Abstract
The outcomes of patients with sepsis are influenced by the contractile function of the right ventricle (RV), but the impact of cardiopulmonary interaction in ICU-mortality of sepsis patients remains unclear. This study aims to investigate the ICU-mortality impact of right ventricular-pulmonary artery (RV-PA) coupling in patients with sepsis. We employed echocardiography to assess patients with sepsis within the initial 24 h of their admission to the ICU. RV-PA coupling was evaluated using the tricuspid annular plane systolic excursion (TAPSE) to pulmonary artery systolic pressure (PASP) ratio. A total of 92 subjects were enrolled, with 55 survivors and 37 non-survivors. TAPSE/PASP ratio assessed mortality with an area under the curve (AUC) of 0.766 (95% CI 0.670–0.862) and the optimal cutoff value was 0.495 mm/mmHg. We constructed a nomogram depicting the TAPSE/PASP in conjunction with IL-6 and Lac for the joint prediction of sepsis prognosis, and demonstrated the highest predictive capability (AUC = 0.878, 95% CI 0.809–0.948). In conclusion, the TAPSE/PASP ratio demonstrated prognostic value for ICU mortality in sepsis patients. The nomogram, which combines the TAPSE/PASP, IL-6, and LAC, demonstrated enhanced predictive efficacy for the prognosis of sepsis patients.
Similar content being viewed by others
Introduction
Sepsis is a common critical illness in intensive care unit (ICU). According to The Third International Consensus for Sepsis and Septic Shock, it is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection1. There are great differences in the number of deaths, age distribution and mortality rate of sepsis among different regions2,3. The incidence of sepsis in elderly individuals older than 65 years in Chinese intensive care units is as high as 57.5%, and the in-hospital mortality is as high as 30%4. Moreover, sepsis and septic shock represent significant and pressing global health challenges.
The definition of sepsis reflects its inherent heterogeneity. Heterogeneity is reflected in the different sources of infection in septic patients, the presence of complications and underlying diseases, and the early diagnosis and treatment5,6. Although it is difficult to accurately predict the prognosis of patients with sepsis, identifying important early indicators and adjusting treatment strategies are highly important for improving patient prognosis. Current studies have shown that many inflammation-based biomarkers, such as IL-6, IL-10, and HMGB1, can reflect the severity of sepsis and correlate well with clinical outcomes, but have proven to be lack generalizability to individual patients—in large part because these biomarkers have common characteristics of early inflammatory response but lack specificity7.
Ultrasound is playing an increasingly important role in the diagnosis and treatment of ICU patients8,9. Recent studies have shown that ultrasound indicators have certain value in evaluating the prognosis of patients with sepsis10,11. Patients with sepsis are prone to right ventricular dysfunction, which is more related to poor prognosis than left ventricular dysfunction12,13. Right ventricular-pulmonary artery (RV-PA) coupling is a measure of the functional match between right ventricular systolic function and afterload exerted by pulmonary vessels, and was assessed by the ratio of right ventricular end-systolic elasticity (Ees) to pulmonary artery elasticity (Es) measured by invasive pressure–volume loops14. However, this is difficult to achieve in routine clinical application. The ratio of tricuspid annular plane systolic excursion (TAPSE) to pulmonary artery systolic pressure (PASP) can be used to assess RV-PA coupling noninvasively and reliably15,16, and studies have shown that this parameter has important prognostic value for some diseases such as heart failure and severe pneumonia17,18,19. In our previous study, we found that patients with sepsis were prone to right heart dysfunction and pulmonary hypertension. Therefore, this study aimed to evaluate the cardiopulmonary interaction function of patients with sepsis in the intensive care unit by the TAPSE/PASP ratio, and to construct a nomogram by combining inflammatory indicators to predict the prognosis of septic patients.
Methods
Study population
This prospective observational study was conducted from September 2020 through September 2023 at a tertiary hospital ICU. All septic patients were screened for enrollment within 24 h after admission. Inclusion criteria are follows: (1) Patients with sepsis met the definition from the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3)3. Infection was confirmed through clinical and laboratory examinations. Additionally, a qSOFA score of ≥ 2 was required, which includes any two or more of the following three criteria: respiratory rate ≥ 22 breaths per minute; systolic blood pressure ≤ 100 mmHg; altered mental status (Glasgow Coma Scale score < 15). (2) age ≥ 18 years. Exclusion criteria included pregnancy, primary pulmonary arterial hypertension, liver cirrhosis, end-stage renal disease, abdominal hypertension and Patients who expired from causes other than septic shock, such as cardiovascular accidents or withdrawal of care by family members.
