Abstract
Objectives
Evidence shows that majority of dermatological disorders affect the health-related quality of life (HRQoL) of patients. However, the extent of its negative impact and predictors has not been studied in Ethiopia. Thus, this study looked at assessing the HRQoL and determinants in patients with dermatological disorders (DDs) attending the University of Gondar Comprehensive Specialized Hospital (UoGCSH).
Results
Patients with dermatological disorders (n = 400) were included in the final analysis using a systematic random sampling technique. The mean age of the participants was 39.79 (± 17.17) years. The average (± SD) score of EQ-5D-5 L was 1.92 (± 0.74). Regarding domains, pain/discomfort accounted for a higher proportion 59 (22.3%) followed by anxiety/depression 61 (15.3%). Receiving topical preparations (β = -0.399, 95% CI: -0.6, − 0.19; < 0.001), systemic only medication (β = -0.378, 95% CI: -0.607, -0.149; p = 0.002), having slight, mild, and moderate skin diseases found to have an inverse association with impaired HRQoL, (β = -0.654, 95% CI; -1.01, -0.290); p < 0.001), (β = -0.748, 95% CI: -0.960, -0.538; p < 0.001), and (β = -0.465, 95% CI: -0.642, -0.283; p < 0.001), respectively. Furthermore, age (β = 0.011, 95% CI: 0.006, 0.016; p = 0.001), long duration with skin disease (β = 0.046, 95% CI: 0.015, 0.352; p = 0.013), and presence of comorbidity (β = 0.251, 95% CI: 0.096, 0.402; p = 0.002) were significant predictors of HRQoL among dermatological disease patients.
Conclusion
Patients with dermatological disease were found to have a compromised HRQoL. Pain /discomfort problems accounted for a higher proportion compared with other domains. Socio-demographic, clinical and medication-related variables were significantly associated with HRQoL.
Similar content being viewed by others
Introduction
Dermatological disorders (DDs) have a significant global public health impact, among the top 10 global diseases [1,2,3]. The most common prevalent skin disorders include acne, atopic dermatitis (eczema), psoriasis, rosacea, skin cancers, vitiligo, herpes zoster, sunburn, tinea pedis, melasma, and contact dermatitis [3].
Most of DDs are chronic and significantly reduce HRQoL among its patients [4]. This disorders are the fourth leading cause of non-fatal diseases, accounting for approximately 1.79% of total disease in the 2013 global burden report [5]. If DDs are not treated properly, several complications can occur [6]. In studies conducted in the United Kingdom [4] and Malaysia [7], the major complications of DDs and their impact on the physical, social, and psychological aspects of a patient’s HRQoL were reported. To accurately determine the impact of burden of skin disease, the patients’ HRQoL must also be considered [8].
Skin diseases have a negative impact on HRQoL. Various studies reported a negative impact of skin disorders including psoriasis, acne vulgaris, cutaneous lupus erythematous, alopecia areata, urticaria, and vitiligo on HRQoL [9,10,11,12,13,14]. A number of variables have been linked to the HRQoL of patients with a specific skin condition. For example, psoriasis patients’ HRQoL is associated with their age, employment status, marital status, disease duration, and self-reported severity [14]. The HRQoL of patients with cutaneous lupus erythematous is influenced by their gender, age, generalized disease, distribution of lesions, and severity [10]. Another study also disclosed that a correlation between low HRQoL and sex, education, income, the presence of systemic lupus erythematous, and disease severity of patients living with DDs [13]. Moreover, socioeconomic factors including large joint families, use of impure water, low education status and exchange of footwear with patients are the major contributing factors. The incidence rate of skin disorders is high due to these factors in resource-limited countries [5].
Despite the fact that they are classified as chronic diseases and among the top four most common diseases affecting the world population [15], the impact of skin disorders is widely underestimated. The direct and indirect cost of treating skin diseases in the United States was 75 and 11 billion US dollars (USD), respectively [5].
