Abstract
Skin diseases are prevalent globally and can have detrimental effects on the individual’s health-related quality of life (HRQoL). The treatment of dermatological patients typically focuses on clinical signs and symptoms and a subjective view of the impact of the disease on the patient’s life. Assessing quality of life can help provide patients with better service, by acknowledging their real needs and interfering with treatment decisions. The aim of the study was therefore to assess quality of life of dermatology outpatients and its associated factors. An analytical cross-sectional study was conducted in the dermatology clinic of Halibet National Referral Hospital in Asmara, Eritrea. HRQoL data were collected between May 6 and August 18, 2022 using a validated standard tool (Skindex-29). Descriptive statistics, logistic regression and paired t-test were employed using Statistical Package for Social Sciences (Version-26.0). A total of 375 dermatology clinic out-patients with a median age of 29 (Interquartile range: 25) were included in the study. The most commonly seen skin diseases were eczema, seborrhoeic dermatitis and tinea pedis. Emotion, symptom, and functioning domains of HRQoL were severely impaired in 75.7%, 50.4% and 57.6% of all dermatology outpatients, respectively. More than half of the respondents (57.9%) had a severely impaired overall HRQoL. In the overall HRQoL, being a rural resident [Adjusted Odds Ratio (AOR) 1.98, 95% CI 1.18, 3.33] and presence of chronic illness (AOR 2.16, 95% CI 1.22, 3.82) were significantly associated with severely impaired overall quality of life. A significantly higher mean score (p < 0.001) was observed in emotion [Mean (M) = 55.60, Standard Deviation (SD) = 21.0] as compared to functioning (M = 46.89, SD = 21.2). On the other hand, significantly higher mean score (p < 0.001) was observed on symptom (M = 54.08, SD = 20.5) as compared to functioning (M = 46.89, SD = 21.2). Skin diseases severely affected the emotion, functioning, and symptom domains of health-related quality of life. This highlights the importance of providing physical and psychosocial support to patients with dermatologic problems.
Similar content being viewed by others
Introduction
Skin diseases are commonly reported health conditions with a significant global public health burden and considerable disability1. Patients with skin diseases may experience severe symptoms such as itching, pain, and discomfort, which can have a profound psychological impact. Moreover, patients with severe dermatologic conditions and lower disease-specific health-related quality of life are more likely to seek extensive medical services2. Doctors are often focused on accurate diagnosis and appropriate treatment of patients’ skin conditions. Although they are aware of the devastating effect of patient’s skin condition on their lives, their quality of life, and the economic and social impact of their disease may earn little attention which could further complicate the condition3. Hence, doctors are encouraged to closely pay attention to the improvement of overall well-being of their patients, as different studies has revealed that, the severity of skin conditions are found to be associated with severely impaired quality of life3,4,5,6,7. Many skin conditions, such as psoriasis, eczema, vitiligo, acne vulgaris, and cutaneous lupus erthyromytosis are rarely life threatening, but they can negatively affect patient’s quality of life8,9,10.
According to a study of the global burden of disease project, skin diseases are responsible for causing 41.6 million disability-adjusted life years making them the fourth leading cause of non-fatal morbidity worldwide11,12. Chronic skin diseases have long-term negative effect on patients’ health-related quality of life, thus it is paramount to have a better understanding of the effect of these diseases and their determinants8. Several risk factors are associated with impaired health-related quality of life13,14. The interaction of skin conditions and their psychological effect, however, is complex, and difficult to identify the root causes. Patients’ self-image, identity, socialization, sexuality, perception and fear of their disease conditions among others were found to be determinants of the overall quality of life of patients attending dermatology clinic15,16,17. It is also important to note that the diagnosis of skin condition and its chronicity were also identified as determinants of the patients’ quality of life15. Despite the above-mentioned facts, management of skin diseases usually focuses on clinical signs and symptoms and on a subjective view of the impact of the disease on the patients’ life18. According to the World Health Organization, quality of life (QoL) is defined as the perception of individuals of their current situation considering their culture and their relationship value system with their goals, expectations, standards and concerns, and their impact on physical health, mental conditions and independency of social relationships19. QoL measures can potentially allow dermatologists to record and monitor a patients progress with valid and reliable methods that allow intrapersonal and interpersonal comparisons3.
