Abstract
The correlation between body mass index (BMI) and the development of cough, shortness of breath, and dyspnea is unclear. Therefore, this study aimed to investigate the association between these parameters. Data from individuals who participated in the National Health and Nutrition Examination Survey between 2003 and 2012 were analyzed. Weighted logistic regression analysis and smoothed curve fitting were used to examine the correlation between BMI and respiratory symptoms. In addition, the relationship between BMI, chronic obstructive pulmonary disease (COPD), and bronchial asthma was examined. Stratified analysis was used to discover inflection points and specific groups. Weighted logistic regression and smoothed curve fitting revealed a U-shaped relationship between BMI and respiratory symptoms. The U-shaped relationship in BMI was also observed in patients with bronchial asthma and COPD. Stratified analysis showed that the correlation between BMI and wheezing and dyspnea was influenced by race. In addition, non-Hispanic black individuals had a higher risk of developing cough than individuals of the other three races [OR 1.040 (1.021, 1.060), p < 0.0001], and they also exhibited an inverted U-shaped relationship between BMI and bronchial asthma. However, the association of BMI with cough, wheezing, dyspnea, COPD, and asthma was not affected by sex. High or low BMI was associated with cough, shortness of breath, and dyspnea, and has been linked to bronchial asthma and COPD. These findings provide new insights into the management of respiratory symptoms and respiratory diseases.
Similar content being viewed by others
Introduction
Respiratory diseases are major contributors to global morbidity and mortality, and respiratory symptoms such as cough, wheezing and exertional dyspnoea are recognisable to patients and may be markers of underlying chronic disease and mortality risk, as well as typical symptoms of chronic obstructive pulmonary disease (COPD) and asthma, which have a serious impact on physical and mental health. Furthermore, the prevalence of asthma has continued to rise over the past three decades1. Notably, more than half of the world's population has symptoms associated with one or more respiratory diseases2,3,4. In the general population, respiratory symptoms are an important prognostic indicator of all-cause mortality in people aged 45–75 years5. Respiratory symptoms and diseases have a profound impact on an individual's health and quality of life.
Body mass index (BMI) is a widely accepted metric for assessing the degree of obesity and overall health of an individual6. Weight and height values are used to calculate a relatively objective parameter, the range of which is used as a measure of body weight7. The World Health Organization (WHO) has identified a BMI range of 18.5‒24.9 kg/m2 as the generally accepted ideal or healthy weight range8. However, obesity was defined as a BMI greater than 30 kg/m29. BMI is an affordable and easily obtainable metric widely used in clinical settings. Many patients with obesity have respiratory symptoms and diseases. A meta-analysis found a correlation between obesity and asthma and that asthma risk increases with increasing BMI10. Furthermore, obesity reportedly leads to increased chronic inflammation in the body11,12. The mechanical effects of obesity result in the narrowing of the airway, which increases respiratory resistance and often manifests as dyspnea and wheezing. However, the “obesity paradox” cannot be ignored13. There are relatively few studies on the effect of low body mass index on respiratory symptoms, but some studies have shown that, as the degree of airway obstruction in COPD patients continues to worsen, COPD patients can lead to an increase in respiratory muscle oxygen consumption and work due to the decrease in lung compliance and increase in respiratory resistance, which can trigger symptoms such as dyspnoea and shortness of breath, leading to gastrointestinal dysfunction, feeding difficulties, etc., and then malnutrition, which can lead to atrophy of respiratory muscles, endurance and contraction are reduced, which can further aggravate the gas trap and airway obstruction, and the decline of pulmonary function in patients with COPD14.
Despite the impact of both obesity and wasting on lung health, there is limited research on the correlation between body mass index (BMI) and respiratory symptoms (cough, wheeze, and dyspnea) in the general US population. With this in mind, our study aimed to explore the relationship between BMI and respiratory symptoms (cough, wheeze, and dyspnoea) using a nationally representative sample from the National Health and Nutrition Examination Survey (NHANES), and to further investigate the correlation between chronic lung diseases (asthma, COPD), which are typified by respiratory symptoms, and depression (including modifiable factors).
