Abstract
We aimed to evaluate the association between periodontitis in the upper jaw and chronic rhinosinusitis (CRS) using the nationwide Korean National Health and Nutrition Examination Survey (KNHANES) data. In this cross-sectional study, data of KNHANES participants enrolled between 2008 and 2012 were reviewed. Periodontitis of the upper teeth was diagnosed by dentists according to the community periodontal index with standardized methods. CRS was diagnosed by otorhinolaryngologists according to the European Position Paper on Rhinosinusitis and Nasal Polyps 2020 with nasal endoscopy findings. We also evaluated the association between periodontitis and CRS according to smoking and drinking status. Univariate and multivariate logistic regression analyses were performed. Overall, 28,761 participants were eligible for analysis, and 210 were diagnosed with CRS. Periodontitis was associated with CRS diagnosis (odds ratio [OR] = 1.391, 95% confidence interval [CI] = 1.013–1.912). Non-drinkers showed no significant association between periodontitis and CRS (OR = 1.142, 95% CI 0.746–1.749). However, among drinkers, periodontitis was significantly associated with CRS (OR = 1.733, 95% CI 1.091–2.753). The number of smokers with CRS was not statistically sufficient and a logistic regression model based on smoking status could not be generated. Individuals with periodontitis in the upper jaw may need to consult an otorhinolaryngologist for comorbid CRS especially according to drinking status.
Similar content being viewed by others
Introduction
Chronic rhinosinusitis (CRS) is defined as an inflammatory disease of the paranasal sinuses that lasts for more than 12 weeks1. The typical clinical manifestations of CRS include nasal discharge, nasal congestion, pain or sense of fullness around the cheeks or forehead, and reduction or loss of smell2. According to recent studies, CRS is prevalent in approximately 10% of the general population, impacting quality of life and increasing the burden of healthcare costs worldwide3,4,5. CRS is primarily treated with medications, and in case of failure of drug interventions, surgical treatment is considered6.
Numerous factors contribute to the pathophysiology of CRS, including host-related and environmental factors7. Previous studies have shown that smoking induces chronic irritation of the upper respiratory epithelium, which is suggestive of its adverse influence on CRS8. Additionally, patients with CRS who have nasal polyps have a high tendency to present with hypersensitivity to alcohol9. Since the etiology of CRS is multifactorial, some patients have persistent or recurrent disease even after aggressive treatment10. Therefore, understanding the pathophysiology of this disease and identifying any relevant intrinsic or extrinsic risk factors are important.
Odontogenic sinusitis accounts for approximately 10% of all CRS cases, most of which are caused by iatrogenic trauma during dental surgery11. In addition to the direct spread of inflammation, as observed in dental implant procedures, chronic periodontitis can also cause CRS through an increase in systemic inflammatory markers12,13. Previous epidemiological studies that have analyzed the correlation between CRS and periodontitis using Korean National Health Insurance Service-Health Screening Cohort data have the following limitation: periodontitis and CRS have been defined on the basis of inconsistent diagnostic measures and by different physicians12,14.
Therefore, in this study, we investigated the correlation between periodontitis and CRS using the Community Periodontal Index (CPI), which was recorded by dentists. To diagnose CRS, otorhinolaryngologists examined the symptoms and endoscopic findings of CRS in each participant. In addition, since smoking and drinking habits are associated with a greater prevalence of inflammatory diseases in patients with periodontitis, we further analyzed the relationship between periodontitis and CRS among smokers and non-smokers and among drinkers and non-drinkers15.
Material and methods
Study population
In this study, data from the Korean National Health and Nutrition Examination Survey (KNHANES) from 2008 to 2012 were used. The KNHANES is a nationwide survey conducted annually in South Korea by the Korea Centers for Disease Control and Prevention to analyze current trends in the health and nutritional status of the population. On the basis of the national census data, approximately 10,000 people were enrolled to represent the Korean population using a random sampling method. They were interviewed, filled out questionnaires on their nutritional and health status, and underwent physical examinations by healthcare providers. The KNHANES survey results are posted on the website every year and can be accessed and used for academic research. Between 2008 and 2012, 392 sampling survey districts were extracted, and 8400 household members participated in the survey. Health surveys and examinations were conducted at the mobile examination center, and nutrition surveys were conducted through direct visits to the target households.