Assessing QoL is important to identify individual, societal and institutional drivers for skin condition-related health problems and guide policy decisions on the risk mitigation plans that need to be in place. No previous study was conducted in Eritrea to measure the quality of life of patients with a wide range of skin conditions. The aim of the study was therefore to assess quality of life of dermatology outpatients and its associated factors in the dermatology clinic of Halibet National Referral Hospital.
Materials and methods
Study design and setting
An analytical cross-sectional study with a quantitative approach was conducted in the dermatology clinic of Halibet National Referral Hospital in Asmara, Eritrea. It is the only national referral hospital with a well-established dermatology department providing services to patients with various skin diseases. In Eritrea, healthcare services are highly accessible and affordable, provided at heavily subsidized or nominal costs through the public health system. The healthcare delivery model is structured on a three-tier basis: the primary level consists of health stations, health centers, and community hospitals, serving as the initial point of contact for patients. The secondary level comprises regional referral hospitals and second-contact hospitals within sub-regions, to which patients are referred from the primary level. The tertiary level is made up of national referral hospitals located in the capital city, Asmara. Patients can be referred to higher-level facilities by their healthcare providers, or they can be self-referred directly to secondary or tertiary hospitals if they deem it necessary. This allows for a streamlined and accessible healthcare system that caters to the diverse medical needs of the population. Data were collected from May 6 to August 18, 2022 for a period of 90 working days.
Source and study population
All outpatients attending the dermatology clinic during the study period were the source population. Patients aged 18 years and above who were diagnosed with any skin diseases and willing to participate formed the study population.
Sample size and sampling technique
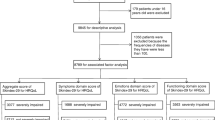
The sample size was computed by considering the finite population correction factor formula: n = NZ2pq/ [pqZ2 + (N−1)d2]. The total sample size (n) was calculated using the following assumptions: expected proportion of patients whose QoL was severely affected by skin disease (p) and those whose QoL is not severely affected by skin disease (q) were taken as 0.5, Z statistic for 95% level of confidence (Z = 1.96), estimated population size (N) of 2700, margin of error (d) of 0.05 and 10% non-response rate. Considering the above assumptions, the final sample size was 375. A systematic random sampling was employed to select subjects from the study population.
Data collection tool and approach
A structured and assisted self-administered data collection tool was used to collect data. The data collection tool had two sections. Section A was intended to record the socio-demographic and background characteristics of the patients such as age, sex, educational level, religion, ethnicity, occupation, and presence of chronic illness. Section B contained a standard and validated tool (Skindex-29) to assess the patients’ health-related quality of life (HRQoL). Skindex-29 consists of 30 items, of which 29 items (with the exception of item 18: side-effects of treatments) are assigned in three domains such as emotions (10 items), symptoms (7 items) and functioning (12 items). Permission to use Skindex-29 was granted from MAPI Research Trust (the organization holding the copyright for the use of the tool). Evidence suggested that this tool exhibits good psychometric properties in terms of measuring HRQoL20. The data collection tool was translated into local language (Tigrigna), translated back to English to assure consistency and finally to Tigrigna by three language and literature experts.
The investigators explained purposes of the study to the participants during their dermatology outpatient visit and those who gave written consent were enrolled in the study. Diagnosis of the skin disease was confirmed by two experienced physicians working in the outpatient dermatology clinic. After confirming the diagnosis, the data collection tool was self-administrated to each patient and filled in a separate room within the dermatology clinic. Besides, a face-to-face interview was conducted for those patients with no formal education and one patient was interviewed at a time to ensure privacy. During submission, investigators checked the filled questionnaire for completeness.
Variables
Quality of life of the dermatology outpatients was considered the dependent variable and the independent variables were socio-demographic and background characteristics such as age, sex, educational level, religion, ethnicity, occupation, and presence of chronic illness.