Materials and methods
Study population
The National Health and Nutrition Examination Survey (NHANES) is a population-based national cross-sectional survey published by the NCHS15. The data collection methods used in this study were approved by the National Center for Health Statistics (NCHS) Ethics Review Board, and written consent was obtained from each participant. Details on Institutional Review Boards of the NCHS are available at (http://www.cdc.gov/nchs/nhanes/irba98.htm). The absence of ethical review was justified by the fact that all data used in the study were publicly accessible and fully anonymized.
The NHANES adopted a complex multistage probability sampling design16 to select participants representative of the civilian, non-institutionalized US population. Moreover, the survey is designed to collect information on the health and nutrition of the US household population. Data on the participants’ health, socioeconomic status, and other factors were collected through family interviews. Participants underwent a physical examination at mobile exam centers, which were designed to collect data from physical and laboratory examinations.
NHANES data from 2003 to 2012 were used in the study. A total of 61,951 individuals participated in NHANES in 2003‒2012. Participants aged < 40 years (n = 40,347) with incomplete respiratory symptom surveys (n = 3542), incomplete BMI data (n = 1104), and missing covariates (n = 4239) were excluded. Data on poverty-income ratio, marital status, educational attainment, and co-morbidities were included. The study involved 12,719 participants (Fig. 1). The study was conducted in compliance with the RECORD reporting guidelines.
BMI
Trained health technicians collected BMI data at mobile exam centers and retrieved body measurements from the physical examination module. BMI was calculated as weight (kg)/[height (m)2].
Respiratory symptoms
Coughing was verified with a “yes” answer to the question: “Do you usually cough on most days for 3 consecutive months or more during the year?”.
Wheezing and dyspnea were verified with a “yes” answer to the question: “In the past 12 months, have you had wheezing or whistling in your chest?” and “Do you experience shortness of breath when traveling quickly on level ground or up small inclines?”.
COPD is defined as a diagnosis of “chronic bronchitis or emphysema.” Asthma was verified with a “yes” answer to the question: “Has a doctor or other health professional ever told you that you have asthma?”.
Study covariates
To mitigate possible bias, we included demographic factors such as age, sex (male/female), race (Mexican–American, non-Hispanic black, non-Hispanic white, other), educational achievement (< high school, high school, college), marital status (divorced/separated/widowed, married/living with a partner, unmarried), household ratio of income to poverty (PIR) (< 1.3, 1.3‒3.5, > 3.5), and smoking status, with intensity measured by the number of cigarettes smoked. Smoking was categorized into three groups: never smoked (smoked less than 100-lifetime cigarettes), former smoker (smoked more than 100-lifetime cigarettes but quit), and current smoker.
Statistical analysis
All data processing and statistical analysis were performed using R (version 4.2.3) and EmpowerStats software (http://www.EmpowerStats.net). Adjustments were made based on mobile exam center weighting to avoid bias in evaluation. Since underweight (BMI < 18.5 kg/m2) participants were only 1.2% of the sample size, we categorised all subjects based on quartiles. To compare differences between groups, weighted χ2 tests were used for categorical variables, and weighted linear regression models were used for continuous variables. Three weighted multiple logistic regression models were used to evaluate the relationship between BMI and respiratory symptoms, COPD, and asthma. The significance of weighting is mainly to make the sample better reflect the overall characteristics. The data in NHANES is a stratified equal probability random sample, and the totality represented by each stratum is different, so weighting is required.
