Abstract
Many patients in Korea use Korean Medicine (KM) after spine surgery, but related research is lacking. Therefore, this retrospective cohort study aimed to analyze factors affecting the use and costs of KM using nationally representative data from the National Health Insurance Service-National Sample Cohort, South Korea. Patients who underwent spinal surgery for spinal diseases from 2011 to 2014 were followed up for 5 years, and their medical care was described. The association between patient and spinal surgery characteristics and the use of KM was analyzed. A two-part model was used to analyze factors affecting the use of KM in patients undergoing spinal surgery. Of 11,802 patients who underwent spinal surgery, 11,367 who met the inclusion criteria were included. Overall, 55.5% were female, 32.3% were aged ≥ 70 years, and 50.2% received KM treatment during the follow-up period. Open discectomy was the most common surgical procedure performed (58.6%), and 40.2% of surgeries were performed because of lumbar disc disorder. Female sex, older age, high Charlson Comorbidity Index score, and use of KM before surgery were associated with increased KM use and expenditure after surgery. In conclusion, patient characteristics, rather than surgical characteristics, appeared to be more strongly associated with the use of KM after surgery, particularly prior experience with KM use. This study is significant in that it analyzed the entire spine surgery to provide a comprehensive view of the use of KM after spine surgery and analyzed the impact of various factors related patients and surgical characteristics on KM use. The results of this study may be useful to patients with spinal diseases, clinicians, and policymakers.
Similar content being viewed by others
Introduction
Back pain is one of the most common causes of chronic pain in adults and is considered an important global health problem owing to its high prevalence and socioeconomic cost1. Back pain is also a major cause of disability. The number of years lived with disability in 2015 was 60.1 million, an increase of approximately 54% compared to that in 20052. In addition, the lifetime prevalence of back pain is as high as 66%3, although it varies from study to study. Back pain is associated with decreased productivity, increased medical expenses, and long-term opioid use2,4,5,6.
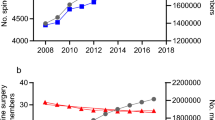
Non-specific back pain is common and associated with spinal diseases, such as intervertebral disc disorders and spinal stenosis, in many cases. Spinal surgery is one of the primary treatment methods for spinal diseases. In many countries, spinal surgery and surgical costs have increased in recent decades7,8,9. In the United States, spinal fusion surgeries increased by 62.3% between 2004 and 2015, and the cost of spinal surgery in 2015 was $10 billion8. According to the 2020 Main Surgery Statistics Yearbook of the National Health Insurance Service, the number of general spine surgeries in Korea was 188,394, the second highest after cataract surgery, and the cost of surgery was the highest at 918.2 billion South Korean won (KRW)10.
As several patients experience pain following spinal surgery11, pain management after spinal surgery is very important12. Many patients manage pain by taking opioids, such as morphine, after spinal surgery13,14. According to a study, more than half of those who used opioids before surgery took opioids 12 months after surgery13, and another study showed that more than 25% of patients took opioids 1 year after spinal surgery14. Medications such as non-steroidal anti-inflammatory drugs and paracetamol are often administered when opioids are being avoided15. Additionally, patients may undergo reoperation or readmission for various reasons16,17,18. The 10-year spinal reoperation rate in Korea was 13.2%; patients in their 60 s had the highest risk19.
South Korea has a dichotomized healthcare system with both western and Korean medicine (KM); the latter is one of the traditional medicine systems used in East Asia along with traditional Chinese medicine. In particular, KM modalities, such as acupuncture, herbal medicine, and Chuna treatment are widely used as conservative treatments for spinal diseases20,21,22,23. According to the 2020 health insurance statistics, back pain is the most frequent indication for the use of KM23.
In particular, many patients receive KM treatment after spinal surgery24,25. However, little is known about the characteristics of patients using KM after spine surgery and the cost of using KM. Understanding this can be helpful to KM clinicians who treat patients in real world and policymakers who establish policies related to coverage and accessibility of KM treatment.
Therefore, this study aimed to characterize the medical care after spinal surgery in Korea and to analyze factors associated with the use of KM after spinal surgery based on data from the National Health Insurance Service–National Sample Cohort (NHIS-NSC), South Korea.
Results
Participants
A total of 11,802 patients underwent spinal surgery for spinal diseases from 2011 to 2014. Patients with spondylopathy (n = 2), other infections, parasitic diseases, and malignant or benign neoplasm (n = 82) were excluded. Patients with a history of spinal surgery within 3 years prior to the first surgery between 2011 and 2014 (n = 351) were also excluded. Finally, 11,367 patients were included in the analysis (Fig. 1).
