Abstract
The aim of this study was to evaluate cytotoxicity and genotoxicity of calcium-silicate based sealers and comparing them with a gold standard—an epoxy-based sealant. Two experimental cell lines were used, gingival fibroblasts (hGF) and monocyte/macrophage peripheral blood cell line (SC). The cytotoxicity (XTT assay) and genotoxicity (comet assay) were evaluated both after 24-h and 48-h incubation. Additionally, after 48-h incubation, the cell apoptosis and cell cycle progression was detected. BioRoot Flow induced a significant decrease in hGF cells viability compared to the negative control groups both after 24-h (p < 0.001) and 48-h incubation (p < 0.01). In group with SC cells, after 24-h incubation significant increase in cells viability was detected for AH Plus Bioceramic Sealer in comparison to negative control (p < 0.05). BioRoot Flow and BioRoot RCS can be considered potentially genotoxic for the hGF cells after 48-h incubation (> 20% DNA damage). BioRoot Flow and BioRoot RCS, may have potential genotoxic effects and induce apoptosis in hGF cells which may irritate periapical tissues, resulting in a delayed healing. The findings of the study would be useful in selection of an appropriate sealant for root canal filling without causing cytotoxicity and genotoxicity.
Similar content being viewed by others
Introduction
Root canal filling is one of the most important stages of endodontic treatment. It should be homogeneous and non-resorbable in order to provide fluid-tight seal of canal space, and inhibit bacterial growth1. The root canal filling consists of a core, which is usually gutta-percha (GP), and a sealant2. Root canal sealers binding the core material to the canal walls, obturate the lateral canals and anastomoses, and fill spaces between cones used in the obturation techniques3,4.
There are many root canal sealers available on the market with different chemical compositions and setting reactions. According to their composition they can be classified into five main groups: zinc oxide eugenol (ZOE) based, calcium hydroxide based, glass ionomer-based, resin-based, and bioceramic sealers1.
AH Plus (Dentsply DeTrey, Konstanz, Germany) is a hydrophobic epoxy-resin sealant (resin-based) that exhibits long-term sealing integrity, low dimensional changes and high radiopacity5. It is widely used in dental practice therefore recommended as the gold standard6,7,8. However, some disadvantages of this material should be acknowledged, namely difficulties in connection to gutta-percha9, questionable cementation to the canal walls in the presence of moisture10, potential cytotoxicity and genotoxicity11 and difficulties in removal during retreatment5.
Calcium silicate-based sealers (CSBS, bioceramic) have become popular recently12. Different forms of CSBS were introduced as powder-liquid and premixed products. CBCS during setting hydration reaction release calcium and hydroxyl ions resulting in pH raise (> 12). As a consequence, these materials exhibit a long-lasting antibacterial effect12,13,14. Furthermore, bioceramic sealers may bond to the root canal dentine as a result of hydroxyapatite formation which combines chemically with dentinal tubules15,16. The main disadvantages of CSBS are difficulty in removal (during retreatment), especially at the apical third16, incompatibility with thermal methods17, resorption over time12 and potentially unfavourable interaction with rising solutions e.g. ethylenediaminetetraacetic acid (EDTA)18.
Among the many desirable features of sealants, one is biocompatibility. According to the International Organization for Standardization (ISO) 1942, the biocompatible material used in dentistry does not cause any adverse local or systemic effects when contact with vital tissue, but provides the most beneficial host response19,20. The toxicity of root canal sealers can be related directly to their components such as eugenol, bisphenol A, resin monomers; substances that are released during the setting reaction (e.g., formaldehyde) or after due to their solubility (e.g., calcium hydroxide). Although sealers are designed to remain inside the canal, due to the flow properties they may be unintentionally forced into the periapical tissues through the apical foramen or/and lateral and accessory canals21,22. Sealants in contact with tissue fluids may dissolve, thereby leading to leaching of components from them. The substances formed due to the degradation of sealants may be in long-term contact with periapical tissues and thus induce cytotoxic and genotoxic effects23,24. They can temporarily or permanently enter the bloodstream or come into contact with other tissue fluids, causing irritation, inflammation and possibly delayed healing after endodontic procedures19,25.
While there are many studies on the cytotoxicity of bioceramic sealers, there are only limited studies investigating their genotoxicity6,26,27. Additionally, most studies focused on dental-driven cell lines and thus analysed the local toxicity effect28,29. Hence, the study on the systemic impact of bioceramic sealers by selecting monocyte/macrophage peripheral blood cell line (SC) should be investigated. In particular, research on cytotoxicity and genotoxicity of BioRoot Flow (Septodont, Saint Maur Des Fosses, France) are missing. Thus, the aim of this in vitro study was to evaluate cytotoxicity and genotoxicity of calcium-silicate based sealers and comparing them with an epoxy-based sealant. The null hypothesis was that there would be no difference among the toxicity presented by the tested sealers.
Materials and methods
Root canal sealers
In the present study, five root canal sealers were analysed: one epoxy-resin based (AH Plus) and four calcium-silicate based sealers (TotalFill BC Sealer, AH Plus Bioceramic Sealer, BioRoot Flow and BioRoot RCS) (Table 1). All experiments were approved by the Committee of Ethics of the Medical University of Lodz, Poland (RNN/269/22/KE; 13/12/2022).
Cell lines and elute preparation
All the in vitro analyses were performed using two experimental cell model lines: human gingival fibroblasts (ATCC CRL-2014) (ATCC; Manassas, VA, USA) and monocyte/macrophage peripheral blood cell line—SC (ATCC CRL-9855) (ATCC; Manassas, VA, USA).