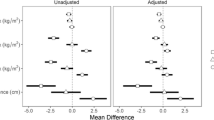
Three models were developed in the study. Model 1 did not account for potential confounding variables. Model 2 adjusted for age, sex, and race. Model 3 adjusted for age, sex, race, marital status, PIR, educational attainment, and smoking. Smoothed curve fitting was used to investigate the possible nonlinear relationships between exposure and outcomes (Fig. 2). If a nonlinear correlation was found, a segmented linear regression model was used to calculate the threshold effect of BMI on respiratory disease based on a smoothing curve. The model was then tested by sex (male, female) and race/ethnicity (non-Hispanic white, Mexican–American, non-Hispanic black, other), and their interaction was also evaluated. Differences with p < 0.05 were considered statistically significant.
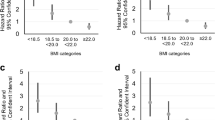
Relationship between BMI and incidence of respiratory symptoms, asthma, and COPD after adjusting for sex, age, race, marital status, PIR, smoking, and education. Panel (A) shows the relationship between BMI and the incidence of cough, panel (B) shows the relationship between BMI and the incidence of dyspnoea, panel (C) shows the relationship between BMI and the incidence of asthma, panel (D) shows the relationship between BMI and the incidence of wheezing, and panel (E) shows the relationship between BMI and the incidence of chronic obstructive pulmonary disease.
Ethical approval
The data collection methods used in this study were approved by the National Center for Health Statistics (NCHS) Ethics Review Board, and written consent was obtained from each participant. Details on Institutional Review Boards of the NCHS are available at (http://www.cdc.gov/nchs/nhanes/irba98.htm). The absence of ethical review was justified by the fact that all data used in the study were publicly accessible and fully anonymized.
Results
Baseline characteristics of individuals categorized by BMI quartiles are presented in Table 1. Overall, 12,719 participants were included in the study. Of these, 3180 participants had a BMI range of 13.2‒24.9 kg/m2, 3175 had a BMI range of 24.9‒28.4 kg/m2, 3180 had a BMI range of 28.4‒32.5 kg/m2, and 3184 had a BMI range of 32.5‒82 kg/m2. Most participants were female (51%) and non-Hispanic white (53.3%), and the prevalence of cough, wheezing, and dyspnea was 11.6%, 10.8%, and 28.2%, respectively. Participants in the lowest BMI quartile (Q1) had higher educational attainment and wealth and comprised a higher proportion of other races than those in the highest BMI quartile (Q4). Table 1 presents the weighted baseline characteristics of applicable participants categorized by BMI quartile. Among the parameters evaluated, smoking was more pronounced in the Q1 group, and the prevalence of smoking-related COPD increased progressively with increasing BMI. The prevalence of respiratory symptoms, COPD, and asthma increased progressively with increasing BMI. In addition, significant differences were observed between the BMI quartile groups with respect to age, race, marital status, annual household income, education, smoking, and the presence of respiratory disease (p < 0.05).
Correlation between respiratory symptoms and BMI
Multifactorial logistic regression analysis showed that BMI was positively associated with wheezing and dyspnoea in the unadjusted model [OR 1.053 (1.042, 1.065), OR 1.066 (1.056, 1.076)] (Table 2). These positive correlations persisted after model 3 was corrected for confounders, and all were statistically significant [OR 1.020, 95% CI 1.008–1.031, p = 0.001; OR 1.060, 95% CI 1.049–1.071, p < 0.0001; OR 1.074, 95% CI 1.064–1.084, p < 0.0001]. After converting BMI from a continuous variable to a categorical variable (quartiles), we found that BMI was nonlinearly associated with the risk of respiratory symptoms (Table 2). This nonlinear relationship persisted after correcting for confounders (Table 2). Furthermore, the nonlinear relationship persisted in diseases associated with respiratory symptoms (COPD and asthma). Curve fitting revealed nonlinear and U-shaped correlations (Fig. 2).
Subgroup analysis
Because BMI standards vary across sex and race, we conducted stratified analysis by sex and race/ethnicity. The interaction factor of race in wheezing and dyspnea (Table 3) indicates that the correlation between BMI and wheezing and dyspnea is influenced by race. In addition, non-Hispanic black individuals had a higher risk of cough for every 1 kg/m2 increase in BMI than the other three races [OR 1.040 (1.021, 1.060), p < 0.0001]. However, we did not find an interaction between BMI and respiratory symptoms, COPD, and asthma, implying that their correlation was not affected by gender (Table 4).
