Abstract
Parental stress occurs when parenting demands exceed the resources available to cope with parenting. Previous research has identified household wealth, educational level, marital status, age, and number of dependent children as predictors of parental stress. However, limited evidence exists from sub-Saharan Africa. This study investigated the sociodemographic predictors of parenting stress among mothers in Kenya and Zambia. This cross-sectional study utilised baseline secondary data from parenting intervention programs implemented in Kisumu County (rural Kenya), Nairobi County (Urban Kenya), and Chisamba District (rural Zambia). Out of 913 caregivers recruited for the parenting program, 844 with complete data were included in the analysis. The mean age was 1.0 (SD = 0.7) years. Parental stress was measured using the Parental Stress Score (PSS) tool and demographic questionnaires were used to collect demographic information. Mean PSS were compared across study sites, and a multiple linear regression model was used to examine associations between sociodemographic predictors (household income, educational level, marital status, maternal age, child age, and number of children aged < 5 years) and PSS, adjusting for clustering and other predictors. From the results, the mean PSS in rural Kenya was 37.6 [SD = 11.8], in urban Kenya was 48.4 [SD = 4.2], and in rural Zambia was 43.0 [SD = 9.1]. In addition, the significant association between PSS and mothers’ income and educational level was only observed in Kenyan study sites (income: Kenya rural β = -0.40, p < 0.001**; Kenya urban, β = − 0.33, p = .02*; Zambia rural, β = − 0.01, p = 0.7) education: Kenya rural, β = − 0.25, p = .005**; Kenya urban, β = − 0.14, p = 0.07; Zambia rural, β = 0.04, p = 0.3). However, marital status, mother’s age, child’s age, and the number of children below five years were not associated with PSS. The results revealed that mothers’ income and education level were negatively associated with PSS, indicating that higher socioeconomic status can buffer the effects of parental stress.
Trial registration Pan African Clinical Trials Registry (https://pactr.samrc.ac.za/) database (ID Number: PACTR20180774832663 Date: 26/July/2018; (ID number: PACTR201905787868050 Date: 06/May/2019.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Parental stress occurs when parenting demands exceed the resources available to cope with parenting1. This negatively affects the overall functioning of the children and their parents, as stress negatively affects parents’ mental health and well-being, resulting in poor psychological and physical health2,3,4. Parental psychological stress may also affect their children’s well-being, that is, their psychological, health, and developmental outcomes. A distressed parent might not be actively engaged in stimulating interactions with their children, which increases the risk of maltreatment and adverse childhood experiences5,6,7,8,9. This makes it important to identify and address predictors of parental stress.
Studies in other countries (Chile, the USA and China) have identified a range of sociodemographic predictors of parental stress. Maternal characteristics such as household wealth, educational level, marital status, age, and the number of children under their care have been indicated as predictors of parental stress10,11,12,13. Poverty has been associated with poor mental health outcomes13,14,15, and dealing with financial difficulties/hardships leads to high stress levels and negatively affects an individual’s health16. Families living in poverty often face challenges such as inadequate financial and educational resources, food insecurity, relationship instability, and overall unpredictability17,18.
Lower educational levels have also been shown to contribute to parenting stress18. Since parents’ education is associated with their knowledge, attitudes, and practices, educated parents are likely to be informed about better parenting practices and practice positive parenting. They are likely to have access to better income to meet their parenting needs, thereby reducing parenting stress. However, other findings have also demonstrated higher parental stress among mothers with high education (postgraduate degree) and significantly lower parenting stress among mothers with intermediate education (university degree/diploma/vocational training)11. These findings could be attributed to the fact that even though education is related to greater resources, which could lead to less parental anxiety, it also facilitates alternative fulfilment, that is, satisfaction with career progression/achievements, which may lead to a greater feeling of dissatisfaction with parenting19. In addition, it could also be attributed to ‘parents’ education anxiety’20 in which a parent experiences tension, panic, worry, and other forms of negative emotions regarding whether their parenting practices positively affect their children’s developmental outcomes.
Regarding marital status, a study in Kenya and Zambia reported that community support systems lessened the parenting burden on mothers, especially support from their spouses21. Specifically, one study found that mothers reported that fathers’ involvement in parenting reduced the stressors that came with parenting21. Such findings have also been evident in other contexts, such as a study in the USA on mothers in low-income settings22. For mothers in low-income settings, marriage could be a great contributor to an improved household financial base, emotional support, and support in caring for the child(ren)23. Marriage quality can also contribute to stress and health outcomes24. Marital quality is often defined as the subjective evaluation of relationships and behaviours in relationships, measured by self-reported attitudes towards one’s partner and marriage. This is often rated as behaviour indicating low quality (hostile or withdrawing behaviours) or high quality (supportive behaviours)24. Low-quality marriage has been associated with the development of mood disorders and vulnerability to mental health-related illnesses25.