Dermatological disorders such as vitiligo and psoriasis affect majority of people of all races. Extensive affected skin may result in social withdrawal, low personal relationships, embarrassment in sexual function, stigmatization, distress, anxiety, and difficulty finding work, all of which can lead to depression and quality of life impairments. Despite significant dermatologic complications and their association with poor HRQoL, no study has used an EQ-5D-5 L to assess health-related quality of life and associated factors in patients with DDs in Ethiopia. The European Quality of Life Group developed the EQ-5D-5 L, a generic, multi-attribute, utility-based health status tool that has recently been advocated to assess patients’ self-reported experiences and perceptions about their health status [16]. Mobility, self-care, daily activities, pain or discomfort, and anxiety or depressive symptoms are the five components of this tool [17]. As a result, this is the first study to use the EQ-5D-5 L to assess HRQoL in patients with DDs. Furthermore, a better understanding of these variables and the establishment of a utility value may improve intervention design and evaluation, as well as the integration of HRQoLassessment during patient care and decision-making.
HRQoL measurements in patients with DDs are extremely important. Besides evaluating treatment plans, dermatologists can learn more about the psychosocial difficulties of skin-related illness patients by assessing HRQoL. Additionally, HRQoL evaluation can highlight the need for psychosocial and psychotherapy interventions in a specific patient [18]. In the vast majority of cases, DDs do not pose a life-threatening risk but greatly impact the patient’s emotional status, social relationships, and daily activities. Many times, assessing the impact of a disease differs between the patient and doctor, which can interfere directly with disorder management. The analysis of HRQoL questionnaire responses allows establishing a relationship between the disease and its overall impact on patient’s life, resulting in satisfactory analysis of disease indications and treatment outcomes [19]. Since there is a lack of information on the level of HRQoand its determinants among dermatological disordered patients in Ethiopia using EQ-5D-5 L instrument, therefore, this study aimed to assess HRQoL and its determinants among different skin disease patients at Gondar University Hospital in Ethiopia.
Methods and materials
Study setting and study period
A facility-based cross-sectional study was conducted at the UoGCSH dermatologic clinic from June to August 2022. The hospital is in the Amhara Regional State of Gondar and is located approximately 750 km from Addis Ababa, Ethiopia’s capital city. It is one of the country’s largest teaching hospitals, with a catchment area of approximately 7 million people.
Study participants and sampling procedures
The study included patients aged 18 and above with any dermatologic disorder and a disease duration of more than or equal to six months. However, patients who had a history of mental illness or were physically unable to complete the survey were excluded.
Sample size and sampling procedure
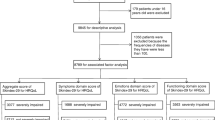
Because no studies used the EQ-5D-5 L in a similar study in Ethiopia, the sample size was determined using the single population proportion formula. To obtain a maximum sample size, an estimated proportion of patients with utility values above the average were deemed 50% and the sample size was calculated. \(n=\frac{{\left(\text{z}\frac{{\alpha }}{2}\right)}^{2}\text{p}(1-\text{p})}{{\text{d}}^{2}}\)\(n=\frac{{\left(1.96\right)}^{2}\left(0.5\right)\left(0.5\right)}{(0.05)2}=384\); where n is the required sample size, Z/2 = 1.96 (the Z score corresponds to a 95% confidence level), P is the proportion of patients with utility greater than the mean, and d is the margin of error, which was set at 0.05. A total of 422 patients were approached, with a 10% margin of error for inappropriate and non-responsive responses. To recruit participants, a systematic random sampling technique was used.
According to ambulatory dermatologic clinic records at the University of Gondar, 610 chronic patients with DDs have visited the clinic on average per month since chronic skin disease patients are advised to visit the dermatologic clinic for a minimum of one month and a maximum of three months. As a result, the total number of chronic skin disease patients visiting over three months was 1830. Given that the sample was collected within three months, the sampling fraction (k-interval) is 4.33 (approximately four). The subjects were selected randomly as per randomized sampling method for data collection.
