Abstract
Males have higher tuberculosis incidence and mortality rates than females. This study aimed to assess how sex differences in tuberculosis incidence and mortality could be explained by sex differences in HIV, antiretroviral treatment (ART) uptake, smoking, alcohol abuse, undernutrition, diabetes, social contact rates, health-seeking patterns, and treatment discontinuation. We developed an age-sex-stratified dynamic tuberculosis transmission model and calibrated it to South African data. We estimated male-to-female (M:F) tuberculosis incidence and mortality ratios, the effect of the abovementioned factors on the M:F ratios and PAFs for the tuberculosis risk factors. Over the period 1990–2019, the M:F ratios for tuberculosis incidence and mortality rates persisted above 1.0, and the figures reached 1.70 and 1.65, respectively, by the end of 2019. In 2019, HIV contributed greater increases in tuberculosis incidence among females than males (54.5% vs. 45.6%); however, females experienced more reductions due to ART than males (38.3% vs. 17.5%). PAFs for tuberculosis incidence due to alcohol abuse, smoking, and undernutrition, in men were 51.4%, 29.5%, and 16.1%, respectively, higher than females (30.1%, 15.4%, and 10.7%, respectively); the PAF due to diabetes was higher in females than males (22.9% vs. 17.5%). Lower health-seeking rates in males accounted for a 7% higher mortality rate in men. The higher burden of tuberculosis in men highlights the need to improve men’s access to routine screening and ensure earlier diagnosis. Sustained efforts in providing ART remain critical in reducing HIV-associated tuberculosis. Additional interventions to reduce alcohol abuse and tobacco smoking are also needed.
Similar content being viewed by others
Introduction
Globally, males experience higher tuberculosis incidence and mortality than females1,2. The male-to-female (M:F) tuberculosis incidence ratio varies by geographic region ranging between 1.1 and 2.51. A meta-analysis of 39 prevalence surveys conducted in 28 countries estimated males to have 2.21 times higher tuberculosis prevalence than females3. Sex disparities in the burden of tuberculosis are driven by multiple factors, including socio-behavioural and biological differences that directly or indirectly affect the risk of exposure to Mycobacterium tuberculosis, acquiring latent infection, or developing active disease4. Biological hypotheses suggest that female sex hormones may protect against susceptibility to infection and the development of tuberculosis disease5. Males may be more exposed to additional risk factors for tuberculosis such as tobacco smoking and alcohol abuse6,7,8. Other conditions that increase susceptibility to tuberculosis disease include HIV, diabetes and undernutrition9,10. These risk factors increase the likelihood of developing tuberculosis by suppressing cell-mediated immunity11,12 and explain a considerable amount of the burden of tuberculosis at the population level2.
HIV, the most potent tuberculosis risk factor, is also distributed differently by sex, with a heavier burden among females than males13. However, compared to females, males are less likely to get tested for HIV and have lower antiretroviral therapy (ART) initiation rates14. Several studies have shown that the age-sex distribution of tuberculosis reflects that of the HIV epidemic15,16,17,18. However, limited studies have quantified the effect of the evolving HIV epidemic and the impact of the rollout of ART on the sex distribution of tuberculosis.
Several analyses have explored explanations for the excess burden of tuberculosis in men. Horton et al. showed that in Vietnam and Malawi, men had higher rates of tuberculosis incidence and longer delays to treatment19. Other studies have suggested that the frequent social contacts men have with other men20, combined with their higher rates of tuberculosis incidence3, likely amplifies their burden of tuberculosis21,22. The Global Burden of Disease Study (GBD) 2019 demonstrated the contribution of smoking, alcohol, and diabetes to sex disparities in tuberculosis mortality, showing that eliminating these risk factors would reduce the global tuberculosis mortality M:F ratios from 1.97 to 1.282.