Patient characteristics associated with KM use
The characteristics of the participants are presented in Table 1. Among 11,367 patients, 6311 (55.5%) were female, and the average age was 59.77 ± 15.93 years. There was a monotonic increase in the frequency of spinal surgery across age categories, with the highest frequency observed in the > 70 years group (32.3%). In addition, 4963 patients (43.7%) had used KM in the year prior to surgery.
A total of 5711 patients received KM treatment during the 5-year follow-up period, accounting for 50.2% of all patients who underwent surgery. In the KM use group, the proportions of females (60.7%), patients aged > 60 years (58.5%), patients residing in metropolitan cities (19.3%), others (40%), and patients with CCI scores > 3 (39.4%) were high. In the KM use group, the average time from discharge to the first use of KM was 522.05 ± 490.23 days, and the median number was 356 days.
Characteristics of index spine surgery according to the use of KM
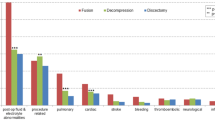
The characteristics of the index spinal surgeries are presented in Table 2. Open discectomy was the most common (6661 patients, 58.6%), followed by fusion (3025 patients, 26.6%), percutaneous vertebroplasty (2385 patients, 21.0%), and laminectomy (2171 patients, 19.1%). Regarding disease type, 40.2% of the surgeries were due to lumbar disc disorder, and by disease sites, 80% were performed in the lumbar spine (l-spine) area. The average length of hospitalization and surgical costs were 14.20 ± 11.11 days and 2537.73 ± 1997.66 US dollars, respectively. In the KM use group, more patients underwent surgery for stenosis than in the non-KM use group, and by surgical site, more patients underwent surgery for the lumbar spine (p < 0.05). In addition, average length of hospitalization and hospitalization costs were quite long (14.57 ± 11.13 days) and high (2555.24 ± 1920.01 US dollars), respectively, in the KM use group.
KM expenditure and the time to the first use of KM
Table 3 presents the KM expenditure and the time to the first use of KM according to the basic characteristics of participants and index surgery. In the KM use group, the median cost for all KM expenses was $172.32 (IQR: 57.85–504.02), and the time to the first use of KM was 356 (IQR: 109–840) days. The KM expenditure was higher and the time to the first use of KM was shorter in female patients, elderly patients, participants with higher CCI scores, and those who had experience with KM use prior to the surgery. A similar tendency was shown when compared with the average expenditure and time (Supplementary Table S4). Meanwhile, Supplementary Table S5 shows KM treatment details and costs received by patients after surgery.
Factors affecting the use of KM after spinal surgery
A two-part model was used to analyze the factors affecting the use of KM and the cost of using KM after spinal surgery. The univariate analysis revealed that female sex, older age, CCI score, and prior experience with KM use were factors that increased the use and medical costs of KM after surgery. Patients living in metropolitan cities and other areas had higher odds of using KM, whereas those living in capital areas had lower odds of using KM and lower medical costs for KM (Table 4).Spinal stenosis and a higher than median cost of spinal surgery were associated with greater odds of using KM and increased KM expenditure.
The final model was determined by analyzing the results of the univariate and multivariate models with all variables included in the univariate analysis (Table 5). Female sex, older age, high CCI score, and prior experience with KM use were factors that increased KM use and expenditure after surgery. The odds for using KM were higher among those living in metropolitan cities. A similar trend was observed in the sensitivity analysis results, in which the use of KM was defined as within 1 year or 3 years instead of 5 years (Tables S6 and S7).
Discussion
With spinal surgery and surgical costs increasing worldwide7,8,9,10, many patients in Korea use KM after spinal surgery24,25. Although several studies have been conducted to show the effectiveness of KM treatments, including acupuncture12,26, electroacupuncture27,28,29, and moxibustion30, no study has investigated the KM use status in patients after spinal surgery.
The present study had a large sample size (N = 11,367 patients) and used nationally representative data. In this study, female sex, older age, high CCI score, and the use of KM before surgery were identified as factors associated with KM use and expenditure. The probability of using KM was high when living in areas with low medical expenses other than Seoul. In addition, in the case of plastic surgery and surgery for stenosis, KM medical expenses were high. Several studies analyzing the general determinants of KM use have reported a high proportion of female and elderly participants in the KM use group31,32,33. Women tend to accept traditional medicine better than men and seek it more frequently34,35. Women and the elderly in Korea often have relatively low socioeconomic status, several chronic diseases, and low subjective health status. According to statistics from Ministry of employment and labor In Korea, the total monthly wage was 2,645,000 Korean won for over years old. This is lower than 3,710,000 in 30 s, 4,195,000 in 40 s, and 3,909,000 in 50 s. By sex, monthly wages were 4,127,000 for male and 2,683,000 for female36. Therefore, the demand for medical care is high; however, there is a high possibility of unmet medical care37,38,39. The results of this study suggest that KM may be considered a means to satisfy the unmet medical needs of women and the elderly after surgery.