HRQoL outcome measures
HRQoL was the primary outcome of this study. The respondents’ HRQoL was assessed using a generic EQ-5D-5 L questionnaire with a 5-level response (from 1 = no problem to 5 = extreme problem) and the EQ-VAS scale, on which the patient marks the overall state of health as a number (0 = worst imaginable state of health, 100 = best imaginable state of health). While the utility value difference between the worst and best is 0–1 (death is 0 and perfect health is 1), the EQ-5D-5 L is highly-sensitive, easy to use, and can generate a single total score based on socially relevant HRQoL measures [20, 21]. Additionally, the EQ-5D-5 L instruments have a good psychometric property in terms of reduced ceiling effects, increase informativity, improved convergent and known-groups validity to measure the health outcome of patients with DDs [22, 23].
Data collection techniques and instruments
Patients were interviewed face-to-face using Amharic questionnaires that included socio-demographic and EQ-5D-5 L scales. The socio-demographic section of the questionnaire inquiries about the respondent’s age, gender, residence, marital status, level of education, occupation, monthly income, health insurance, use of any alternative medication, medication availability, and affordability, and history of any substance use (alcohol, tobacco, or khat). Clinical characteristics were also collected by data collectors through medical chart review.
The Amharic version of the EuroQol Group’s Portable Valuation Technology (EQ-PVT) protocol was used to create the Amharic version of the EQ-5D-5 L. It was possible and culturally acceptable to estimate preferences for health states [24].
Data quality control
The study questionnaire was meticulously designed to collect all the necessary information. Data collectors were trained prior to collecting data. A pretest was conducted by randomly selecting patients from their medication records to ensure the uniformity and understandability of the data collection tool, and any necessary changes were made. The pre-tested patients were excluded from the final analysis. Data was gathered by the investigator and trained nurses. In addition, the visual method was used to recheck checklist accuracy and completeness for any missing, incorrect, or unreadable information. Any discrepancies or ambiguities were quickly resolved.
Data analysis and interpretation
Before coding, the data was checked for completeness and then entered into the Epi Info Version 7 database and exported to SPSS Version 26 for analysis. The study patients’ characteristics were described using descriptive statistics such as means, medians, proportions, tables, and figures. First, all statistical methods for all variables were checked to ensure that they met the test assumptions (normality test, correlation coefficients test, linearity test, outliers test, multicollinearity test, and homoscedasticity test), and those that did were included in the multivariable analysis (age, gender, residence, marital status, level of education, health insurance, use of alternative medication, alcohol use, khat chewing, duration of the disease, duration of the medication, treatment modality, and comorbidity). However, the following variables were excluded from the multivariable analysis due to one or more deviations from the linear regression assumption: occupation, monthly income, affordability, availability, smoking history, and type of skin diseases. The data’s linearity was investigated by plotting the dependent variable on the y-axis and the independent variables on the x-axis in separate scatter plots. To investigate the relationship between the mean HRQoL score and another continuous variable, the P-P plot was used. Similarly, by drawing a line through the center of each level’s observations, the linear relationship between categorical variables was investigated. The variables with no linear relationship to the outcome were removed from the analysis. The variation around the regression line was examined by plotting the standardized residuals vs. the standardized projected values of the dependent variable, and it was found to be constant for all xi values for each X variable. The data distribution was examined using a histogram, a normal probability map of the residuals, and the Shapiro-Wilk test, which revealed that the residuals were roughly normally distributed. The unstandardized coefficient was used to express the regression analysis results. The beta coefficient, expressed in standard deviation units, represents the average change in the dependent variable for each unit increase in the predictor variable. Bivariable and multivariable linear regression were used to identify the independent predictor variables of HRQoL. The fitness of the model was assessed, as well as the strength and direction of associations between the dependent and independent variables, using an adjusted odds ratio (AOR) and 95% confidence intervals (CI). To declare statistical significance, a p-value less than 0.05 was used. The models’ suitability was assessed using the goodness-of-fit test.
