducted in triplicate, and means along with standard deviations (SD) were calculated. A normality test was performed to assess the distribution of the samples. Mean differences were analyzed using the independent two-tailed student’s t-test between two groups and ANOVA between three or more groups using GraphPad Prism version 10.0.0 for Windows (GraphPad Software, Boston, Massachusetts USA). A significance level of less than 0.05 (P < 0.05) was considered statistically significant.
Data availability
Data and materials supporting the findings of this study are available in the article and its Supplementary Figures. The RNA-seq datasets mentioned in this study have been deposited in the DNA Data Bank of Japan (DDBJ) Sequence Read Archive (DRA) under accession number DRA003917.
References
Slots, J. Periodontitis: Facts, fallacies and the future. Periodontol 2000 75, 7–23 (2017).
Liu, J. et al. Periodontal bone-ligament-cementum regeneration via scaffolds and stem cells. Cells https://doi.org/10.3390/cells8060537 (2019).
Xu, X. Y. et al. Concise review: Periodontal tissue regeneration using stem cells: Strategies and translational considerations. Stem Cell Transl. Med. 8, 392–403 (2019).
Iwata, T. et al. Validation of human periodontal ligament-derived cells as a reliable source for cytotherapeutic use. J. Clin. Periodontol. 37, 1088–1099 (2010).
Kim, S. H. et al. Alveolar bone regeneration by transplantation of periodontal ligament stem cells and bone marrow stem cells in a canine peri-implant defect model: A pilot study. J. Periodontol. 80, 1815–1823 (2009).
Liu, Y. L. et al. MiR-17 modulates osteogenic differentiation through a coherent feed-forward loop in mesenchymal stem cells isolated from periodontal ligaments of patients with periodontitis. Stem Cells 29, 1804–1816 (2011).
Kato, H. et al. A synthetic oligopeptide derived from enamel matrix derivative promotes the differentiation of human periodontal ligament stem cells into osteoblast-like cells with increased mineralization. J. Periodontol. 84, 1476–1483 (2013).
Chen, X. et al. Nuclear factor-κB modulates osteogenesis of periodontal ligament stem cells through competition with β-catenin signaling in inflammatory microenvironments. Cell Death Dis. https://doi.org/10.1038/cddis.2013.14 (2013).
Liu, W. et al. TCF3, a novel positive regulator of osteogenesis, plays a crucial role in miR-17 modulating the diverse effect of canonical Wnt signaling in different microenvironments. Cell Death Dis. https://doi.org/10.1038/cddis.2013.65 (2013).
Agrawal, A. et al. WikiPathways 2024: Next generation pathway database. Nucleic Acids Res. https://doi.org/10.1093/nar/gkad960 (2023).
Peacock, J. D., Levay, A. K., Gillaspie, D. B., Tao, G. & Lincoln, J. Reduced Sox9 function promotes heart valve calcification phenotypes in vivo. Circ. Res. 106, 712–719 (2010).
James, A. W., Levi, B., Xu, Y., Carre, A. L. & Longaker, M. T. Retinoic acid enhances osteogenesis in cranial suture-derived mesenchymal cells: Potential mechanisms of retinoid-induced craniosynostosis. Plast. Reconstr. Surg. 125, 1352–1361 (2010).
Wang, L. T., Chen, L. R. & Chen, K. H. Hormone-related and drug-induced osteoporosis: A cellular and molecular overview. Int. J. Mol. Sci. https://doi.org/10.3390/ijms24065814 (2023).
Sun, L. T., Ma, J. F., Chen, J., Pan, Z. J. & Li, L. J. Bioinformatics-guided analysis uncovers AOX1 as an osteogenic differentiation-relevant gene of human mesenchymal stem cells. Front. Mol. Biosci. https://doi.org/10.3389/fmolb.2022.800288 (2022).
Yan, Z. & He, Q. LINC01234 sponging of the miR-513a-5p/AOX1 axis is upregulated in osteoporosis and regulates osteogenic differentiation of bone marrow mesenchymal stem cells. Mol. Biotechnol. 65, 2108–2118 (2023).
Onizuka, S. et al. ZBTB16 as a downstream target gene of osterix regulates osteoblastogenesis of human multipotent mesenchymal stromal cells. J. Cell. Biochem. 117, 2423–2434 (2016).
Giguere, V. & Evans, R. M. Chronicle of a discovery: The retinoic acid receptor. J. Mol. Endocrinol. 69, T1–T11 (2022).
Krezel, W., Ruhl, R. & de Lera, A. R. Alternative retinoid X receptor (RXR) ligands. Mol. Cell. Endocrinol. 491, 110436 (2019).
