Abstract
Purpose
Studies from developed countries suggest a dramatic increase in the utilization of spine surgery in recent decades, however less is known about spine surgery rates in the developing world. The aim of this study was to investigate ten-year trends in the incidence of spine surgery within South Africa’s largest open medical scheme.
Methods
This retrospective review included adult inpatient spine surgeries funded by the scheme between 2008 and 2017. The incidence of spine surgery was investigated by age group-overall and for degenerative pathologies, fusion and instrumentation. Surgeons per 100,000 members were determined. Trends were evaluated by linear regression and by crude 10-year change in incidence.
Results
A total of 49,575 spine surgeries were included. The incidence of surgery for lumbar degenerative pathology showed a significant upward trend among 60–79 year olds but declined among 40–59 year olds. The incidence of lumbar fusion and lumbar instrumentation declined significantly among 40–59 year olds with little change among 60–79 year olds. The ratio of orthopaedic spinal surgeons decreased from 10.2 to 6.3 per 100,000 members whereas the ratio of neurosurgeons decreased from 7.6 to 6.5 per 100,000.
Conclusion
Spine surgery in the South African private healthcare sector bears some similarity to developed countries in that it is dominated by elective procedures for degenerative pathology. However, the findings did not reflect the marked increases in the utilization of spine surgery reported elsewhere. It is hypothesized that this may be partly related to differences in the supply of spinal surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With technological advances and improved surgical techniques, indications for spinal surgery have widened considerably in recent decades [1, 2]. Studies from developed countries suggest that this has led to a dramatic increase in the utilization of spine surgery for degenerative pathologies, increased use of instrumentation and increased spine surgery among elderly patients [1,2,3,4,5,6,7,8,9]. This trend has been particularly prominent in fee-for-service settings such as the United States [7, 9], although it has also been observed in national, tax-funded health systems [3, 5, 10]. Less is known about spine surgery trends in developing countries, such as South Africa. In the South African private healthcare sector, spine surgery is dominated by elective surgery for degenerative pathologies and, in this regard, is likely similar to the profile of spine surgery in developed countries [1]. Surgeons have a high degree of discretion over the course of treatment and are reimbursed largely on a fee-for-service basis. Nevertheless, it is unclear whether the trend of increasing rates of spine surgery are present in this context. The aim of this study was to investigate trends in the incidence of spine surgery within South Africa’s largest open medical scheme over a ten-year period, with a particular focus on elective surgery for degenerative pathologies.
Methods
Design
This retrospective review included inpatient spine surgeries funded by the largest open medical scheme in South Africa between the 1st of January 2008 and the 31st of December 2017. The incidence of spine surgery was investigated based on the member’s first spine surgery within the study period and did not account for members who had more than one spine procedure. Surgeries included in the analysis were intended to represent index surgeries.
Setting
This study was set in the South African private healthcare sector, which serves approximately 16% of the population and is accessed largely by those with medical scheme membership. The total number of beneficiaries from all medical schemes, both open and closed, was 7.87 million in 2008 and 8.87 million in 2017 [11]. The medical scheme which funded the spine surgeries in the current study had an open market share of 56% and covered approximately 2,778,000 total beneficiaries as of December 2017 [12].
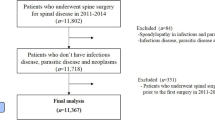
Patients
All members of the medical scheme ≥ 18 years of age who underwent inpatient spinal procedures in South Africa during the study period were identified by the scheme for inclusion in the study. The investigators subsequently reviewed the diagnostic and procedure codes for each event and excluded members from the analysis according to the following criteria: (i) procedure codes indicated medical management only, (ii) the “index” spine surgery was identified as a revision procedure based on diagnostic and/or procedure codes, (iii) diagnostic codes were not spine related plus procedure codes failed to confirm that a spine surgery had taken place.
Variables
The spine surgery data was provided by the medical scheme in the form of an anonymized dataset extracted from the scheme’s records. Variables included member demographics, comorbidity ICD-10 codes, surgery ICD-10 code, surgery Complete Current Procedural Terminology for South Africa (CCSA) codes, surgeon specialization and year of surgery. Each primary surgeon was assigned a unique anonymous code by the scheme such that it was possible to identify surgeries performed by the same primary surgeon.