Between 2008 and 2012, 150 otorhinolaryngologists from 47 institutions recorded detailed medical interviews and endoscopic findings. Since objective diagnostic findings, such as endoscopy findings, are essential for diagnosing CRS, we used the data from the above-mentioned period in this study. Participants who are 18 years old or more were enrolled for the study.
Diagnosis of chronic rhinosinusitis according to the European Position Paper on Rhinosinusitis and Nasal Polyps 2020 guidelines
We followed the European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS) 2020 guidelines as diagnostic criteria when selecting the participants for the CRS group. According to these guidelines, two of the following four symptoms must be present for diagnosing CRS: nasal obstruction, rhinorrhea, facial pain/pressure, and loss of smell. In addition, inflammation of the sinuses must be proven through objective findings using nasal endoscopy. From 2008 to 2012, additional analyses using nasal endoscopy were performed in the KNHANES by otorhinolaryngologists.
Dental examination
Dental examination was performed by public health dentists, who measured the depth of the periodontal pocket using a periodontal probe with a 0.5 mm ball tip. They scored the dental health status of each individual using the CPI, which is an indicator of periodontal disease severity. Scores are assigned on the basis of the following five criteria: healthy periodontal tissue (CPI 0), gingival bleeding on probing (CPI 1), presence of tartar (CPI 2), and depth of periodontal pocket (probing depth of 4–5 mm indicates CPI 3 and that of ≥ 6 mm indicates CPI 4). CPI scores of 1 and 2 indicate gingivitis, and those of 3 and 4 indicate periodontitis, which require more aggressive treatment. In the KNHANES, CPI 3 and 4 groups were defined as having periodontal diseases. Examiners checked the molars and premolars of the upper and lower jaws on the left side to assign scores. The right side examination was conducted with the same method. We excluded the data of central incisor, lateral incisor and canine teeth. Our study specifically analyzed the correlation between periodontitis in upper teeth and CRS; therefore, in this manuscript, the term “CPI positive” will be used to indicate CPI scores 3 or 4 in the upper teeth, regardless of the presence of periodontitis in the lower teeth.
Statistical analyses
In this study, the analysis was conducted using Statistical Analysis System version 9.4 (SAS Institute, Inc., Cary, NC, USA). The baseline characteristics of the participants included age, sex, income, education level, occupation, drinking, smoking, residence, obesity, hypertension, and diabetes mellitus; these were used to adjust for confounding factors. These characteristics were analyzed using chi-square tests and one-way analyses of variance to determine the differences between the normal and CRS groups. Logistic regression analyses were performed to estimate the association between variables, including the odds ratio (OR) and 95% confidence interval, and the significance level was set at p < 0.05. The confounding variables were adjusted using multivariable logistic regression analysis to exclude the potential relevant variables. The significance level of the multivariable analysis was set at p < 0.25.
As a secondary analysis, we created drinker and non-drinker subgroups, as well as smoker and non-smoker subgroups, and analyzed the correlation between the CPI score and CRS in each group.
Ethical considerations
All methods in this study was conducted according to the guidelines laid down in the Declaration of Helsinki. The KNHANES has been reviewed and approved annually by the Research Ethics Review Committee of the KCDC (IRB No. 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, and 2012-01EXP-01-2C). Written informed consent was obtained from all participants of the KNHANES.
Ethics approval and consent to participate
This study is based on the previously conducted research data of National Research Foundation of Korea which are open to the public. Therefore, the ethical approval and patient consent were not needed in this study.
Results
Association between CRS and CPI scores
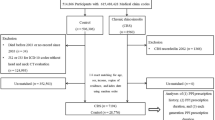
Of 43,266 participants in the KNHANES study between 2008 and 2012, only 28,761 were eligible for inclusion after excluding participants aged < 18 years, with missing data, or with a nasal mass or tumor according to endoscopic findings. Of the final 28,761 participants, 28,551 were in the control group, and 210 (0.73%) met the criteria of the EPOS 2020 guidelines for CRS (Fig. 1).