Maternal age has also been reported as a predictor of parental stress. Specifically, mothers between 30 and 35 years of age reported less stress than mothers who were younger or older than this age10. Younger mothers are likely to experience parenting stress due to limited financial and social support and experience in childcare. On the other hand, older parents might experience stigma towards older parenthood and lack social support from extended families, which might affect their psychological well-being. In a study in the USA by Dougall et al.26 mothers older than 40 years reported that even though having children in their forties was advantageous for career establishment and financial security, it also meant that they lacked parenting energy. In addition, the number of children under mothers’ care is also a predictor of parental stress, with mothers with more than one child below eight years reporting higher parental stress levels12. Qian et al.12 found that two-child families in China had higher parenting stress than only-child families. This could be attributed to the financial and other support needs of more than two children in these age groups. In addition, mothers with more than one child reported requiring more time and energy to meet parenting demands12. These effects are significant in understanding contexts such as Kenya and Zambia, where it is estimated that there are an average of four children per family27,28. In sub-Saharan Africa (SSA), the geographical area of the African continent that is situated south of the Sahara desert and includes 48 countries and encompassing Middle, Eastern, Southern, and Western Africa29) context, qualitative research in Tanzania showed that family finances, marital relationships, child-related factors such as illness, and economic resources within the community contribute to parental stress30. Other studies in the SSA context have identified an association between mental health and parental stress, and male caregivers who perceived parenting as a burden had higher parenting stress scores7,31. However, there is limited evidence on socio-demographic predictors in the SSA context, where factors such as the poverty index are very high compared to developed countries.
The present study is a secondary analysis of existing studies from SSA. This offers a cost-effective and ethically responsible approach to research, particularly in low-resource settings, where securing funding for primary research can be challenging. Additionally, by utilising secondary data, researchers can maximise the contributions of participants’ data, yielding new scientific insights without the need for additional time, money, or resources. Studies have utilised this approach, especially in SSA, where there is limited research funding, thereby enriching the literature and promoting a more sustainable and ethical model by making use of available data32. Therefore, we used datasets from three previous studies conducted in Kenya and Zambia and investigated the association between mothers’ demographic characteristics, such as age, income, education, marital status, number of children below five years of age, and parental stress level. Utilisation of these three distinct studies provides conceptual replication attempts across multiple settings which helps establish how generalizable such findings are. The PSS tool was used to obtain information from parents on their experience of undertaking day-to-day parental responsibility33. This study aimed to investigate the association between mothers’ demographic characteristics and PSS.
Methodology
Study design
This cross-sectional study utilised baseline secondary data from parenting intervention programs implemented in Kisumu County (rural Kenya), Nairobi County (urban Kenya), and Chisamba District (rural Zambia)28. In these three studies, participants were assigned to either the intervention group, which provided a parenting program, or the control group, which received standard care from the Ministry of Health and Education. Participants were drawn from villages/clusters. These clusters were purposively selected to ensure a buffer zone between the intervention and the control arms. In both rural Kenya and rural Zambia study sites, the parenting program intervention was implemented by the Episcopal Relief and Development (ERD) team, together with the Zambia Anglican Council Programmes (ZACOP) in Zambia and with ACK Development Services (ADS) Nyanza in Kenya. This program targeted children below three years of age and focused on enhancing caregivers’ parenting skills to promote their children’s growth and development34. For urban Kenya, the African Population and Health Research Centre (APHRC) in partnership with Val Partners and the Ministry of Health implemented an Early Childhood Development (ECD) mobile phone technology application to help young mothers track and respond to their children's developmental progress in a timely manner. This program aimed to improve caregivers’ knowledge, attitudes, and practices on children’s growth and development through training, the use of mobile phone technology to track and stimulate their children’s growth and development, identification of developmental delays, mentorship visits by the Community Health Volunteer (CHVs), and referral to a health facility to address the identified developmental delays.
Study sites
The study reported in this paper was conducted in both Kenya and Zambia. In Kenya’s rural areas, the study was conducted in the Awasi-Onjiko ward, Nyando sub-county, and Kisumu County. Nyando sub-county had a lower uptake of immunisation, at 76.6%, compared to the county average of 82%. The proportion of mothers who attended four ANC visits was also lower in Nyando (48.4%), compared to the county average of 49.7%). In addition, the greater Nyanza region has a higher HIV prevalence rate of 19.3%, which is above the national average of 5.9%35. The study site in which the parenting program intervention was implemented was identified by the Ministry of Health (MOH) Health Information System (HIS) as the most vulnerable area in the entire Nyando sub-county.