The median days until first medical use after surgery for KM users was 8 days, while the median days until first KM use was 365 days. In other words, KM was used about a year after surgery, which was later than using conventional treatment. This suggested that patients tend to use conventional treatment in the early stages after surgery, but seek KM when symptoms become chronic and do not approved. The CCI score, surgical cost, and hospitalization days were higher in the KM use group, suggesting that patients with relatively severe diseases used KM more often. In particular, the proportion of patients who underwent surgery for stenosis in the KM use group was high, which reflects the recent rapid increase in the use of KM for stenosis. According to the health insurance statistics of the NHIS, the number of patients using KM for stenosis in 2010 increased by approximately three and a half times from 38,090 to 134,337 in 2020. This is a significant increase compared with the 1.8-fold increase in the number of patients with stenosis within the same period. However, only few studies on the effects of KM on stenosis have been conducted, and additional research on this topic is required.
Prior experience with KM use was the most influential factor for the use of KM after surgery. In other words, patients who received KM treatment were more likely to continue to choose KM. Several factors influence the patients’ choice of treatment. In an interview study conducted by Kim et al.40, personal experiences and advice from people in one’s network were shown to be important factors in choosing a treatment method. These factors particularly influenced the decision to choose the KM treatment. Patients who directly or indirectly experienced the effects of KM treatment had a positive perception of KM and chose KM rather than surgery. Patel et al.41 revealed through interviews that individuals' positive experiences and word-of-mouth about acupuncture had an impact on the pursuit of traditional Chinese medicine. Another study42 found that when choosing a primary care physician or specialist, information or recommendations from acquaintances were more important than other factors.
These individual and community experiences often lead to the formation of medical beliefs, which affect treatment selection and medical service usage patterns more than any other objective factors43,44. With respect to the medical beliefs that lead to the selection of KM, KM is believed to be superior and to have fewer side effects with less toxicity, in addition to the recognition of limitations in drug treatment41,45,46. The high rate of KM use after surgery in patients with KM experience means that past KM experience helped form these positive medical beliefs about KM. In addition, the longer the treatment period, the more patients learn about and try various treatments. As a result, patients may be reminded of past experiences they had forgotten, and there is a possibility that they will use KM as they collect more information about various treatments and stories from acquaintance. Accordingly, a long treatment period may be a factor that increases KM use rate, but this study was not able to isolate this factor.
Ultimately, this study revealed that patient characteristics (particularly, previous experience in using KM), rather than surgical-related characteristics, affected the use of KM after surgery. This finding was similar to the factors affecting the general use of KM.
Meanwhile, KM treatment generally consists of acupuncture, electroacupuncture, pharmacopuncture, herbal medicine, and Chuna manual therapy. There are several studies showing that such KM treatment has the potential to be an effective treatment for improving pain and function in patients after spine surgery. In a study in which 16 weeks of KM treatment was conducted on 120 patients with persistent postoperative pain26, the visual analogue scale (VAS) for back and lower extremity pain improved from 6.1 to 2.9 and from 5.4 to 2.4 respectively after 6 months. In one systematic review12, it was found that acupuncture treatment 24 h after surgery showed a positive effect on pain reduction compared to sham treatment. Another study comparing the usual care and electroacupuncture combination with the usual care in patients with pain after spine surgery, the combination treatment with electroacupuncture was more effective and cost-effective in improving VAS and Oswestry disability index.
This study had some limitations. The data utilized for the analyses were obtained from the NHIS-NSC database, and only information from this database could be analyzed. The data provided by the sample cohort were based on claims submitted by medical institutions for reimbursement; therefore, non-covered items were not included. Furthermore, surgery and KM have a high proportion of non-covered items. Hence, the cost calculated in this study might have underestimated the actual cost incurred in the real world. However, since patients rarely receive only non-covered treatment, it is very unlikely that there will be bias in the results of KM use analysis.
In addition, diagnosed diseases and types of surgery were described using disease and procedure codes only. Other potentially important factors, such as operative time, amount of transfused blood, and degree of pain before and after surgery, were not considered because of data limitations. If these factors had been investigated, a more diverse and rich analysis of the factors affecting KM use would have been possible. However, despite the limitations of the data, we extracted as many surgery-related outcomes as possible through various operational definitions such as surgery complexity and disease type, and also extracted as many variables as possible for patient characteristics. Additional studies that thoroughly describe the characteristics of surgery using surgery-related outcome variables are needed.
