Abstract
Demyelination is generated in several nervous system illnesses. Developing strategies for effective clinical treatments requires the discovery of promyelinating drugs. Increased GABAergic signaling through γ-aminobutyric acid type A receptor (GABAAR) activation in oligodendrocytes has been proposed as a promyelinating condition. GABAAR expressed in oligodendroglia is strongly potentiated by n-butyl-β-carboline-3-carboxylate (β-CCB) compared to that in neurons. Here, mice were subjected to 0.3% cuprizone (CPZ) added in the food to induce central nervous system demyelination, a well-known model for multiple sclerosis. Then β-CCB (1 mg/Kg) was systemically administered to analyze the remyelination status in white and gray matter areas. Myelin content was evaluated using Black-Gold II (BGII) staining, immunofluorescence (IF), and magnetic resonance imaging (MRI). Evidence indicates that β-CCB treatment of CPZ-demyelinated animals promoted remyelination in several white matter structures, such as the fimbria, corpus callosum, internal capsule, and cerebellar peduncles. Moreover, using IF, it was observed that CPZ intake induced an increase in NG2+ and a decrease in CC1+ cell populations, alterations that were importantly retrieved by β-CCB treatment. Thus, the promyelinating character of β-CCB was confirmed in a generalized demyelination model, strengthening the idea that it has clinical potential as a therapeutic drug.
Similar content being viewed by others
Introduction
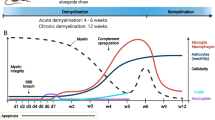
Demyelinating diseases represent an important percentage of disabling disorders in the nervous system (NS). Finding potent and specific promyelinating drugs is necessary to develop strategies that could allow for effective clinical treatments. Recent research has proposed that γ-aminobutyric acid (GABA) signaling is involved in myelination control1,2,3,4 and that GABARs, both GABAR type A (receptor-channel, GABAAR) and GABAR type B (coupled to G proteins, GABABR), expressed in oligodendroglial cell membranes participate in phenomena that promote myelination1,2,5,6. However, the development of specific drugs that act on oligodendrocyte receptors is still far from complete, this lack of knowledge affects not only the study of GABAergic signaling’s physiological role during oligodendroglial differentiation but also the development of drugs with clinical potential. The stimulation of GABAergic signaling during myelination should be done with specific drugs that act on the GABARs expressed in the oligodendroglial lineage. Current evidence indicates that GABAAR is involved in promoting or regulating myelination in different models6,7. The main GABAAR expressed in oligodendrocytes (OLs) has characteristics that distinguish it from receptors that are mostly expressed in neurons and astrocytes3,8. Thus, the GABAAR expressed in the membrane of oligodendrocyte precursor cells (OPCs) and mature OLs presents a combination that includes the α3 and γ1 subunits. The most likely composition corresponds to a α3β2γ1 receptor8. This receptor is potentiated by several β-carbolines, including n-butyl-β-carboline-3-carboxylate (β-CCB), which has a potent positive effect3. The binding site of various β-carbolines (including β-CCB) was originally described as that for benzodiazepines. However, other reports have proposed different binding sites such as that for loreclezole9. Our recent studies have shown that, in the case of oligodendroglial cells, β-CCB acts mainly as a positive modulator through a different binding site than that for benzodiazepines, either the classical binding site or the so-called low-affinity binding site8. Moreover, we have also shown that the action of β-CCB (and other β-carbolines) on the receptor expressed in cortical neurons in vitro is differential concerning the oligodendroglial receptor5,8. Thus, we hypothesized that β-CCB enhances oligodendroglial GABAergic communication in in vivo models5 and promotes the myelination process. β-CCB, was originally described as an inverse agonist of neuronal GABAAR, is a probable endogenous modulator of GABAAR expressed in the central NS (CNS)10. Systemically, β-CCB does not produce behavioral alterations, unlike other β-carbolines (e.g., DMCM, β-CCM) which act as convulsant agents and anxiogenics10,11. Indeed, β-CCB has no convulsant effect per se, even when it is administered to mice at doses of up to 100 mg/Kg11. In vitro experiments showed that β-CCB did not exhibit either potentiation or a robust effect as an inverse agonist on the GABAA response of cortical neurons kept in culture8, supporting that observed in the whole animal.
We have previously shown that β-CCB treatment promotes remyelination in a focal demyelination model5,12. Here, we investigated whether the effect of β-CCB extends to other regions in the CNS. For this, we conducted a longitudinal study with MRI and a cross-sectional analysis with BGII specific histology and IF using the NG2+ and CC1+ oligodendroglial markers. Thus, we administered β-CCB to animals that were previously subjected to 0.3% CPZ in the food to induce myelin loss in the CNS, a well-known model for multiple sclerosis (MS)13,14,15, and tested whether β-CCB administration affected the rate and degree of remyelination. The results suggested that the myelin increase induced by β-CCB during the recovery period was not homogeneous across the different areas studied. Overall, β-CCB had a robust promyelinating effect in brain white matter (corpus callosum, fimbria, internal capsule, and cerebellar peduncles). This remyelination can be well monitored in some regions using MRI. In the cerebral cortex (mctx), β-CCB did not have a clear effect, whereas in some areas of the hippocampus it exhibited a mild effect. Thus, the promyelinating character of β-CCB was confirmed in a model of generalized demyelination, supporting the idea that β-carbolines have the potential to be used as therapeutic drugs against demyelinating diseases, as it has been shown elsewhere12, this promyelinating action could be explained by its potentiating effect on the oligodendroglial GABAAR.
Results
Cuprizone intake promotes alterations in white matter assessed by BGII staining and T2-weighted images
Several studies have shown that microstructural alterations in CPZ-demyelinated mice can be evaluated through T2-weighted images (T2-wi) in vivo, as the images show hyperintense areas that correlate with less myelin content16,17. Thus, this is a way to confirm the effect of CPZ intake and an obvious advantage when performing longitudinal studies17,18. Here, we first used T2-wi to detect hyperintensity in different white matter areas. We found that 0.3% CPZ intake for three weeks caused significant changes in the T2-wi signal intensity in all animals that ingested CPZ (n = 38), an effect that lasted for several weeks after mice were switched back to a normal diet. Microstructural changes were evaluated in CPZ-demyelinated animals subjected to CPZ for 3 weeks plus 3 subsequent weeks fed with normal diet (3 + 3w protocol) and comparing them versus the control (CTRL) group. T2-wi signal intensity was evaluated and compared in the anterior corpus callosum (acc, P = 0.0001), medial corpus callosum (mcc, P < 0.0001), and cerebellar white matter (cerebellum, P = 0.0007), which are commonly used to evaluate myelin content in several protocols14,19,20,21. As opposed to CTRL group, CPZ-demyelinated animals exhibited T2-wi signal hyperintensity in the three areas (Fig. 1a,b). This hyperintensity remained up to six weeks after initiating the intake. During this time frame, we also observed a ≈2% mortality rate in the CPZ intake group.