Human gingival fibroblasts cell line (hGF-1)
Cell cultures were maintained under standard conditions (37 °C; 5% pCO2; 95% humidity) according to the manufacturer guidelines. Cells were cultured in Dulbecco Modified Eagle Medium (DMEM) with fetal bovine serum (10%) (ATCC; Manassas, VA, USA) and 1% penicillin/streptomycin (P/S) solution (ScienCell Research Laboratories, advertising San Diego, CA, USA). Cells were passaged when the culture reached 90–95% confluency.
Monocyte/macrophage peripheral blood cell line (stem cells; SC)
Cell cultures were maintained under standard conditions (37 °C; 5% pCO2; 95% humidity) according to the manufacturer guidelines. Cells were cultured in Iscove's Modified Dulbecco's Medium (IMDM) with 4-mML-glutamine adjusted to 1.5 g/L sodium bicarbonate (ATCC; Manassas, VA, USA) and supplemented with 0.05 mM 2-mercaptoethanol (Sigma- Aldrich Corp., St. Louis, MO, USA), 0.1 mM hypoxanthine and 0.016 mM thymidine (90%) (ATCC; Manassas, VA, USA), fetal bovine serum (10%) (ATCC; Manassas, VA, USA) and 1% penicillin/streptomycin (P/S) solution (ScienCell Research Laboratories, advertising San Diego, CA, USA). Cells were divided when the culture reached 90–95% maturity.
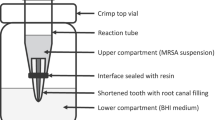
Elute preparation
The sealants were prepared in accordance with the manufacturers’ recommendations. For the cytotoxicity and genotoxicity tests, 1.4 g of each sealant was use and for apoptosis and cycle analysis, 0.7 g were spread on the lower surface of a sterile 50 mL centrifuge tube. After setting time, sealants were covered with 3.5 mL of culture medium and eluted for 24 h in a humidified atmosphere containing 5% CO2. After this time, 5 mL was collected from each tube and filtered to remove particulate matter. These elutes were then diluted tenfold in culture medium to bring it into contact with the cultured cells.
Cytotoxicity analysis
The cytotoxicity of the sealers was measured using a colorimetric, resazurin-based assay kit (Sigma Aldrich Corp., St. Louis, MO, USA). The mechanism is based on the irreversible reduction of resazurin by dehydrogenase enzymes to pink and bright red fluorescent resorufin only in metabolically active cells. The whole experiments were performed in triplicate with similar results. SC and hGF cells were seeded in 96 well plates (8 × 103/well) and after 24 h investigated compounds were added at the appropriate concentrations. Untreated cells cultured in a complete medium were used as a negative control, whereas cells incubated with 100% dimethyl sulfoxide (DMSO) comprised a positive control. Cells were incubated for 24 h and 48 h at 37 °C, respectively. Then, the cell plates were centrifuged and 100 μL of a 10% resazurin solution was added to each well. After 4-h incubation at 37 °C absorbance at 600 nm and a reference wavelength of 690 nm was measured with a Synergy HT spectrophotometer (BioTek, Vermont, VT, USA)30,31.
Genotoxicity assessment
The alkaline version of the comet assay to analyse deoxyribonucleic acid (DNA) damage in specific cells was used for genotoxicity evaluation of the tested materials. Assays were prepared in 12-well plates by adding 5 × 104 cells/well and after 24 h test compounds were added at the appropriate concentrations. Cells preserved in highly toxic 10% DMSO (Sigma-Aldrich Corp., St. Louis, MO, USA) was a positive control, whilst cells suspended in 1 mL of complete culture medium constituted a negative control. The specimens were incubated for 24 h and 48 h. Cells suspended in 0.37% low melting point (LMP) agarose (Sigma-Aldrich Corp., St. Louis, MO, USA) were placed on microscope slides that were previously coated with normal melting point (NMP) agarose (Sigma-Aldrich Corp., St. Louis, MO, USA). Preparations were incubated in lysis buffer at pH 10 (2.5-M NaCl, 10-mM Tris, 100-mM EDTA), containing TritonX-100 (Sigma-Aldrich Corp., St. Louis, MO, USA), at a final concentration of 1% at 4 °C for 60 min. After 1-h incubation, the specimens were incubated in development buffer (300-mM NaOH, 1-mM EDTA) for 20 min at 4 °C and this was followed by electrophoresis (32 mA, 17 V, 20 min) at 4 °C in electrophoretic buffer (30-mMNaOH, 1-mM EDTA). Finally, 4′,6-Diamidino-2-phenylindole (DAPI) was used for staining, and the obtained data were evaluated under a fluorescence microscope by assessing the percentage of DNA in the comet tail30,31.
Apoptosis detection
The fluorescein isothiocyanate FITC Annexin V Apoptosis Detection Kit I (FITC Annexin V Apoptosis Detection Kit I, BD Bioscences, NJ, USA) was used to assess apoptotic cell death. Assays were prepared in 12-well plates by adding 1 × 106 cells/well and after 24 h test compounds were added at the appropriate concentrations and incubated for 48 h. The positive control comprised cells treated for 16 h with 1 μM staurosporine (Sigma-Aldrich Corp., St. Louis, MO, USA), while negative control represented cells incubated for 48 h in complete culture medium. Afterwards, the cells were washed twice with cold phosphate-buffered saline (PBS) (Sigma-Aldrich Corp., St. Louis, MO, USA) and then double-stained with: annexin V (an early apoptosis marker) and propidium iodide (PI) (cell membrane disintegration, necrosis, and late apoptosis marker). CytoFLEX (Beckman Coulter, Brea, CA, USA) was used to calculate the percentage of apoptotic cells by flow cytometry (FC) and the obtained data were analysed using Kaluza Analysis 1.5 A (Beckman Coulter, Brea, CA, USA)30,31.