It is also unfortunate that clinical outcome data such as VAS and ODI could not be analyzed due to database limitations. If such data were available, it would have been possible to analyze changes in outcomes according to KM use. In the future, research can be conducted to examine changes in outcomes according to the use of KM by combining database and hospital data.
Nevertheless, this study is the first to analyze the use of KM after spinal surgery in detail. In particular, all types of spinal surgery were analyzed, and this study was not limited to specific widely studied surgeries, such as stenosis and lumbar disc herniation, to provide a comprehensive view of the use of KM after spinal surgery. In addition, the effects of various patient and surgical characteristics on the use of KM were analyzed through various operational definitions, and the belief formed through experience in using KM was considered as a major factor influencing the health-seeking behavior of using KM. The results of this study provide useful information to KM clinicians who treat patients in real world and policymakers who establish policies related to coverage and accessibility of KM through a deep understanding of patients who use KM after surgery.
In conclusion, female sex, older age, high CCI score, and prior experience with KM use were factors that increased KM use and expenditure after surgery. Additional research can be conducted by combining other variables that cannot be extracted from this database with the database. The results of this study may be useful to clinicians, and policymakers.
Methods
Study design
This retrospective cohort study included patients who underwent spinal surgery for spinal diseases from 2011 to 2014 and were followed up for 5 years. For these patients, medical care for spinal diseases was investigated. In addition, patients’ and spinal surgery characteristics, use and costs of KM after spinal surgery, and factors associated with the use of KM were analyzed. This study was reviewed and qualified as an exemption by the Institutional Review Board of Kyung Hee University (approval no.: KHSIRB-22-261, approval date: 31 May 2022). The principles expressed in the Declaration of Helsinki were adhered to in the study’s analysis. As the study analyzed publicly available data, it was exempted from the consent process by the Institutional Review Board of Kyung Hee University. All personal information was de-identified by the NHIS prior to public release.
Data source
Data from the NHIS-NSC 2.2 database from 2011 to 2019 were analyzed in this study. Korea has a nationwide medical insurance system; hence, most people are enrolled in the National Health Insurance Service (NHIS). In the case of covered items, medical costs are paid by the NHIS and the patient. For reimbursement of the co-payment, each medical institution submits insurance claims to the NHIS containing detailed information about the service provided. Accordingly, the NHIS contains data related to the use of medical care by the entire population. The NHIS established and used a sample cohort with a stratified sampling of the entire population for research purposes47. The NHIS-NSC 2.2 database comprises sample data from a randomly selected and stratified sample of 2.2% of the Korean population in 2006 who were followed up until 2019.
Participants
This retrospective cohort study included patients who underwent spinal surgery for back pain and spinal diseases between 2011 and 2014 (Fig. 2). Patients with infections, parasitic diseases, malignant/benign neoplasms, or fractures were excluded. Moreover, patients with spinal tuberculosis, brucella spondylitis, enterobacterial spondylitis, and spondylopathy were excluded. In addition, patients with a history of spinal surgery within 3 years before the first surgery between 2011 and 2014 were excluded. Therefore, patients who underwent surgery for the first time were included. Spinal diseases were defined based on the disease names of the 7th Korean Standard Classification of Disease (KCD-7) and 10th International Standard Classification of Disease (ICD-10). The inclusion and exclusion KCD-7 codes are listed in Supplementary Table S1. Lastly, patients who used KM at least once within the 5 years of follow-up were assigned to the KM use group, whereas those who did not use KM were assigned to the non-KM use group.
Variables
Index surgery
The index date for spinal surgery was defined as the hospitalization date of the index hospitalization during which spinal surgery was performed. In Korea, even one hospitalization episode can cause multiple claims for various reasons; therefore, the definition of index hospitalization episodes should be carefully considered. In this study, based on claims that included surgery, connected claims with a hospitalization date with a 1-day interval from the discharge date were considered as one hospitalization episode. However, hospitalization episodes were excluded (1) in cases of outpatient procedures, (2) when the disease codes in the connected claims were not disease inclusion codes, and (3) when the institution was different from the institution where the surgery was performed.
In addition, if there was another spinal surgery in the connected claims, the claim was defined as another hospitalization episode and considered a reoperation. Claims that occurred in the same institution during hospitalization were added to the index hospitalization episode (Fig. 3).
Index surgery date and hospitalization episode. (A) No connected claim; one claim was considered as one hospitalization episode. (B) If there were two connected claims with no surgical records, the two claims were regarded as one hospitalization episode, and the admission date for the first claim was set as the index surgery date. (C) If there were connected claims with surgical records, each claim was regarded as an independent hospitalization episode, and the admission date for each claim was set as the index date.