CPZ intake (0.3%) induces hyperintensity of the T2-wi signal in white matter that correlated with a decrease in BGII staining. (a) The top diagram illustrates the 3 + 3w protocol course, below, are shown tree representative T2-wi coronal images acquired before CPZ intake (0w in the diagram), after 3w of CPZ intake (CPZ (3w)), and after 3 subsequent weeks with normal diet reestablished (CPZ (3 + 3w)). Images illustrate the following areas of interest (yellow arrows): anterior corpus callosum (acc), medial corpus callosum (mcc), and cerebellar white matter (cerebellum). (b) Quantitative representation of longitudinal changes in normalized T2-wi signal intensity (ROI/CFS) estimated for each area analyzed. Gray asterisks correspond to longitudinal comparison within the CPZ group. ANOVA, n = 4 for control (CTRL) and n = 4–7 CPZ groups, respectively. (c) Brain coronal sections stained with BGII under the conditions shown in (a). Like in (a), the cerebral anterior (acc, + 0.62 mm from bregma) and medial (mcc, − 1.70 mm from bregma) sections are illustrated. The third column depict a cerebellar section (cerebellum, − 6.24 mm from bregma). (d) Relative intensity of staining (RIS) by BGII of acc, mcc, and cerebellum for control (3w; n = 4–5) and CPZ (3w; n = 4–7), and for control (6w; n = 4–7) and CPZ (6w; n = 4–7) samples. ANOVA, *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
To verify if changes in T2-wi correlated with demyelinating damage, tissues from both the CPZ group and the CTRL group were divided and processed for BGII staining at two time points, first at the end of CPZ intake (3 weeks) and second at the end of the 3 + 3w protocol (Fig. 1c). Then, we evaluated the relative intensity of staining (RIS)5,22 and found that the 3w CPZ group presented a clear decrease in RIS for the mcc (P = 0.0057) and cerebellum (P = 0.0014), compared to the respective CTRL group (Fig. 1d). Also, at the end of the 3 + 3w protocol all three areas presented a significant decrease in RIS in the CPZ group, acc (P = 0.0047), mcc (P = 0.0195), and cerebellum (P = 0.0005) (Fig. 1d). Taken together, evidence suggested that in several regions CPZ intake caused T2-wi signal hyperintensity and a decrease in RIS observed through BGII staining, and that this consistently occurred as soon as 3 weeks after CPZ intake. Both effects were consistent with demyelination. All the animals that were included in subsequent experiments were tested during CPZ administration protocol to confirm the T2-wi hyperintensity changes in the described areas.
CPZ intake induced alterations in diffusion tensor imaging metrics in cerebral and cerebellar white matter
To complement the longitudinal protocol, we conducted an MRI analysis using diffusion tensor imaging (DTI). DTI analysis has been widely used to describe white matter alterations. Here we used DTI to further detail the changes caused by CPZ intake. Fractional anisotropy (FA) index and radial diffusivity (λ⊥) ratio are two metrics calculated from this DTI analysis. Both metrics have been successfully used in experimental models to detect myelin abnormalities5,23. The apparent diffusion coefficient (ADC) was also calculated for each region. ADC is a parameter with an inverse pattern to that of the FA index. This provides robustness to the significance of the observed change24. Finally, the axial diffusivity (λ||) ratio was evaluated to obtain information about axonal integrity25.
In this study, DTI metrics were evaluated for the corpus callosum (acc and mcc), fimbria, and the internal capsule (ic) in the cerebral white matter (Fig. 2). The superior (scp), middle (mcp), and inferior (icp) cerebellar peduncles were also evaluated (Fig. 3). Significant changes in DTI metrics were observed as early as 3 weeks after the start of CPZ ingestion, compared with the CTRL group. The FA index decreased in the mcc (P = 0.0028), fimbria (P = 0.0025), and icp (P = 0.0148) and these changes remained for up to three weeks after mice returned to a normal diet (3 + 3w protocol; mcc, P < 0.0001; icp, P = 0.0088). At 3 + 3w, we also detected significant differences in the acc (P = 0.0009) and ic (P = 0.0017) compared against the CTRL group. Regarding the ADC, after 3 weeks of CPZ intake, we observed a significant increase in the 3 cerebellar peduncles versus the CTRL group (scp, P = 0.0034; mcp, P = 0.0111; icp, P < 0.0001). These increases had a partial recovery at 3 + 3w for scp and mcp. Moreover, there was a significant increase in the ADC for the acc (P = 0.0012), mcc (P = 0.0017), fimbria (P = 0.0093) and ic (P = 0.0003) structures at 3 + 3w, compared to control animals, or even when values from the same CPZ group were compared versus the parameter before starting CPZ intake. Finally, λ⊥ ratio analysis showed a significant increase in the fimbria (P = 0.0018), ic (P = 0.0021), and the three cerebellar peduncles (scp, P = 0.0008; mcp, P = 0.0003; icp, P = 0.0015) after three weeks of CPZ intake, compared to the control group. At 3 + 3w, a significant increase was maintained in the acc (P < 0.0001), mcc (P < 0.0001), fimbria (P = 0.0014), ic (P < 0.0001), and icp (P = 0.0182). Although there is a mild recovery for mcp and scp at 3 + 3w.
Diffusion tensor imaging (DTI) metrics for different brain structures of CPZ-demyelinated animals. (a) Principal diffusion vector (PDV) and fractional anisotropy (FA) maps during CPZ intake in anterior and medial brain coronal sections. FA maps were made before CPZ intake (Pre-CPZ; 0w), after 3 weeks of CPZ intake [CPZ (3w)], and after the subsequent three weeks with normal diet reestablished [CPZ (3 + 3w)]. Five areas of interest are indicated: corpus callosum (both acc and mcc), fimbria, internal capsule (ic), and medial cortex (mctx). (b) DTI metrics: FA, apparent diffusion coefficient (ADC), radial diffusivity (λ⊥), and axial diffusivity (λ||) ratio for the five areas depicted in (a) and were plotted Pre-CPZ (0w), CPZ (3w), and CPZ (3 + 3w) stages. Data represent the mean ± S.D. n = 4–16 for control group and n = 4–29 for CPZ-demyelinated group. Dark red asterisks correspond to a longitudinal comparison within the CPZ group, while black asterisks signal comparisons between groups. ANOVA. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
DTI metrics of cerebellar peduncles in CPZ-demyelinated animals. Graphics show the FA, ADC, λ⊥, and λ|| metrics for the superior (scp), medial (mcp), and inferior (icp) cerebellar peduncle of control animals (n = 4–16) and the CPZ-demyelinated group (n = 14–29) for the different CPZ stages: Pre-CPZ (0w), CPZ (3w), and CPZ (3 + 3w) as indicated. Data represent the mean ± S.D. Dark red asterisks correspond to a longitudinal comparison within the CPZ group, while black asterisks signal comparisons between groups (CPZ vs. control) using ANOVA. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001.
Taken together, the results indicated that CPZ intake induced alterations in MRI metrics, suggesting demyelination. These alterations appeared after the third week of continuous CPZ protocol. The data also support that demyelination continued even after drug administration was withdrawn (i.e., at 3 + 3w), a result that was consistent with previous reports26,27,28,29. A different result was obtained from the mctx, as DTI metrics did not present variations during CPZ intake (Fig. 2, lower panel). All analyses indicated, as expected, that both cerebral and cerebellar white matter structures were affected by CPZ intake (Figs. 2 and 3). Changes observed by DTI analysis were consistent with demyelination.
β-CCB administration ameliorates the demyelination effect induced by CPZ intake
Previous studies have shown that β-CCB potentiates the response of GABAARs expressed in OPCs and OLs in culture, and that it has a promyelinating effect in a model of focal demyelination of the rat icp3,5,8,12. Identification of white matter structures that seem to undergo CPZ-induced demyelination, as assessed by MRI metrics and histology, allowed us to evaluate a generalized promyelinating effect of β-CCB. First, a histological analysis was realized for the areas illustrated in Fig. 4: mcc, fimbria, ic, scp, mcp, and icp. These areas were analyzed for the CTRL group, the CPZ group, and the CPZ group that was treated with β-CCB (CPZ + β-CCB). For the latter, β-CCB (1 mg/Kg) was administered by intraperitoneal injection from week 6 to week 9 in the 3 + 6w protocol, as indicated in the methods section, while the CPZ group that was not treated with β-CCB was injected with vehicle alone under the same administration protocol (see diagram in Fig. 4a). At the end of β-CCB treatment, samples from all three experimental groups were processed for BGII, and RIS was evaluated (Fig. 4a,b). Quantification showed that, for the CPZ group, RIS was significantly low compared to the CTRL group in all structures analyzed (mcc, P = 0.0466; fimbria, P = 0.0499; ic, P = 0.0487; scp, P = 0.0003; mcp, P = 0.0083; icp, P = 0.0028). However, we found that in the CPZ + β-CCB treated group, the RIS values were significantly higher than those estimated in the CPZ group (mcc, P = 0.0461; fimbria, P = 0.0410; ic, P = 0.04871; scp, P < 0.0001; mcp, P < 0.0001; icp, P < 0.0001). Moreover, RIS values of the CPZ + β-CCB treated group did not show statistical differences compared with those of the CTRL group, except for scp (P = 0.0386) and mcp (P = 0.0272). Thus, the histological evidence suggested that systemic administration of β-CCB had a promyelinating effect on the white matter that had been previously demyelinated by CPZ intake. Interestingly, no differences were observed in another white matter structure analyzed, the lateral cingulum (lc), that did not show differences when comparing the CTRL group, CPZ group, and the CPZ + β-CCB group (see Fig. 5b).