Chang, R. C. et al. miR-223 plays a key role in obesogen-enhanced adipogenesis in mesenchymal stem cells and in transgenerational obesity. Endocrinology https://doi.org/10.1210/endocr/bqad027 (2023).
Shoucri, B. M., Hung, V. T., Chamorro-García, R., Shioda, T. & Blumberg, B. Retinoid X receptor activation during adipogenesis of female mesenchymal stem cells programs a dysfunctional adipocyte. Endocrinology 159, 2863–2883 (2018).
Shoucri, B. M. et al. Retinoid X receptor activation alters the chromatin landscape to commit mesenchymal stem cells to the adipose lineage. Endocrinology 158, 3109–3125 (2017).
Shimo, T. et al. Expression and role of IL-1beta signaling in chondrocytes associated with retinoid signaling during fracture healing. Int. J. Mol. Sci. https://doi.org/10.3390/ijms21072365 (2020).
Wu, D. et al. Retinoic acid signaling in development and differentiation commitment and its regulatory topology. Chem. Biol. Interact. https://doi.org/10.1016/j.cbi.2023.110773 (2024).
Daruwalla, A., Choi, E. H., Palczewski, K. & Kiser, P. D. Structural biology of 11-retinaldehyde production in the classical visual cycle. Biochem. J. 475, 3171–3188 (2018).
Guo, L. et al. All-trans retinoic acid inhibits the osteogenesis of periodontal ligament stem cells by promoting IL-1β production via NF-ΚB signaling. Int. Immunopharmacol. https://doi.org/10.1016/j.intimp.2022.108757 (2022).
Karakida, T., Yui, R., Suzuki, T., Fukae, M. & Oida, S. Retinoic acid receptor γ-dependent signaling cooperates with BMP2 to induce osteoblastic differentiation of C2C12 Cells. Connect. Tissue Res. 52, 365–372 (2011).
Mahro, M. et al. Characterization and crystallization of mouse aldehyde oxidase 3: From mouse liver to heterologous protein expression. Drug Metab. Dispos. 39, 1939–1945 (2011).
Zhong, G. et al. Aldehyde oxidase contributes to all-retinoic acid biosynthesis in human liver. Drug Metab. Dispos. 49, 202–211 (2021).
Hu, J. M. et al. Expression of GPR43 in brown adipogenesis is enhanced by rosiglitazone and controlled by PPARγ/RXR heterodimerization. PPAR Res. https://doi.org/10.1155/2018/1051074 (2018).
Hamza, M. S. et al. Identification of PPARγ/rxr binding sites and direct targets during adipogenesis. PLoS One https://doi.org/10.1371/journal.pone.0004907 (2009).
Kim, S., Li, A., Monti, S. & Schlezinger, J. J. Tributyltin induces a transcriptional response without a brite adipocyte signature in adipocyte models. Arch .Toxicol. 92, 2859–2874 (2018).
Langenbach, F. & Handschel, J. Effects of dexamethasone, ascorbic acid and beta-glycerophosphate on the osteogenic differentiation of stem cells in vitro. Stem Cell Res. Ther. 4, 117 (2013).
Giles, A. J. et al. Dexamethasone-induced immunosuppression: Mechanisms and implications for immunotherapy. J. Immunother. Cancer https://doi.org/10.1186/s40425-018-0371-5 (2018).
Shangguan, Y. F. et al. Low-activity programming of the PDGFRβ/FAK pathway mediates H-type vessel dysplasia and high susceptibility to osteoporosis in female offspring rats after prenatal dexamethasone exposure. Biochem. Pharmacol. https://doi.org/10.1016/j.bcp.2021.114414 (2021).
Gould, B. S. & Woessner, J. F. Biosynthesis of collagen. The influence of ascorbic acid on the proline, hydroxyproline, glycine, and collagen content of regenerating guinea pig skin. J. Biol. Chem. 226, 289–300 (1957).
Thaler, R. et al. Vitamin C epigenetically controls osteogenesis and bone mineralization. Nat. Commun. 13, 5883 (2022).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-delta delta C(T)) method. Methods 25, 402–408 (2001).
Acknowledgements
This study was supported by the Japan Society for the Promotion of Science, KAKENHI (grant number 23K24531 to Takanori Iwata). We thank Dr. Kazuki Morita and Dr. Jiacheng Wang at Department of Periodontology, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University for their kind supports.
Author information
Authors and Affiliations
Contributions
S.S. performed the experiments, analyzed the data and drafted the manuscript. T.I. designed and supervised the study. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, S., Iwata, T. Role of AOX1 on RXR signaling regulates osteoblastogenesis in hPDLMSCs. Sci Rep 14, 16767 (2024). https://doi.org/10.1038/s41598-024-68009-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68009-2
- Springer Nature Limited