In Zambia, the parenting program was implemented in the Mwantaya and Chamuka wards of Chisamba District in Central Province. The Chisamba district has a population of 103,983, with a higher HIV prevalence rate than the national average (13.4%)36. Notably, malnutrition rates were high, with stunted growth in children below five years (42.1%). In addition, Mwantaya Ward has only one health clinic despite being sparsely populated36.
In urban Kenya, the study was conducted in the Korogocho ward within the Ruaraka sub-county, Nairobi County. Nairobi County, which has 17 sub-counties, has a total population of approximately 4,004,40037. Korogocho is a densely populated ward with 41,946 residents and is characterised by high levels of poverty, high birth rates, and a large proportion of young mothers; 25 per cent of mothers of children under five are aged less than 20 years38. Poor feeding and childcare practices have been documented among these mothers and are associated with a high stunting rate (50%) and a high infant mortality rate of 57 deaths per 1000 live births38. The Korogocho ward was selected for the implementation of the parenting program because of its poor indicators of maternal and child health outcomes39.
Sample size calculation
In rural Kenya, the sample size was calculated based on Hemming and Girling’s study40 with six clusters in each arm and a fixed number of clusters. The number of mothers per arm was 132, implying a total sample size of 264 for the two arms. Due to limited resources, with six clusters in each arm, the intracluster correlation (ICC) was set at 0.02, the effect size at 0.43, and the dropout rate at 10%. A similar sampling calculation was performed for rural Zambia40, with an assumed minimum detectable effect size of 0.4 with an ICC of = 0.03. The team also estimated a confidence interval of 95%, a power of 80%, and a dropout rate of 10%. Thus, the total sample size for each arm was n = 255 (510 mothers). However, only 395 mothers (children aged < 18 months or pregnant women in the third trimester) met the inclusion criteria. The inclusion criteria included vulnerability status (for example, health and nutrition indicators, HIV exposure and poverty levels) and long-term residency (more than one year) in the study area.
In the Kenyan urban study, the sample size was calculated using the G*Power program, where the program was set to a one-sided t-test involving the difference between two independent means40. Using a priori power analysis, we inputted the values of 0.05 and 0.84 the significance levels and a power of respectively. Additionally, equal-sized sample groups were assumed, meaning that the allocation ratio of N1 (intervention group) to N2 (control group) was one. The calculation produced a sample size of 100 for each group, which allowed for a 10% attrition rate gave a result of 110. A total of 254 households were recruited.
Study sample
Out of 913 caregivers recruited for the parenting program 844 with complete data were included in the analysis. We included mother-infant pairs from the three studies that participated in the baseline (Kenya rural, n = 231; Kenya urban, n = 235; Zambia rural, n = 378) with complete data on the outcome and predictors variables as shown in Fig. 1. Therefore, based on the original studies, assumptions could yield a detectable effect size of 0.4 with an ICC of 0.03, a confidence interval of 95%, and 80% power.
Measures
Parental Stress Score (PSS) was used for the outcome and sociodemographic predictor information was collected using a questionnaire for mothers questionnaires. Trained Research Assistants administered the questionnaire using an interviewer-assisted method, and the average duration for each respondent was estimated to be one hour. The questionnaire covered items on mothers’ socio-demographics, caregiving knowledge, attitudes, and practices, PSS, health-seeking behaviours, and the Ages and Stages Questionnaire (ASQ).
PSS outcome measure
This study focused on parental stress levels, measured using the PSS tool to obtain information on parents’ feelings and perceptions of their parenting experience. Studies on the validity and reliability of PSS tools have indicated good internal consistency, construct validity, convergent validity, and test–retest reliability33,41,42,43,44,45. Notably, for this study, Cronbach’s alpha coefficient for the internal consistency of the items in the PSS was acceptable for all study sites (Kenya rural: 0.80, Kenya urban: 0.74, and Zambia rural: 0.84). The mothers’ PSS responses were assigned scores based on a 5-point Likert Scale (1 = Strongly Disagree, 2 = Disagree, 3 = Not Sure, 4 = Agree, 5 = Strongly Agree) (Table 1). To compute the PSS, items 1, 2, 5, 6, 7, 8, 17, and 18 were reversed and scored as follows: (1 = 5) (2 = 4) (3 = 3) (4 = 2) (5 = 1) as shown in Table 1. The item scores were then summed. A low score signifies a low level of stress, and a high score indicates a high level of stress. The overall possible scores on the scale ranged from 18 to 90.