Cell cycle analysis
The analysis of the cell cycle was performed by FC using PI staining. Assays were prepared in 12-well plates by adding 1 × 106 cells/well and after 24 h tested compounds were added at the appropriate concentrations and incubated for 48 h. The positive control constituted cells treated for 16 h with 1 μM nocodazole (Sigma-Aldrich Corp., St. Louis, MO, USA), whereas cells cultured in a complete medium for 48 h constituted a negative control. Afterwards, cells were washed twice with cold PBS (Sigma-Aldrich Corp., St. Louis, MO, USA) and then preserved with ice-cold 70% ethanol at − 20 °C for 20 min. Before staining with PI solution (10 μg/mL) (Sigma-Aldrich Corp., St. Louis, MO, USA) cells were processed with RNase A DNase & Protease-free (10 mg/mL) (Canvax Biotech, Córdoba, Spain) and incubated at 37 °C for 1 h. The percentage of cells in each phase of the cell cycle was assessed using Kaluza Analysis 1.5A software (Beckman Coulter, Brea, CA, USA). In the DNA content histograms, the x-axis showed the DNA content measured by PI fluorescence, while the y-axis indicated the number of cells30,31.
Statistical analysis
All statistical analyses were evaluated with the statistical software package Statistica 13 (StatSoft, Kraków, Poland). The Shapiro–Wilk test was used to confirm the normality of the data. The Student’s t-test was used for paired normally distributed samples comparison, otherwise the Mann–Whitney rank sum test was performed. All analyses in each experiment were based on the results of three independent tests. Statistically significant differences are presented in the graphs as follows: *p < 0.05; **p < 0.01; ***p < 0.001 compared to negative control.
Results
Analysis of the cytotoxicity of the sealers
The cytotoxicity analysis showed that BioRoot Flow induced a significant decrease in hGF cells viability compared to the negative control groups both after 24-h and 48-h of incubation (Fig. 1A,B) (p < 0.001). Moreover, BioRoot RCS significantly reduced number of vital hGF cells after 48 h (p < 0.01) when compared with negative control.
In group with SC cells, after 24-h incubation the significant increase in cells viability was detected for AH Plus Bioceramic Sealer in comparison with negative control (p < 0.05) (Fig. 2A,B).
Analysis of the genotoxicity of sealers
Considering the hGF cell line, both after 24-h and 48-h statistically significant higher DNA damage compared to the negative control was observed for all sealers except for TotalFill BC Sealer (Fig. 3). In case of the SC cell line, after 24-h incubation, DNA damage compared to the negative control was statistically significantly higher for all sealers except for AH Plus and TotalFill BC Sealer (Fig. 3). With a 48-h incubation time for this line, statistically higher DNA damage was found for all evaluated sealers (Fig. 4) compared to negative control.
Apoptosis detection
After 48-h incubation, BioRoot Flow and BioRoot RCS significantly induced apoptosis in hGF group; ca. 78% and 83% of cells were at the early and late stages of apoptosis, respectively (Fig. 5). Additionally, none of the tested compounds evoked a significant increase in the level of apoptotic and necrotic SC cells (Fig. 6) (p > 0.05).
Analysis of the cell cycle progression
After 48-h incubation, the cell cycle progression of the hGF and SC cells treated with all tested root canal sealers was similar to the cells cultured in the complete medium (p > 0.05) (Figs. 7, 8).
Discussion
Root canal sealers should be biocompatible since they can be in direct contact with the periapical tissues (in case of material extrusion) or indirectly through the products released during the setting reaction32. Therefore, before employment of the material in clinical practice, potential cytotoxicity and genotoxicity should be verified21. In the present study the null hypothesis was rejected, because statistically significant differences in cytotoxicity and genotoxicity were found between tested sealers.
It is worth highlighting that no studies, to date, have evaluated the biocompatibility of endodontic sealers using multiple in vitro tests as presented in this study. Furthermore, two cell lines were used, which provided the assessment of both local and systemic effects of the tested materials. What is more, the results of the study may be helpful in choosing the appropriate material in endodontic treatment.
In the present study, the endodontics sealers were tested after the initial setting of 24 h and 48 h to simulate what happens clinically 1 and 2 days after root canal system obturation. Therefore, the toxicity of the tested materials was related to the components released after hardening or the result of irritation by the substances not reacted during the setting reaction.
Cytotoxicity of root canal sealers
AH Plus was the most widely studied in cytotoxicity assessment, thus in our study was considered as the reference sealer19,33,34,35,36,37,38. In the present study, set AH Plus exhibited above 90% of viable hGF and SC cells after both incubation periods. Thus, it can be regarded as non-cytotoxic, since according to ISO 10993 standards, a sealer is cytotoxic if cell viability is below 70%34,35. This result is in accordance with previous studies39,40,41. In contrast, some studies indicated cytotoxicity of this sealer34,35, especially when freshly mixed (non-hardening)19,36. The release of small amount of formaldehyde or bisphenol-A during setting reaction of the epoxy resin, were indicated as a potential cytotoxic substance in AH Plus composition34,35,37. On the contrary, some studies reported stronger toxicity of the set sealer38,40. The discrepancies between studies may be explained by different experimental conditions including sample preparation, exposure time and cell cultures (2D or 3D). In 3D cell aggregates, there is a stronger interaction between the cells and the matrix when compared to 2D cell culture, thus reduced ability to penetrate the sealant extracts which results in lower cytotoxic effect40. Most studies confirmed that toxicity of this sealant decreased with observation time and might persist even up to 2 weeks19,25,42,43.