Surgery ICD-10 code descriptions were analysed and categorized according to pathology type and spine region. As far as possible, pathology categories were named according to the terminology used in the ICD-10 code. The pathologies “disc disorder”, “stenosis” and “spondylosis” are strongly associated with degenerative processes and these categories were pooled to represent the minimum level of degenerative pathology. For the most part, spine region was identified from the surgery ICD-10 code. However, when the ICD-10 code did not specify a spine region, procedure codes were checked for this information. Spine region was classified as cervical, thoracic, lumbar or unspecified. Procedure codes were analysed by a fellowship-trained spine surgeon and specific surgical elements were categorized as present or absent in each surgery. Surgical elements of interest included the use of any spinal fusion and use of instrumentation.
In addition to the surgery dataset, the scheme provided the total number of members per age bracket per year and this served as denominator data for calculating the incidence of spine surgery.
Data analysis
Categorical descriptive variables were presented as frequencies and percentages. The crude incidence of spine surgery per 10,000 members was calculated as follows [(number of surgeries/number adult members) × 10,000]. The age-stratified incidence of spine surgery, overall and by categories of interest, was calculated in the same manner, adjusting the numerator and denominator as appropriate. Categories of interest included surgeries for degenerative pathology, fusion and instrumentation. Furthermore, sub-analyses were conducted to investigate trends in spine surgeries by cervical and lumbar region. The number of unique surgeons billing to the scheme each year and the ratio of surgeons to 100,000 members was presented. In addition, the number of surgeries billed per surgeon per year, an indicator of scheme-specific surgeon volume, was reported as a median and interquartile range.
Trends in spine surgery were evaluated by fitting a linear regression model to the incidence of spine surgery by year. The magnitude and direction of the regression slope was used to provide interpretation of the trend and trends were regarded as statistically significant when the slope differed from zero at p ≤ 0.05. The crude ten-year change in incidence, taken as the difference in incidence between 2008 and 2017, was provided as additional descriptive information in some cases. Analyses were conducted using jamovi version 1.6 (www.jamovi.org) and GraphPad Prism version 9.2.0 for Mac OS, GraphPad Software, San Diego, California USA, www.graphpad.com.
Results
A total of 54,998 adult scheme members underwent inpatient spinal procedures during the study period. However 5423 procedures were excluded on the following basis: 200 involved medical management only, 4686 were revision surgeries and 537 had insufficient evidence of a spine surgery. The remaining 49,575 were included in the analysis. The characteristics of the included members and the specialization of the operating surgeon are shown in Table 1.
Crude incidence of spine surgery
The number of adult scheme members increased from approximately 1.4 million in 2008 to approximately 2 million in 2017. This was accompanied by a 26% increase in the number of spine surgeries, from 4357 in 2008 to 5494 in 2017 (Fig. 1a). A regression model fitted to the incidence of spine surgery by year showed a modest, significant downward trend (slope = − 0.42, R2 = 0.77, p < 0.001) (Fig. 1b). Overall, the crude incidence of spine surgery decreased by 13%, from 31 per 10,000 members in 2008 to 27 per 10,000 members in 2017.
Age-stratified incidence of spine surgery
Members and surgeries stratified by age group are shown in Fig. 2. While 18–39 year olds made up the largest proportion of adult scheme members (Fig. 2a), the absolute number of spine surgeries was highest in 40–59 year olds (Fig. 2b). The incidence of spine surgery was highest among those 60–79 years old, followed by those ≥ 80 years old (Fig. 2c). Regression models showed a significant downward trend in the incidence of spine surgery across all age groups, although the slope was smaller for 18–39 year olds than for the older age groups (Fig. 2c) (Table 2).
Degenerative pathology, fusion and instrumentation
Trends in the incidence of spine surgery by categories of interest and by spine region are shown in Fig. 3 and the associated regression analysis results in Table 2. Furthermore, crude ten-year changes in incidence are presented in Fig. 4. Analysis by spine region showed a significant upward trend in lumbar degenerative pathology surgery among 60–79 year olds with a ten-year increase of 5.0 surgeries per 10,000 (Figs. 3g, 4c, Table 2). Furthermore, there was a significant upward trend in cervical degenerative pathology surgery among ≥ 80 year olds with a ten-year increase of 4.1 surgeries per 10,000 (Figs. 3d, 4b, Table 2). In contrast, lumbar spine surgery for degenerative conditions declined significantly among 18–39 year olds and 40–59 year olds (Fig. 3g, Table 2). The incidence of cervical and lumbar fusion surgeries remained stable in 60–79 year olds and ≥ 80 year olds, however there was a significant decline lumbar fusion surgeries in the younger age groups (Fig. 3h, Table 2). The incidence of cervical and lumbar instrumentation surgeries also remained similar in 60–79 year olds, accompanied by a significant decline in lumbar instrumentation among the younger age groups (Fig. 3i, Table 2). Lastly, there was a significant increase in cervical instrumentation among ≥ 80 year olds with a ten-year increase of 4.2 surgeries per 10,000 (Figs. 3f, 4b, Table 2).