Sociodemographic predictor measures
The predictors were the following sociodemographic characteristics: income, education level, marital status, mother’s age, child’s age, and number of children aged < 5 years. Information on these were collected via a structured questionnaire. Mothers’ incomes are reported in bands (below USD 50, between USD 50 and 100, and above USD 100 per month). Mothers’ level of education was categorised as primary, secondary, and postsecondary education, which included college and vocational education. Marital status was categorised as married (living together/cohabiting, legally married) or unmarried (single, divorced, separated, or widowed). The number of children aged < 5 years under care included all those living in the same household, including nonbiological children.
Statistical analysis
Data cleaning and analysis were performed using the R software and R Studio46. A multiple linear regression model was used to determine the association between mothers’ parenting stress scores and their sociodemographic characteristics, with adjustments for clustering and the study arm (control/intervention) at each study site. In the unadjusted model, the outcome variable was PSS, while the predictor variables were income, education level, marital status, mother’s age, child’s age, and number of children aged < 5 years. In the adjusted model, we added covariates (clusters and study arms). The full analysis code is available at the Open Science Framework (https://osf.io/yfxjc).
Ethics approval and consent to participate
Permission to use these datasets was granted by the African Population and Health Research Centre (APHRC). The APHRC obtained ethical approval from the Institutional Review Boards (IRBs) of Kenya and Zambia to conduct these studies at the three study sites. Written informed consent was obtained from the study participants before data were collected. For respondents who could neither read nor write, a thumbprint was used as a signature in the presence of a witness. Consent was obtained at every round of data collection. Consent documents and the questionnaire were translated into Kiswahili (Kenya urban study site), Dholuo (Kenya rural study site), and Nyanja and Tonga (Zambia rural study site). Confidentiality of the data and the participants’ privacy were always observed during and after data collection. These rural and urban studies were registered under the trial registration numbers PACTR20180774832663 and PACTR201905787868050, respectively. All methods were performed in accordance with the relevant guidelines and regulations of the Declaration of Helsinki. For example, respect for individuals, the right to make informed decisions, and the recognition of vulnerable groups.
Informed consent process
The data collectors sought informed consent from all study participants before they were interviewed. For those who were not able to read, the information sheet was read to them in their local language, and they were asked to provide a thumbprint to signify their consent. Ethical research committees in both countries approved the use of a thumbprint or signature. The ethical research committees in both countries approved the use of a thumbprint or signature (Amref Health Africa’s Ethics and Scientific Review Committee in Kenya and the ERES Converge in Zambia).
Patient and public involvement
To design and implement this study, national and regional stakeholders from the Ministry of Health and Education were involved as part of the study team. Data collectors were also recruited from the study community. Stakeholders participated in the selection of the study site based on health indicators.
Results
Descriptive statistics
Descriptive statistics for sociodemographic characteristics are provided in Table 2. Mothers had a mean age of approximately 27 years in the two rural populations, whereas the urban population had a slightly higher mean age of approximately 29 years. More than 70% of the mothers reported that they had a marital relationship. Notably, most mothers reported that their educational level was secondary school or lower. Regarding their monthly incomes, most participants from the urban population reported a higher income (above USD 100) than the participants in the rural study sites. Slightly more than 60% of the participants reported that they had one child less than 5 years of age.
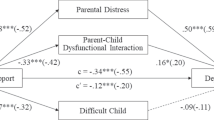
The mean PSS were higher at Kenya’s urban study site than at the two rural study sites (Kenya rural: 37.6 [SD = 11.8], Kenya urban: 48.4 [SD = 4.2], and Zambia rural: 43.0 [SD = 9.1]), as shown in Fig. 2. Notably, in the Kenya rural study site, children’s mean age (in years) at preintervention was 0.8 (SD = 0.7) in the Kenyan rural site, while in the Zambia rural study site, children’s mean age at preintervention was 0.9 (SD = 0.6) in the Zambia site and 3.4 (SD = 0.4) in the urban Kenyan population.
Modelling results on sociodemographic predictors of PSS
We also sought to establish associations between household income, educational level, marital status, maternal age, child age, number of children under five years of age, and mothers’ PSS.
The results of the unadjusted linear regressions showed that in Kenya’s rural study site, the mean PSS of mothers with an income above USD 50 was 0.428 standard deviations lower than that of mothers with a monthly income of less than USD 50 (β = − 0.428 [95% CI − 1.483, − 0.518], p < 0.01***). A similar trend was observed at Kenya’s urban study site, with a standard deviation of 0.341 (β = − 0.341 [95% CI − 1.638, − 0.221], p = 0.01*).