Numerous studies suggested that CSBS sealers may present lower cytotoxic potential contrasted to other types of root canal sealers25,44,45,46,47,48. In the case of bioceramic sealants, the cytotoxic effect may be related to the release of substances during the setting and subsequent dissolution of the material (calcium ions)40, the addition of radiopacifiers or thickening agents49, the content of oxides, mainly barium oxide50, and the formation of hydroxyapatite49.
In the present study only the BioRoot Flow can be considered as locally moderately cytotoxic (30–59%), as it significantly reduced only hGF cells viability compared to negative control and the cytotoxic effect increased after 48-h incubation. It should be emphasized that up to date in the literature there have been no studies on BioRoot Flow; presumably the local cytotoxicity of this material may be due to some components such as acrylamide which is a thickener and flocculating agent. Studies confirmed its cytotoxicity against different cell lines (HEK293, A549), which increases with higher concentrations and longer exposure time51,52.
The other tested CSBS sealants met ISO cytotoxicity criterium (> 70% viable cells)34,35. BioRoot RCS was reported as less toxic compared to zinc-oxide materials44,45,47 or resin-based sealer (AH Plus)48,53. Contrary, in the present study this material exhibited higher cytotoxicity than AH Plus against hGF (local cytotoxicity). In addition, one study reported moderate-slight cytotoxicity (57.51%) of BioRoot RCS to NIH 3T3 fibroblasts cells37. Non-cytotoxic effect of TotalFill BC Sealer was confirmed by others which is in accordance with the present results46. Additionally, TotalFill BC Sealer exhibited less cytotoxicity than freshly mixed resin-based sealer (AH Plus)48 and zinc-oxide sealer (Pulp Canal Sealer; Kerr, Romulus, MI, USA)54. In contrast, one study showed higher cytotoxicity of TotalFill BC Sealer when compared to AH Plus (set material)54. Moreover, AH Plus Bioceramic Sealer was reported less cytotoxic compared to AH Plus34,35; however, in the present study both materials exhibited no cytotoxicity (> 90%) against tested cells. In addition, in the group of SC cells after 24 h, AH Plus Bioceramic Sealer significantly increased cell viability (~ 112%), which may indicate the ability of this material to stimulate cell proliferation15. It may be hypothesised that this phenomenon facilitates tissue regeneration.
Genotoxicity of root canal sealers
The genotoxicity tests were carried out to verify the effects of tested material on the genetic material of cells, which may affect their integrity26. Bankoglu et al. reported that DNA damage above 20% negatively affected cell viability, therefore, for in vitro experiments where this level of damage was found, it is recommended to provide cell survival data in parallel55. Accordingly, to this recommendation, in the present study, despite many statistically significant differences between the sealants and the negative control, only BioRoot Flow and BioRoot RCS can be considered potentially genotoxic for the hGF cells after 48-h incubation. It should be mentioned that it is the first study analysing the genotoxicity of BioRoot Flow, so direct comparison of results was not possible. It might be hypothesised that the genotoxicity of BioRoot Flow is caused by a sealer component—acrylamide. This chemical compound can be transformed to a more active metabolite, glycidamide, which increases genotoxicity51,56,57. In addition, research confirmed its effect on genome destabilization (e.g., nuclear condensations, fragmentations)52 and oxidative stress51. In the case of BioRoot RCS, genotoxicity may result from incomplete setting of the material, which is mixed manually. BioRoot RCS in one study showed the lowest genotoxic potential, although the higher concentration of this sealer showed negligible double-strand break formation thus may be considered as potentially genotoxic58.
There was no consensus in the literature regarding the genotoxicity of resin-based materials19,58,59,60. Some studies concluded that AH Plus is significantly more genotoxic than other sealers19,59, while others reported no genotoxicity which was in accordance with present results58,60. The unset epoxy-resin sealants were found to be more genotoxic than set material19. The genotoxicity of AH Plus was associated with the release of resin monomers, which enhance the formation of reactive oxygen species (ROS)61. As a consequence, the level of protective enzymes is disrupted, thus contributing to DNA damage and apoptosis61. Additionally, bisphenol-A and formaldehyde are widely considered as carcinogens and may promote genome instability61,62,63.
Studies investigating genotoxic potential of CSBS present inconclusive results27,58,59,61. Calcium silicate materials were claimed to exhibit the lowest genotoxicity potential when compared with other sealers group61, while others found TotalFill BC Sealer to be genotoxic58, but less than zinc oxide sealant (L929 cells)27 and AH Plus (FMM1 cells)59. Contrary, in our study, TotalFill BC Sealer was not statistically genotoxic for both tested cell lines regardless of the observation time.