Histological BGII analysis of the β-CCB effect on brain and cerebellar white matter structures during CPZ intake. (a) The top diagram illustrates the 3 + 6w protocol course, below, images illustrate coronal slices in corpus callosum (mcc, white arrows), as well as in fimbria (white arrows), internal capsule (ic, black arrows), the superior (scp, white arrows), middle (mcp, white arrows), and inferior (icp, white arrows) cerebellar peduncle regions stained with BGII at the end of the 3 + 6w protocol course for a CTRL group that was fed with normal diet for 9 weeks (n = 4), CPZ group (injected with vehicle from week 6 to 9; n = 4), and the CPZ + β-CCB group that received β-CCB from week 6 to 9 (n = 4–7). (b) Box graphs represent the RIS evaluated for each condition as described in (a). Note that β-CCB in the CPZ + β-CCB group promoted an increase in RIS in all structures analyzed. ANOVA, *P < 0.05, **P < 0.01, ***P < 0.001. Each bar represents mean ± S.D.
Histological BGII analysis of the β-CCB effect on brain gray matter and lateral cingulum in CPZ-demyelinated animals. (a) Images illustrate areas of the medial cerebral cortex (mctx, white box in top row), hippocampal CA3 (CA3, black box in top row, amplified and signaled by black arrows in the central row), and lateral cingulum (lc, yellow area in bottom row); all images are in a coronal view. Samples were stained with BGII at the end of the 3 + 6w protocol following the diagram in Fig. 4a. Thus, CTRL group (n = 4–5) was fed with normal diet for 9 weeks, CPZ group (n = 5–6) was injected with vehicle from week 6 to 9, and CPZ + β-CCB group received 1 mg/Kg β-CCB (n = 5–6). (b) Box graphs represent the RIS evaluated for each condition. Note that β-CCB in the CPZ + β-CCB group promoted an increase in RIS only in the CA3 area. ANOVA, ****P < 0.0001. Each bar represents mean ± S.D.
CPZ intake also generated significant demyelination in gray matter structures such as the neocortex and hippocampus30. Thus, we were interested in exploring these gray matter structures of significance for cognitive functions (Fig. 5) and relevant for pathologies such as MS. For this, experimental groups were treated as described above and then histologically analyzed by evaluating the RIS. The quantitative analysis (Fig. 5b) revealed that at the end of CPZ intake there was a profound reduction of RIS, suggesting that myelin content decreased in both mctx (P < 0.0001) and hippocampus (P < 0.0001). β-CCB administration did not appear to have a promyelinating effect on the mctx, as the RIS values did not improve in the CPZ + β-CCB group (P < 0.0001). Also, the effect of β-CCB on the hippocampus in general did not appear to be significant. However, by performing an analysis of distinct hippocampal substructures, we noted that β-CCB lead to an increase in RIS in the CA3 area (CA3, P < 0.0001), however, RIS did not recover control levels, suggesting a limited promyelinating effect (Fig. 5b).
DTI analysis of CPZ-demyelinated animals treated with β-CCB
The histological results suggested that β-CCB treatment promoted the recovery of CPZ-demyelinated animals, particularly in white matter regions. Thus, finding highly reliable areas of the nervous system concerning myelin content changes, reported by MRI, will be useful for developing a method to monitor these changes longitudinally. This would facilitate pharmacological testing with potential substances that enhance remyelination. It is well known that interpreting microstructural changes is limited under current technical imaging conditions. However, longitudinally tracking the process will stimulate the search for reliable protocols. The histological data confirm the promyelinating effect of β-CCB administration; therefore, the following MRI analysis was performed to determine the areas where DTI metrics can confirm this effect.
The bar graphs in Fig. 6 show the parameter values obtained by DTI analysis for all areas analyzed: mcc, fimbria, ic, and the three cerebellar peduncles (scp, mcp, and icp). DTI metrics were evaluated at the end of treatment with β-CCB and compared versus the CPZ group injected with vehicle. It was found that all fimbria values (FA, P = 0.0009; ADC, P = 0.0068; λ⊥, P = 0.0186) were consistent with the histological findings, while those for mcc (FA, P = 0.0442; λ⊥, P = 0.0471) and ic (FA, P = 0.0477; ADC, P = 0.0086) correlated partially (Fig. 6). Specifically, it was identified a significant increase in the FA index in animals treated with β-CCB or decreases in ADC and λ⊥ ratio values, all of which indicate a possible increase in myelin content. Finally, the λ|| ratio did not exhibit significant changes. Metrics analyzed for the cerebellar peduncles did not correlate with the histological findings. Thus, β-CCB showed a potential generalized promyelinating effect in the brain of CPZ-demyelinated adult animals as analyzed by BGII histology, however, these findings are only partially correlated with DTI metrics.
DTI metric analysis of the β-CCB effect on white matter structures in CPZ-demyelinated animals. Effect of β-CCB treatment on white matter metrics evaluated by MRI; bar graphs indicate mean ± S.D. (dotted lines represent the mean for the control group) for FA, ADC, λ⊥, and λ|| metrics obtained at the final stage of β-CCB administration for the mcc, fimbria, and ic regions and the three cerebellar peduncles (scp, mcp, and icp), and comparing the metrics computed for the CPZ group vs. the CPZ + β-CCB group. Every point in graphics is the value for a given brain analyzed (n = 3–4 for each group). Student's t-test. *P < 0.05, **P < 0.01, ***P < 0.001.
On the other hand, DTI metric analysis indicated that myelin did not increase in the mctx (Fig. 7) in animals treated with β-CCB. This result supports the histological findings. It is important to mention, however, that DTI analysis for mctx did not show changes elicited by CPZ intake at 3 + 3w (see Fig. 2a). This result differs from that of the histological analysis (Fig. 5). In the case of CA3 in the hippocampus, DTI metrics for the group treated with β-CCB did not show changes compared to the respective control. Thus, DTI parameters were inconsistent with the histological observations, particularly for regions of gray matter analyzed here.
DTI metric analysis of the β-CCB effect on cerebral gray matter structures in CPZ-demyelinated animals. Effect of β-CCB treatment on cerebral gray matter metrics evaluated by MRI; bar graphs indicate mean ± S.D. (dotted lines represent the mean for the control group) for FA, ADC, λ⊥, and λ|| metrics obtained at the final stage of β-CCB treatment for the mctx and CA3 regions, comparing the metrics computed for the CPZ group vs. the CPZ + β-CCB group. Every point in graphics is the value for a given brain analyzed (n = 3–4 for each group). Student's t-test.