When adjusted for clustering and study arm, the results from Kenyan rural sites showed that the mean PSS of mothers with income above USD 50 was 0.403 standard deviation lower than that of mothers with a monthly income less than USD 50 (β = − 0.403 [95% CI − 1.422, − 0.455], p < 0.01***). A similar trend was observed in Kenya's urban study site, with a standard deviation of 0.325 (β = − 0.325 [95% CI − 1.598, − 0.174], p = 0.02*), as shown in Tables 3, 4, and 5. Notably, the income category ‘above USD 100’ was excluded from Kenyan rural study site modelling, as no participants were in this category. Similarly, the above secondary education was excluded from the Zambia rural study site model for the same reason.
The results from the unadjusted linear regressions showed that, in Kenya’s rural study site, the mean PSS of mothers with secondary education was 0.26 a standard deviation lower than that of mothers with primary education (β = − 0.262 [95% CI − 0.866, − 0.187], p = 0.01**). The findings from Kenya’s urban and Zambia’s rural sites showed no association between education and parental stress (Kenya’s urban study site: β = − 0.147 [95% CI − 0.622, 0.014], p = 0.06; Zambia rural: β = − 0.63 [95% CI − 0.122, 0.378], p = 0.3).
When adjusted for clustering and study arm, the results from Kenyan rural sites showed that the mean PSS of mothers with secondary education was 0.25 a standard deviation lower than that of mothers with primary education (β = − 0.250 [95% CI − 0.838, − 0.667], p = 0.01**). The findings from Kenya’s urban and Zambia’s rural sites showed no association between education and parental stress (Kenya’s urban study site: β = − 0.14 [95% CI − 0.607, 0.030], p = 0.07; Zambia rural: β = − 0.042 [95% CI − 0.167, 0.337], p = 0.3). In addition, the findings on other predictors, such as marital status, mother’s age, child age, and number of children aged < 5 years, showed no significant association with PSS across the study sites as shown in Tables 3, 4, and 5.
Discussion
This study aimed to establish predictors of parental stress using baseline datasets from three studies in two African countries (rural Kenya, rural Zambia, and urban Kenya). The results showed that parental stress was associated with at least two factors: the mother’s income and educational level. In addition, the mean PSS were slightly above scores observed in a study in a low-resourced setting in South Africa in which the baseline mean PSS for the treatment group was 33.1 (SD = 8.7) and the control group was 33.4 (SD = 8.2). We speculate that the higher PSS in Kenya and Zambia settings could be attributed to a higher proportion of the population living in low socioeconomic status compared to South Africa. In addition, cultural variations within communities could have influenced parenting practices and, thereby, variation in PSS.
Findings on high PSS, especially in the poor urban population, as observed in this study, could illuminate the challenges encountered by women in combining childcare and work in poor urban settings, as reported in other studies47. Such scores were not reported in rural Zambia and Kenya because of communal childcare practices. That is, the childcare burden is often spread among extended family members, such as grandparents and other relatives48. Mothers can leave their children to their grandparents or other relatives while working and carrying out household chores. However, such practices are uncommon in urban settings, where mothers often take their children to childcare facilities when they go to work. Notably, the quality of such childcare services is often poor, which could cause parents to worry about whether their child is receiving the right services49. Therefore, we speculate that this could be the reason for the higher parental stress at the Kenyan urban study site.
Our findings on the predictors of PSS established that the PSS was associated with the mothers’ income in Kenyan study sites. These findings extend those of other studies that have shown associations between household income and mothers’ PSS50. Such findings were also observed in a study conducted on perceived stress related to COVID-19, in which mothers from low-income households reported more uncertainty about their health than their counterparts with higher incomes51. Notably, these studies have been carried out in other contexts that do not represent sub-Saharan Africa. Although the findings of the current study were not consistent across the study sites, it is notable that the mean difference in PSS was consistent across the study sites. Therefore, these findings highlight the need for maternal health and childcare interventions to reduce parental stress levels by improving household incomes and reducing childcare-related expenditures, such as providing quality and affordable childcare services.
An association between PSS and mothers’ education levels were also observed, though varied across the study sites. These results were similar to another study of sociodemographic predictors of chronic stress in mothers22. To enhance parenting skills and reduce stress, it is suggested that mothers with less formal education could benefit from engaging in parenting programs, which have been shown to positively impact their children’s development52. Therefore, community parenting programs or social groups could assist parents in sharing their parenting challenges and coming up with potential solutions, thereby reducing the stressors that come with parenting. Surprisingly, the number of children aged < 5 years under care was not associated with parental stress at the three study sites. However, similar findings on parental burnout in SSA have been reported in a study conducted in Somalia among women seeking Maternal and Child Health (MCH) services53 and in Uganda among parents of primary school children54. In addition, the findings on marital status, mother's age, and the age of the youngest child were also surprising. Notably, we could not find any study on sociodemographic predictors of parental stress in the SSA context for comparison with our findings. Therefore, future studies could generate further evidence on the specific sociodemographic predictors of PSS among parents in socially deprived settings.