Smoothing curve fitting analysis
After adjusting for all covariates (Model 3), smoothing curves were used to visualize the relationship between BMI and respiratory symptoms, COPD, and asthma across races (Fig. 3). The overall smoothing curve indicates a nonlinear relationship between BMI and respiratory symptoms, with inflection points of 25.56 kg/m2, 20.85 kg/m2, and 22.7 kg/m2 (log-likelihood ratio = 0.006; log-likelihood ratio = 0.002; log-likelihood ratio < 0.001). The same U-shaped relationship was found in COPD, with an inflection point of 24.12 kg/m2 (log-likelihood ratio < 0.001) (Fig. 3; Table 5). Some U-shaped relationships were also found when the results were analyzed by race, with non-Hispanic white individuals having an optimal BMI of 22.68 kg/m2 [OR 0.899 (0.847, 0.955), p = 0.0005; OR 1.076 (1.066, 1.086), p < 0.0001] associated with the lowest odd ratio (OR) for dyspnea symptoms, and Mexican–American and non-Hispanic white individuals having optimal BMIs of 26.91 kg/m2 [OR 0.850 (0.742, 0.974) p = 0.0191; OR 1.098 (1.048, 1.149) p < 0.0001) and 22.21 kg/m2 (OR 0.809 (0.744, 0.880) p < 0.0001; OR 1.043 (1.030, 1.056) p < 0.0001] associated with the lowest OR for COPD prevalence, respectively. However, a significant nonlinear relationship was observed between BMI and COPD (log likelihood ratio = 0.046) among non-Hispanic black individuals, the probability of COPD prevalence increased for each BMI unit change (> 24.85 kg/m2) (OR 1.053 (1.033, 1.073) p < 0.0001) (Table 5). In addition, among non-Hispanic black individuals, there was an inverted U-shaped relationship between BMI and bronchial asthma (Fig. 3); however, this relationship was not described in Table 5, which may be related to differences in analysis methods or insufficient sample size.
The relationship between BMI and the incidence of respiratory symptoms, asthma, and COPD after adjusting for sex, age, marital status, income, smoking, and education. Panel (A) shows the relationship between BMI and the incidence of cough, panel (B) shows the relationship between BMI and the incidence of dyspnoea, panel (C) shows the relationship between BMI and the incidence of asthma, panel (D) shows the relationship between BMI and the incidence of wheezing, and panel (E) shows the relationship between BMI and the incidence of COPD.
Discussion
In this cross-sectional study of Americans aged > 40 years, a U-shaped relationship between BMI and respiratory symptoms was observed. A U-shaped relationship between BMI and all-cause mortality, including respiratory diseases, has been reported previously17. Thus, our study supports similar previous findings with a different population sample. According to our findings, a U-shaped correlation exists between BMI and cough, wheezing, and dyspnea. In addition to respiratory symptoms, the association between BMI and asthma and COPD was found to follow a U-shaped pattern. The risk of respiratory symptoms, COPD, and bronchial asthma increased when BMI was less than or greater than the inflection point.
Cough, wheezing, and dyspnea are the most common respiratory symptoms and are common in patients with COPD and asthma. Respiratory symptoms are an important indicator of various respiratory diseases, which increase the risk of death due to pulmonary disease, particularly obstructive pulmonary disease18. The Global Lung Initiative defines wheezing and dyspnea as predictors of poor prognosis in pulmonary dysfunction, and cough is associated with a poor prognosis in COPD19,20. BMI is an accepted indicator of health and obesity, and coughing, wheezing, and shortness of breath are associated with cardiopulmonary disease. Dyspnea and wheezing are common in people with high BMI21,22. BMI ≥ 30 kg/m2 is one of the diagnostic criteria for obesity hypoventilation syndrome, of which dyspnea is a typical clinical symptom. Large fat deposits also alter the mechanical properties of respiration, leading to wheezing23,24. Furthermore, BMI is negatively correlated with blood oxygen levels and significantly affects lung capacity in obese individuals with BMI ≥ 30 kg/m2, even if they do not have cardiopulmonary disease25. Landt et al. found a correlation between BMI and chronic cough, indicating that individuals with obesity are two to three times more likely to develop cough than healthy individuals26.