The minimum sample size required for the logistic regression analysis used in this study was calculated using the G*power program, based on the variable with the smallest effect size among the factors influencing periodontitis in the previous study16. With a two-tailed test, where OR = 1.22, R2 other X = 0.7, significance level α = 0.05, and power of 0.80, the minimum sample size was 4794 individuals. Among the subjects in the KNHANES, the final number of participants who met the inclusion criteria was 28,761, which is sufficiently larger than the calculated minimum sample size.
The baseline characteristics of all participants included basic information for each group, such as age, sex, education level, occupation, and residence, in addition to obesity, hypertension, diabetes, drinking, and smoking (Table 1). In the univariate analysis, age, sex, income, education, drinking, smoking, residency, and CPI showed significant differences (p < 0.25). These variables were analyzed using multivariable logistic regression. In this analysis, age, sex, income, education level, residence, drinking, and smoking were not significantly different between the normal and CRS groups. Only the proportion of patients with CRS with CPI positivity was significantly higher than that of the normal group (p < 0.05) (Table 2).
Alcohol and smoking
The participants were divided into drinking and non-drinking groups, with 13,225 drinkers and 14,657 non-drinkers. In the drinking group, 91 patients met the criteria for CRS diagnosis, and 14,566 were classified as normal. Among these participants, we analyzed the ORs of age, sex, income, residency, obesity, hypertension diagnosis, and CPI in the CRS and normal groups. Only the CPI was significantly higher in the CRS group than in the normal group, with an OR of 1.733 (95% confidence interval = 1.091–2.753) (p = 0.02) (Table 3). Using the same method, in the non-drinking group, the subgroup of CRS had 111 participants, and the normal group had 13,124 participants. The analysis items were income, education, smoking, residence, hypertension diagnosis, and CPI. Unlike in the drinking group, the difference in the CPI between the two subgroups was not statistically significant among non-drinkers.
We also divided the patients into smoker and non-smoker groups; 5840 participants were smokers, and 22,049 were non-smokers. Among the smoker group, 48 satisfied the diagnostic criteria of CRS, and this number was too small to be modeled; therefore, statistical analysis was not possible.
Discussion
Among 28,761 participants of the KNHANES from 2008 to 2012, periodontitis of the upper jaw was significantly associated with CRS, showing a high OR in the multivariable logistic regression analysis. After analyzing 14,657 participants, this tendency was found to be more prominent among the drinker group than among the non-drinker group. The association between CRS and periodontitis among the smokers was not statistically analyzed owing to the small sample size.
This is the first study on CRS conducted using the nationwide large-scale KNHANES, which represents the health and nutritional status of the general Korean population17. Although the correlation between CRS and periodontitis has been analyzed before, this study is meaningful because both dentists and otorhinolaryngologists were involved in the diagnosis of the participant’s current status, and it was not dependent on the self-questionnaire or diagnostic codes. Therefore, the participants of this study were diagnosed by specialists, and the diagnostic criteria for CRS were based on the EPOS 2020 guidelines.
Odontogenic sinusitis is an inflammatory disease of the sinonasal mucosa induced by dental pathology, and it often results from previous dental procedures or trauma that induces maxillary sinus inflammation11. The most common cause of odontogenic CRS is iatrogenic injury of the mucoperiosteum or Schneiderian membrane, which allows inflammation to mechanically spread to the maxillary sinus18. This etiology accounts for approximately 65.7% of odontogenic sinusitis cases19. Hence, odontogenic sinusitis has been the focus when examining the effects of iatrogenic trauma in the upper tooth region on CRS development. We hypothesized that not only direct trauma from iatrogenic dental procedures, but also the spread of inflammation from periodontitis can indirectly induce microscopic structural changes in the Schneiderian membrane. Since the participants with periodontitis in this study included those with dental inflammation and not just those with iatrogenic damage, the findings suggest that periodontitis unassociated with iatrogenic injury could also affect the occurrence of CRS.