Study limitations
Despite using three study sites that present diverse, disadvantaged populations in SSA, we could not draw a conclusive link between parental stress and mothers’ sociodemographic characteristics. Noting that the population represented in this study was from three distinct studies with different study designs and geographical locations, it might be difficult to separate naturally occurring effects from regional and study-design effects. Another limitation was that the mothers’ sociodemographic characteristics were based on self-reporting, which could have introduced reporting biases. In addition, our study focused on mothers’ parenting stress. Considering the potential contributions of paternal parenting stress to parenting practices and children’s developmental outcomes, future studies could focus on investigating predictors of paternal parenting stress and its effects on parenting practices and children’s developmental outcomes. Therefore, these findings are indicative of the association between mothers’ socio-demographic characteristics and PSS but do not prove causality.
Conclusions and policy implications
This study aimed to determine the predictors of parental stress among mothers in low-resource SSA settings. The findings indicated that parental stress was associated with at least two factors: the mother’s income and educational level. However, PSS was not related to other sociodemographic factors such as marital relationship, age of the child, age of the mother, and number of children aged below five years under their care. If our findings are replicated in the same setting, it will be prudent for interventions to focus on improving maternal mental health through poverty-alleviation-related interventions, such as subsidising childcare services and improving household income in poor urban and rural settings.
Data availability
The datasets used and analysed during the current study are available from the corresponding author upon reasonable request.
References
Abidin, R., Flens, J. R. & Austin, W. G. The parenting stress index. In Forensic Uses of Clinical Assessment Instruments 297–328 (Lawrence Erlbaum Associates Publishers, 2006).
Daundasekara, S. S., Schuler, B. R., Beauchamp, J. E. S. & Hernandez, D. C. The mediating effect of parenting stress and couple relationship quality on the association between material hardship trajectories and maternal mental health status. J. Affect. Disord. 290, 31–39 (2021).
Hamarat, E. et al. Perceived stress and coping resource availability as predictors of life satisfaction in young, middle-aged, and older adults. Exp. Aging Res. 27(2), 181–196 (2001).
Schulz, R. & Sherwood, P. R. Physical and mental health effects of family caregiving. Am. J. Nurs. 108(9), 23–27 (2008).
Deater-Deckard, K. Parenting stress and children’s development: Introduction to the special issue. Infant Child Dev. 14(2), 111–115 (2005).
Guajardo, N. R., Snyder, G. & Petersen, R. Relationships among parenting practices, parental stress, child behaviour, and children’s social-cognitive development. Infant Child Dev. 18(1), 37–60 (2009).
Ice, G. H., Sadruddin, A. F. A., Vagedes, A., Yogo, J. & Juma, E. Stress associated with caregiving: An examination of the stress process model among Kenyan Luo elders. Soc. Sci. Med. 74(12), 2020–2027 (2012).
Riley, M. R., Scaramella, L. V. & McGoron, L. Disentangling the associations between contextual stress, sensitive parenting, and children’s social development. Fam. Relat. 63(2), 287–299 (2014).
Cabrera, N. J., Fagan, J., Wight, V. & Schadler, C. Influence of mother, father, and child risk on parenting and children’s cognitive and social behaviors. Child Dev. 82(6), 1985–2005 (2011).
Oyarzun-Farias, M. L. A., Cova, F. & Bustos Navarrete, C. Parental stress and satisfaction in parents with pre-school and school age children. Front. Psychol. 12, 683117 (2021).
Parkes, A., Sweeting, H. & Wight, D. Parenting stress and parent support among mothers with high and low education. J. Fam. Psychol. 29(6), 907–918 (2015).
Qian, G. Y., Mei, J., Tian, L. & Dou, G. Assessing mothers’ parenting stress: Differences between one- and two-child families in China. Front. Psychol. https://doi.org/10.3389/fpsyg.2020.609715 (2021).
Santiago, C. D., Kaltman, S. & Miranda, J. Poverty and mental health: How do low-income adults and children fare in psychotherapy?. J. Clin. Psychol. 69(2), 115–126 (2013).
Brown, S. M. et al. Parental buffering in the context of poverty: Positive parenting behaviors differentiate young children’s stress reactivity profiles. Dev. Psychopathol. 32(5), 1778–1787 (2020).
Ho, L. L. K. et al. Impact of poverty on parent-child relationships, parental stress, and parenting practices. Front. Public Health 10, 849408 (2022).