Trends in the incidence of spine surgery by age group and categories of interest: a degenerative pathology, all spine regions, b fusion surgeries, all spine regions, c instrumentation surgeries, all spine regions, d degenerative pathology, cervical region, e fusion surgery, cervical region, f instrumentation surgery, cervical region, g degenerative pathology, lumbar region, h fusion surgeries, lumbar region, i instrumentation surgery, lumbar region
Spine surgeon trends
For 539 (1.1%) of the 49,575 surgeries, there was no unique neurosurgeon or orthopaedic surgeon code available. These “unassigned” surgeries were evenly distributed across the study period. The number of unique orthopaedic surgeons and neurosurgeons performing spine surgery each year was determined from the remaining 49,036 surgeries.
There was a reduction in the number of orthopaedic spinal surgeons billing to the scheme per year, from 142 in 2008 to 127 in 2017. This was accompanied by a downward trend in the ratio of orthopaedic spinal surgeons to adult scheme members (Fig. 5a) (slope = − 0.48, R2 = 0.86, p < 0.001). Overall, the ratio of orthopaedic spinal surgeons to members decreased by 37% from 10.2 per 100,000 members in 2008 to 6.3 per 100,000 members in 2017. In contrast, there was an increase in the number of neurosurgeons billing to the scheme per year, from 106 in 2008 to 130 in 2017. This was accompanied by a minor downtrend trend in the ratio of neurosurgeons to adult members (Fig. 5a) (slope = − 0.14, R2 = 0.68, p = 0.004). Overall, the ratio of neurosurgeons decreased by 13%, from 7.6 per 100,000 in 2008 to 6.5 per 100,000 in 2017.
The median number of index spine surgeries billed to the scheme each year by surgeon specialization is shown in Fig. 5b. The volume of surgeries billed by neurosurgeons remained similar with a median of 27 in 2008 and 26 in 2017. The volume of index surgeries billed by orthopaedic surgeons increased somewhat from 3 in 2008 to 6 in 2017.
Discussion
The first finding of the study was that there was a 13% decrease in the crude incidence of spine surgery among adult members of the largest open medical scheme in South Africa between 2008 and 2017. Age-stratified analysis showed that a significant downward trend was present across all age groups. To gain greater understanding of these high-level trends, the incidence of spine surgery was examined within various categories related to spine surgery utilization.
Increased utilization is typically explained in terms of widened indications for spine surgery along with overuse of imaging, surgeon enthusiasm and financial incentives [13, 14]. The second finding was that there were significant upward trends in the incidence of surgery for lumbar degenerative pathology among 60–79 year olds and cervical degenerative pathology among ≥ 80 year olds, suggesting widened surgical indications and increased use of surgery in the elderly. However, there was a concomitant decline in surgery for lumbar degenerative pathology among 40–59 year olds. These mixed findings are in contrast to existing studies from Finland, Norway and England, which reported an increased incidence of spine surgery for degenerative conditions in all age groups ≥ 40 years old [3, 5, 10]. In the case of ≥ 80 year olds, increased surgery for cervical spine degenerative pathology was in keeping with previous findings [3]. However, the study did not demonstrate an increase in surgery for lumbar degenerative pathology in the elderly as reported elsewhere [5, 10]. One possible explanation may be that widened indications for spine surgery were offset by increased use of outpatient interventions such as pain procedures, steroid injections and physiotherapy, particularly in patients under 60 years old. Unfortunately it was not possible to evaluate this in the current data and trends in outpatient spinal interventions constitute an interesting topic for future study.
Spine surgery utilization has also previously been assessed in terms of fusion surgeries and use of instrumentation, which may partly represent financial incentive towards more costly surgeries. The third finding was that there was there was a significant decline in the incidence of both lumbar fusion and lumbar instrumentation among 40–59 year olds with little change in the use of these techniques among 60–79 year olds. Among ≥ 80 year olds there was a tendency towards increased fusion and a significant upward trend in cervical instrumentation. Thus the findings did not support a noticeable shift towards more costly surgeries, apart from within the small elderly population. The decline in fusion and instrumentation among 40–59 year olds is likely related to the reduced incidence of spinal surgery for lumbar degenerative pathology in this age group. In contrast, a previous study from Norway reported a substantial increase in complex surgeries, including fusion, for lumbar degenerative conditions among older adults and among the elderly in particular [10].