In South Africa, the male tuberculosis prevalence is approximately 1.6 times that in females23. However, limited analyses have evaluated how modifiable risk factors explain sex disparities at a population level. Understanding the factors that drive sex disparities and the overall burden of tuberculosis is essential for identifying where tuberculosis control efforts need to focus. The specific objectives of this study were to 1) quantify the effect of the evolving HIV epidemic and the impact of the rollout of ART on the sex distribution of tuberculosis incidence and mortality over the period 1990–2019; 2) estimate the sex-specific population attributable fraction (PAF) for undernutrition, smoking, alcohol, diabetes and HIV (2019); 3) to estimate the impact of sex differentials in a) tuberculosis health seeking b) HIV testing and ART initiation, c) social mixing patterns and d) tuberculosis treatment retention.
Methods
The tuberculosis model structure
We developed an age-sex-stratified deterministic compartmental model of the tuberculosis and HIV epidemics for the South African adult population (aged 15 + years). The core tuberculosis states were modelled following conventions described by previous studies19. The risk of infection depends on the mean contact rates, proportions of contacts in each age and sex group24, the probability of transmission per contact, and the prevalence of infectious tuberculosis. Transitions between states include tuberculosis infection, progression to tuberculosis disease, natural recovery, diagnosis and treatment initiation (Fig. 1). The outcomes we modelled included cure and treatment failure, and death on treatment, where the rates were estimated from electronic tuberculosis treatment register (ETR) for drug-susceptible tuberculosis (which used different definitions, as shown in Supplementary table 11)25,26,27. Following cure by tuberculosis treatment, two post-treatment states are defined: short-term (within six months after cure) and long-term (six or more months after cure). In both states, individuals are at risk of reinfection, whereas in the short-term post-treatment state, individuals are at a greater risk of recurrent TB due to relapse28.
The tuberculosis model was integrated within the Thembisa HIV model29. The model is also age-sex-stratified, and the HIV epidemic is simulated dynamically from 1985. HIV-infected sub-populations are further stratified by HIV testing history, CD4 count, and duration since ART initiation. This model also captures changes in the ART guidelines over time and is calibrated to South African HIV data29. HIV is assumed to affect the tuberculosis natural history parameters. These HIV effects are modelled as relative risks, depending on CD4 count and receipt of ART.
To capture age and sex differences in tuberculosis incidence, we applied the cumulative multiplicative effect of selected risk factors (alcohol abuse, smoking, undernutrition, and poorly controlled diabetes) to rates of progression to tuberculosis disease. We defined undernutrition as having a body mass index (BMI) < 18.5 kg/m230, smoking as those currently smoking tobacco products and accounted for the effects of current smoking and duration of smoking31, alcohol abuse as consuming at least 40 g of alcohol on a single day8, and diabetes as having HbA1c > 6.5% or Fasting Blood Glucose > 120 mg/dl30. These risk factors were selected based on evidence for their effect on developing tuberculosis disease and data reflecting their relatively high prevalence in South Africa (supplementary material). We obtained the age-sex-stratified prevalence of these risk factors from surveys7,30. Estimates for the relative effect of these risk factors were obtained from published studies8,9,10,11,31 and were varied in the calibration process to account for uncertainty around them.
The assumed health-seeking patterns in the model were based on South African studies. We assumed different health facility attendance rates for individuals: 1) with tuberculosis, attending health facilities due to tuberculosis-related symptoms; 2) without tuberculosis, attending due to other health conditions; and 3) without tuberculosis, attending due to tuberculosis-like symptoms. In addition, we assumed that females were more likely to seek care than males3, HIV-infected individuals had higher health seeking rates than HIV-uninfected individuals32, and smear-positive individuals experienced more tuberculosis symptoms than smear-negative individuals33. We also modelled the specificity and sensitivity of the diagnostic algorithm implemented in the model.
Once individuals start the six-month tuberculosis treatment course, the following outcomes were considered: cure, failure, discontinuation, and death. Males were assumed to have higher treatment discontinuation rates than females. Although the base rates of tuberculosis mortality on treatment were initially set the same in males and females, these base rates were adjusted to reflect sex differences in health-seeking patterns. We based treatment outcome assumptions on the electronic tuberculosis treatment register (ETR.net) (supplementary material)27.