Lantz, P. M., House, J. S., Mero, R. P. & Williams, D. R. Stress, life events, and socioeconomic disparities in health: Results from the Americans’ changing lives study. J. Health Soc. Behav. 46(3), 274–288 (2005).
Combs-Orme, T. & Cain, D. S. Poverty and the daily lives of infants. J. Child. Poverty 12(1), 1–20 (2006).
Tang, E., Cheng, R. W. Y. & Fung, W. K. Perceived parental stress in face of kindergarten children’s academic setback: Roles of parents’ goals and education. Eur. J. Psychol. Educ. 36(2), 439–451 (2021).
Nomaguchi, K. M. & Brown, S. L. Parental strains and rewards among mothers: The role of education. J. Marriage Fam. 73(3), 621–636 (2011).
Wu, K., Wang, F., Wang, W. & Li, Y. X. Parents’ education anxiety and children’s academic burnout: The role of parental burnout and family function. Front. Psychol. 12, 764824 (2022).
Okelo, K. et al. Parent and implementer attitudes on gender-equal caregiving in theory and practice: Perspectives on the impact of a community-led parenting empowerment program in rural Kenya and Zambia. BMC Psychol. 10(1), 162 (2022).
Bates, R. A. et al. Sociodemographics and chronic stress in mother–toddler dyads living in poverty. Dev. Psychobiol. 63(6), e22179 (2021).
Wilcox, W. B. et al. Why marriage matters, thirty conclusions from the social sciences. Inst. Am. Values Natl. Marriage Project 2011.
Kiecolt-Glaser, J. K. Marriage, divorce, and the immune system. Am Psychol 73(9), 1098–1108 (2018).
Robles, T. F. Marital quality and health: Implications for marriage in the 21st century. Curr. Dir. Psychol. Sci. 23(6), 427–432 (2014).
Mac Dougall, K., Beyene, Y. & Nachtigall, R. D. ‘Inconvenient biology:’ Advantages and disadvantages of first-time parenting after age 40 using fertilization. Hum. Reprod. 27(4), 1058–1065 (2012).
Jere, M. Adolescent fertility rates in a rural community in north-western Zambia: A retrospective study. Trop. Dr. 48(3), 213–217 (2018).
Kitsao-Wekulo, P. et al. An evaluation of the effectiveness of a community-based parenting empowerment program to improve nurturing care of young children in Kenya and Zambia. Int. J. Clin. Trials 6(3), 122 (2021).
Division UNS. Standard Country or Area Codes for Statistical Use (M49).
Ahun, M. N., Jeong, J., Kieffer, M. P., Mwanyika-Sando, M. & Yousafzai, A. K. Maternal and paternal perspectives on parenting stress in rural Tanzania: A qualitative study. Ssm-Ment. Health 1, 100030 (2021).
Guo, N. et al. Mental health related determinants of parenting stress among urban mothers of young children - Results from a birth-cohort study in Ghana and Cote d’Ivoire. BMC Psychiatry 14, 1–12 (2014).
Kabanda, S. M. et al. Data sharing and data governance in sub-Saharan Africa: Perspectives from researchers and scientists engaged in data-intensive research. S. Afr. J. Sci. 119(56), 1–12 (2023).
Berry, J. O. & Jones, W. H. The parental stress scale - Initial psychometric evidence. J. Soc. Pers. Relat. 12(3), 463–472 (1995).
Murdock, D. E., Munsongo, K. & Nyamor, G. Scaling the moments that matter® early childhood development model: How communities’ monitoring for change contributes to sustainable impact. Front. Public Health 11, 1165991 (2023).
KNBS: Kenya Population and Housing Census Volume I: Population by County and Sub-county (2019).
(CSO) CSO: Zambia. Zambia Demographic and Health Survey 2013–14. Lusaka (2015).
KNBS: Kenya Demographic and Health Survey 2014. In. Edited by Statistics KNBo. https://dhsprogram.com/pubs/pdf/fr308/fr308.pdf (2014).
Beguy, D., Ndugwa, R. & Kabiru, C. W. Entry into motherhood among adolescent girls in two informal settlements in Nairobi, Kenya. J. Biosoc. Sci. 45(6), 721–742 (2013).
Kitsao-Wekulo, P. et al. Development and feasibility testing of a mobile phone application to track children’s developmental progression. PLoS One 16(7), e0254621 (2021).
Hemming, K., Girling, A. J., Sitch, A. J., Marsh, J. & Lilford, R. J. Sample size calculations for cluster randomised controlled trials with a fixed number of clusters. BMC Med. Res. Methodol. 11, 1–11 (2017).