In order for an increase in the incidence of spine surgery to occur, there must be an increase in spine surgery supply as well as in utilization. This would generally require more spine surgeons, more surgeries per surgeon, or both. The role of the spine surgery supply in increased spine surgery utilization has been highlighted in previous studies [1, 3, 15]. For example, in Finland, an increase in the incidence of surgery for cervical spine degenerative disease coincided with a doubling of the number of neurosurgeons, and, in Japan, an increase in the number of spine surgeries between 2003 and 2017 was accompanied by an increase of 61 to 103 surgeries per surgeon per year and an increase in the number of spine surgeons per hospital [1, 3]. Similarly, differences in spine surgeons per capita and the number of hospitals offering spine surgery were cited as an important factor likely underpinning differences in spine surgery utilization between the United States and Canada [15]. In contrast, the current findings did not suggest an increase in spine surgery supply. The majority of spine surgeries were performed by neurosurgeons and both neurosurgeons per capita and the median number of surgeries per neurosurgeon changed relatively little over the study period. Furthermore, there was a reduction in the number of orthopaedic spinal surgeons.
The supply of neurosurgeons in South Africa is largely determined by the availability of registrar posts. Furthermore, it is advocated that neurosurgeons or orthopaedic surgeons intending to practise spine surgery complete a spine surgery fellowship. It is possible that limited registrar posts and fellowships may constrain the supply of spine surgery to a greater extent in South Africa than in developed countries. In addition, not all qualified and/or fellowship-trained surgeons may add to the supply of spine surgery due to emigration, another phenomenon that would be expected to be more prevalent in South Africa than in developed countries [16, 17]. Thus, it is hypothesized that the South African setting may not allow for the increased supply of spine surgery referred to in previous reports [1, 3], in turn limiting the potential for increased spine surgery rates. Lastly, the reduction in orthopaedic spinal surgeons may be partly related to the soaring medical insurance and patient litigation reported in South Africa from 2008 onwards [18, 19]. These developments may have deterred orthopaedic surgeons from practicing spine surgery whereas spinal surgery is covered by the high medical insurance for which neurosurgeons are already liable.
A notable limitation of the study was that it was based on data collected for administrative purposes and was dependent on the accuracy of the pathology and procedure codes provided. Pathology, in particular, may be coded in slightly different ways and coding practices may change over time. For example, the apparent increase in stenosis reported over the study period is likely to reflect a shift in ICD-10 coding rather than a true shift in pathology profile; such shifts may sometimes occur due to funder reimbursement policies. Nevertheless, this is unlikely to affect the overall findings of the study. The findings relate to presumed index surgeries billed to a single scheme; while they provide a representation of the private sector, they do not indicate total spine surgeries or total surgeon volume. Finally, the regression models applied were intended to provide an objective measure of trend rather than achieve the optimal fit for the data. Some models achieved significance with very small slope coefficients, suggesting statistical rather than “real-world” significance in such cases.
Conclusion
Spine surgery in the South African private healthcare sector bears some similarity to developed countries in that it is dominated by elective procedures for degenerative pathology. However, the current findings did not reflect the marked increases in the utilization of spine surgery reported elsewhere. It is hypothesized that this contrast may be partly related to the supply of spinal surgery in different settings. Future studies may investigate the incidence of non-surgical management of spine pathology, holistic evaluation of spine surgeon numbers and surgery volumes, and outcomes following spinal surgeries in South Africa. Furthermore, studies on rates of spine surgery from other developing countries would also be of interest and would allow for a more global view of spine surgery trends .