Variable measurement and interpretation
Quality of life was measured with Skindex-29 using 5-point Likert scale ranging from ‘never’ to ‘all the time’. As per the scale guideline, a score of ‘0’, ‘25’, ‘50’, ‘75’ and ‘100’ was given to the responses ‘never’, ‘rarely’, ‘sometimes’, ‘often’ and ‘all the time’, respectively. A scale score was computed by dividing the mean of a patient’s responses by the items in a given scale. On the other hand, as per the scale guideline, missing of more than 25% of responses to an item, missing of more than 25% of the items in a domain, and an item with multiple answers (considered as missing item) were not present in this study. Higher score within domains illustrated a higher impact of the skin disease on the patients’ quality of life.
According to a literature, the Skindex-29 cut-off scores for severely impaired HRQoL were recognized and showed to have the highest accuracy3. As such, the cut-off scores for severely impaired HRQoL of ≥ 52 points on symptoms, ≥ 39 on emotions, ≥ 37 on functioning, and ≥ 44 on the total score were used in this analysis.
Quality assurance
The data collection tool (along with Tigrigna Version of Skindex-29) was peer-reviewed by a panel of experts in the fields of medicine, pharmacy, pharmaco-epidemiology, public health, and epidemiology to verify face and content validity. The data collection tool was then modified as per the comments given by the experts and subject to a pre-test. The pre-test was conducted on 38 participants from 13 to 16 April, 2022 in the dermatology outpatient clinic of Halibet National Referral Hospital. It aided in assessing translation accuracy, estimation of time needed to complete the questionnaire, and familiarizing data collectors. A two-day training workshop was provided for data collectors to clearly understand the study objectives, questionnaires, and approach of conducting the face-to-face interview. To ensure reliability, two pharmacists, NB and TT, who had prior similar experience were selected and oriented to conduct the data collection so as to understand the within and between inter-rater uniformity.
Statistical analysis
The collected data were entered using CSPro (version 7.0), cleaned and exported to IBM Statistical Package for Social Sciences (SPSS) [Version 26.0] for statistical analysis. Descriptive analysis was performed using percentages and mean (Standard Deviation (SD)). The scores of the domains of QoL were computed from the respective items and converted to 100%. Furthermore, the scores were categorized into binary as per the guidelines of the Skindex-29 tool. The factors that affect the domains of QoL and total QoL binary responses were assessed primarily using bivariate logistic regression. Factors that were significant at bivariate were retained for multivariable logistic regression and adjusted odds ratios (AORs) were computed consequently as a measure of association. To determine which domain of the QoL is highly affected, paired t-test was employed for comparisons. Tables and figures were used to present the results. The level of significance for all variables was tested at p value less than 0.05.
Ethical approval and consent to participate
Ethical approval was obtained from Ministry of Health (MOH) research ethics and protocol review committee (reference number: 03/09/2019). Besides, permission was obtained beforehand from the medical director and head of outpatient department of the dermatology clinics of Halibet national referral hospital where the actual study and the pre-test were conducted. Study participants were informed about the objectives of the study and written informed consent was obtained before enrollment into the study. Information obtained from this study was kept confidential and used only for this study’s purpose. This study conforms to the principles outlined in the Declaration of Helsinki (2013).
Results
Socio-demographic and background characteristics
A total of 375 participants with a median age of 29 (IQR: 25) were enrolled in the study. Two-hundred and one participants (53.6%) were males. The majority of the participants were urban inhabitants (77.3%), aged between 18 and 40 years (67.2%), and completed their secondary education (49.6%). Moreover, 56% of the participants were employed, and 81.6% of them had no chronic illness (Table 1). Detailed socio-demographic and background characteristics of the study population are depicted in Table 1.
Of the 375 participants, a total of 516 skin diseases were documented. The most commonly observed skin diseases were eczema (10.1%, n = 52), seborrhoeic dermatitis (7.9%, n = 41), tinea pedis (7.2%, n = 37) and acne vulgaris (5.6%, n = 29) (Table 2).
Quality of life of the dermatologic outpatients using Skindex-29
In the emotion domain, majority of the respondents (n = 260/375, 69.3%) reported that they frequently worried that their skin condition might get worse. Moreover, most of them (61.6%) frequently worried about getting scars from their skin conditions. However, only one in five of the participants (19.5%) reported that they frequently get frustrated by their skin condition (Table 3). The mean (SD) score of the emotion domain was 55.60 (21.0) out of 100. A total of 284 participants had a severely impaired emotion domain (Fig. 1).