The inflammatory condition of the bony compartment could explain the association between CRS and periodontitis. Osteomyelitis is an inflammatory condition of the bone, beginning in the medullary cavity and extending to the bony cortex. Patients with chronic periodontitis have a high tendency to develop osteomyelitis20,21. The proposed etiology is the biofilm produced by oral anaerobes, which can even influence inflammation in distant bones, such as the femur, through the blood stream22. Moreover, periodontitis can induce pathological changes in tissues adjacent to the oral cavity, such as the upper jaws, with great ease, leading to chronic inflammation of the paranasal sinuses.
Anatomical proximity may also explain the association between CRS and periodontitis. A similar mechanism can be found in deep neck infection, which is characterized by cellulitis or abscess formation in the cervical spaces and fascial plane23. The most common cause of deep neck infection is dental infection, which spreads along the connective tissue from the oral cavity to the adjacent cervical spaces24. Similarly, both the maxillary gingiva and sinus are in proximity to the maxillary bone, enabling the easy spread of inflammation from one structure to the other through the maxillary bone. We speculate that the commonality of inflammatory conditions and anatomical proximity may have created a link between CRS and periodontitis.
In a previous study, chronic alcohol consumption was found to have systemic effects and to induce multifocal osteonecrosis25. Osteonecrosis refers to the destruction of bony compartments, such as bone cells and marrow, leading to a prominent chronic inflammatory state26. According to some studies, osteonecrosis induces inflammation of the synovial membrane, activating immune cells in the joints, even in patients without confounding symptoms of arthritis27. Since the oral mucosa of the upper jaw comes in direct contact with alcohol, necrotic changes in the bony structure or mucosa, including the Schneiderian membrane, are more likely to occur. Alcohol-induced necrotic changes in the maxilla may cause an inflammatory response like CRS, which is similar to the pathogenesis of arthritis, thereby inducing immune cell responses in the joints of patients with systemic osteonecrosis.
Meanwhile, although there was no independent contribution in the multivariable logistic regression analyses, residence, education level, and household income showed statistically significant difference between the participants with CRS and control in the baseline characteristics analysis. In the international guideline the aggravating or contributing effect of the demographic factors were reviewed and it has been stated that the causal link cannot be clearly established28. As for our data from the KNHANES, the effect of atmospheric exposure could have been more significant for participants who live in rural area than urban area. Several studies reported that air pollutants such as particulate matter with aerodynamic diameters ≤ 10 µm (PM10) in the atmosphere has association with CRS29,30. From the results of this study, it is rather difficult to define the exact causal relationship between CRS and the baseline demographic factors. However, the multivariable regression analysis showed that after correction of the other factors, CPI was the independent factor associated with CRS, and it can be assumed that worse periodontal status could have been related to rural area residency, lower household income, or lower education level.
A limitation of this study is that a causal relationship between CRS and periodontitis could not be identified owing to the cross-sectional design. Further, KNHANES data from only 2008 to 2012 include the endoscopic findings of otorhinolaryngologists. After 2013, no endoscopic findings are available, which prevents analysis of the current trend of the relationship between CRS and CPI. Moreover, although specialists’ endoscopic findings were used to diagnose CRS, some patients may have had polyps or discharge in the posterior part of the nasal cavity (for example, the posterior ethmoid sinus or sphenoid sinus), which are difficult to detect and may have remained undiagnosed. Computed tomography of the paranasal sinuses could help identify participants with CRS more accurately. Finally, CPI measurements are affected by the pressure applied during probing and by inter-examiner variability (approximately 66% for sensitivity and 85% for specificity)31, which may have contributed to errors, considering that KNHANES is a large-scale study. Another limitation regarding dental examination is that CPI was not graded for each tooth but according to the four areas of oral cavity; upper right, upper left, lower right, and lower left.
Conclusions
We analyzed data of 28,761 KNHANES participants enrolled between 2008 and 2012 using multivariable logistic regression. In this study, CRS was diagnosed using the EPOS 2020 guidelines, considering patients’ symptoms and endoscopic findings, and periodontitis was defined on the basis of CPI scores. These results demonstrated a significant association between CRS and periodontitis. We also divided the patients into subgroups according to their smoking and drinking status. Among drinkers, the CPI was significantly high in patients with CRS, while CPI and CRS show no statistically significant association among non-drinkers. Meanwhile, the subgroup of smokers was not analyzed because of the small sample size. Therefore, even in the absence of a history of invasive dental procedures, periodontitis could influence the development of CRS; this indicates that appropriate oral hygiene care might lower the incidence of CRS.