Calibration
We used a Bayesian approach to calibrate the model. Prior distributions were set to represent uncertainty in key model parameters (Table 1), and other parameters were fixed at values estimated in earlier model calibrations (supplementary material)34. The main data sources used as calibration targets included sex-stratified recorded numbers of tuberculosis deaths from the vital register for 1997–2016; the ETR for sex-stratified numbers of people initiating drug-susceptible tuberculosis treatment (2004–2016), deaths on treatment (2004–2016), and HIV prevalence in treated tuberculosis patients (2008–2016). We also relied on the National Institute for Communicable Diseases for the number of microbiological tests performed (2004–2012)15. Lastly, we also used the active tuberculosis prevalence data (2018)23.
For the calibration process, likelihood functions were defined to represent the goodness of fit to these calibration targets, allowing for possible under- or over-reporting in the vital register and the ETR data. We simulated posterior distributions numerically using Incremental Mixture Importance Sampling. Importance sampling was used to draw a sample of parameter combinations from regions of the parameter space that yielded the highest likelihood values to generate posterior estimates35. The means for the model estimates were calculated from 1000 posterior samples, and 95% confidence intervals were calculated by taking the 2.5th and 97.5th percentiles of the posterior sample (supplementary material).
Model experiments and outcomes
We estimated M:F ratios for tuberculosis incidence and mortality using the model-estimated rates of new tuberculosis cases and deaths under the baseline scenario (A) which represents the actual tuberculosis and HIV epidemic up to 2019, incorporating sex differences.
To assess the effect of a specific factor on tuberculosis incidence and mortality, and the M:F ratios, we ran individual counterfactual scenarios (B1-11) where each factor was excluded or set equal in males and females in the model, and then compared the model outputs to the outputs obtained in the baseline scenario (A) (Table 2). We calculated sex-stratified percentage increases in tuberculosis incidence and mortality due to HIV; percentage decreases in tuberculosis incidence and mortality due to ART; and tuberculosis incidence PAFs due to smoking, alcohol abuse, undernutrition, diabetes, and HIV. Lastly, we calculated percentage changes in M:F ratios for tuberculosis incidence and mortality under the baseline compared to all counterfactual scenarios.
Ethics
This modelling analysis relied on aggregated data drawn from publicly available data sources which are presented in the supplementary material, and human ethics review was not required.
Results
Overall, the model estimates for tuberculosis prevalence and mortality were consistent with the sex-stratified observed data, with a higher burden in males than females (Fig. 2a,b). Tuberculosis prevalence and deaths rose rapidly during the early 1990s, peaked in the mid-2000s to late-2000s, and subsequently declined until 2019. The 2019 estimated tuberculosis prevalence in males was 1.06% (95% CI 1.0–1.12%) and 0.58% (95% CI 0.56–0.62%) in females. Tuberculosis deaths in 2019 were 32 000 (95% CI 29 000–35 000) in males and 21 000 (95% CI 19 000–22 000) in females.
Sex-specific tuberculosis prevalence and mortality in adults, 1990–2019. (a) Blue and red solid lines represent model estimates for tuberculosis prevalence in males and females, respectively. Black dots represent the 2018 TB prevalence survey with 95% confidence intervals. (b) Blue and red solid lines represent model estimates for tuberculosis mortality in males and females, respectively. Black dots represent recorded mortality, adjusted for the cause of death misclassification and missing fields. All dashed lines represent 95% confidence intervals.
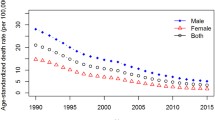
Over the 1990–2019 period, the M:F ratios for tuberculosis mortality and incidence were consistently greater than 1.0. The M:F ratios for tuberculosis incidence and deaths were the highest in the early 1990s (Fig. 3a,b, black); if HIV had not been present in South Africa, the M:F ratios would have remained relatively stable, at around 2.0 (Fig. 3a,b, green). As the HIV epidemic rapidly grew in the South African population, tuberculosis mortality and incidence for both sexes increased (1996–2002). However, females had a more substantial increase in tuberculosis incidence and mortality due to HIV than males (Fig. 3c,d). Consequently, the M:F ratios for tuberculosis incidence and mortality declined and reached their lowest points in the mid-2000s to late-2000s (Fig. 3a,b, black).