Analysis of oligodendroglial lineage cells after β-CCB administration in the CPZ model
As mentioned above, β-CCB acts on GABAAR expressed in OLs and OPCs maintained in vitro, acting as a positive allosteric modulator3. It is also known that OPCs are the main source of remyelination, and GABAergic signaling could be involved in OPCs proliferation and maturation6. In this context, the promyelinating effect of β-CCB administrated in vivo may occur through GABA response potentiation in the oligodendroglial lineage (see also ref.12). Therefore, to identify a possible direct effect of β-CCB, we performed an immunolabeling analysis of OPC and mature OL populations using the NG2 and CC1 markers, respectively1,31,32 (Fig. 8a). For this, samples were processed at the end of β-CCB treatment to quantify either NG2+ signal and CC1+ cells for different cerebral white matter structures (mcc, fimbria, and ic) and one gray matter structure (mctx) in three experimental conditions: CTRL, CPZ group and CPZ + β-CCB (Fig. 8b). The results showed that the fimbria, ic, and mcc in the CPZ group presented a significant increase in the NG2+ signal (fimbria, P = 0.0033; ic, P = 0.0003; mcc, P < 0.0001) and a decrease in the number of CC1+ cells (fimbria, P = 0.0002; ic, P < 0.0001; mcc, P < 0.0001) compared to CTRL group. However, the CPZ + β-CCB group showed an important reversal of the latter pattern for both NG2+ signal area (fimbria, P = 0.0130; ic, P = 0.0011; mcc, P = 0.0093) and in the number of CC1+ cells (fimbria, P = 0.0007; ic, P < 0.0001; mcc, P = 0.0005), although the recovery observed did not reach control levels for the mcc (NG2+, P < 0.0001; CC1+, P = 0.0189). Finally, for mctx, CPZ intake did not produce significant changes in the NG2+ signal but induced a robust decrease in the number of CC1+ cells (P < 0.0001), a change that β-CCB was not able to revert (P < 0.0001).
Effect of β-CCB on the oligodendroglial lineage population after CPZ ingestion. (a) Illustrative images of coronal sections of the corpus callosum (mcc) with CC1/NG2/DAPI labeling, showing panoramic micrographs (left) as magnifications (right) of the dotted boxes shown in the panoramic images. Samples were acquired for the CTRL group (n = 4–7), the CPZ group (n = 3), and the CPZ + β-CCB group (n = 4) as explained in Fig. 4. (b) Box graphs represent the area of NG2 (white arrows) signal and CC1+ (gray arrows) cells quantified for each condition as indicated and corresponding to the groups described in (a). ANOVA, *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. Each bar represents the mean ± S.D.
Together, these results suggest that CPZ administration generated an increase in NG2+ cells in white matter structures but not in gray matter structures. It also caused a decrease in CC1+ cells in both white and gray matter structures. Finally, β-CCB treatment induced a reduction of the NG2+ cell population and a parallel increase in CC1+ cells in white matter. However, β-CCB did not show any significant effect on the oligodendroglial population analyzed in the mctx.
Discussion
Here we showed that β-CCB acts as a promyelinating factor in different areas of the brain that were previously demyelinated by the CPZ intake protocol. It was shown that the promyelinating effect of β-CCB can be transversely tracked with specific histology by BGII or IF. Furthermore, changes in the demyelination-remyelination process can be followed through longitudinal analysis with MRI.
This information could help to develop experimental protocols for longitudinal monitoring of the myelinating process and to study the mechanisms activated by molecules that promote the process. Eventually, this will boost the development of novel therapeutic strategies for the treatment of demyelinating illnesses.
There are multiple demyelinating pathologies, each one with its unique characteristics and causal agents. An example of these pathologies is MS that is a demyelinating pathology of the CNS that affects both white matter and gray matter33,34. The CPZ intake model is a widely used experimental approach that produces characteristics resembling those of MS, and it allows researchers to evaluate the processes of demyelination and remyelination13,14,35. In this work, we used the CPZ model to induce changes in myelin content under a three-week administration protocol26,27,28,29,30,36,37,38,39,40,41,42,43.
We determined that 0.3% CPZ for three weeks caused substantial changes in myelin content indicators. To reach this conclusion, we assessed the myelin changes with different techniques, the first of which was T2-wi. This MRI technique has been used to study the evolution of MS through changes in lesion volumes44. Hyperintensity changes revealed by T2-wi provided a profile of possible areas suffering from demyelination. Thus, all animals included in the CPZ group were validated using T2-wi analysis. However, changes in hyperintensity can also be caused by inflammation and edema45,46, so a more detailed analysis is required to determine the possible causes of the observed changes (see47). Through our T2-wi analysis, we found that the CPZ protocol in mice, caused clear hyperintense areas in the corpus callosum and the white matter of the cerebellum. To confirm that these areas showed decreased myelin content, brain samples from these animals were processed with the BGII myelin-specific staining method48. We found that areas that showed hyperintensity in the T2-wi analysis coincided with brain regions that showed a significant decrease in BGII staining. This finding suggests that both methods highlighted demyelination as a probable cause of the observed changes. Thus, at least for these two brain areas, T2-wi can be useful to quickly evaluate the action of experimental agents that affect myelination such as short periods of CPZ intake.
In some structures, diffusion magnetic resonance imaging (dMRI) was necessary in addition to T2-wi in order to evaluate different parameters that together provided more specific information on the microstructure of myelin in the CNS23,25,49,50. Before proceeding with this analysis, we examined the areas that had been demyelinated by CPZ using BGII staining and, more importantly, we confirmed the promyelinating effect of β-CCB in several brain regions. It has been previously described that β-CCB has a promyelinating effect on focal demyelination in the rat icp5,12. Here, we show that the β-CCB treatment in mice demyelinated by CPZ intake promotes the recovery of myelin content in various structures. This finding clearly indicates that the possible promyelinating effect of β-CCB is more generalized in the NS.
The significant demyelination of gray matter structures in the CPZ model resembles that of MS patients30,33. Hence, we decided to analyze two gray matter structures: the mctx and the hippocampus. Histological findings showed that CPZ caused a clear decrease in BGII staining intensity in both structures but it was also observed that β-CCB treatment did not seem to cause myelin recovery. Nevertheless, when performing an analysis of hippocampal substructures, we found that β-CCB seemed to promote the partial recovery of BGII staining that was restricted to the CA3 area, suggesting a focalized promyelinating effect and the involvement of context-dependent factors. It is important to point out that histological analysis by BGII showed that the lateral cingulum (lc) did not present a decrease in myelin induced by CPZ intake, this confirmed results previously reported in this regard51. Furthermore, we did not observe β-CCB-induced changes in the lc. This supports the idea that the changes caused by CPZ and the lack of effects on the gray matter of the CPZ + β-CCB group represented reliable results, as the lc area acted as a sort of staining control.
In general, histological studies confirmed that in various areas of cerebral and cerebellar white matter, treatment with β-CCB promoted a recovery of myelin content evaluated by the intensity of BGII staining, suggesting that β-CCB acts as a general promyelinating agent in various tracts of the CNS.
It was therefore important to use MRI to evaluate the changes resulting from β-CCB treatment (CPZ + β-CCB group). This was done at the end of the trial with β-CCB and was important to determine whether the metrics obtained would support the histological results when these were compared with the CPZ group. First, we analyzed the cerebellar peduncles. Previous research has shown that these tracts are also affected by CPZ as well as in MS patients52,53. The metrics obtained by DTI analysis did not show significant changes between both groups; thus, the calculated metrics were not indicative of an improvement in myelin content and did not support the results obtained with histology. In contrast, when the mcc, fimbria, and ic areas were evaluated by DTI, diverse changes in metrics supported significant differences between the CPZ + β-CCB group and the CPZ group. In particular, we observed that metrics differed in the fimbria of these two groups. These differences were consistent with a promyelinating effect in the CPZ + β-CCB group. For example, the increase in FA in parallel with the significant decrease in the ADC and λ⊥ ratio are metrics consistent with an increase in myelin content, clearly supporting the idea of a promyelinating effect produced by β-CCB. Moreover, the increase in FA in both the mcc and ic indicated a possible increase in myelin content, which was further supported by a decrease in the λ⊥ ratio and ADC in the mcc and ic, respectively. Finally, the metrics evaluated for mctx and the CA3 area did not show significant changes. However, as mentioned, β-CCB treatment did not cause an increase in BGII staining in the mctx.
The contrast between DTI metrics and the histological analysis when comparing the CPZ and CPZ + β-CCB groups could have several explanations, and more experiments will be needed to determine the causes. However, this study indicates that white matter structures like the corpus callosum, ic, or fimbria were consistent in several DTI metrics and histological data. In the case of the fimbria, this is of interest because previous studies using different intoxication protocols showed that CPZ (0.2–0.25%) had a partial or no effect on this structure30,54. In our protocol, CPZ (0.3% for three weeks) produced significant demyelination, as suggested by DTI and histological examination, this difference is more probably due to the higher dose used here.