Furthermore, in the domain of symptoms, more than half of the respondents (56%) experienced skin itching all the time. Besides, about 44.5% of them reported that their skin condition frequently burns or stings. On the other hand, 72% of the participants reported that water rarely bothered their skin condition during bathing and hand washing. The mean (SD) score of the symptoms domain was 54.08 (20.5) out of 100. One-hundred eighty-nine of all the participants had severely impaired symptom domain.
In the functioning domain, about 38.7% of the respondents reported that their skin condition made it hard to work or do hobbies and it also affected their social life. Out of 328 participants who started a sexual life, 79.3% reported that their skin condition rarely interfered with their sex life. Moreover, 70.9% of the respondents reported that their skin condition made showing affection difficult. The mean (SD) score of the functioning domain was 46.89 (21.2) out of 100. A total of 216 participants had a severely impaired functionality (Fig. 1).
The overall mean (SD) score of the quality of life was 51.44 (18.9) out of 100. A total of 217 (57.9%) of the study participants had severely impaired QoL (Fig. 1).
Of the commonly seen skin diseases, patients with eczema, lichen planus, seborrhoeic dermatitis, psoriasis, acne vulgaris, and vitiligo had a severely impaired HRQoL outcome (Table 4). However, patients with pityriasis versicolor had no severely impaired HRQoL outcome.
Determinants of health-related quality of life
Binary logistic regression analysis revealed that patients aged 41–59 years old (Crude Odds Ratio (COR) 1.93, 95% CI 1.16, 3.21), those with no formal education (COR 2.74, 95% CI 1.26, 5.98), patients with a primary educational level (COR 3.29, 95% CI 1.53, 7.06), and rural residents (COR 2.00, 95% CI 1.22, 3.29) were found to have a significant association with severely impaired QoL within the symptom domain (Table 5). Furthermore, those with a primary educational level (COR 3.19, 95% CI 1.20, 8.46) and chronic illness (COR 2.49, 95% CI 1.18, 5.25) were significant associates of severely impaired QoL within the emotion domain.
In the functioning domain, patients aged 60 and above (COR 0.41, 95% CI 0.21, 0.80), rural residents (COR 1.68, 95% CI 1.01, 2.79), and those with chronic illness (COR 2.09, 95% CI 1.19, 3.69) were significantly associated with severely impaired QoL. Besides, being a rural resident (COR 1.90, 95% CI 1.13, 3.18) and presence of chronic illness (COR 2.07, 95% CI 1.17, 3.64) were significantly associated with severely impaired QoL within the overall HRQoL.
Multivariable logistic regression indicated that dermatology patients with a primary educational level were two times more likely to experience severely impaired symptom than those with a higher education (AOR 2.60, 95% CI 1.12, 6.03). Moreover, rural residents were approximately two times more likely to experience severely impaired symptom than urban residents (AOR 1.71, 95% CI 1.02, 2.86) (Table 6).
Dermatology patients with a primary educational level were approximately three times more likely to experience severely impaired emotions than those with a higher education (AOR 2.94, 95% CI 1.10, 7.86). Patients with chronic illnesses were two times more likely to experience severely impaired emotions than their counterparts (AOR 2.36, 95% CI 1.11, 4.99).
The elderly population was 64% less likely to experience severely impaired functioning than adults (AOR 0.36, 95% CI 0.18, 0.73). Moreover, rural residents were approximately two times more likely to experience severely impaired functioning than urban residents (AOR 1.82, 95% CI 1.08, 3.08). Patients with chronic illnesses were two times more likely to experience severely impaired functioning than their counterparts (AOR 2.21, 95% CI 1.23, 3.98).
In terms of overall health-related quality of life, rural residents were approximately two times more likely to experience severely impaired quality of life than urban residents (AOR 1.98, 95% CI 1.18, 3.33). Patients with chronic illnesses were two times more likely to experience severely impaired quality of life than their counterparts (AOR 2.16, 95% CI 1.22, 3.82) (Table 6).