The study was approved by the ethics committee of our institution. Informed consent was obtained from family members. All methods employed in this study adhered to pertinent guidelines and regulations.
Echocardiograph
Bedside echocardiography was performed for each patient on the first day of ICU admission, we considered the impact of positive pressure ventilation on right atrial load and right ventricle-pulmonary artery coupling ratio. Therefore, all ultrasound data were collected before the initiation of mechanical ventilation. All parameters were measured by an experienced physician (X.Zhang). The echocardiographic parameters included the right ventricular area change rate (FAC), and tricuspid annular plane systolic pressure excursion (TAPSE) (Supplementary Fig. 1A). The pulmonary artery systolic pressure (PASP) was calculated by the Eq. 4* (tricuspid regurgitation velocity squared) + right atrial pressure (RAP) (Supplementary Fig. 1B). We employed variations in the inferior vena cava inner diameter (IVC-D) to estimate right atrial pressure (RAP), which was estimated as 3 mmHg when IVC-D was < 21mm and the IVC respiratory variability (∆IVC) was < 50%.; When the IVC-D was ≥ 21mm and ∆IVC was ≥ 50%, the estimated valve was 15mmHg; If either criterion is met, the RAP is estimated as 8mmHg. The left ventricular ejection fraction (LVEF) was assessed using the Simpson biplane method. Each metric underwent a trifold measurement with subsequent calculation of the corresponding averages. A subset of patients, without knowledge of prior examination results, underwent a repeat assessment of right ventricle to pulmonary artery (RV-PA) coupling measurements by a second sonographer (W.Wei) to evaluate interobserver consistency.
Other parameters collected
We systematically collected patient demographic information, encompassing variables such as heart rate (HR), blood pressure, respiratory rate. Simultaneously, Acute Physiology and Chronic Health Evaluation (APACHE) II and Sequential Organ Failure Assessment (SOFA) scores were calculated within the initial 24 h of hospital admission. Furthermore, we documented sepsis-related laboratory indicators, including red cell distribution width (RDW), blood lactate (LAC), interleukin-6 (IL-6), procalcitonin (PTC), and cardiac enzyme profiles.
Statistical analysis
The data were analyzed with R 4.1.2 software. The quantitative data were tested for the Shapiro‒Wilk normality test, and normally distributed data are presented as the mean ± standard deviation. Between-group comparisons were conducted with the independent samples t-test. Nonnormally distributed data were expressed as medians (P25, P75), and the rank-sum test was used for comparisons between groups. The chi-square test was used for categorical variables. Multiple logistic regression was employed for factor selection, to assess independent contributors. The predictive efficacy of each independent factor was evaluated using receiver operating characteristic (ROC) curves, and Kaplan–Meier survival curves were plotted for key indicators. We constructed a nomogram for the joint diagnosis of key indicators and assessed the model's stability using a calibration curve. Delong's test was uesed to compare the diagnostic capabilities of various indicators. P < 0.05 indicated statistical significance.
Ethics approval and consent to participate
This study was approved by the ethics committee of the Yijishan hospital, and we obtained informed consent from all patients or their family.
Results
Patient general characteristics
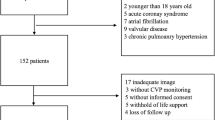
From September 2020 to September 2023, 99 patients with sepsis were enrolled based on the inclusion criteria. Seven patients were excluded due to poor image quality, resulting in a final sample size of 92 patients, among whom 53 survived and 37 died during ICU admission (Fig. 1).
The characteristics of the population parameters were compared between the survival group and non-survivor group using the Student's t-test, Fisher’s exact test and the chi-square test. The results revealed statistically significant differences in the Apache II score (p < 0.001) and SOFA score (p < 0.001), while other indicators such as age, sex, education, blood pressure, and heart rate, were not significantly different. The most common source of infection was pulmonary, followed by gastrointestinal (Table 1).