Results
Sociodemographic characteristics of participants
Total 422 dermatologic patients approached for this study, 400 (a response rate of 94.8%) were included in the final analysis. More than half of the participants (56%) were female. The participants’ mean (± SD) age was 39.8 (± 17.2) years. Higher number of the patients (58.3%) had health insurance. Half of the participants 193 (48.3%) had used traditional medications to treat their skin illnesses (Table 1).
Clinical characteristics of patients with dermatological disorders
More than 64.2% of patients started to experience dermatologic symptoms before turning 40 years old. More than half (53%) of the patients had a disease duration of fewer than 5 years. Frequency of psoriasis was the highest at 13.5%, followed by acne (11.5%) and skin infections (11.2%). Around 136 (34%) patients were living with at least one kind of coexisting disease. The majority of the participants used the topical mode of treatment (273, 68.3%) (Table 2).
The severity of dermatologic diseases
Regarding the severity of skin diseases, more than three-fourths (35.5%) of the participants had moderate skin diseases and only 3.3% of the participants were categorized as slight skin diseases according to physician diagnosis (Fig. 1).
Prescribing pattern of medications at the dermatologic clinic
In this study, patients received topical corticosteroids for treating psoriasis. The most commonly prescribed steroids are Betamethasone dipropionate, Betamethasone dipropionate plus amphotericin B, and Mometasone furoate, with frequency of 62 (15.5%),41 (10.3%), and 86 (21.5%), respectively. Methotrexate was used by 18 (4.5%) participants only (Table 3).
HRQOL of patients with dermatological disorders
The overall mean (± SD) scores of EuroQol and EQ-VAS of the participants were 1.92 (0.74) and 68.93 (24.24), respectively. Concerning HRQoL domains, pain or discomfort was the most common health problem in patients with skin diseases (22.3%), followed by anxiety or depression (15.3% (Table 4).
Associations between the HRQoL and other variables
To identify potential variables influencing the health-related quality of life of patients with various skin diseases, a linear regression analysis was used. The linear regression model fitness was tested and found to be significantly associated (F = 13.45; p < 0.001). A multivariable analysis identified factors that may be associated with HRQOL, including age, treatment modality, the severity of the skin disease, and the presence of comorbidity. The regression results showed that the model explained 44.7% of the variance, and the variance inflated factor was less than five for all variables.
Respondents whose age increased by one increased the risk of severely impaired HRQoL scores by 0.011 times (95%CI (0.006, 0.016), p < 0.001). Compared with participants who had a combination of both topical and systemic dermatologic medications, those who had only topical preparations and those who took only systemic medications had decreased risks of severely impaired HRQoL, with a β score of -0.399 (95% CI: -0.602, -0.191), p < 0.001), and a β score of -0.378 (95% CI: -0.607, -0.149), p = 0.002, respectively. Patients having slight, mild, and moderate skin diseases had less likely risk of having impaired HRQoL compared to patients who had very severe skin diseases, with a β score of -0.654 (95% CI: -1.01, -0.290), p < 0.001; a score of -0.748 (95% CI: -0.960, -0.538), p < 0.001; and a score of -0.465 (95% CI: -0.642, -0.283), p < 0.001; respectively. Respondents who had a longer duration with dermatological conditions had 0.046 times (95%CI (0.015, 0.352), p = 0.013) the risk of severely impaired HRQoL. On average, patients who had other comorbid conditions other than skin diseases had 0.251 times (95% CI (0.096, 0.402; p = 0.002) more severely impaired HRQoL than those without comorbid conditions. The above-listed variables had been identified as significant predictors of health-related quality of life, but the other variables had lost their effect on multiple variable analyses (Table 5).
Discussion
To the best of our knowledge, this is the largest cross-sectional study to look HRQoL and factors influencing a standardized HRQoL among patients with skin diseases, with the potential to account for multiple factors for dermatological disorders. The five independent factors identified (age, severity, duration, treatment modality, and comorbidity) were significantly related to HRQoL, as measured by EuroQol domain scores.