A Chi-square test for trend analysis indicated that there was no significant association between the number of skin diseases in an individual patient and the overall quality of life outcome (χ2 = 2.34, p = 0.126) (Table 7).
Comparison of the domains of quality of life
Paired comparison of the domains of QoL revealed significantly higher mean score (p < 0.001) in emotion (M = 55.60, SD = 21.0) as compared to functioning (M = 46.89, SD = 21.2). On the other hand, significantly higher mean score (p < 0.001) was observed on symptom (M = 54.08, SD = 20.5) as compared to functioning (M = 46.89, SD = 21.2). However, the mean scores of emotion and symptom were not significantly different (MD = 1.51, 95% CI − 0.31, 3.33, p = 0.103) (Fig. 2).
Discussion
Skin diseases compromise the quality of life of dermatology patients. The problems encountered from skin diseases include physical, psychological, and social consequences21. In this study, skin diseases severely impaired the health-related quality of life of study participants in terms of symptoms, emotions, and functioning. The majority of the dermatology outpatients experienced negative emotional effects from their skin diseases worrying about the severity, scarring, and worsening of their condition. Moreover, two out of five subjects felt depressed due to their skin condition. Skin diseases often lead to changes in appearance and negative body image which are associated with poor quality of life16. When patients face new symptoms or conditions, they react with fear and concern, impacting their well-being and treatment outcomes17. Dermatology patients are also more likely to experience psychiatric comorbidities compared to healthy individuals22. Our findings emphasize the importance of addressing adverse psychological outcomes associated with skin diseases which was in line with studies conducted in China8, South Korea23, and the UK24. Therefore, providing psychological support to dermatology patients is crucial due to the increased risk of psychiatric problems associated with skin diseases. This is supported by a UK study where 77% of the respondents would benefit from more psychological support24.
For about half of the respondents, skin diseases severely affected their quality of life in terms of symptoms. Most of them experienced constant itching, burning, or stinging. One out of five patients reported that water worsened their skin condition during bathing and hand washing. The symptoms associated with skin diseases can compromise the quality of life of patients thereby leading to subjective distress and emotional problems. In similar studies, physical symptom was found to be associated with greatest impact on their HRQoL6,22. In another study, patients with skin presentation of rashes compared to lesions were also found to have a severely impaired quality of life. Moreover, patients with extensive area of skin involvement suffer far greater than patients with skin cancer25.
More than half of the dermatologic outpatients experienced severely impaired functioning due to their skin condition. Several patients reported limitations in daily work and social life interaction, hobbies, and/or forced to stay at home. This aligns with findings of another study, that reported the skin conditions negatively affect patients’ routine activities and their social interactions and was associated with increased psychiatric morbidity7. Acquiring a primary educational level and being a rural resident were significantly associated with severely impaired quality of life within the symptom domain. Moreover, having a primary educational level and presence of systemic chronic illness were significantly associated with severely impaired emotional domain.
Being a rural resident and presence of systemic chronic illness were significantly associated with severely impaired functional domain and quality of life in general which is similar to findings reported from Belgium26. In other comparable study, individuals who are unemployed or living in rural areas were significantly affected4. Presence of other systemic chronic illness can aggravate the quality of life of patients which urges healthcare professionals and program managers to focus on a holistic approach that includes psychotherapy to improve the overall QoL of patients.
Moreover, dermatologic patients aged 18–40 years were significantly associated with severely impaired functioning likely due to unique challenges they face. The visibility and stigma of skin conditions can have a greater impact on socially and professionally active adults. Moreover, the psychosocial effects, such as poor body image and low self-confidence, could be more detrimental for adults with a well-established sense of identity and social dynamics. Hence, it is important to pay attention to optimal care that targets all aspects of health problems thereby improving their life conditions. As per the findings of the study, patients with atopic dermatitis (eczema), lichen planus, seborrhoeic dermatitis, psoriasis, acne vulgaris, and vitiligo were found to have significantly impaired overall QoL and had shown a profound psychosocial impairment. However, in a similar study conducted in Saudi Arabia, patients with eczematous dermatitis, connective tissue diseases and immunological disorders scored significantly higher in the symptom domain27.