Cells apoptosis
After the necrosis cell content is released into the adjacent tissues, that stimulates immune cells to release enzymes and reactive oxygen, sustaining the inflammatory process; thereby causing a delayed healing40,64. In the present study, gingival fibroblast necrosis was mainly induced by BioRoot Flow and BioRoot RCS; ca 78% and 83% of cells were at the early and late stages of apoptosis, respectively. The assay for apoptosis authenticated results obtained in the cytotoxicity and genotoxicity assays. Hence, these results were in disagreement with previous study, in which BioRoot RCS revealed more than 87% of viable cells after exposure65.
In a study evaluating AH Plus, the authors detected 85.45% apoptotic cells in early and late-stage40 which was in contrary with the obtained results in the present study: > 80% of viable cells in both cell lines. In addition, one study showed that the highest cell death was observed at high concentrations of tested calcium silicate-based sealers (MTA Fillapex; Angelus Indústria de Produtos Odontológicos S/A, Londrina, PR, Brazil and TotallFill BC Sealer)46.
Cells progression cycle and models
The cell cycle progression analysis showed not statistically significant changes compared to the negative control in case of the tested sealants. It is worth emphasising there are no studies on the cell cycle available in the literature, therefore a direct comparison of the results was not possible. It should be noted that any discrepancies between our results when compared with other in vitro studies could be related to methodological differences, such as materials setting conditions (whether materials were freshly mixed or set), sealer concentration (dissoluted or not), exposure time, cell type, and cytotoxicity and genotoxicity assays used. Various methods are used to assess the biocompatibility in vitro including cytotoxicity, genotoxicity tests, apoptosis detection and/or cell cycle progression30,31. Most studies apply test of cytotoxicity based on reduction of tetrazolium salts with different cell models with accordance to ISO standard 10993-5: 199921,66. The advantage of these methods include simplicity, speed, precision, and reproducibility27. Moreover, the dental materials may induce genome instability thus comet assay method can be used for the quantitative DNA damage assessment (ISO10993-3). The test is very sensitive and detects the smallest level of DNA damage and requires a short time to perform at minimal cost and a limited number of cells per sample. The apoptosis, necrosis and cell cycle analysis are usually indirectly detected via the flow cytometry (FC)67. This method uses impermeable fluorescent dyes, such as propidium iodide (PI) capable of binding and labelling DNA fragments thereby providing a rapid and precise evaluation67.
In the literature different cell models for cell viability assessment were used including human cells, namely: gingival fibroblasts37,68, dental pulp stem cells69, osteoblasts53,70, periodontal ligament cells43,47 or human osteoblast-like cells (MG63)71, and non-human cells e.g.: L929 mouse fibroblasts71,72 or Chinese hamster fibroblasts (V79)21. In dental materials science, human cell lines derived from oral tissues were preferred for cytotoxicity and genotoxicity evaluation73. Fibroblasts are the main components of connective tissue and the dominant type of periodontal ligament cells that will contact endodontic sealers37. For that reason, immortalized human gingival fibroblasts (hGF) were used in this study because they can be cultured in a small number of passages, resulting in minimal cellular changes due to cell culture manipulation38. Beside the local effect, the assessment of systemic toxicity is very important, which, according to the PN-EN ISO 10993-11: 2018 standard, should be assessed on monocytes/macrophages as a stage of preclinical testing of biological materials, therefore second cell line (SC) was chosen for this experimental study30.
Limitations and future perspective
Some limitations of the present study should be acknowledged. Firstly, the in vitro character of the study makes it impossible to assess the long-term effects occurring in human body. The study does not include some important factors e.g., host defence, which can prevent the toxicity of materials and thus protect against disintegration or disruption of the genome of cells. Further studies should include the development of a model to evaluate root canal sealers using a blood flow system that attenuates the toxic effects of dental materials. In addition, periapical or osteoblast cell lines were not used on this study which can be considered as a limitation and should be further investigated in future studies. Also, less commonly used cells e.g. neuronal cells can be used in the tests and brought in contact with sealants limited to an apical area. With the extensive demand for bioceramic materials, longitudinal and multicentre clinical trials are essential to provide a broader view of their features to clinicians. Moreover, different mixing techniques of investigated materials may also contribute to heterogeneity of findings. In other words, BioRoot RCS demands manual measurement and mixing of product components in contrast to other tested bioceramic sealers that are ready to use. Although this is the first study to evaluate the biocompatibility of BioRoot Flow, more in vitro and in vivo investigations are needed to verify and better understand the current findings. It is recommended that further research be undertaken using both traditional microscopic and spectroscopic techniques. Confocal laser scanning microscopy (CLSM), transmission electron microscopy (TEM) along with scanning electron microscopy (SEM) can help to investigate surface topography and visualise rapid chemical and biochemical properties of bioceramic sealers74. The above-mentioned techniques could be supplemented by atomic force microscopy (AFM), particularly when the surface roughness and nanomechanical properties in natural conditions (i.e. body fluids) should be investigated74. Moreover, spectroscopic methods such as Fourier Transform Infrared Spectroscopy (FT-IR) and X-ray Spectroscopy would help to further analyse these materials75. The former could provide more valuable data on microstructural and surface properties and the setting reactions of bioceramic sealers whereas X-ray Photoelectron Spectroscopy (XPS) and X-ray diffraction (XRD) would give an insight into the elemental compositions and the degree of crystallinity of these materials75.
Nevertheless, the correct choice of endodontic materials including sealers is essential for general health. It must be noted that when they are released from root apex or lateral and accessory canals, the leaching components may induce cytotoxic and genotoxic effects as they can enter the bloodstream. The consequences of such an effect on the infection development or neuronal cells needs to be further investigated.
Conclusions
From this study, the following could be concluded:
-
1.