Algarvio, S., Leal, I. & Maroco, J. Parental stress scale: Validation study with a Portuguese population of parents of children from 3 to 10 years old. J. Child Health Care 22(4), 563–576 (2018).
Harding, L., Murray, K., Shakespeare-Finch, J. & Frey, R. Understanding the parental stress scale with a foster carer cohort. Fam. Relat. 69(4), 865–879 (2020).
Leung, C. & Tsang, S. K. M. The Chinese parental stress scale: Psychometric evidence using rasch modeling on clinical and nonclinical samples. J. Pers. Assess. 92(1), 26–34 (2010).
Pontoppidan, M., Nielsen, T. & Kristensen, I. H. Psychometric properties of the Danish Parental Stress Scale: Rasch analysis in a sample of mothers with infants. Plos One 13(11), e0205662 (2018).
Zelman, J. J. & Ferro, M. A. The parental stress scale: Psychometric properties in families of children with chronic health conditions. Fam. Relat. 67(2), 240–252 (2018).
Team RC. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/ (2016).
Clark, S., Kabiru, C. W., Laszlo, S. & Muthuri, S. The impact of childcare on poor urban women’s economic empowerment in Africa. Demography 56(4), 1247–1272 (2019).
Swadener, E. B., Kabiru, M. & Njenga, A. Does the village still raise the child? A collaborative study of changing child-rearing and community mobilization in Kenya. Early Educ. Dev. 8(3), 285–306 (1997).
Nampijja, M., Okelo, K., Wekulo, P. K., Kimani-Murage, E. W. & Elsey, H. Improving the quality of child-care centres through supportive assessment and ‘communities of practice’ in informal settlements in Nairobi: Protocol of a feasibility study. BMJ Open 11(3), e042544 (2021).
Nagy, E. et al. Low socioeconomic status, parental stress, depression, and the buffering role of network social capital in mothers. J. Ment. Health 31(3), 340–347 (2022).
Scrimin, S. et al. Effects of socioeconomic status, parental stress, and family support on children’s physical and emotional health during the COVID-19 pandemic. J. Child Fam. Stud. 31(8), 2215–2228 (2022).
Black, M. M. et al. Early childhood development coming of age: Science through the life course. Lancet 389(10064), 77–90 (2017).
Abshir, J. N. L., Osman, F., Dahir, G. & Dahlberg, A. Parental burnout among Somali mothers: Associations with mental health, perceived social support, and sociodemographic factors. PLOS Glob. Public Health 3(10), e0002501 (2023).
Brathwaite, R. et al. Typology and correlates of parental stress among caregivers of children with DBDs in low-resourced communities in Uganda. PLOS Glob. Public Health 3(8), e0002306 (2023).
Acknowledgements
The financial support from Episcopal Relief & Development and Grand Challenges Canada for the research activities reported here is gratefully acknowledged. The authors of this paper would also like to thank the survey respondents, the Moments That Matter (MTM) program staff, and the various stakeholders who participated in this study. We also gratefully acknowledge the contributions of the data collectors in Kenya and Zambia.
Funding
These three studies in which we used baseline datasets were funded by Episcopal Relief and Development funded this study with grants from the Conrad N. Hilton Foundation, Grand Challenges, Canada. In addition, while writing this manuscript, KO was supported by the Baily Thomas Charitable Fund TRUST/VC/AC/SG/469207686. BA was supported by the Baily Thomas Charitable Fund TRUST/VC/AC/SG/469207686, the European Union’s Horizon 2020 Research and Innovation Programme under the Marie Skłodowska-Curie grant agreement No. 813546, the Data-Driven Innovation, and the UK Economic and Social Research Council (ES/W001519/1). IH was supported by the UK Economic and Social Research Council (ES/W001519/1).
Author information
Authors and Affiliations
Contributions
K.O. Questionnaire development, data collection, manuscript concept, manuscript writing, statistical analysis, discussion, corresponding author. A.L.M. Statistical analysis, theoretical framework, manuscript concept, and manuscript writing. J.K. Statistical analysis, manuscript concept, and manuscript writing. I.H. Statistical analysis and manuscript writing. P.K.-W. Project manager, data collection, questionnaire development, and manuscript writing. S.O. Questionnaire development, data collection, and manuscript writing. E.W. Questionnaire development, data collection, and manuscript writing. B.A. Theoretical framework, manuscript concept, manuscript writing discussion, and overall guidance. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Okelo, K.O., Kitsao-Wekulo, P., Onyango, S. et al. Sociodemographic predictors of parenting stress among mothers in socio-economically deprived settings in rural and urban Kenya and Zambia. Sci Rep 14, 13055 (2024). https://doi.org/10.1038/s41598-024-63980-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-63980-2
- Springer Nature Limited