The EuroQol tool was used to assess HRQoL among patients with various DDs in this institution-based study. According to the findings of this study, the overall mean (± SD) HRQoL and VAS scores were 1.92 (± 0.74) and 68.93 (± 24.24), respectively, out of 5 and 100. Our participants’ overall mean score was higher than the findings obtained during a study at Vietnam [25]. This could be because majority of our study population was elderly, and there was significant socioeconomic difference between the study groups.
In terms of HRQoL domains, pain or discomfort and anxiety or depression were the two most significantly affected parameters. The fact that most DDs symptoms are visible, as well as the impact that emotional anguish has on daily activities and employment, may have been the most visible consequence. Our findings reaffirmed the importance of considering the psychological impairment of patients withDDs. This is consistent with previous research findings [9, 12, 26,27,28,29]. Hence the link between DDs and mental problems are related, psycho dermatology is categorized into three mechanisms: The primary psychological diseases that cause self-inflicted diseases of the skin (trichotillomania); secondary psychophysiological disorders brought on by skin conditions that cause different emotional states (stress). Third, psychiatric disorders brought on by disfiguring skin (ichthyosis, acne conglobata, vitiligo), which can result in states of fear, depression, or suicidal thoughts [30].
Dermatological disorders have a negative impact on patients’ mental and physical health [31,32,33], which can greatly decline HRQoL [32, 33]. Patients may experience sadness or anxiety circumstances that can be explained by the advent of immune problems and elevated in proinflammatory cytokine concentrations [25]. In addition to the painful or itchy conditions that patients must endure throughout the course of diseases [34, 35]. Furthermore, previous research has suggested that people with skin conditions may face social stigma as a result of their atypical skin [36, 37]. Anxiety and depression were reported by more than 70% of the participants in this study, which was higher than the prevalence of these conditions in populations with other chronic illnesses like respiratory and cardiovascular diseases [32, 36].
As expected, the severity of the illness had an effect on the HRQoL of patients with DDs. Similar findings have been reported in studies among patients with psoriasis, acne, cutaneous lupus erythematosus (CLE), and alopecia areata [9, 10, 14, 27]. The current findings also revealed a link between significantly lower HRQoL scores and disease duration, as well as other chronic diseases. This demonstrates the chronic nature of skin diseases and their long-term consequences which was also found previously among patients suffering with psoriasis [14, 26] and CLE [10]. However, no statistically significant relationships have been discovered in studies on vitiligo [11], urticaria [12], and alopecia areata [27].
The participants’ age was found to be an independent predictor of HRQoL in dermatologic patients. This finding is consistent with the findings from Portugal [38]. The cause could be age-related increases in the risk of comorbidities and physical activity limitations, which lead to poorer HRQoL. Dermatological disorder patients who received single therapy had better HRQoL than those who received combination therapy. These finding are consistent with the study conducted in Portugal they disclosed that patient those who have received single treatment had better HRQoL than those received multiple treatment [38]. This finding may be explained by the fact that single therapy has higher treatment satisfaction, fewer pills or injections, lower medication costs, and potentially fewer side effects than combination therapy.
Strengths and limitations of this study
The results of this study could be used to make several recommendations. First, patients with skin illnesses should receive appropriate pain treatment and psychological counseling services, given that anxiety, depression, and pain are extremely common in this population. In addition, using a brief, straightforward tool, regular monitoring of HRQoL should be carried out to monitor the development in addressing the disparities between various groups of people, such as socioeconomic groups of people with skin diseases.
One of the study’s strengths is that it included a large number of people with skin conditions and adjusted for a total of 12 skin conditions before identifying characteristics linked to severely reduced HRQoL. By controlling for other variables, these findings can be used to assess the likelihood of severely reduced HRQoL in patients with the common skin illnesses studied in during this study.
This study has a few methodological issues that must be addressed. First, due to the limitations of the cross-sectional design, we were unable to determine the precise causal links between predictor variables and HRQoL. As a result, more longitudinal research is required. Second, measurement error was possible because the HRQoL data were self-reported subjectively.