The U-shaped correlation between BMI and COPD and asthma suggests that high or low BMI can negatively affect the respiratory system. Lambert et al. found that obese patients with COPD have a poor prognosis, including increased dyspnea and activity limitation, which severely affects their quality of life27. Weight loss is often recommended for people with high BMI. However, the obesity paradox states that high BMI sometimes has a differential effect on COPD morbidity and mortality; excessive weight loss can increase COPD mortality28. Thus, whether patients with COPD should be encouraged to lose weight remains unclear.
We stratified analyses by race to examine differences in the effect of BMI on respiratory symptoms between races. Notably, some differences in BMI standards exist between different races; however, no specific numerical classification standards exist. It is generally believed that the body fat rate of black individuals is lower compared to other races. If calculated according to the BMI formula, black individuals may have a higher BMI than the standard values; however, owing to differences in socioeconomic status, the prevalence of obesity in black individuals is also higher29.
Obesity-related health disparities are particularly prevalent among Mexican Americans30. Among US adults aged ≥ 20 years, being overweight or obese is more common among Mexican Americans31. The prevalence of obesity and obesity-related complications is exacerbated in the U.S.-Mexico border region32. Black individuals have higher bone mass and bone density than white individuals, which contributes to the generally higher BMI in black individuals and explains the higher optimal BMI associated with the lowest risk of COPD prevalence among Mexican-Americans and non-Hispanic black individuals compared with white individuals in our study33.
The U-shaped relationship between BMI and respiratory symptoms suggests that attention should not be focused only on those with a high BMI; too low a BMI can also be detrimental to health. Studies have shown that too low a BMI increases the risk of cardiovascular disease, and a phenotype with a BMI of less than 18.5 kg/m2 is associated with an increased risk of all-cause mortality34,35. Low BMI increases the risk of death from respiratory diseases36,37. Individuals with lower BMI are more likely to develop COPD and have lower lung function compared to those with higher BMI38. These results suggest that the risk of small airway obstruction in underweight individuals deserves more attention and that excessive wasting may also affect the prognosis of patients with COPD.
Our study differs from previous studies in that a nationally representative sample that includes potential covariates was used, which makes our findings more generalizable and reliable. Nevertheless, some limitations must be considered in the interpretation of these results. Since the NHANES database is a cross-sectional database, it was impossible to distinguish between cause and effect. Second, despite the statistical techniques used to adjust for confounding variables, the possibility of interference from other confounding factors cannot be completely ruled out (Supplementary Information 1).
Conclusion
We demonstrated that both excessively high and excessively low BMIs are associated with respiratory symptoms, such as cough, asthma, and dyspnea, as well as between asthma and COPD, which exhibit U-shaped relationships. These observations may help us better understand and manage respiratory diseases.
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation. All relevant data are within its Supporting Information files. The datasets used in this study are freely available from the National Health and Nutrition Examination Survey (NHANES). The data can be accessed at: https://www.cdc.gov/nchs/nhanes/index.htm.
References
Voll-Aanerud, M., Eagan, T. M., Wentzel-Larsen, T., Gulsvik, A. & Bakke, P. S. Respiratory symptoms, COPD severity, and health related quality of life in a general population sample. Respir. Med. 102(3), 399–406 (2008).
Stavem, K., Johannessen, A., Nielsen, R. & Gulsvik, A. Respiratory symptoms and respiratory deaths: A multi-cohort study with 45 years observation time. PLoS One 16(11), e0260416 (2021).