Data availability
The KNHANES data are open to the public; therefore, any researcher can obtain the raw data by requesting it on the website (https://knhanes.kdca.go.kr/knhanes/eng/index.do).
Abbreviations
- CRS:
-
Chronic rhinosinusitis
- CPI:
-
Community periodontal index
- EPOS:
-
European Position Paper on Rhinosinusitis and Nasal Polyps
- KNHANES:
-
Korean National Health and Nutrition Examination Survey
- CI:
-
Confidence interval
- OR:
-
Odds ratio
References
Xu, X., Reitsma, S., Wang, Y. & Fokkens, W. J. Highlights in the advances of chronic rhinosinusitis. Allergy 76, 3349–3358 (2021).
Fokkens, W. J. et al. Executive summary of EPOS 2020 including integrated care pathways. Rhinology 58, 82–111 (2020).
Hong, P., Pereyra, C. A., Guo, U., Breslin, A. & Melville, L. Evaluating complications of chronic sinusitis. Case Rep Emerg Med 2017, 8743828 (2017).
Shaghayegh, G. et al. Chronic rhinosinusitis, S. aureus biofilm and secreted products, inflammatory responses, and disease severity. Biomedicines 10, 1362 (2022).
Hamilos, D. L. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol 128, 693–707 (2011) (quiz 708-699).
Dharmarajan, H., Falade, O., Lee, S. E. & Wang, E. W. Outcomes of dupilumab treatment versus endoscopic sinus surgery for chronic rhinosinusitis with nasal polyps. in Int Forum Allergy Rhinol (2021).
Matsuwaki, Y. et al. Chronic rhinosinusitis: Risk factors for the recurrence of chronic rhinosinusitis based on 5-year follow-up after endoscopic sinus surgery. Int. Arch. Allergy Immunol. 146(Suppl 1), 77–81 (2008).
Tamashiro, E., Cohen, N. A., Palmer, J. N. & Lima, W. T. Effects of cigarette smoking on the respiratory epithelium and its role in the pathogenesis of chronic rhinosinusitis. Braz. J. Otorhinolaryngol. 75, 903–907 (2009).
De Schryver, E. et al. Alcohol hyper-responsiveness in chronic rhinosinusitis with nasal polyps. Clin. Exp. Allergy 47, 245–253 (2017).
van Agthoven, M., Uyl-de Groot, C. A., Fokkens, W. J., van de Merwe, J. P. & Busschbach, J. J. Cost analysis of regular and filgrastim treatment in patients with refractory chronic rhinosinusitis. Rhinology 40, 69–74 (2002).
Little, R. E., Long, C. M., Loehrl, T. A. & Poetker, D. M. Odontogenic sinusitis: A review of the current literature. Laryngoscope Investig. Otolaryngol. 3, 110–114 (2018).
Keller, J. J., Wu, C. S. & Lin, H. C. Chronic rhinosinusitis increased the risk of chronic periodontitis: A population-based matched-cohort study. Laryngoscope 123, 1323–1327 (2013).
Aldaham, S., Foote, J. A., Chow, H. H. & Hakim, I. A. Smoking status effect on inflammatory markers in a randomized trial of current and former heavy smokers. Int. J. Inflamm. 2015, 439396 (2015).
Byun, S. H. et al. Increased risk of chronic periodontitis in chronic rhinosinusitis patients: A longitudinal follow-up study using a national health-screening cohort. J. Clin. Med. 9, 1170 (2020).
Kim, J. W. et al. Rheumatoid arthritis is associated with early tooth loss: Results from Korea National Health and Nutrition Examination Survey V to VI. Korean J. Intern. Med. 34, 1381–1391 (2019).
Genco, R. J. & Borgnakke, W. S. Risk factors for periodontal disease. Periodontology 2000(62), 59–94 (2013).
Kweon, S. et al. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 43, 69–77 (2014).