Conclusions
Patients with DDs were found to have compromised HRQoL. Pain/discomfort and anxiety/ depression are the two most severely affected domain of HRQoL compared to the other domain. Socio- demographic, clinical and medication related variables were significantly associated with HRQoL of DDs patients. Therefore, future researchers would be worked on HRQoL and its associated factors in patients with DDs on at lower health care facilities that may not have the infrastructure and resources available in higher level facilities.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available due to data security regulations and participant confidentiality, but are available from the corresponding author on reasonable request.
Abbreviations
- DDs:
-
Dermatological diseases
- CLE:
-
Cutaneous lupus erythematosus
- EQ-5D-5L:
-
The EuroQol-5 Dimensions-5 Levels
- HRQoL:
-
Health related quality of life
- QoL:
-
Quality of life
- UoGCSH:
-
University of Gondar Comprehensive specialized hospital
References
Bickers DR et al. The burden of skin diseases: 2004: a joint project of the American Academy of Dermatology Association and the Society for Investigative Dermatology. 2006. 55(3): p. 490–500.
Hay RJ et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. 2014. 134(6): p. 1527–34.
Jain A et al. Multi-type skin diseases classification using OP-DNN based feature extraction approach. 2022. 81(5): p. 6451–76.
Basra MK, Shahrukh MJERoP, Research O. Burd skin Dis. 2009;9(3):271–83.
Seth D et al. Global burden of skin disease: inequities and innovations. 2017. 6(3): p. 204–10.
Hameed N et al. Multi-class multi-level classification algorithm for skin lesions classification using machine learning techniques. 2020. 141: p. 112961.
Kassab YW et al. The impact of skin disorders on patients’ quality of life in Malaysia. 2019. 4: p. 001–9.
Chren M-M, Weinstock MA. Conceptual issues in measuring the burden of skin diseases. in Journal of Investigative Dermatology Symposium Proceedings. 2004. Elsevier.
Jones-Caballero M et al. Quality of life in mild to moderate acne: relationship to clinical severity and factors influencing change with treatment. 2007. 21(2): p. 219–26.
Klein R et al. Quality of life in cutaneous lupus erythematosus. 2011. 64(5): p. 849–58.
Ongenae K et al. Effect of vitiligo on self-reported health‐related quality of life. 2005. 152(6): p. 1165–72.
Staubach P et al. Quality of life in patients with chronic urticaria is differentially impaired and determined by psychiatric comorbidity. 2006. 154(2): p. 294–8.
Vasquez R et al. A multicentre, cross-sectional study on quality of life in patients with cutaneous lupus erythematosus. 2013. 168(1): p. 145–53.
Zachariae R et al. Quality of life in 6497 nordic patients with psoriasis. 2002. 146(6): p. 1006–16.
Flohr C. and R.J.B.J.o.D. Hay, Putting the burden of skin diseases on the global map. 2021, Wiley Online Library. p. 189–190.
Brauer CA et al. Trends in the measurement of health utilities in published cost-utility analyses. 2006. 9(4): p. 213–8.
Brooks R. and E.J.H.p. Group, EuroQol: the current state of play. 1996. 37(1): p. 53–72.
Augustin M et al. Quality of life measures for dermatology: definition, evaluation, and interpretation. 2012. 1: p. 148–159.
Radtke M et al. Evaluation of quality of care and guideline-compliant treatment in psoriasis. 2009. 219(1): p. 54–8.
Tran BX et al. Quality of life profile and psychometric properties of the EQ-5D-5L in HIV/AIDS patients. 2012. 10(1): p. 1–8.
van Reenen M, B.J.R.E.R F, Janssen. EQ-5D-5L user guide: basic information on how to use the EQ-5D-5L instrument. 2015: p. 9.
Koszorú K et al. Comparing the psychometric properties of the EQ-5D-3L and EQ-5D-5L descriptive systems and utilities in atopic dermatitis. 2023. 24(1): p. 139–52.
Yfantopoulos J, Chantzaras A, J.A.o.D S. Assessment of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in psoriasis. 2017. 309: p. 357–70.