The skin is certainly the most visible organ determining appearance and skin diseases have a detrimental effect on physical, emotional and functional domains of quality of life outcome and social interaction. The importance of this research and its findings are probably of specific interest to countries with socio-economic and cultural status similar to that of Eritrea. Program managers and policy makers are recommended to introduce psychosocial support activities in dermatologic clinics and organize continuous awareness-raising program on early treatment and understanding of skin disease. Besides, dermatologists and other healthcare professionals need to consider treating the soul along with the body to minimize impact of skin diseases.
Limitation of the study
Due to the cross-sectional nature of the study, cause-effect relationship could not be established. This study was conducted in dermatology clinic of a tertiary care hospital, and thus, the findings could not be generalizable to other similar patients attending primary and secondary level health facilities.
Conclusion
Skin diseases severely affected the emotional, functional and symptom domains of health-related quality of life of dermatologic patients. Overall, being a rural resident and having a chronic illness were significantly associated with severely impaired quality of life. To improve the quality of life of patients, program managers and health facility managers should consider introducing psychosocial support in dermatology clinics.
Data availiability
The data used in this study and Tigrigna version of Skindex-29 are available from the corresponding author and can be accessed upon reasonable request.
Abbreviations
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- COR:
-
Crude odds ratio
- HRQoL:
-
Health-related quality of life
- IQR:
-
Interquartile range
- M:
-
Mean
- MD:
-
Mean difference
- Md:
-
Median
- MOH:
-
Ministry of Health
- SD:
-
Standard deviation
- SPSS:
-
Statistical package for social sciences
- QoL:
-
Quality of life
- WHO:
-
World Health Organization
References
Hay, R. J. et al. The global burden of skin disease in 2010: An analysis of the prevalence and impact of skin conditions. J. Investig. Dermatol. 134, 1527–1534 (2014).
Verhoeven, E. W. et al. Skin diseases in family medicine: Prevalence and health care use. Ann. Family Med. 6, 349–354 (2008).
Finlay, A. Y. The burden of skin disease: Quality of life, economic aspects and social issues. Clin. Med. 9, 592 (2009).
Nguyen, S. H. et al. Health-related quality of life impairment among patients with different skin diseases in Vietnam: A cross-sectional study. Int. J. Environ. Res. Public Health 16, 305 (2019).
Gurel, M. S., Yanik, M., Simsek, Z., Kati, M. & Karaman, A. Quality of life instrument for Turkish people with skin diseases. Int. J. Dermatol. 44, 933–938 (2005).
Ahmad Fuat, M. S., Mat Yudin, Z., Muhammad, J. & Mohd Zin, F. Quality of life and Its associated factors among patients with psoriasis in a semi-Urban Northeast Malaysia. Int. J. Environ. Res. Public Health 19, 11578 (2022).
Zachariae, R., Zachariae, C., Ibsen, H. H. W., Mortensen, J. T. & Wulf, H. C. Psychological symptoms and quality of life of dermatology outpatients and hospitalized dermatology patients. Acta Dermato Venereol. 84, 205–212 (2004).
He, Z. et al. Factors affecting health-related quality of life in patients with skin disease: Cross-sectional results from 8,789 patients with 16 skin diseases. Health Qual. Life Outcomes 18, 1–9 (2020).
Jayaprakasam, A., Darvay, A., Osborne, G. & McGibbon, D. Comparison of assessments of severity and quality of life in cutaneous disease. Clin. Exp. Dermatol. 27, 306–308 (2002).
Lasek, R. J. & Chren, M.-M. Acne vulgaris and the quality of life of adult dermatology patients. Arch. Dermatol. 134, 454–458 (1998).
Karimkhani, C. et al. Global skin disease morbidity and mortality: An update from the global burden of disease study 2013. JAMA Dermatol. 153, 406–412 (2017).
Seth, D., Cheldize, K., Brown, D. & Freeman, E. E. Global burden of skin disease: Inequities and innovations. Curr. Dermatol. Rep. 6, 204–210 (2017).