Gulsvik, A. Prevalence of respiratory symptoms in the city of Oslo. Scand. J. Respir. Dis. 60(5), 275–285 (1979).
Gulsvik, A., Bakke, P. S., Brøgger, J., Nielsen, R. & Stavem, K. Respiratory symptoms and mortality in four general population cohorts over 45 years. Respir. Med. 170, 106060 (2020).
Voll-Aanerud, M. et al. Respiratory symptoms in adults are related to impaired quality of life, regardless of asthma and COPD: Results from the European community respiratory health survey. Health Qual. Life Outcomes 8, 107. https://doi.org/10.1186/1477-7525-8-107 (2010).
Jin, J. JAMA patient page. Medications for weight loss: Indications and usage. JAMA 313(21), 2196 (2015).
Ikramuddin, S. et al. Effect of reversible intermittent intra-abdominal vagal nerve blockade on morbid obesity: The ReCharge randomized clinical trial. JAMA 312, 915–922 (2014).
Frostad, A., Soyseth, V., Haldorsen, T., Andersen, A. & Gulsvik, A. Respiratory symptoms and 30 year mortality from obstructive lung disease and pneumonia. Thorax 61(11), 951–956 (2006).
Yang, L. & Colditz, G. A. Prevalence of Overweight and Obesity in the United States, 2007–2012. JAMA Intern Med. 175(8), 1412–1413 (2015).
Beuther, D. A. & Sutherland, E. R. Overweight, obesity, and incident asthma: A meta-analysis of prospective epidemiologic studies. Am. J. Respir. Crit. Care Med. 175(7), 661–666 (2007).
Bastard, J. P. et al. Elevated levels of interleukin 6 are reduced in serum and subcutaneous adipose tissue of obese women after weight loss. J. Clin. Endocrinol. Metab. 85(9), 3338–3342 (2000).
Roth, C. L., Kratz, M., Ralston, M. M. & Reinehr, T. Changes in adipose-derived inflammatory cytokines and chemokines after successful lifestyle intervention in obese children. Metabolism 60(4), 445–452 (2011).
Giri Ravindran, S. et al. The obesity paradox in chronic heart disease and chronic obstructive pulmonary disease. Cureus 14(6), e25674 (2022).
Stephenson, H., Roberts, M., Klimkeit, E. & Smith, T. Uncovering undernutrition in chronic obstructive pulmonary disease: Beyond body mass index. Respir. Med. 205, 107026. https://doi.org/10.1016/j.rmed.2022.107026 (2022).
Chen, T. C. et al. National Health and Nutrition Examination Survey: Estimation Procedures, 2011–2014. Vital Health Stat. 2(177), 1–26 (2018).
National Center for Health Statistics. NCHS Research Ethics Review Board (ERB) Approval. 2017 [14/06/2022]; https://www.cdc.gov/nchs/nhanes/irba98.htm.
Bhaskaran, K., Dos-Santos-Silva, I., Leon, D. A., Douglas, I. J. & Smeeth, L. Association of BMI with overall and cause-specific mortality: A population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 6(12), 944–953. https://doi.org/10.1016/S2213-8587(18)30288-2 (2018).
Marcus, B. S., McAvay, G., Gill, T. M. & Vaz Fragoso, C. A. Respiratory symptoms, spirometric respiratory impairment, and respiratory disease in middle-aged and older persons. J. Am. Geriatr. Soc. 63(2), 251–257 (2015).
Celli, B. R. Predictors of mortality in COPD. Respir. Med. 104(6), 773–779 (2010).
Jubber, A. S. Respiratory complications of obesity. Int. J. Clin. Pract. 58(6), 573–580 (2004).
Sutherland, E. R. Linking obesity and asthma. Ann. N. Y. Acad. Sci. 1311, 31–41 (2014).
Littleton, S. W. & Tulaimat, A. The effects of obesity on lung volumes and oxygenation. Respir. Med. 124, 15–20 (2017).