BGII staining showed a clear effect of β-CCB on myelin enhancement in several regions, although when analyzed with MRI there was correlation with some areas while not with others (e.g., cerebellar peduncles). This could be explained either due to a low technical resolution or due to specific concomitant changes (e.g., inflammation) resulting from the demyelination-remyelination process in different areas. Thus, areas that exhibit edema, inflammation, or other alterations could interfere with an adequate evaluation of DTI metrics, as has been discussed elsewhere55,56. Interestingly, in previous studies carried out in rats5,12, the demyelination-remyelination process was followed effectively in the icp region with both techniques. However, since the present study used mice, the technical characteristics of MRI protocols are substantially different. In addition, focal demyelination process and systemic demyelination caused by CPZ surely present significant differences in terms of the cellular responses provoked by either method.
In this study we showed that β-CCB had no effect on gray matter regions such as the mctx, as determined by both BGII and MRI. However, it is clear that CPZ had a significant effect on myelin content, as this has been documented before30,57,58. Similarly, no significant changes were observed in the hippocampus of the β-CCB-treated group, yet in the CA3, β-CCB-treatment seemed to partially reproduce the positive effect observed in other areas. One possible explanation for the lack of effect is a divergence in β-CCB action mechanisms at different areas of the CNS. Differences are expected due to ample evidence of genotypic and functional diversity of oligodendroglial cells59,60,61 and especially of the expression of GABAAR with different molecular compositions62, but also due to differences in the specific environmental contexts of each area63. These difference could determine the interaction between oligodendroglial cells and distinct cell types, mainly astrocytes and neurons64,65,66,67. In this sense, the divergence in regulatory remyelination mechanisms is dependent on intrinsic and extrinsic factors as well as epigenetic mechanisms68,69,70,71.
The promyelinating effect of β-CCB might be related to its potentiating effect on the response to GABA in cells of the oligodendroglial lineage3,5,8,12. It is known that OPCs are the main source of remyelination, where GABAergic signaling could be involved in OPC migration, proliferation, and differentiation processes6. In OPCs, GABAAR activation causes depolarization that activates voltage-gated channels with a consequent influx and increase in cytosolic Ca2+. It is also known that intracellular Ca2+ increase is involved in OPC proliferation, migration, and differentiation to myelinating cells72,73. Thus, potentiation of oligodendroglial GABAergic signaling induced by β-CCB might promote the activation of this cascade, resulting in OPC differentiation to mature OLs12. Quantitative immunolabeling analysis of OPCs and OLs using NG2 and CC1 markers indicated that CPZ intake caused a significant increase in the number of NG2+ cells and a decrease in CC1+ cells in white matter structures. These changes in the dynamics of oligodendroglial lineage populations were reversed by systemic treatment with β-CCB. In this way, the decrease in the number of NG2+ cells could be due to the fact that β-CCB enhanced the GABA response in precursor cells that eventually would promote their maturation to OLs, as suggested by the increase in CC1+ cells. The CPZ intake did not generate an increase in NG2+ cells in the mctx, but a clear decrease in CC1+ cells was found. This result was consistent with a demyelination process evidenced by BGII staining. Low OPC density, even after CPZ intake, might explain an inefficacy in generating new myelinating OLs in the mctx. However, more experiments are needed to clarify the process underlying this phenomenon.
Finally, it is well known that determining the content of myelin in the gray matter is complicated using DTI analysis74. This effect was reflected when comparing mctx metrics obtained from the CTRL group and the CPZ-demyelinated group, where the metrics did not suggest a decrease in myelin, even though histology showed clear images consistent with demyelination. In this case, more advanced methods for image acquisition and analysis are necessary to study gray matter areas. A final hypothesis to explain these discrepancies in gray matter structures is that CPZ intoxication is known to cause neuronal death, which would lead to axonal degeneration and an irreversible loss of myelin75,76. More studies are required to assess whether this deleterious effect could also explain the lack of β-CCB effects in the gray matter.
In summary, our results indicated that 0.3% CPZ administered for three weeks in the diet induced demyelination in mice. This brief protocol allowed for a better management of experimental groups with low animal mortality. It also allowed us to track the demyelinating and remyelinating stages of the model with the main purpose of evaluating the promyelinating effects of drugs with therapeutic potential. Here, we show that β-CCB, a positive allosteric modulator of the oligodendroglial GABAAR, has a robust promyelinating effect in different cerebral and cerebellar areas inducing an increase in the population of CC1+ mature oligodendrocytes.
Materials and methods
Study approval
All experiments were performed according to the procedures approved by the Ethics Committee of the Instituto de Neurobiología, Universidad Nacional Autónoma de México. Experiments were performed in C57BL/6J wild-type male mice (8 weeks old) following the Guide for the Care and Use of Laboratory Animals (National Institute of Health). Animals were kept under conventional housing conditions (22 ± 2 °C, 55 ± 10% humidity, 12 h day/night cycle and with ad libitum access to food and water) at the Instituto de Neurobiología, Universidad Nacional Autónoma de México. All possible efforts were made to minimize animal suffering and the number of animals used, and procedures complied with ARRIVE guidelines.
Experimental design
Animals in the control (CTRL) group were fed with normal diet for either 3, 6, or 9 weeks. To induce demyelination, a group of animals were fed with food containing 0.3% CPZ for 3 weeks and subsequently switched back to normal diet for 3 (3 + 3w protocol; Fig. 1a) or 6 (3 + 6w protocol; Fig. 4a) more weeks. 3 + 6w groups were injected intraperitoneally the last 3 weeks of the protocol either with vehicle alone (CPZ group) or, as this is detailed below, were injected with β-CCB (CPZ + β-CCB). Myelin content was evaluated at 4 points: (1) Before CPZ ingestion (0w; using MRI), (2) After 3 weeks of CPZ intake (3w; using both MRI and BGII), (3) At the end of 3 more weeks under normal diet (3 + 3w protocol; MRI and BGII), and (4) After 3 subsequent weeks in which animals were either treated with β-CCB or injected with vehicle alone (3 + 6w protocol; MRI and BGII). Additionally, at point 4, cell populations of the oligodendroglial lineage were analyzed by IF.
Cuprizone-induced demyelination
The animals had an acclimatization period to the experimental location for 1 week before beginning the study38. Experimental demyelination was induced by feeding 8-week-old male C57BL/6J mice with a diet containing 0.3% CPZ39,42 [bis(cyclohexanone)oxaldihydrazone] mixed with standard food (Specially Formulated Prolab, Laboratory Animal Diet. LabDiet) for three weeks26,27,28,29,30,36,37,38,39,40,41,42,43 and subsequently reestablishing the normal diet, for either three (3 + 3w protocol) or six weeks (3 + 6w protocol) depending on the experiment, a period in which the demyelination process continues26,27,28,29.
β-CCB administration
For in vivo β-CCB injection, aliquots of β-CCB solution were prepared as treatment and vehicle solution as a control. Every day before injection, 1 mg of β-CCB was diluted in DMSO and saline (2%/98% v/v) mixture (saline was 0.9% NaCl), whose volume was 1 mL per aliquot. The mixture was sonicated for 60 min at 37 °C. Then, vehicle alone (injected to CPZ group) or 1 mg/Kg β-CCB5,12 (injected to CPZ + β-CCB group) solution was intraperitoneally (i.p.) administered. Either injection was given every 24 h for three more weeks after six weeks of beginning the experiment (i.e., 3w CPZ intake and then reestablishing normal diet at the end of the third week), to complete a 3 + 6w protocol (see diagram in Fig. 4a). Mice were randomly assigned to each treatment based on a blinded analysis. In all cases, β-CCB treatment did not cause obvious alterations in animal behavior (e.g., anxious-like behavior).