Characteristics of spinal surgery
The characteristics of spinal surgery, including type of surgery, complexity of surgery, type of disease, disease area, type of institution, length of hospital stay, and cost of surgery were investigated. The types of surgery were classified as fusion, open discectomy, percutaneous endoscopic lumbar decompression (PELD), nucleolysis, percutaneous plasty, laminectomy, cervical spine laminoplasty, corpectomy, and reduction. The complexities of surgery were classified as non-invasive, open surgery, or open surgery with an instrument. If multiple surgical codes were applied in one hospitalization episode, duplication was allowed for the types of surgery and included in the classification of the complexity of surgery. For convenience, the type of surgery was classified during factor analysis as decompression (discectomy, laminectomy, or no fusion), fusion, percutaneous plasty (only percutaneous plasty), and others. All spinal surgeries were defined based on procedure codes in the claims. The codes were selected based on previous studies24,48. The procedure codes for the classification of types and complexities of surgery are presented in Supplementary Table S2.
Disease types were classified as lumbar disc disorder, fracture, stenosis, deforming dorsopathy, cervical disc disorders, spondylosis, inflammatory spondylopathies, dorsalgia, dorsopathy, and other spondylopathies. For factor analysis, spondylosis, inflammatory spondylopathies, dorsalgia, dorsopathy, and other spondylopathies were grouped because of their low frequency. Disease areas were classified as cervical, thoracic, and lumbar spines (Supplementary Table S3). All classifications were based on the KCD-7. Surgical institutions were classified into tertiary general hospitals, general hospitals, hospitals, and clinics, according to the national classification criteria. The classification criteria for spinal surgery were decided through an internal meeting of the research team.
Patient characteristics
Variables related to patient characteristics were selected based on the Andersen healthcare utilization model49 and information available from this database. The Andersen model is the most basic model that explains patients' medical utilization. In this study, sex, age, area of residence, prior experience with KM use were included as predisposing factors, income level as enabling factors, and CCI as necessary factors. Age was classified as < 20, 20–29, 30–39, 40–49, 50–59, 60–69, and > 70 years old. Income was categorized into four stages by reclassifying the 10th decile classification in the data. Residential areas were classified as Seoul, capital areas, metropolitan cities, and others. The capital areas included Gyeonggi-do and Incheon, whereas the metropolitan cities included Daejeon, Daegu, Gwangju, Ulsan, and Busan. CCI was calculated based on all diseases that occurred in the year before the index date and was classified as 0, 1, 2, 3, and 4 points or more. In addition, the use of KM for spinal diseases during the year before the index date was included as a variable.
Use of KM
The use of KM within the follow-up period, the total cost of KM treatment, and the time until the first use of KM were determined.
Statistical analysis
Descriptive statistics were calculated to describe the characteristics of patients and index surgery in the KM and non-KM use groups. Continuous variables are presented as mean and standard deviation (SD), whereas categorical variables are expressed as frequency and percentage. The differences between the two groups were analyzed using the chi-square test and independent t-test.
Medical expenditures for KM use and the time until the first use of KM according to the basic characteristics of patients and index surgery in the KM use group are presented as medians and interquartile ranges. Differences in characteristics were examined using the Wilcoxon rank-sum test.
A two-part model50,51 was used to analyze factors affecting the use of KM in patients who underwent spinal surgery. This technique is used for semi-continuous data with abundant zero values, such as medical expenditure52. In a two-part model, analysis consists of a process of determining the probability of a positive value occurring and a process of predicting the positive value. In this study, the prediction of the mean dependent variable and KM expenditure also depends on two factor s. The probability of patients using KM was modeled in the first part of the two-part model. In the second part, the main concern was to predict medical expenditure by patients using KM.
For the first part, of the possible logit and probit models, the logit model was used because it is widely used for the analyses of this nature. The difference between the results of the two models is not significant; thus, either model may be used51. In the second part, the generalized linear model (GLM) requires choosing a link function and a distribution family. First, the Box-Cox test was used to determine the link function. In this study, all univariate and multivariate models showed a scalar power close to 0; therefore, the natural log link function was selected53. Next, gamma distribution was used for the distribution family. The gamma distribution is a flexible distribution that can be used when analyzing continuous, positively skewed, and positive data54. Therefore, GLM with gamma distribution is commonly used to analyze data with mass zeros and right-skewed distribution, such as medical expenditure55.