Echocardiographic and laboratory parameters
There were significant differences between the two groups in echocardiographic indices, including the TAPSE and TAPSE/PASP, as well as laboratory parameters such as LAC, and IL-6, with all p-values less than 0.001. Furthermore, FAC (p = 0.034), RVS (p = 0.023), PASP (p = 0.015), RDW (p = 0.004), and CK (p = 0.020) also exhibited statistically significant differences between the two groups (Table 2).
RV-PA coupling as a predictive factor
We plotted ROC curves for indicators with statistically significant differences, and the results demonstrated that the TAPSE/PASP had the highest AUC (0.952, CI 0.88–0.96) among the individual metrics (Fig. 2). The sensitivity, specificity, positive predictive value, and negative predictive value for the TAPSE/PASP were 0.83 (0.69–0.92), 0.64 (0.49–0.78), 0.71 (0.57–0.82), and 0.78 (0.62–0.90), respectively (Table 4). These results are consistent with previous studies, suggesting that the TAPSE/PASP is a reliable predictor of prognosis in patients with sepsis20. In addition, the Apache II score, SOFA score, as well as IL-6 and LAC also exhibited promising predictive performance, with AUCs of 0.729 (0.624–0.835), 0.721 (0.617, 0.825), 0.746 (0.641, 0.851), and 0.720 (0.612, 0.823), respectively. The optimal thresholds for Apache II scores, SOFA scores and TAPSE/PASP were 22.5. 7.5and 0.495, respectively (Table 3).
We included indicators that demonstrated significant differences between the two groups in a multivariate logistic regression model. The results revealed that IL-6 (OR 1.00, 95% CI 1.00–1.00, p = 0.035), LAC (OR 1.38, 95% CI 1.07–1.89, p = 0.023), and TAPSE/PASP (OR 0.92, 95% CI 0.88–0.96, p = 0.002) were found to be independent prognostic factors for sepsis patients (Table 4). The Kaplan–Meier curves for estimated survival showed that ICU mortality was significantly greater in septic patients with TAPSE/ PASP ≤ 0.495 mm/mmHg than in patients with TAPSE/PASP > 0.495 mm/mmHg (HR: 25.92, p < 0.001) (Fig. 3).
Nomogram construction and effectiveness evaluation
We constructed a predictive model based on TAPSE/PASP, IL-6, and LAC, and generated a nomogram (Fig. 4). The ROC curve for the model showed an AUC of 0.878 (95% CI 0.809–0.948) (Fig. 2, Table 4). The Delong test revealed that the predictive performance was superior to each individual variable (P < 0.05). The calibration curve of the nomogram demonstrated high accuracy, with mean squared error (MSE) and mean absolute error (MAE) of 0.00061 and 0.02, respectively (Supplementary Fig. 2), indicating the stability of the model.
Consistency test
In the present study, a cohort of 92 septic patients was analyzed, with a subset of 26 patients selected randomly for the purposes of repeatability and consistency analysis. Bland–Altman plots revealed the low mean biases (Supplementary Fig. 3). The results demonstrated good repeatability and consistency of the TAPSE/PASP measurements in patients with sepsis.
Discussion
Hemodynamic disturbances are commonly encountered in critically ill patients with sepsis21. They play a pivotal role in the pathophysiology of sepsis, contributing to the complex cascade of events that may lead to multiple organ dysfunction syndrome (MODS) and increased mortality. Therefore, timely recognition and targeted management are crucial in addressing the challenges posed by hemodynamic instability in severe sepsis patients. Bedside ultrasound is playing an increasingly important role in the diagnosis and monitoring of septic patients22.