Magnetic resonance imaging
All experimental groups were scanned at four times points: (1) Before CPZ ingestion, (2) After 3 weeks of CPZ intake, (3) At the end of 3 more weeks under normal diet (3 + 3w protocol), and (4) After 3 subsequent weeks in which animals were either treated with β-CCB or injected with vehicle alone (3 + 6w protocol). Anesthesia was induced with 2% isoflurane (in compressed air) using an anesthetic chamber and then maintained under 0.8–1% with a facemask during the procedure. T2-wi and diffusion magnetic resonance imaging (dMRI) were performed at the Laboratorio Nacional de Imagenología por Resonancia Magnética (LANIREM) using a 7 T magnet (Bruker Pharmascan 70/16US), interfaced to a Paravision 6.0.1 console (Bruker, Ettlingen, Germany), and with a Helium-cooled two-channel rat-head coil (Bruker Cryoprobe). DTI data sets were acquired using a spin-echo, single-shot echoplanar imaging sequence with the following parameters: slice thickness = 0.35 mm, slice gap = 0.1 mm, no physiological gating, RT = 2.23 s, ET = 23.4 ms, FOV = 28 × 28 mm2, image size = 150 × 150 mm, 40 diffusion directions, two different b values: 650 and 1250 s/mm2, 1 average, 46 slices, and with a total scanning time of 19 min, 19 s and 27 ms. T2-wi was acquired with the following parameters: slice thickness = 0.5 mm, inter-slice gap = 0.15 mm, RT = 4.2 s, ET = 33 ms, FOV = 30 × 15 mm2, image size = 256 × 256 mm2, rare factor = 8, 2 averages and 25 slices, and with a total scanning time of 4 min and 48 s. Pre-processing of dMRI data sets included both reduction of motion and eddy current-induced geometric distortions by linear transformation of each volume to the average non-diffusion weighted volume and denoising via random matrix theory77. The MRtrix software package (http://www.mrtrix.org) was used to estimate the tensor model, from which we derived fractional anisotropy (FA) maps, principal diffusion vector (PDV), radial and axial diffusivities (λ⊥ and λ||, respectively), and the apparent diffusion coefficient (ADC). Region of interest (ROI) of acc, mcc, ic, fimbria, cerebellum, scp, mcp, icp, CA3 of the hippocampus, and mctx were manually delineated on PDV images. DTI parameters were calculated using ROI analysis.
Black-Gold II staining
For histological examination, mice were transcardially perfused with 0.1 M phosphate-buffered saline (PBS) (pH 7.4) followed by 4% paraformaldehyde (PFA) in the same buffer; subsequently, the brains were dissected. Then, to cryopreserve them, they were placed in a PBS 30% sucrose solution (50 mL PBS/15 g sucrose) for 24 h. After cryopreservation, coronal sections with a thickness of 50 µm were obtained in a cryostat (Leica CM 1850) at a temperature between – 24 °C and – 26 °C and suspended in PBS. BGII staining, a myelin-specific aurohalophosphate compound48, was performed in suspension for the evaluation of myelin content5,12. For this, each 50 µm section was rinsed with ultrapure water for 2 min, then incubated in BGII solution (dissolved at 0.3% in 0.9% NaCl solution) for 12–20 min at 60–65 °C. Subsequently, the sections were rinsed with PBS for 2 min and then with 1% sodium thiosulfate (Na-Thio) for 3 min at 60–65 °C, and finally a series of two rinses with PBS for 2 min each. Then, sections were placed on slides and xylol was added for 1 min. Subsequently, DPX medium was added and a coverslip was placed. For myelinated zone assessment, tissue sections for BGII were visualized and analyzed under a microscope, and representative images were acquired with a Leica ICC50 HD camera (Leica Microsystems, Wetzlar, Germany). The relative intensity of myelin BGII staining (RIS) in selected brain areas was quantified using ImageJ software (version 1.52i). After converting the images to grayscale, the relative intensity was obtained from a given ROI, calculated by normalizing intensity values from each ROI against the background intensity value from each section22, applying the following relationship: RIS = (intensity of background − mean intensity of labeling in ROIs)/intensity of background.
Immunofluorescence
To examine cell populations of the oligodendroglial lineage, specifically OPCs and OLs, 50 µm thick coronal sections were immunoassayed with antibodies against oligodendroglial cell-specific markers: mouse anti-APC/CC1 (1:250; Sigma-Aldrich, OP80) for mature OLs1,31,32 and rabbit anti-NG2 (1:250; Millipore, AB5320) for OPCs1,32. First, the fixed sections were washed and permeabilized in PBS with 0.1% Tween-20. Next, the sections were incubated in a blocking buffer solution (PBS, 5% BSA, and 0.3% Triton X-100) for 30 min at 4 °C. They were then incubated with the primary antibodies (diluted in PBS containing 5% goat serum and 0.1% Tween-20) overnight at 4 °C. Sections were then rinsed in PBS with 0.1% Tween-20 and incubated for 4 h at 4 °C with one of the following Alexa fluorophores-conjugated: 1:300 goat anti-mouse IgG (H + L) conjugated to Alexa Fluor 488 (Invitrogen, A-11001) or 1:300 goat anti-rabbit IgG (H + L) conjugated to Alexa Fluor 594 (Abcam, ab150080) depending on the host species of the primary antibodies. To identify the cell nuclei, five washes were performed in PBS with 0.1% Tween-20, and the sections were subsequently stained with 4′,6-diamidino-2-phenylindole dihydrochloride (4 μg/mL DAPI, Molecular Probes, D1306) and mounted on Mowiol (Sigma-Aldrich, 81381). In all cases, to corroborate the absence of nonspecific interactions of the secondary antibodies, the primary antibodies were omitted. Finally, the preparations were visualized under an LSM880 laser scanning confocal microscope (Zeiss, Oberkochen, DE). Each slice was then observed using a 20 × objective and images were acquired with a Z step size of 1 μm, forming a 3 × 1 tile-scan mosaic. Visualization and quantitative analysis of each Z-stack was performed using the NIH (USA) ImageJ software (https://imagej.net) and regions of interest (ROI) were outlined using the freehand selection tool. In the ROIs, the proportional area corresponding to the mark of NG2+ cells was estimated with respect to the total area of the ROI and in the case of the mature OLs, the proportion of CC1+ cells was estimated with respect to the total number of nuclei using the “Analyze Particles” plugin from ImageJ (https://imagej.net/imaging/particle-analysis). For each marker analyzed, it was considered as positive immunoreactive cell those that stand out from the background. The values were expressed as % of the total.
Substances
β-CCB was obtained from Tocris Bioscience (Bristol, UK) and isoflurane from PiSa Lab (Guadalajara, JAL, México). All salts, PFA, CPZ and xylenes were acquired from Sigma-Aldrich (St. Louis, MO, USA). The BGII myelin staining kit was acquired from Millipore (EMD Millipore Corp., Billerica, MA, USA), and DPX mounting medium was from Fisher Scientific (FS, Fair Lawn, NJ, USA).
Statistical analysis
All data are expressed as mean ± S.D. The means of two groups were compared using a Student's t-test or, when appropriate, an analysis of variance (ANOVA) followed by post-hoc comparisons of individual means using the Fisher correction. Animals were randomized to treatment according to local practice in participating centers. We assumed an effect size of around 1.4 (Cohen's d estimate calculation) and 80% power in detecting changes between group means in the in vivo experiments with a significance level of 0.05, which is consistent with previous studies using similar experimental models5,16,58. Homoscedasticity was verified using Levene's test. The Kolmogorov–Smirnov test was used to verify the normal distribution of the data. Statistical analysis was performed using GraphPad Prism software. Differences were significant at P < 0.05 (the exact values for P were indicated in the corresponding results section).
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Zonouzi, M. et al. GABAergic regulation of cerebellar NG2 cell development is altered in perinatal white matter injury. Nat. Neurosci. 18, 674–682 (2015).
Hamilton, N. B. et al. Endogenous GABA controls oligodendrocyte lineage cell number, myelination, and CNS internode length. Glia 65, 309–321 (2017).
Arellano, R. O. et al. Axon-to-glia interaction regulates GABAA receptor expression in oligodendrocytes. Mol. Pharmacol. 89, 63–74 (2016).