AH Plus Bioceramic Selaer enhanced the viability of the SC cells after 24-h incubation.
-
2.
BioRoot Flow exhibited moderate cytotoxicity locally.
-
3.
BioRoot Flow and BioRoot RCS exhibited potential genotoxicity for the hGF cells after 48-h incubation.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Reszka, P. et al. A comparative chemical study of calcium silicate-containing and epoxy resin-based root canal sealers. Biomed. Res. Int. 2016, 9808432 (2016).
Kikly, A., Jaâfoura, S., Kammoun, D. & Sahtout, S. Sealing ability of endodontic cements: An in vitro study. Int. J. Dent. 2020, 5862598 (2020).
Palanivelu, C. R. et al. An in vitro comparative evaluation of distribution of three different sealers by single-cone obturation technique. J. Pharm. Bioallied Sci. 11, S438–S441 (2019).
Primus, C. M., Tay, F. R. & Niu, L.-N. Bioactive tri/dicalcium silicate cements for treatment of pulpal and periapical tissues. Acta Biomater. 96, 35–54 (2019).
Borges, Á. H. et al. Physicochemical properties and surfaces morphologies evaluation of MTA FillApex and AH plus. Sci. World J. 2014, 589732 (2014).
Erdogan, H., Yildirim, S. & Cobankara, F. K. Cytotoxicity and genotoxicity of salicylate- and calcium silicate-based root canal sealers on primer human periodontal ligament fibroblasts. Aust. Endod. J. 47, 645–653 (2021).
Silva, E. J. N. L., Cardoso, M. L., Rodrigues, J. P., De-Deus, G. & Fidalgo, T. K. D. S. Solubility of bioceramic- and epoxy resin-based root canal sealers: A systematic review and meta-analysis. Aust. Endod. J. 47, 690–702 (2021).
Garrido, A. D. B. et al. Laboratory evaluation of the physicochemical properties of a new root canal sealer based on Copaifera multijuga oil-resin. Int. Endod. J. 43, 283–291 (2010).
Eldeniz, A. U. & Ørstavik, D. A laboratory assessment of coronal bacterial leakage in root canals filled with new and conventional sealers. Int. Endod. J. 42, 303–312 (2009).
Roggendorf, M. J., Ebert, J., Petschelt, A. & Frankenberger, R. Influence of moisture on the apical seal of root canal fillings with five different types of sealer. J. Endod. 33, 31–33 (2007).
Najafzadeh, R., Fazlyab, M. & Esnaashari, E. Comparison of bioceramic and epoxy resin sealers in terms of marginal adaptation and tubular penetration depth with different obturation techniques in premolar teeth: A scanning electron microscope and confocal laser scanning microscopy study. J. Fam. Med. Prim. Care 11, 1794 (2022).
Radwanski, M. et al. A micro-CT analysis of initial and long-term pores volume and porosity of bioactive endodontic sealers. Biomedicines 10, 2403 (2022).
Zavattini, A., Knight, A., Foschi, F. & Mannocci, F. Outcome of root canal treatments using a new calcium silicate root canal sealer: A non-randomized clinical trial. J. Clin. Med. 9, 782 (2020).
Chopra, V., Davis, G. & Baysan, A. Physico-chemical properties of calcium-silicate vs. resin based sealers—A systematic review and meta-analysis of laboratory-based studies. Materials (Basel, Switzerland) 15, 229 (2021).
Kharouf, N. et al. Physicochemical and mechanical properties of premixed calcium silicate and resin sealers. J. Funct. Biomater. https://doi.org/10.3390/jfb14010009 (2023).
Farrayeh, A. et al. Effectiveness of two endodontic instruments in calcium silicate-based sealer retreatment. Bioengineering (Basel, Switzerland) 10, 362 (2023).
Oliveira, D. S. et al. Suboptimal push-out bond strengths of calcium silicate-based sealers. Int. Endod. J. 49, 796–801 (2016).
Asawaworarit, W., Pinyosopon, T. & Kijsamanmith, K. Comparison of apical sealing ability of bioceramic sealer and epoxy resin-based sealer using the fluid filtration technique and scanning electron microscopy. J. Dent. Sci. 15, 186–192 (2020).
Kim, M. et al. Cytotoxicity and genotoxicity of epoxy resin-based root canal sealers before and after setting procedures. Life 12, 1–10 (2022).
Williams, D. F. On the mechanisms of biocompatibility. Biomaterials 29, 2941–2953 (2008).
Fonseca, D. A. et al. Biocompatibility of root canal sealers: A systematic review of in vitro and in vivo studies. Materials (Basel). 12, 1–34 (2019).
Özdemir, O. & Kopac, T. Cytotoxicity and biocompatibility of root canal sealers: A review on recent studies. J. Appl. Biomater. Funct. Mater. 20, 22808000221076324 (2022).
Camilleri, J., Atmeh, A., Li, X. & Meschi, N. Present status and future directions: Hydraulic materials for endodontic use. Int. Endod. J. 55, 710–777 (2022).
Elyassi, Y., Moinzadeh, A. & Kleverlaan, C. Characterization of leachates from 6 root canal sealers. J. Endod. 45, 623–627 (2019).
Giacomino, C. M., Wealleans, J. A., Kuhn, N. & Diogenes, A. Comparative biocompatibility and osteogenic potential of two bioceramic sealers. J. Endod. 45, 51–56 (2019).