Welie AG et al. Valuing health state: an EQ-5D-5L value set for Ethiopians. 2020. 22: p. 7–14.
Nguyen SH et al. Health-related quality of life impairment among patients with different skin diseases in Vietnam: a cross-sectional study. 2019. 16(3): p. 305.
He Z et al. Factors affecting health-related quality of life in patients with skin disease: cross-sectional results from 8,789 patients with 16 skin diseases. 2020. 18(1): p. 1–9.
Janković S et al. Quality of life in patients with alopecia areata: a hospital-based cross‐sectional study. 2016. 30(5): p. 840–6.
Lee SH et al. Psychological health status and health-related quality of life in adults with atopic dermatitis: a nationwide cross-sectional study in South Korea. 2018. 98(1): p. 89–97.
Sampogna F et al. Association between poorer quality of life and psychiatric morbidity in patients with different dermatological conditions. 2004. 66(4): p. 620–4.
Kieć-Swierczyńska M et al. The role of psychological factors and psychiatric disorders in skin diseases. 2006. 57(6): p. 551–5.
Balp M-M et al. The impact of chronic urticaria from the patient’s perspective: a survey in five european countries. 2015. 8(6): p. 551–8.
Møller AH et al. A systematic literature review to compare quality of life in psoriasis with other chronic diseases using EQ-5D-derived utility values. 2015. 6: p. 167.
Yang Y, Brazier J, L.J.T.E.J.o.H E, Longworth. EQ-5D in skin conditions: an assessment of validity and responsiveness. 2015. 16(9): p. 927–39.
Lasek RJ, Chren M-MJAoD. Acne vulgaris and the quality of life of adult dermatology patients. 1998. 134(4): p. 454–8.
O’Donnell B et al. Chronic urticaria: impact on quality of life. 1997. 136(2): p. 197–201.
Hrehorów E et al. Patients with psoriasis feel stigmatized. 2012. 92(1).
Reich K et al. Once-weekly administration of etanercept 50 mg improves patient-reported outcomes in patients with moderate-to-severe plaque psoriasis. 2009. 219(3): p. 239–49.
Prazeres F, Santiago LJH. and q.o.l. outcomes, relationship between health-related quality of life, perceived family support and unmet health needs in adult patients with multimorbidity attending primary care in Portugal: a multicentre cross-sectional study. 2016. 14(1): p. 1–11.
Acknowledgements
We forward our appreciation to the clinical directors of UoGCSH for allowing us to conduct this research. Our special appreciation goes to the study participants for their volunteer participation.
Funding
The study did not get any funding.
Author information
Authors and Affiliations
Contributions
EAB participated in the conception, data curation, methodology, and project administration. AKS contributed in data curation, methodology, validation and interpreted the data. The initial manuscript was written by all contributors. The final manuscript was read and approved by both authors, who also supplied the material and a critical review.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance and approval were obtained from the Institutional review board (IRB) of the University of Gondar on June 26/2022 with a reference number (SOP/257/2022). Hospital directors and heads of the Department of Dermatology were informed about the purpose of the study to obtain agreement cooperation on. In order to protect respondent privacy throughout the gathering and analyzing of data, survey medical files digits rather than patient identifiers were used. All of the data collecting equipment was locked securely PI password-protected the databases for constrained access throughout the duration of the investigation. The data was only used to achieve the study’s objectives. Written informed consent was obtained directly from participants for those read and write and consent from a parent and/or legal guardian was secure for the illiterate population after explaining the study’s goal and purpose and. Also, each subject was made aware that engagement was optional and that they could end the study at any point if they felt uncomfortable with the questionnaires. All methods were performed with the relevant guidelines and regulations. No conflicts of interest were risen during this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Belachew, E.A., Sendekie, A.K. Health-related quality of life and its determinants in patients with different dermatological disorders at the University of Gondar Comprehensive Specialized Hospital. BMC Res Notes 16, 191 (2023). https://doi.org/10.1186/s13104-023-06442-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-023-06442-8