Kalakh, S. & Mouihate, A. Enhanced remyelination during late pregnancy: Involvement of the GABAergic system. Sci. Rep. 9, 1–16 (2019).
Cisneros-Mejorado, A. J. et al. Demyelination-remyelination of the rat caudal cerebellar peduncle evaluated with magnetic resonance imaging. Neuroscience 439, 255–267 (2020).
Serrano-Regal, M. P. et al. Expression and function of GABA receptors in myelinating cells. Front. Cell. Neurosci. 14, 1–15 (2020).
Reyes-Haro, D., Cisneros-Mejorado, A. & Arellano, R. O. Therapeutic potential of GABAergic signaling in myelin plasticity and repair. Front. Cell Dev. Biol. 9, 1–8 (2021).
Ordaz, R. P. et al. GABAA receptors expressed in oligodendrocytes cultured from the neonatal rat contain α3 and γ1 subunits and present differential functional and pharmacological properties. Mol. Pharmacol. 99, 133–146 (2021).
Thomet, U., Baur, R., Scholze, P., Sieghart, W. & Sigel, E. Dual mode of stimulation by the β-carboline ZK 91085 of recombinant GABAA receptor currents: Molecular determinants affecting its action. Br. J. Pharmacol. 127, 1231–1239 (1999).
Izquierdo, I. A game with shifting mirrors. Trends Pharmacol. Sci. 10, 473–476 (1989).
Novas, M. L., Wolfman, C., Medina, J. H. & de Robertis, E. Proconvulsant and ‘anxiogenic’ effects of n-butyl β carboline-3-carboxylate, an endogenous benzodiazepine binding inhibitor from brain. Pharmacol. Biochem. Behav. 30, 331–336 (1988).
Cisneros-Mejorado, A. J., Ordaz, R. P., Garay, E. & Arellano, R. O. β-carbolines that enhance GABAA receptor response expressed in oligodendrocytes promote remyelination in an in vivo rat model of focal demyelination. Front. Cell. Neurosci. 18, 9730 (2024).
Zhan, J. et al. The cuprizone model: Dos and do nots. Cells 9, 843 (2020).
Torkildsen, Ø., Brunborg, L. A., Myhr, K.-M. & Bø, L. The cuprizone model for demyelination. Acta Neurol. Scand. 117, 72–76 (2008).
Zhen, W. et al. An alternative cuprizone-induced demyelination and remyelination mouse model. ASN Neuro 9, 5174 (2017).
Tagge, I. et al. Spatio-temporal patterns of demyelination and remyelination in the cuprizone mouse model. PLoS ONE 11, 1–24 (2016).
Wang, N. et al. Probing demyelination and remyelination of cuprizone mice model using multimodality MRI. J. Magn. Reson. Imaging 50, 1852–1865 (2019).
Ding, S. et al. Demyelination and remyelination detected in an alternative cuprizone mouse model of multiple sclerosis with 7.0 T multiparameter magnetic resonance imaging. Sci. Rep. 11, 1–11 (2021).
Groebe, A. et al. Cuprizone treatment induces distinct demyelination, astrocytosis, and microglia cell invasion or proliferation in the mouse cerebellum. Cerebellum 8, 163–174 (2009).
Milbocker, K. A. et al. Reduced and delayed myelination and volume of corpus callosum in an animal model of fetal alcohol spectrum disorders partially benefit from voluntary exercise. Sci. Rep. 12, 1–17 (2022).
Yi Teo, R. T. et al. Structural and molecular myelination deficits occur prior to neuronal loss in the YAC128 and BACHD models of Huntington disease. Hum. Mol. Genet. 25, 2621–2632 (2016).
Hakkarainen, H. et al. MRI relaxation in the presence of fictitious fields correlates with myelin content in normal rat brain. Magn. Reson. Med. 75, 161–168 (2016).
Song, S. K. et al. Demyelination increases radial diffusivity in corpus callosum of mouse brain. Neuroimage 26, 132–140 (2005).
Barkovich, A. J. Concepts of myelin and myelination in neuroradiology. Am. J. Neuroradiol. 21, 1099–1109 (2000).
Song, S. K. et al. Diffusion tensor imaging detects and differentiates axon and myelin degeneration in mouse optic nerve after retinal ischemia. Neuroimage 20, 1714–1722 (2003).
Doan, V. et al. Abbreviated exposure to cuprizone is sufficient to induce demyelination and oligodendrocyte loss. J. Neurosci. Res. 91, 363–373 (2013).
Große-Veldmann, R. et al. Lesion expansion in experimental demyelination animal models and multiple sclerosis lesions. Mol. Neurobiol. 53, 4905–4917 (2016).
Hochstrasser, T., Exner, G. L., Nyamoya, S., Schmitz, C. & Kipp, M. Cuprizone-containing pellets are less potent to induce consistent demyelination in the Corpus Callosum of C57BL/6 mice. J. Mol. Neurosci. 61, 617–624 (2017).
Scheld, M. et al. Neurodegeneration triggers peripheral immune cell recruitment into the forebrain. J. Neurosci. 36, 1410–1415 (2016).
Koutsoudaki, P. N. et al. Demyelination of the hippocampus is prominent in the cuprizone model. Neurosci. Lett. 451, 83–88 (2009).
Balia, M., Benamer, N. & Angulo, M. C. A specific GABAergic synapse onto oligodendrocyte precursors does not regulate cortical oligodendrogenesis. Glia 65, 1821–1832 (2017).
Viganò, F. et al. GPR17 expressing NG2-Glia: Oligodendrocyte progenitors serving as a reserve pool after injury. Glia 64, 287–299 (2016).
Albert, M., Antel, J., Brück, W. & Stadelmann, C. Extensive cortical remyelination in patients with chronic multiple sclerosis. Brain Pathol. 17, 129–138 (2007).
Dobson, R. & Giovannoni, G. Multiple sclerosis: A review. Eur. J. Neurol. 26, 27–40 (2019).
Michael Conn, P. Animal Models for the Study of Human Disease (Elsevier Inc., 2017).
Morgan, M. L. et al. Cuprizone-induced demyelination in mouse brain is not due to depletion of copper. ASN Neuro 14, 175909142211263 (2022).
Skripuletz, T., Gudi, V., Hackstette, D. & Stangel, M. De- and remyelination in the CNS white and grey matter induced by cuprizone: The old, the new, and the unexpected. Histol. Histopathol. 26, 1585–1597 (2011).
Toomey, L. M. et al. Cuprizone feed formulation influences the extent of demyelinating disease pathology. Sci. Rep. 11, 22594 (2021).
Bernal-Chico, A. et al. P2x7 receptors control demyelination and inflammation in the cuprizone model. Brain Behav. Immun. Health 4, 100062 (2020).
Kipp, M., Nyamoya, S., Hochstrasser, T. & Amor, S. Multiple sclerosis animal models: A clinical and histopathological perspective. Brain Pathol. 27, 123–137 (2017).
Kumar, S., Biancotti, J. C., Yamaguchi, M. & de Vellis, J. Combination of growth factors enhances remyelination in a cuprizone-induced demyelination mouse model. Neurochem. Res. 32, 783–797 (2007).
Manterola, A. et al. Deregulation of the endocannabinoid system and therapeutic potential of ABHD6 blockade in the cuprizone model of demyelination. Biochem. Pharmacol. 157, 189–201 (2018).
Matsushima, G. K. & Morell, P. The neurotoxicant, cuprizone, as a model to study demyelination and remyelination in the central nervous system. Brain Pathol. 11, 107–116 (2001).
Lee, M. A., Smith, S., Palace, J. & Matthews, P. M. Defining multiple sclerosis disease activity using MRI T2-weighted difference imaging. Brain 121, 2095–2102 (1998).
Brück, W. et al. Inflammatory central nervous system demyelination: Correlation of magnetic resonance imaging findings with lesion pathology. Ann. Neurol. 42, 783–793 (1997).