Castro-Añón, O. et al. Obesity-hypoventilation syndrome: Increased risk of death over sleep apnea syndrome. PLoS One 10, 0117808 (2015).
Schachter, L. M. et al. Obesity is a risk for asthma and wheeze but not airway hyperresponsiveness. Thorax 56(1), 4–8 (2001).
Landt, E. M., Çolak, Y., Nordestgaard, B. G., Lange, P. & Dahl, M. Risk and impact of chronic cough in obese individuals from the general population. Thorax 77(3), 223–230 (2022).
Casas-Vara, A. et al. The obesity paradox in elderly patients with heart failure: Analysis of nutritional status. Nutrition 28(6), 616–622 (2012).
Lambert, A. A. et al. Obesity is associated with increased morbidity in moderate to severe COPD. Chest 151, 68–77 (2017).
Kim, E. K. et al. Impact of body mass index change on the prognosis of chronic obstructive pulmonary disease. Respiration 99, 943–953 (2020).
Kumanyika, S. K., Whitt-Glover, M. C. & Haire-Joshu, D. What works for obesity prevention and treatment in black Americans? Research directions. Obes. Rev. 15(Suppl 4), 204–212. https://doi.org/10.1111/obr.12213 (2014).
Dominguez, K. et al. Vital signs: Leading causes of death, prevalence of disease and risk factors, and use of health services among Hispanics in the United States-2009–2013. Morb. Mortal Wkly Rep. 64, 469–478 (2015).
Flegal, K. M. et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 307, 491–497 (2012).
Fisher-Hoch, S. P. et al. Socioeconomic status and prevalence of obesity and diabetes in a Mexican American community, Cameron County, Texas, 2004–2007. Prev. Chron. Dis. 7, A53 (2010).
Barondess, D. A., Nelson, D. A. & Schlaen, S. E. Whole body bone, fat, and lean mass in black and white men. J. Bone Miner. Res. 12(6), 967–971. https://doi.org/10.1359/jbmr.1997.12.6.967 (1997).
Huisman, H. W., Schutte, R., Venter, H. L. & van Rooyen, J. M. Low BMI is inversely associated with arterial stiffness in Africans. Brit. J. Nutr. 113(10), 1621–1627 (2015).
Yates, W. R., Johnson, C., McKee, P. & Cannon-Albright, L. A. Genetic analysis of low BMI phenotype in the Utah Population Database. PLoS One 8(12), e80287 (2013).
Prospective Studies Collaboration et al. Body-mass index and cause-specific mortality in 900,000 adults: Collaborative analyses of 57 prospective studies. Lancet 373(9669), 1083–1096 (2009).
Lopez-Jimenez, F. Speakable and unspeakable facts about BMI and mortality. Lancet 373, 1055–1056 (2009).
Grigsby, M. R. et al. Low body mass index is associated with higher odds of COPD and lower lung function in low- and middle-income countries. COPD 16(1), 58–65 (2019).
Acknowledgements
We appreciate all the participants and staff of NHANES 2003–2012 for their precious contributions.
Funding
This research was supported by Shandong Province Taishan Scholar Project (No: tsqn202306392).
Author information
Authors and Affiliations
Contributions
X.L. obtained funding. Y.Z. and Y.S. designed the study. Y.Z. and Y.S. collected the data. Y.Z. and X.Y.L. analyzed the data. Y.S. and X.Y.L. drafted the manuscript, X.Y.L., Y.Y.L. and F.W. is responsible for checking and verifying the data. X.L. participated in the research design and editor of the manuscript. All authors contributed to the interpretation of the results and critical revision of the manuscript for important intellectual content and approved the final version of the manuscript and have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, Y., Zhang, Y., Liu, X. et al. Association between body mass index and respiratory symptoms in US adults: a national cross-sectional study. Sci Rep 14, 940 (2024). https://doi.org/10.1038/s41598-024-51637-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-51637-z
- Springer Nature Limited