References
Kobayashi K, Sato K, Kato F et al (2022) Trends in the numbers of spine surgeries and spine surgeons over the past 15 years. Nagoya J Med Sci 84:155–162. https://doi.org/10.18999/nagjms.84.1.155
Kim P, Kurokawa R, Itoki K (2010) Technical advancements and utilization of spine surgery–international disparities in trend-dynamics between Japan, Korea, and the USA. Neurol Med Chir 50:853–858. https://doi.org/10.2176/nmc.50.853
Kotkansalo A, Leinonen V, Korajoki M et al (2019) Surgery for degenerative cervical spine disease in Finland, 1999–2015. Acta Neurochir 161:2147–2159. https://doi.org/10.1007/s00701-019-03958-6
Xu Y, Yen D, Whitehead M et al (2019) Use of instrumented lumbar spinal surgery for degenerative conditions: trends and costs over time in Ontario, Canada. Can J Surg 62:393–401. https://doi.org/10.1503/cjs.017016
Sivasubramaniam V, Patel HC, Ozdemir BA, Papadopoulos MC (2015) Trends in hospital admissions and surgical procedures for degenerative lumbar spine disease in England: a 15-year time-series study. BMJ Open 5:e009011. https://doi.org/10.1136/bmjopen-2015-009011
Deyo RA, Gray DT, Kreuter W et al (2005) United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 30:1441–1445. https://doi.org/10.1097/01.brs.0000166503.37969.8a
Weinstein JN, Lurie JD, Olson PR et al (2006) United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine (Phila Pa 1976) 31:2707–2714. https://doi.org/10.1097/01.brs.0000248132.15231.fe
Machado GC, Maher CG, Ferreira PH et al (2017) Trends, complications, and costs for hospital admission and surgery for lumbar spinal stenosis. Spine (Phila Pa 1976) 42:1737–1743. https://doi.org/10.1097/BRS.0000000000002207
Martin BI, Mirza SK, Spina N et al (2019) Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976) 44:369–376. https://doi.org/10.1097/BRS.0000000000002822
Grotle M, Småstuen MC, Fjeld O et al (2019) Lumbar spine surgery across 15 years: trends, complications and reoperations in a longitudinal observational study from Norway. BMJ Open 9:e028743. https://doi.org/10.1136/bmjopen-2018-028743
Council for Medical Schemes (2017) Council for Medical Schemes annual report 2017–2018. https://www.medicalschemes.co.za/publications/#2009-2012-wpfd-2017-18-annual-report. Accessed 25 Aug 2021
Discovery Health Medical Scheme results highlights for the six months ended 31 December (2017). https://www.discovery.co.za/medical-aid/annual-reports-and-financials. Accessed 11 Oct 2022
Bederman SS, Rosen CD, Bhatia NN et al (2012) Drivers of surgery for the degenerative hip, knee, and spine: a systematic review. Clin Orthop Relat Res 470:1090–1105. https://doi.org/10.1007/s11999-011-2004-x
Lurie JD, Birkmeyer NJ, Weinstein JN (2003) Rates of advanced spinal imaging and spine surgery. Spine (Phila Pa 1976) 28:616–620. https://doi.org/10.1097/01.BRS.0000049927.37696
Cram P, Landon BE, Matelski J et al (2019) Utilization and outcomes for spine surgery in the United States and Canada. Spine (Phila Pa 1976) 44:1371–1380. https://doi.org/10.1097/BRS.0000000000003083
Crush J, Pendleton W (2011) Brain flight: the exodus of health professionals from South Africa. Int J Migr Health Soc Care 6:3–18. https://doi.org/10.5042/ijmhsc.2011.0059
Labonté R, Sanders D, Mathole T et al (2015) Health worker migration from South Africa: causes, consequences and policy responses. Hum Resour Health 13:1–16. https://doi.org/10.1186/S12960-015-0093-4/FIGURES/7
Bateman C (2011) Medical negligence pay-outs soar by 132%–subs follow. S Afr Med J 101:216–218. https://doi.org/10.7196/SAMJ.4881
East S, Snyckers C (2011) Orthopaedic litigation in South Africa: a review of the Medical Protection Society data base involving orthopaedic members over the last 10 years. S Afr Med J 10:71–79
Acknowledgements
The anonymised data analysed for the purposes of this study was obtained from Discovery Health Medical Scheme, registration number 1125, and with the support and assistance of Discovery Health (Pty) Ltd, an accredited administrator and managed care provider for medical schemes. Discovery Health Medical Scheme and Discovery Health (Pty) Ltd had no influence on the methodology used, analysis completed and conclusions drawn in this research, and the outcome of the research is entirely independent from Discovery Health Medical Scheme and Discovery Health (Pty) Ltd.
Funding
Open access funding provided by Stellenbosch University. No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
Conceptualization [TM, JD], Methodology [TM, JD], Formal analysis [TM], Writing–Original draft [TM], Writing–Review and editing [RD, AV, JD].
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflict of interest to declare.
Ethical approval
The study was approved by the Health Research Ethics Committee of Stellenbosch University (reference number N20/11/118) and by the Research Governance Committee of the medical scheme. Furthermore, the study was performed in line with the principles of the Declaration of Helsinki. A waiver of informed consent was granted by the ethics committee due to the use of retrospective, anonymized data. The dataset analysed during the study is not publicly available due to a confidentiality agreement signed with the medical scheme. The data may be made available upon reasonable request, pending consultation with the scheme.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mann, T.N., Dunn, R.N., Vlok, A.J. et al. Incidence of spine surgery in the South African private healthcare sector: ten-year trends within a large open medical scheme. Eur Spine J 32, 3015–3022 (2023). https://doi.org/10.1007/s00586-023-07816-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07816-z