Ahmed, A., Leon, A., Butler, D. C. & Reichenberg, J. Quality-of-life effects of common dermatological diseases. Semin. Cutan. Med. Surg. 32, 101–109 (2013).
Balieva, F. The psychological burden and life quality in patients with skin disease: A European study in dermatological patients. http://urn.nb.no/URN:NBN:no-73810 (2019).
Saimbi, D., Raju, M., Dubey, V. & Dey, V. K. Skindex-29 to determine quality of life and emotional factors in dermatological conditions. Ann. Natl. Acad. Med. Sci. (India) 53, 041–050 (2017).
Potocka, A., Turczyn-Jablonska, K. & Kiec-Swierczynska, M. Self-image and quality of life of dermatology patients. Int. J. Occup. Med. Environ. Health 21, 309 (2008).
Martínez-García, E., Affleck, A., Rakvit, P., Arias-Santiago, S. & Buendía-Eisman, A. Exploring patients’ insight, concerns, and expectations at dermatology clinic: An observational study in 2 Centers in Scotland and Spain. J. Patient Exp. 7, 1197–1202 (2020).
David, S., Ahmed, Z., Salek, M. & Finlay, A. Y. Does enough quality of life-related discussion occur during dermatology outpatient consultations?. Br. J. Dermatol. 153, 997–1000 (2005).
Haas, B. K. Clarification and integration of similar quality of life concepts. Image J. Nurs. Scholarsh. 31, 215–220 (1999).
Lewis, V. & Finlay, A. Y. Journal of Investigative Dermatology Symposium Proceedings 169–180 (Elsevier).
Basra, M. K. & Shahrukh, M. Burden of skin diseases. Expert Rev. Pharmacoecon. Outcomes Res. 9, 271–283 (2009).
Tejada, C. D., Mendoza-Sassi, R. A., Almeida, H. L. Jr., Figueiredo, P. N. & Tejada, V. F. Impact on the quality of life of dermatological patients in southern Brazil. An. Bras. Dermatol. 86, 1113–1121 (2011).
Lee, S. H. et al. Psychological health status and health-related quality of life in adults with atopic dermatitis: A Nationwide cross-sectional study in South Korea. Acta Dermatol. Venereol. 98, 89–97 (2018).
Kanji, A. Perspective on living with a skin condition and its psychological impact: A survey. J. Patient Exp. 6, 68–71. https://doi.org/10.1177/2374373518774397 (2019).
Shah, M. & Coates, M. An assessment of the quality of life in older patients with skin disease. Br. J. Dermatol. 154, 150–153 (2006).
Van Wilder, L. et al. The impact of multimorbidity patterns on health-related quality of life in the general population: Results of the Belgian Health Interview Survey. Qual. Life Res. 31, 551–565. https://doi.org/10.1007/s11136-021-02951-w (2022).
Abolfotouh, M. A. et al. Quality of life in patients with skin diseases in central Saudi Arabia. Int. J. Gen. Med. 5, 633–642 (2012).
Acknowledgements
The authors sincerely thank the study participants for their time and willingness to participate in the study. The authors also greatly acknowledge the support of Dr Luul Banteyrga (Medical Director of Halibet National Referral Hospital), Dr. Yonas Kflay, Dr. Habtom Gebrekidan, and all staff of the dermatology clinic of the hospital in facilitating the data collection process.
Funding
There was no source of funding for the study or manuscript preparation.
Author information
Authors and Affiliations
Contributions
N.A. and D.G.W. conceived the idea. All the authors participated in the design of the study protocol. T.T. and N.B. collected the data. E.H.T. performed the statistical analysis. N.A. assisted in analyzing the data and interpreting the results analyzed. The manuscript was drafted by T.T., N.A., D.G.W. and E.H.T. and finally critically reviewed for its intellectual content by N.B. and M.R.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tewelde, T., Abdu, N., Weldemariam, D.G. et al. Quality of life of dermatology outpatients and its associated factors in Halibet National Referral Hospital in Asmara, Eritrea. Sci Rep 14, 16272 (2024). https://doi.org/10.1038/s41598-024-67224-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67224-1
- Springer Nature Limited