This study focused on right ventricular-pulmonary artery coupling (RV-PA) measured by echocardiography, combined with biochemical markers, to assess the early status of septic patients for predicting their prognosis. According to the general data analysis, nearly half of the septic patients had infections originating from the lungs, and a significant number of patients experienced concurrent right heart dysfunction. Additionally, the results indicated an increase in pulmonary artery systolic pressure in the non-survivor group (p = 0.015). The match relationship between myocardial contractility and ventricular afterload determines stroke volume, as well as the end-systolic pressure of the ventricle and arteries23. This interplay is a crucial determinant of cardiopulmonary function. RV-PA coupling is considered to reflect the matching between the right ventricle systolic function, represented by TAPSE, and its afterload, represented by PASP24. In the study, the TAPSE/PASP were significantly different between the survivor and non-survivor groups (p < 0.001). According to the subsequent multivariate logistic regression analysis, the TAPSE/PASP served as an independent predictor of the prognosis of septic patients, with an AUC of approximately 0.766 (0.670, 0.862) and an optimal cutoff value of approximately 0.495. These findings are consistent with the results of previous studies20,25. The Kaplan–Meier survival estimates revealed that ICU mortality was significantly greater in patients with TAPSE/PASP ≤ 0.495 mm/mmHg (log-rank 25.92, p < 0.001). In this study, the cause of death among the patients was septic shock. Septic shock is characterized by severe circulatory, cellular, and metabolic abnormalities, leading to systemic hemodynamic changes. These changes include reduced systemic vascular resistance and increased cardiac output, potentially resulting in right ventricular overload and dysfunction. This condition may be reflected in the multiple organ failure and elevated pulmonary artery pressures observed in the deceased patients. Different causes of death can affect echocardiographic parameters differently. For instance, patients who die from other causes such as acute myocardial infarction or pulmonary embolism might exhibit different patterns of ventricular dysfunction on echocardiography. However, in our cohort, the consistency of septic shock as the cause of death provides a clearer interpretation of the TAPSE/PASP ratio. It underscores the specific impact of septic shock on RV-PA coupling. Our findings support RV-PA coupling as a valuable prognostic tool in septic patients, particularly those at risk of developing septic shock. The TAPSE/PASP ratio reflects the dynamic interaction between right ventricular function and pulmonary artery pressure, serving as a reliable predictor of outcomes in this critically ill population.
Currently, there is substantial variation in the ability of various biomarkers and ultrasound indicators to predict the prognosis of septic patients across different studies, and the overall efficacy of these biomarkers tends to be moderate26. Comprehensive prediction and personalized treatment27 of multiple indicators of sepsis patients will be the future development trend5. Therefore, this study constructed a nomogram of TAPSE/PASP combined with biochemical markers IL-6 and LAC to diagnose the prognosis of sepsis patients. The results revealed that the predictive AUC of the nomogram was 0.878 (95% CI 0.809–0.948), surpassing the predictive efficacy of individual indicators, including SOFA score and Apache II score (DeLong test, p < 0.05). RV-PA uncoupling leads to the disturbance of cardiopulmonary interactions, exacerbates right ventricular dysfunction, decreases cardiac output and oxygen content, and may cause tissue hypoperfusion of small capillaries28. On the other hand, inflammatory factors in sepsis, such as IL-6 and lactate, act on blood vessels, triggering the formation of thrombi and constriction of small blood vessels in sepsis. On the other hand, septic inflammatory factors such as IL-6 and lac can act on blood vessels, which may cause serious complications such as disseminated intravascular coagulation (DIC), affecting tissue perfusion, and even leading to multiple organ failure and death in severe cases29. Therefore, sepsis, as a systemic immune response, is more accurate predicting the prognosis of sepsis patients through comprehensive evaluation of multiple indicators30.
This study has several limitations. First, this was a single-center study with a limited sample size. Further validation through larger sample sizes and continuous monitoring is essential. Second, this study chose to assess the condition of septic patients on the first day of ICU admission, before the initiation of mechanical ventilation. It is important to note that mechanical ventilation can significantly impact the RV-PA. During mechanical ventilation, the increase in inspiratory transpulmonary pressure raises RV afterload. When alveolar pressure surpasses left atrial pressure, pulmonary artery pressure becomes the downstream pressure opposing RV ejection. A study demonstrates a linear relationship between tidal volume (Vt), driving pressure, transpulmonary pressure, and the RV end-systolic pressure–volume relationship31. With increasing tidal volume, RV afterload also increases. Moreover, the increase in right heart afterload may affect the estimation of right atrial pressure by influencing right heart filling and pulmonary artery pressure. in subsequent research, we will delve into exploring the effects of mechanical ventilation and various mechanical ventilation parameters on the hemodynamics of patients with sepsis. Third, the presence of minimal or no tricuspid regurgitation in some patients may lead to partial bias in the measurement of PASP.