The effect of HIV and ART on male-to-female (M:F) ratios for tuberculosis incidence and mortality, 1990–2019. First row: M:F ratios for tuberculosis incidence (a) and mortality (b) (1990–2019). The solid black lines represent the baseline scenario where the effects of HIV and the rollout of ART from the year 2000 were present in the model. The solid green lines represent the counterfactual scenario where HIV was absent from the model. The solid red lines represent the counterfactual scenario where HIV was present, but ART was not introduced. Second row: Percentage increase in tuberculosis incidence (c) and mortality (d) due to HIV. The solid red lines represent female tuberculosis incidence and mortality, and the solid blue lines represent males. Third bottom row: Percentage reduction in tuberculosis incidence (e) and mortality (f) due to ART. All dashed lines represent 95% confidence intervals. ART = antiretroviral therapy; TB = tuberculosis.
If ART had not been rolled out in South Africa, the M:F ratio for tuberculosis incidence and mortality would have continued to decline (Fig. 3a,b, red dotted). However, with the expansion of ART from the mid-2000s, the M:F ratios increased, reaching 1.70 (95% CI 1.65–1.73) for incidence and 1.65 (95% CI 1.59–1.70) for mortality in 2019.
Over time, HIV led to a greater relative increase in tuberculosis incidence and mortality in females than males. In 2019, HIV contributed to a 54.0% (95% CI 53.1–56.4%) and 62.9% (95% CI 60.9–66.0%) increase in female tuberculosis incidence and mortality, respectively (Fig. 3c,d, red). Among males, HIV led to 45.6% (95% CI 44.5–46.1%) increase in tuberculosis incidence and 57.4% (95% CI 55.8–60.7%) increase in tuberculosis mortality (Fig. 3c,d; blue). However, females benefited more from ART than males. In 2019, ART resulted in 38.3% (95% CI 37.1–39.5%) and 52.1% (95% CI 51.2–53.1%) reductions in tuberculosis incidence and mortality among females, respectively (Fig. 3e,f, red). For males, ART led to 17.5% (95% CI 15.8–19.1%) and 28.8% (95% CI 27.3–30.3%) reductions in tuberculosis incidence and mortality, respectively, in 2019 (Fig. 3e,f, blue).
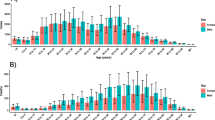
The PAFs of tuberculosis incidence due to alcohol abuse, smoking, and undernutrition were higher in males than females, estimated at 51.4% (95% CI 48.4–54.4%), 29.5% (95% CI 26.5–33.1%) and 16.1% (95% CI 14.1–18.3%) respectively among males in 2019 (Fig. 4); among females, the estimated PAFs were 30.1% (95% CI 28.0–32.2%), 15.4% (95% CI 13.8–17.8%) and 10.7% (95% CI 9.3–12.2%) respectively. On the other hand, the PAFs of tuberculosis incidence due to diabetes and HIV were higher in females (22.9% (95% CI 20.6–25.2%) and 54.5% (95% CI 53.1–56.4%) respectively) than in males (diabetes: 17.5% (95% CI 15.7–19.3%) and HIV: 45.6% (95% CI 44.5–46.9%).
In the counterfactual scenario where HIV was assumed absent, and all other factors' effects were set equal for males and females, the tuberculosis incidence M:F ratio reduced from 1.7 to 1.01, relative to the baseline scenario (40.7% reduction); for mortality, the M:F ratio reduced from 1.65 to 0.93, (43.6% reduction) (Table 3). In the counterfactual scenario where we assumed equal annual rates of HIV testing and ART initiation in males and females, the tuberculosis incidence and mortality M:F ratios reduced by 3.4% and 8.2%, respectively. When we assumed no ART, the tuberculosis incidence and mortality M:F ratios reduced by 25.1% and 32.7%, respectively. In the individual counterfactual scenarios where alcohol abuse, smoking and undernutrition were excluded, the tuberculosis incidence M:F ratios reduced by 30.5%, 16.8% and 6.1%, respectively. On the other hand, excluding HIV and diabetes led to 19.6% and 7.0% increases in the M:F ratios, respectively.