The final model was determined by referring to the results of the univariate models and multivariate model including all variables used in univariate models. For the univariate model, the following variables were analyzed; sex, age, income, region, CCI, Use of KM before surgery, type of surgery, complexity of surgery, types of disease, disease sites, type of institutions, costs of surgery, length of stay. The results are presented with odds ratios (OR) and 95% confidence intervals (95% CI) in the first part and coefficient and robust standard error (SE) in the second part.
In addition, the marginal effects for each variable are shown with a 95% CI. Marginal effects are an alternative way to express results that can add an intuitive understanding to the meaning of the analysis. They measure the effect of a one-unit change in a specific explanatory variable on the conditional mean of a dependent variable. In other words, the marginal effect of a specific variable indicates changes in the result due to changes in a specific explanatory variable when all other explanatory variables are fixed at the average56.
Medical expenditures were calculated in Korean won (KRW) and converted to the United States dollars using the average exchange rate from 2011 to 2019 (1119.11 KRW/USD). All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and Stata 17 (StataCorp, College Station, TX, USA) with the “twopm” command.
Ethics statement
The current study was reviewed and qualified as an exemption by the Institutional Review Board of Kyung Hee University (KHSIRB-22-261). The principles expressed in the Declaration of Helsinki were adhered to in the study’s analysis. As the study analyzed publicly available data, no consent was obtained from patients; all personal information was de-identified by the NHIS prior to public release.
Data availability
This study incorporated data from the National Health Insurance Service Sample Cohort 2.2 (2002–2019), released by the Korean National Health Insurance Service in response to the researchers’ request. The detailed cohort profile and methods for obtaining data are explained in the following sources: Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. International Journal of Epidemiology. 2016. https://doi.org/10.1093/ije/dyv319. PubMed PMID:26822938.
References
Chung, S.-S. et al. A nationwide retrospective study of opioid management patterns in 2,468 patients with spinal pain in Korea. Asian Spine J. 10(6), 1122 (2016).
James, S. L. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet 392(10159), 1789–1858 (2018).
Hoy, D. et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 64(6), 2028–2037 (2012).
Herman, P. M., Broten, N., Lavelle, T. A., Sorbero, M. E. & Coulter, I. D. Healthcare costs and opioid use associated with high-impact chronic spinal pain in the United States. Spine 44(16), 1154 (2019).
Lee, H. et al. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain 156(6), 988–997 (2015).
Hartvigsen, J. et al. What low back pain is and why we need to pay attention. The Lancet 391(10137), 2356–2367 (2018).
Kim, C. H. et al. Increased volume of lumbar surgeries for herniated intervertebral disc disease and cost-effectiveness analysis. Spine 43(8), 585–593 (2018).
Martin, B. I. et al. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine 44(5), 369–376 (2019).
Grotle, M. et al. Lumbar spine surgery across 15 years: Trends, complications and reoperations in a longitudinal observational study from Norway. BMJ Open 9(8), e028743. https://doi.org/10.1136/bmjopen-2018-028743 (2019).
National Health Insurance Service. 2020 Main Surgery Statistical Yearbook. Available at: https://kosis.kr/statHtml/statHtml.do?orgId=350&tblId=DT_350004N_A005_1&vw_cd=MT_OTITLE&list_id=350_35004_6&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=K2&path=%252Fcommon%252Fmeta_onedepth.jsp
Sommer, M. et al. The prevalence of postoperative pain in a sample of 1490 surgical inpatients. Eur. J. Anaesthesiol. 25(4), 267–274 (2008).
Cho, Y. H. et al. Acupuncture for acute postoperative pain after back surgery: A systematic review and meta-analysis of randomized controlled trials. Pain Pract. 15(3), 279–291 (2015).
Dunn, L. K. et al. Incidence and risk factors for chronic postoperative opioid use after major spine surgery: A cross-sectional study with longitudinal outcome. Anesthesia Analgesia 127(1), 247 (2018).
Warner, N. S. et al. Association between spine surgery and availability of opioid medication. JAMA Netw. Open 3(6), e208974. https://doi.org/10.1001/jamanetworkopen.2020.8974 (2020).
Bajwa, S. J. S. & Haldar, R. Pain management following spinal surgeries: An appraisal of the available options. J. Craniovertebr. Junction Spine 6(3), 105 (2015).
Lewin, A. M. et al. Rates, costs, return to work and reoperation following spinal surgery in a workers’ compensation cohort in New South Wales, 2010–2018: A cohort study using administrative data. BMC Health Serv. Res. 21(1), 955. https://doi.org/10.1186/s12913-021-06900-8 (2021).
Villavicencio, A., Rajpal, S., Lee Nelson, E., Avoian, S. & Burneikiene, S. Unplanned 30-day readmission rates after spine surgery in a community-based hospital setting. Clin. Neurol. Neurosurg. 191, 105686. https://doi.org/10.1016/j.clineuro.2020.105686 (2020).