Conclusions
The TAPSE/PASP exhibits substantial predictive value for the prognosis of patients with sepsis. Moreover, the nomogram constructed with TAPSE/PASP, IL-6, and LAC demonstrated enhanced predictive efficacy. These findings provide insights for enhancing the individualized prognostic assessment of patients with sepsis.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ICU:
-
Intensive care unit
- LVEF:
-
Left Ventricular Ejection Fraction
- FAC:
-
Fractional Area Change
- TAPSE:
-
Tricuspid Annular Plane Systolic Excursion
- PASP:
-
Pulmonary Artery Systolic Pressure
- RV-PA:
-
Right Ventricular Pulmonary Artery Coupling
- RDW:
-
Red Cell Distribution Width
- LAC:
-
Lactic Acid
- IL-6:
-
Interleukin-6
References
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810. https://doi.org/10.1001/jama.2016.0287 (2016).
Rudd, K. E. et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 395, 200–211. https://doi.org/10.1016/s0140-6736(19)32989-7 (2020).
Fleischmann-Struzek, C. et al. Incidence and mortality of hospital- and ICU-treated sepsis: Results from an updated and expanded systematic review and meta-analysis. Intensive Care Med. 46, 1552–1562. https://doi.org/10.1007/s00134-020-06151-x (2020).
Weng, L. et al. National incidence and mortality of hospitalized sepsis in China. Crit. Care 27, 84. https://doi.org/10.1186/s13054-023-04385-x (2023).
Yang, Y. et al. Development and validation of a nomogram for predicting the prognosis in cancer patients with sepsis. Cancer Med. 11, 2345–2355. https://doi.org/10.1002/cam4.4618 (2022).
Stanski, N. L. & Wong, H. R. Prognostic and predictive enrichment in sepsis. Nat. Rev. Nephrol. 16, 20–31. https://doi.org/10.1038/s41581-019-0199-3 (2020).
Hotchkiss, R. S. et al. Sepsis and septic shock. Nat. Rev. Dis. Primers 2, 16045. https://doi.org/10.1038/nrdp.2016.45 (2016).
Ma, Q. et al. Respiratory variability of Valvular peak systolic velocity as a new indicator of fluid responsiveness in patients with septic shock. Shock 60, 11–17. https://doi.org/10.1097/shk.0000000000002142 (2023).
Yu, J., Zheng, R., Yang, P. & Wang, D. Construction of a predictive model and prognosis of left ventricular systolic dysfunction in patients with sepsis based on the diagnosis using left ventricular global longitudinal strain. J. Intensive Care 10, 29. https://doi.org/10.1186/s40560-022-00621-8 (2022).
Zhao, J. L., Wang, R., Dai, Q. C. & Dong, S. M. The value of right ventricular ultrasound assessment and cardiac biomarkers in the prognosis of sepsis. Eur. Rev. Med. Pharmacol. Sci. 27, 7891–7897. https://doi.org/10.26355/eurrev_202309_33547 (2023).
Lu, N. F. et al. Early diastolic peak velocity of mitral valve annulus and right ventricular systolic tricuspid annular velocity as predictors in assessing prognosis of patients with sepsis. Risk Manag. Healthc. Policy 16, 921–930. https://doi.org/10.2147/rmhp.S407929 (2023).
Lanspa, M. J. et al. Right ventricular dysfunction in early sepsis and septic shock. Chest 159, 1055–1063. https://doi.org/10.1016/j.chest.2020.09.274 (2021).
Kim, J. S., Kim, Y. J., Kim, M., Ryoo, S. M. & Kim, W. Y. Association between right ventricle dysfunction and poor outcome in patients with septic shock. Heart 106, 1665–1671. https://doi.org/10.1136/heartjnl-2020-316889 (2020).
He, Q. et al. Clinical usefulness of right ventricle-pulmonary artery coupling in cardiovascular disease. J. Clin. Med. https://doi.org/10.3390/jcm12072526 (2023).
D’Alto, M. et al. Right ventricular-arterial uncoupling independently predicts survival in COVID-19 ARDS. Crit. Care 24, 670. https://doi.org/10.1186/s13054-020-03385-5 (2020).
Bowcock, E. M., Gerhardy, B., Huang, S. & Orde, S. Right ventricular outflow tract Doppler flow analysis and pulmonary arterial coupling by transthoracic echocardiography in sepsis: A retrospective exploratory study. Crit. Care 26, 303. https://doi.org/10.1186/s13054-022-04160-4 (2022).
Bursi, F. et al. Impact of right ventricular-pulmonary circulation coupling on mortality in SARS-CoV-2 infection. J. Am. Heart Assoc. 11, e023220. https://doi.org/10.1161/jaha.121.023220 (2022).