Só, B. B. et al. Genotoxicity and cytotoxicity comparison of calcium silicate-based and resin-based sealers on human periodontal ligament stem cells. Eur. Endod. J. 7, 129–134 (2022).
Nair, A. V. et al. Comparative evaluation of cytotoxicity and genotoxicity of two bioceramic sealers on fibroblast cell line: An in vitro study. J. Contemp. Dent. Pract. 19, 656–661 (2018).
Sanz, J. L. et al. Microstructural composition, ion release, and bioactive potential of new premixed calcium silicate-based endodontic sealers indicated for warm vertical compaction technique. Clin. Oral Investig. 25, 1451–1462 (2021).
Sanz, J. L. et al. Cytocompatibility and bioactive potential of AH plus bioceramic sealer: An in vitro study. Int. Endod. J. 55, 1066–1080 (2022).
Kunert, M. et al. The cytotoxicity and genotoxicity of bioactive dental materials. Cells 11, 3238 (2022).
Wawrzynkiewicz, A. et al. The cytotoxicity and genotoxicity of three dental universal adhesives—An in vitro study. Int. J. Mol. Sci. 21, 3950 (2020).
Kapralos, V. et al. On the biocompatibility of endodontic sealers. Swiss Dent. J. 132, 586–597 (2022).
Lyu, W.-J., Bai, W., Wang, X.-Y. & Liang, Y.-H. Physicochemical properties of a novel bioceramic silicone-based root canal sealer. J. Dent. Sci. 17, 831–835 (2022).
de Souza, L. C., Neves, G. S. T., Kirkpatrick, T., Letra, A. & Silva, R. Physicochemical and biological properties of AH plus bioceramic. J. Endod. 49, 69–76 (2023).
Mann, A. et al. Evaluation of the physicochemical and biological properties of EndoSequence BC Sealer HiFlow. J. Endod. 48, 123–131 (2022).
Lee, B.-N. et al. Anti-inflammatory and osteogenic effects of calcium silicate-based root canal sealers. J. Endod. 45, 73–78 (2019).
Tolosa-Monfà, A., Veroni, A., Blasi-Cabús, J., Ballester-Palacios, M.-L. & Berástegui-Jimeno, E. Cytotoxicity comparison of Bio C Sealer against multiple root canal sealers. J. Clin. Exp. Dent. 15, e110–e117 (2023).
Poggio, C., Riva, P., Chiesa, M., Colombo, M. & Pietrocola, G. Comparative cytotoxicity evaluation of eight root canal sealers. J. Clin. Exp. Dent. 9, e574–e578 (2017).
da Silva, E. J. N. L., Zaia, A. A. & Peters, O. A. Cytocompatibility of calcium silicate-based sealers in a three-dimensional cell culture model. Clin. Oral Investig. 21, 1531–1536 (2017).
Szczurko, G. et al. Effect of root canal sealers on human periodontal ligament fibroblast viability: Ex vivo study. Odontology 106, 245–256 (2018).
Al-Hiyasat, A. S., Tayyar, M. & Darmani, H. Cytotoxicity evaluation of various resin based root canal sealers. Int. Endod. J. 43, 148–153 (2010).
Silva, E. J. N. L. et al. Evaluation of cytotoxicity and physicochemical properties of calcium silicate-based endodontic sealer MTA Fillapex. J. Endod. 39, 274–277 (2013).
Jung, S. et al. Evaluation of the biocompatibility of root canal sealers on human periodontal ligament cells ex vivo. Odontology 107, 54–63 (2019).
Camps, J., Jeanneau, C., El Ayachi, I., Laurent, P. & About, I. Bioactivity of a calcium silicate–based endodontic cement (BioRoot RCS): Interactions with human periodontal ligament cells in vitro. J. Endod. 41, 1469–1473 (2015).
Dimitrova-Nakov, S. et al. In vitro bioactivity of Bioroot™ RCS, via A4 mouse pulpal stem cells. Dent. Mater. 31, 1290–1297 (2015).
Zhou, H. et al. In vitro cytotoxicity of calcium silicate-containing endodontic sealers. J. Endod. 41, 56–61 (2015).
Jeanneau, C., Giraud, T., Laurent, P. & About, I. BioRoot RCS extracts modulate the early mechanisms of periodontal inflammation and regeneration. J. Endod. 45, 1016–1023 (2019).
Alsubait, S. A. et al. Cytotoxicity of different concentrations of three root canal sealers on human mesenchymal stem cells. Biomolecules 8, 68 (2018).
Janini, A. C. P. et al. In vitro evaluation of cytotoxicity in human osteoblastic cells and antimicrobial activity in the biofilm of different root canal sealers. Res. Soc. Dev. 11, e430111032842 (2022).
Shokrzadeh, M., Motafeghi, F. S., Lotfizadeh, A., Ghorbani, M. & Haddadi Kohsar, A. Cytotoxicity and mineralization activity of calcium silicate-based root canal sealers compared to conventional resin-based sealer in human gingival fibroblast cells. Int. J. Dent. 2023, 4376579 (2023).
Celik, F. S., Cora, T. & Yigin, A. K. Investigation of genotoxic and cytotoxic effects of acrylamide in HEK293 cell line. J. Cancer Prev. Curr. Res. 9, 260–264 (2018).
Kacar, S., Vejselova, D., Kutlu, H. M. & Sahinturk, V. Acrylamide-derived cytotoxic, anti-proliferative, and apoptotic effects on A549 cells. Hum. Exp. Toxicol. 37, 468–474 (2018).