Rienmüller, A. C., Krieg, S. M., Schmidt, F. A., Meyer, E. L. & Meyer, B. Reoperation rates and risk factors for revision 4 years after dynamic stabilization of the lumbar spine. Spine J. 19(1), 113–120 (2019).
Noh, S. H. et al. Risk factors for reoperation after lumbar spine surgery in a 10-year Korean national health insurance service health examinee cohort. Sci. Rep. 12(1), 1–9 (2022).
Park, S.-Y. et al. Comparative effectiveness of chuna manipulative therapy for non-acute lower back pain: A multi-center, pragmatic, randomized controlled trial. J. Clin. Med. 9(1), 144 (2020).
Lee, J. et al. Pain, disability, and MRI changes in lumbar disc herniation patients treated with integrative medicine: Ten-year results of an observational study. Integr. Med. Res. 11(2), 100833 (2022).
Kim, D. et al. Long-term follow-up of spinal stenosis inpatients treated with integrative Korean medicine treatment. J. Clin. Med. 10(1), 74 (2020).
Health Insurance Review & Assessment Service. 2020 National Health Insurance Statistical Yearbook. Available at: https://kosis.kr/statHtml/statHtml.do?orgId=350&tblId=DT_35001_A180111&vw_cd=MT_OTITLE&list_id=350_35001_6&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=K2&path=%252Fcommon%252Fmeta_onedepth.jsp.
Ye, S.-A., Kim, N.-K. & Song, Y.-K. Analysis of medical and Korean medical services utilization after lumbar surgery patients: Using health insurance review and assessment service’s patients sample data. J. Korean Med. Rehabil. 29(4), 89–100 (2019).
Moon, S.-Y., Shin, K.-M., Shin, J.-Y., Kwon, O.-J. & Lee, J.-H. Integrative medicine for postoperative patients: A survey of Korean medicine doctors. Evid. Based Complement. Altern. Med. 2017. https://doi.org/10.1155/2017/4650343 (2017).
Lee, J. et al. Long-term Course of Failed Back Surgery Syndrome (FBSS) patients receiving integrative Korean medicine treatment: A 1 year prospective observational multicenter study. PLoS ONE 12(1), e0170972 (2017).
Heo, I. et al. Multicentre randomised controlled clinical trial of electroacupuncture with usual care for patients with non-acute pain after back surgery. Br. J. Anaesthesia 126(3), 692–699 (2021).
Kim, N., Shin, K.-M., Seo, E.-S., Park, M. & Lee, H.-Y. Electroacupuncture with usual care for patients with non-acute pain after back surgery: Cost-effectiveness analysis alongside a randomized controlled trial. Sustainability 12(12), 5033 (2020).
Shin, D. et al. Effectiveness of electroacupuncture for patients with failed back surgery syndrome: A systematic review and meta-analysis. J. Acupunct. Res. 39(3), 159–169 (2022).
Lee, D.-H., Park, H.-S. & Hwang, J.-S. The clinical study on the effects of moxibustion to FBSS (failed back surgery syndrome). J. Acupunct. Res. 23(3), 67–75 (2006).
Park, J.-E. & Kwon, S.-M. Determinants of the utilization of oriental medical services by the elderly. J. Korean Med. 32(1), 97–108 (2011).
Seo, Y.-J., Kang, S.-H., Kim, Y.-H., Choi, D.-B. & Shin, H.-K. Systematic review on the customers’ use of and satisfaction with oriental medical services. J. Korean Med. 31(1), 69–80 (2010).
Seo, S., Park, B. H. & Choi, S.-J. A study on the sociodemographic characteristics of adult users of Korean traditional medicine. J. Korean Public Health Nurs. 30(1), 136–148 (2016).
Chen, P.-H., Huang, S.-M., Lai, J.C.-Y. & Lin, W.-L. Determinants of health-seeking behavior toward Chinese or Western medicine in Taiwan: An analysis of biobank research database. Complement. Ther. Clin. Pract. 48, 101592 (2022).
Liu, C.-T., Wu, B.-Y., Hu, W.-L. & Hung, Y.-C. Gender-based differences in mortality and complementary therapies for patients with stroke in Taiwan. Complement. Ther. Med. 30, 113–117 (2017).