Singh, I. et al. Sex-related differences in dynamic right ventricular-pulmonary vascular coupling in heart failure with preserved ejection fraction. Chest 159, 2402–2416. https://doi.org/10.1016/j.chest.2020.12.028 (2021).
Bok, Y., Kim, J. Y. & Park, J. H. Prognostic role of right ventricular-pulmonary artery coupling assessed by TAPSE/PASP ratio in patients with acute heart failure. J. Cardiovasc. Imaging 31, 200–206. https://doi.org/10.4250/jcvi.2023.0055 (2023).
Zhang, H. et al. Prognostic implications of tricuspid annular plane systolic excursion/pulmonary arterial systolic pressure ratio in septic shock patients. Cardiovasc. Ultrasound 18, 20. https://doi.org/10.1186/s12947-020-00198-y (2020).
Virág, M., Leiner, T., Rottler, M., Ocskay, K. & Molnar, Z. Individualized hemodynamic management in sepsis. J. Pers. Med. https://doi.org/10.3390/jpm11020157 (2021).
Sweeney, D. A. & Wiley, B. M. Integrated multiorgan bedside ultrasound for the diagnosis and management of sepsis and septic shock. Semin. Respir. Crit. Care Med. 42, 641–649. https://doi.org/10.1055/s-0041-1733896 (2021).
Li, S., Wan, X., Laudanski, K., He, P. & Yang, L. Left-sided ventricular-arterial coupling and volume responsiveness in septic shock patients. Shock 52, 577–582. https://doi.org/10.1097/shk.0000000000001327 (2019).
Guazzi, M. et al. Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: An index of right ventricular contractile function and prognosis. Am. J. Physiol. Heart Circ. Physiol. 305, H1373-1381. https://doi.org/10.1152/ajpheart.00157.2013 (2013).
Zhang, H. et al. Prognostic implication of a novel right ventricular injury score in septic patients. ESC Heart Fail. 10, 1205–1213. https://doi.org/10.1002/ehf2.14289 (2023).
Tan, M., Lu, Y., Jiang, H. & Zhang, L. The diagnostic accuracy of procalcitonin and C-reactive protein for sepsis: A systematic review and meta-analysis. J. Cell Biochem. 120, 5852–5859. https://doi.org/10.1002/jcb.27870 (2019).
De Backer, D. et al. A plea for personalization of the hemodynamic management of septic shock. Crit. Care 26, 372. https://doi.org/10.1186/s13054-022-04255-y (2022).
Topyła-Putowska, W., Tomaszewski, M., Wojtkowska, A. & Wysokiński, A. Novel echocardiographic measurements of right ventricular-pulmonary artery coupling in predicting the prognosis of precapillary pulmonary hypertension. J. Pers. Med. https://doi.org/10.3390/jpm13121627 (2023).
Iba, T., Levi, M. & Levy, J. H. Sepsis-induced coagulopathy and disseminated intravascular coagulation. Semin. Thromb. Hemost. 46, 89–95. https://doi.org/10.1055/s-0039-1694995 (2020).
He, Y. et al. Clinical characteristics and risk factors associated with ICU-acquired infections in sepsis: A retrospective cohort study. Front Cell Infect. Microbiol. 12, 962470. https://doi.org/10.3389/fcimb.2022.962470 (2022).
Slobod, D. et al. Right ventricular loading by lung inflation during controlled mechanical ventilation. Am. J. Respir. Crit. Care Med. 205(11), 1311–1319. https://doi.org/10.1164/rccm.202111-2483OC (2022).
Funding
National Natural Science Foundation of China (NSFC): 81801970. Natural Science Research Project of the Higher Education in Anhui Province: KJ2020A0616. Wannan Medical College Natural Research Project WK202215.
Author information
Authors and Affiliations
Contributions
M.Q. and D.C.Y. participated in drafting, W.W. and M.Q. participated in data collecting and analysing. S.C.C., L.B.Z., C.C. and Z.I.H. participated in conceptualising and data collecting. M.Q. and L.B.H. read and revised the manuscript. Z.X. and W.J.Y. supervised and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ma, Q., Ding, C., Wei, W. et al. The value of right ventricular pulmonary artery coupling in determining the prognosis of patients with sepsis. Sci Rep 14, 15283 (2024). https://doi.org/10.1038/s41598-024-65738-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65738-2
- Springer Nature Limited