De Groot, C. J. A. et al. Post-mortem MRI-guided sampling of multiple sclerosis brain lesions: Increased yield of active demyelinating and (p)reactive lesions. Brain 124, 1635–1645 (2001).
Fallier-Becker, P., Bonzheim, I. & Pfeiffer, F. Cuprizone feeding induces swollen astrocyte endfeet. Pflügers Arch. Eur. J. Physiol. 474, 1275–1283 (2022).
Schmued, L. et al. Introducing Black-Gold II, a highly soluble gold phosphate complex with several unique advantages for the histochemical localization of myelin. Brain Res. 1229, 210–217 (2008).
Budde, M. D., Xie, M., Cross, A. H. & Song, S. K. Axial diffusivity is the primary correlate of axonal injury in the experimental autoimmune encephalomyelitis spinal cord: A quantitative pixelwise analysis. J. Neurosci. 29, 2805–2813 (2009).
Song, S. K. et al. Dysmyelination revealed through MRI as increased radial (but unchanged axial) diffusion of water. Neuroimage 17, 1429–1436 (2002).
Schmidt, T. et al. Regional heterogeneity of cuprizone-induced demyelination: Topographical aspects of the midline of the Corpus callosum. J. Mol. Neurosci. 49, 80–88 (2013).
Blakemore, W. F. Demyelination of the superior Cerebellar peduncle in the mouse induced by cuprizone. J. Neurol. Sci. 20, 63–72 (1973).
Preziosa, P. et al. Relationship between damage to the cerebellar peduncles and clinical disability in multiple sclerosis. Radiology 271, 822–830 (2014).
Kipp, M. et al. The hippocampal fimbria of cuprizone-treated animals as a structure for studying neuroprotection in multiple sclerosis. Inflamm. Res. 60, 723–726 (2011).
Assaf, Y. & Pasternak, O. Diffusion tensor imaging (DTI)-based white matter mapping in brain research: A review. J. Mol. Neurosci. 34, 51–61 (2008).
Winklewski, P. J. et al. Understanding the physiopathology behind axial and radial diffusivity changes-what do we Know?. Front. Neurol. 9, 92 (2018).
Skripuletz, T. et al. Cortical demyelination is prominent in the murine cuprizone model and is strain-dependent. Am. J. Pathol. 172, 1053–1061 (2008).
Wergeland, S., Torkildsen, Ø., Myhr, K. M., Mørk, S. J. & Bø, L. The cuprizone model: Regional heterogeneity of pathology. Apmis 120, 648–657 (2012).
Spitzer, S. O. et al. Oligodendrocyte progenitor cells become regionally diverse and heterogeneous with age. Neuron 101, 459-471.e5 (2019).
Chittajallu, R., Aguirre, A. & Gallo, V. NG2-positive cells in the mouse white and grey matter display distinct physiological properties. J. Physiol. 561, 109–122 (2004).
Marisca, R. et al. Functionally distinct subgroups of oligodendrocyte precursor cells integrate neural activity and execute myelin formation. Nat. Neurosci. 23, 363–374 (2020).
Gutierrez, B. A., González-Coronel, J. M., Arellano, R. O. & Limon, A. Transcriptional and bioinformatic analysis of GABAA receptors expressed in oligodendrocyte progenitor cells from the human brain. Front. Mol. Neurosci. 16, 232 (2023).
Viganò, F., Möbius, W., Götz, M. & Dimou, L. Transplantation reveals regional differences in oligodendrocyte differentiation in the adult brain. Nat. Neurosci. 16, 1370–1372 (2013).
Patt, L. et al. Impact of developmental changes of GABAA receptors on interneuron-NG2 glia transmission in the hippocampus. Int. J. Mol. Sci. 24, 13490 (2023).
Domingues, H. S., Portugal, C. C., Socodato, R. & Relvas, J. B. Oligodendrocyte, astrocyte, and microglia crosstalk in myelin development, damage, and repair. Front. Cell Dev. Biol. 4, 1–16 (2016).
Benamer, N., Vidal, M., Balia, M. & Angulo, M. C. Myelination of parvalbumin interneurons shapes the function of cortical sensory inhibitory circuits. Nat. Commun. 11, 5151 (2020).
Liu, Y. et al. Interactions of glial cells with neuronal synapses, from astrocytes to microglia and oligodendrocyte lineage cells. Glia 71, 1383–1401 (2023).
Moyon, S., Liang, J. & Casaccia, P. Epigenetics in NG2 glia cells. Brain Res. 1638, 183–198 (2016).
Rosenberg, S. S., Kelland, E. E., Tokar, E., De La Torre, A. R. & Chan, J. R. The geometric and spatial constraints of the microenvironment induce oligodendrocyte differentiation. Proc. Natl. Acad. Sci. USA 105, 14662–14667 (2008).
Gudi, V. et al. Spatial and temporal profiles of growth factor expression during CNS demyelination reveal the dynamics of repair priming. PLoS ONE 6, e22636 (2011).
Mayoral, S. R. & Chan, J. R. The environment rules: Spatiotemporal regulation of oligodendrocyte differentiation. Curr. Opin. Neurobiol. 39, 47–52 (2016).
Paez, P. M., Fulton, D., Colwell, C. S. & Campagnoni, A. T. Voltage-operated Ca2+ and Na+ channels in the oligodendrocyte lineage. J. Neurosci. Res. 87, 3259–3266 (2009).
Tong, X. P. et al. Ca2+ signaling evoked by activation of Na+ channels and Na+/Ca2+ exchangers is required for GABA-induced NG2 cell migration. J. Cell Biol. 186, 113–128 (2009).
Assaf, Y. Imaging laminar structures in the gray matter with diffusion MRI. Neuroimage 197, 677–688 (2018).
An, J. et al. Temporal and spatial evolution of various functional neurons during demyelination induced by cuprizone. J. Neurophysiol. 126, 1756–1771 (2021).
Ogunlade, B., Fidelis, O. P., Afolayan, O. O. & Agie, J. A. Neurotherapeutic and antioxidant response of D-ribose-L-Cysteine nutritional dietary supplements on Alzheimer-type hippocampal neurodegeneration induced by cuprizone in adult male wistar rat model. Food Chem. Toxicol. 147, 111862 (2021).
Jelescu, I. O. et al. In vivo quantification of demyelination and recovery using compartment-specific diffusion MRI metrics validated by electron microscopy. Neuroimage 132, 104–114 (2016).
Acknowledgements
We thank the personnel at the INB-UNAM Animal Facility and Juan Ortiz-Retana for assistance during MRI acquisition. Imaging was performed at LANIREM. We also thank Nydia Hernández Ríos, Martín García Servín, Alejandra Castilla León, María A. Carbajo Mata, Leopoldo González Santos, Ramón Martínez Olvera, Remy Ávila, Reinher Pimentel and the LANCAM for their technical assistance and thank Jessica González Norris for editing this manuscript. F. V-U., is a PhD student (CONAHCYT student grant to CVU: 857777) from Programa de Doctorado en Ciencias Biomédicas at Universidad Nacional Autónoma de México (UNAM). This work was supported by grants from PAPIIT-UNAM-México No. IN205822 and CONAHCYT CF-319740 to ROA laboratory, and CONAHCYT CF-1771 to AJC-M (CONAHCYT-Researcher, IxM). RPO is a Postdoctoral Researcher (CVU: 700811) at CONAHCYT, Mexico.
Author information
Authors and Affiliations
Contributions
Participated in research design: ROA, AJC-M, EG, FV-U. Conducted experiments: AJC-M, FV-U, RPO. Analyzed the data: ROA, AJC-M, EG, RPO, FV-U. Wrote or contributed to the writing of the manuscript: ROA, AJC-M, EG, RPO, FV-U.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vélez-Uriza, F., Ordaz, R.P., Garay, E. et al. N-butyl-β-carboline-3-carboxylate (β-CCB) systemic administration promotes remyelination in the cuprizone demyelinating model in mice. Sci Rep 14, 13988 (2024). https://doi.org/10.1038/s41598-024-64501-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64501-x
- Springer Nature Limited