Ministry of employment and labor. 2022 survey report on labor conditions by employment type. Available at: https://kosis.kr/statHtml/statHtml.do?orgId=350&tblId=DT_35001_A180111&vw_cd=MT_OTITLE&list_id=350_35001_6&scrId=&seqNo=&lang_mode=ko&obj_var_id=&itm_id=&conn_path=K2&path=%252Fcommon%252Fmeta_onedepth.jsp
Park, M. The factors affecting unmet medical needs in elderly by using Korea health panel data 2011. J. Korean Data Anal. Soc. 16(2), 1017–1030 (2014).
전경숙, 최은숙, 이효영. 의료이용의 남녀차이와 영향요인에 관한 연구. 韓國保健看護學會誌. 2010;24(2):182–96.
Mustard, C. A., Kaufert, P., Kozyrskyj, A. & Mayer, T. Sex differences in the use of health care services. N. Engl. J. Med. 338(23), 1678–1683 (1998).
Kim, D. et al. Influencing factors for choosing Korean medicine treatments after spinal surgery or spinal surgery recommendation in patients with spinal pain: A semi-structured interview study. Complement. Med. Res. 29(4), 320–329 (2022).
Patel, A. & Chen, Y. Patients’ reasons for seeking traditional Chinese medicine: A qualitative study. J. Prim. Health Care 10(4), 338–342 (2018).
Tu, H. T. & Lauer, J. R. Word of Mouth and Physician Referrals Still Drive Health Care Provider Choice (Center for Studying Health System Change, 2008).
Ng, T. K. C., Lo, M. F., Fong, B. Y. F. & Yee, H. H. L. Predictors of the intention to use traditional Chinese medicine (TCM) using extended theory of planned behavior: A cross-sectional study among TCM users in Hong Kong. BMC Complement. Med. Ther. 22(1), 113. https://doi.org/10.1186/s12906-022-03598-x (2022).
Kang, J.-T., Chen, C.-F. & Chou, P. Knowledge, attitude and behavioral intention of Chinese traditional medicine among outpatients. Taiwan J. Public Health 13, 432–441 (1994).
Hung, J. Y., Chiou, C. J. & Chang, H. Y. Relationships between medical beliefs of superiority of Chinese or western medicine, medical behaviours and glycaemic control in diabetic outpatients in Taiwan. Health Soc. Care Community 20(1), 80–86 (2012).
Shang, X. et al. Satisfaction and preference for traditional Chinese medicine drugs among guardians of children with acute bronchiolitis. J. Altern. Complement. Med. 21(10), 623–627 (2015).
Lee, J., Lee, J. S., Park, S.-H., Shin, S. A. & Kim, K. Cohort profile: The national health insurance service-national sample cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 46(2), e15 (2017).
Koh, W. et al. Impact of acupuncture treatment on the lumbar surgery rate for low back pain in Korea: A nationwide matched retrospective cohort study. PLoS ONE 13(6), e0199042 (2018).
Andersen, R. A Behavioral Model of Families’ Use of Health Services. Research Series No. 25. (Center for Health Administration Studies, University of Chicago, Chicago, 1968).
Belotti, F., Deb, P., Manning, W. G. & Norton, E. C. twopm: Two-part models. Stata J. 15(1), 3–20 (2015).
Deb, P. & Norton, E. C. Modeling health care expenditures and use. Annu. Rev. Public Health 39, 489–505 (2018).
Neelon, B., O’Malley, A. J. & Smith, V. A. Modeling zero-modified count and semicontinuous data in health services research part 1: Background and overview. Stat. Med. 35(27), 5070–5093 (2016).
Deb, P., Norton, E. C. & Manning, W. G. Health Econometrics Using Stata (Stata Press, 2017).
Kurz, C. F. Tweedie distributions for fitting semicontinuous health care utilization cost data. BMC Med. Res. Methodol. 17(1), 1–8 (2017).
Lima, F., Ferreira, P. & Leal, V. Health and housing energy expenditures: A two-part model approach. Processes 9(6), 943 (2021).
Williams, R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 12(2), 308–331 (2012).
Funding
This work was supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) and the Ministry of Health & Welfare, Republic of Korea (Grant Number: HF21C0111).
Author information
Authors and Affiliations
Contributions
Conceptualization: D.K. and B.H.J. Data curation: D.K. Formal analysis: D.K. Funding acquisition: Y.J.L. Methodology: S.P. and J.S.P. Supervision: B.H.J. Validation: S.P. and J.S.P. Visualization: D.K. Writing—original draft: D.K. and Y.J.L. Writing—review and editing: S.G.K, Y.C.S., and C.R.D.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, D., Lee, Y.J., Jang, BH. et al. Analysis of factors associated with the use of Korean medicine after spinal surgery using a nationwide database in Korea. Sci Rep 13, 20177 (2023). https://doi.org/10.1038/s41598-023-47454-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-47454-5
- Springer Nature Limited