Jung, S. et al. Cytotoxic effects of four different root canal sealers on human osteoblasts. PLoS One 13, e0194467 (2018).
Loushine, B. A. et al. Setting properties and cytotoxicity evaluation of a premixed bioceramic root canal sealer. J. Endod. 37, 673–677 (2011).
Bankoglu, E. E., Schuele, C. & Stopper, H. Cell survival after DNA damage in the comet assay. Arch. Toxicol. 95, 3803–3813 (2021).
Mucci, L. A. & Wilson, K. M. Acrylamide intake through diet and human cancer risk. J. Agric. Food Chem. 56, 6013–6019 (2008).
Bandarra, S. et al. Mechanistic insights into the cytotoxicity and genotoxicity induced by glycidamide in human mammary cells. Mutagenesis 28, 721–729 (2013).
Eldeniz, A. U., Shehata, M., Högg, C. & Reichl, F. X. DNA double-strand breaks caused by new and contemporary endodontic sealers. Int. Endod. J. 49, 1141–1151 (2016).
Candeiro, G. T. M. et al. Cytotoxicity, genotoxicity and antibacterial effectiveness of a bioceramic endodontic sealer. Int. Endod. J. 49, 858–864 (2016).
Martinho, F. C. et al. Comparison of cytotoxicity, genotoxicity and immunological inflammatory biomarker activity of several endodontic sealers against immortalized human pulp cells. Int. Endod. J. 51, 41–57 (2018).
Dos Santos Costa, F. M., Fernandes, M. H. & Batistuzzo de Medeiros, S. R. Genotoxicity of root canal sealers: A literature review. Clin. Oral Investig. 24, 3347–3362 (2020).
Gupta, S. K., Saxena, P., Pant, V. A. & Pant, A. B. Release and toxicity of dental resin composite. Toxicol. Int. 19, 225–234 (2012).
Schweikl, H., Spagnuolo, G. & Schmalz, G. Genetic and cellular toxicology of dental resin monomers. J. Dent. Res. 85, 870–877 (2006).
Pawinska, M., Szczurko, G., Luczaj-Cepowicz, E., Marczuk-Kolada, G. & Holownia, A. Cytotoxicity and oxidative stress induction by root canal sealers in human periodontal ligament fibroblasts: An in vitro study, Iran. Endod. J. 16, 164–175 (2021).
Collado-González, M. et al. Biocompatibility of three new calcium silicate-based endodontic sealers on human periodontal ligament stem cells. Int. Endod. J. 50, 875–884 (2017).
Dhopavkar, V. V. et al. Comparative evaluation of cytotoxic and genotoxic effects of three resin-based sealers by 3, (4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay and comet assay—An in vitro study. Contemp. Clin. Dent. 12, 376 (2021).
Hu, X.-M. et al. Guidelines for regulated cell death assays: A systematic summary, a categorical comparison, a prospective. Front. cell Dev. Biol. 9, 634690 (2021).
Teixeira, A. B. V. et al. Cytotoxic and genotoxic effects in human gingival fibroblast and ions release of endodontic sealers incorporated with nanostructured silver vanadate. J. Biomed. Mater. Res. B. Appl. Biomater. 109, 1380–1388 (2021).
Victoria-Escandell, A. et al. Cellular responses in human dental pulp stem cells treated with three endodontic materials. Stem Cells Int. 2017, 8920356 (2017).
Suciu, I. et al. Biocompatibility testing on cell culture of some root canal sealers used in endodontics. Rom. Biotechnol. Lett. 21, 11543–11549 (2016).
Jiang, Y., Zheng, Q., Zhou, X., Gao, Y. & Huang, D. A comparative study on root canal repair materials: A cytocompatibility assessment in L929 and MG63 cells. Sci. World J. 2014, 463826 (2014).
Benetti, F. et al. Cytotoxicity and biocompatibility of a new bioceramic endodontic sealer containing calcium hydroxide. Braz. Oral Res. 33, e042 (2019).
Illeperuma, R. P. et al. Immortalized gingival fibroblasts as a cytotoxicity test model for dental materials. J. Mater. Sci. Mater. Med. 23, 753–762 (2012).
Nawrocka, A. et al. Traditional microscopic techniques employed in dental adhesion research-applications and protocols of specimen preparation. Biosensors 11, 408 (2021).
Kaczmarek, K., Leniart, A., Lapinska, B., Skrzypek, S. & Lukomska-Szymanska, M. Selected spectroscopic techniques for surface analysis of dental materials: A narrative review. Materials (Basel) 14, 2624 (2021).
Acknowledgements
This research was funded by Grant No. 503/2-148-04/503-21-001 from the Medical University of Lodz.
Author information
Authors and Affiliations
Contributions
Conceptualization: M.L.S., M.R.; methodology: I.M., W.R.K., G.G. and M.R.; formal analysis: M.L.S. and M.R.; investigation: M.R., W.R.K., G.G.; writing—original draft preparation: M.R., W.R.K., G.G., N.S.; writing—review and editing: M.L.S. and M.Ö.; visualization: G.G. and M.R.; supervision: M.L.S. and M.R.; project administration: M.L.S. and M.R.; funding acquisition: M.L.S., M.R., J.S.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Radwanski, M., Rozpedek-Kaminska, W., Galita, G. et al. Cytotoxicity and genotoxicity of bioceramic root canal sealers compared to conventional resin-based sealer. Sci Rep 14, 4124 (2024). https://doi.org/10.1038/s41598-024-54726-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-54726-1
- Springer Nature Limited