Zirk, M. et al. Odontogenic sinusitis maxillaris: A retrospective study of 121 cases with surgical intervention. J. Craniomaxillofac. Surg. 45, 520–525 (2017).
Lechien, J. R. et al. Chronic maxillary rhinosinusitis of dental origin: A systematic review of 674 patient cases. Int. J. Otolaryngol. 2014, 465173 (2014).
Hajishengallis, G. & Chavakis, T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat. Rev. Immunol. 21, 426–440 (2021).
Parrish, L. C., Kretzschmar, D. P. & Swan, R. H. Osteomyelitis associated with chronic periodontitis: A report of three cases. J. Periodontol. 60, 716–722 (1989).
Itoh, N. et al. Femoral osteomyelitis caused by oral anaerobic bacteria with mixed bacteremia of Campylobacter rectus and Parvimonas micra in a chronic periodontitis patient: A case report. BMC Infect. Dis. 22, 613 (2022).
Maharaj, S., Ahmed, S. & Pillay, P. Deep neck space infections: A case series and review of the literature. Clin. Med. Insights Ear Nose Throat 12, 1179550619871274 (2019).
Marioni, G. et al. Deep neck infection with dental origin: Analysis of 85 consecutive cases (2000–2006). Acta Otolaryngol. 128, 201–206 (2008).
Matsumoto, K., Ogawa, H. & Akiyama, H. Multifocal osteonecrosis secondary to chronic alcohol ingestion. Case Rep. Orthop. 2015, 137273 (2015).
Goodman, S. B. & Maruyama, M. Inflammation, bone healing and osteonecrosis: From bedside to bench. J. Inflamm. Res. 13, 913–923 (2020).
Rabquer, B. J. et al. Synovial inflammation in patients with osteonecrosis of the femoral head. Clin. Transl. Sci. 2, 273–278 (2009).
Fokkens, W. J. et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 58, 1–464 (2020).
Park, M., Lee, J. S. & Park, M. K. The effects of air pollutants on the prevalence of common ear, nose, and throat diseases in South Korea: A national population-based study. Clin. Exp. Otorhinolaryngol. 12, 294–300 (2019).
Mady, L. J. et al. Air pollutants may be environmental risk factors in chronic rhinosinusitis disease progression. Int. Forum Allergy Rhinol. 8, 377–384 (2018).
Su, C. W., Yen, A. M., Lai, H., Chen, H. H. & Chen, S. L. Receiver operating characteristic curve-based prediction model for periodontal disease updated with the calibrated community periodontal index. J. Periodontol. 88, 1348–1355 (2017).
Acknowledgements
This research was supported by the Statistical Support Project for Writing Medical Papers using the KNHANES at the Korea University Anam Hospital. We thank Editage (www.editage.co.kr) for English language editing.
Funding
This research was supported by the Basic Science Research Program, National Research Foundation of Korea, funded by the Ministry of Science and Technology and the Ministry of Science, ICT and Future Planning (2017R1A2B2003575, NRF-2020R1A2C1006398), the Ministry of Science and ICT (2020R1C1C1012288), Republic of Korea, under the ICT Creative Consilience program (IITP-2023-2020-0-01819) supervised by the IITP (Institute for Information and Communications Technology Planning and Evaluation), and a grant of the Korea Health Technology R&D Project (HI17C0387) (HR22C1302) through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea. This research was also supported by a Korea University grant and a grant from Korea University Medical Center and Anam Hospital, Seoul, Republic of Korea.
Author information
Authors and Affiliations
Contributions
J.K. and M.H. were major contributors in writing the manuscript, interpreted the result and design the study concept Y.J. analyzed the statistical data using the raw materials. B.C. and D.L. investigated the background and imported main data from the raw materials. S.L. substantively revised the work, and T.K. the corresponding author have made substantial contributions to the concept and study design.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kwak, J., Han, M., Jeong, Y. et al. Periodontitis of maxillary teeth screened by community periodontal index is associated with chronic rhinosinusitis defined by EPOS 2020 guideline. Sci Rep 13, 17722 (2023). https://doi.org/10.1038/s41598-023-43474-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-43474-3
- Springer Nature Limited