The counterfactual scenario for health-seeking patterns (equal male and female rates) led to a 7.7% decrease in the M:F ratio for TB mortality. When social contact rates were the same in males and females, the M:F ratios for tuberculosis incidence and mortality slightly increased by 3%. Lastly, in the treatment discontinuation counterfactual scenario (male discontinuation rate set at the same value as female rate), there were negligible changes in the M:F ratios for tuberculosis incidence and mortality.
Discussion
Our model suggests that despite variations in the M:F ratios for tuberculosis incidence and mortality over the 1990–2019 period, overall tuberculosis mortality and incidence were consistently higher in males than females. The higher tuberculosis incidence in males may partly be explained by alcohol abuse and smoking, which are highly prevalent in males and increase the risk of developing tuberculosis through weakening cell-mediated immunity11,12. Low ART uptake among men compared to women also explains the excess burden of tuberculosis in males. ART substantially reduced the contribution of HIV to tuberculosis incidence in both sexes; however, higher levels of HIV testing and ART initiation among females compared to males36 led to females experiencing greater relative reductions in tuberculosis due to ART than males. We also showed that health-seeking delays explain the higher mortality among males, while sex differences in social mixing patterns and treatment discontinuation had minor effects on sex disparities in tuberculosis.
HIV had a greater effect on tuberculosis incidence and mortality among females than males due to the higher HIV prevalence in females13. Consequently, the M:F ratios for tuberculosis incidence and mortality declined during the mid-1990s to early 2000s as HIV was rapidly increasing. However, the expansion of the ART program substantially reduced tuberculosis incidence and mortality, and the higher levels of ART coverage in women compared to men36 have meant that male tuberculosis rates have not declined to the same extent as those in women. These findings are consistent with other studies demonstrating that although HIV prevalence was higher among females, males still had a greater burden of tuberculosis than females15,17. Hermans and colleagues showed that HIV led to substantial relative increases in tuberculosis notification rates among females than males between 1993 and 2013; and the scale-up of ART led to substantial declines in females' relative tuberculosis notification rates compared to males17. Altogether, the modelled HIV and ART effects on the sex distribution of tuberculosis support the hypothesis that if HIV removed the protection females have against tuberculosis disease5, ART restored this protection 17.
In contrast with our tuberculosis incidence estimates for 2019, the GBD study estimated higher tuberculosis incidence in females than males for South Africa2. This disparity was attributed to the higher burden of HIV in females than in males 2,13. Differences in methodological approaches and data sources may explain these discrepancies between our estimates and those by the GBD. For instance, the GBD used meta-regression models and relied on mortality data to estimate tuberculosis incidence from mortality-incidence ratios2. In contrast, we used a dynamic transmission model which accounts for the tuberculosis natural history, impact of HIV and interventions.
Nonetheless, our tuberculosis mortality estimates were consistent with the GBD estimates, with higher mortality in males than females. The GBD suggested that the excess tuberculosis mortality in males was mainly due to alcohol abuse and smoking among HIV-negative individuals2. We also found alcohol and smoking to be important contributors to the overall tuberculosis incidence and sex differences. Tuberculosis incidence PAFs due to smoking and alcohol abuse were higher in males than females, and we demonstrated that if smoking or alcohol abuse were removed individually, M:F ratios for tuberculosis incidence would reduce by approximately 17% or 30%, respectively. This reflects the increased exposure males have to these risk factors, which are also likely to increase the progression to tuberculosis disease11,12. On the other hand, because HIV and diabetes are relatively more prevalent in females than males, females had higher PAFs for HIV and diabetes.
In the counterfactual scenario where males' health-seeking rates were increased and set equal to female health-seeking rates, the overall tuberculosis incidence and mortality declined slightly. This counterfactual scenario was associated with a 7% reduction in the M:F ratio for tuberculosis mortality, suggesting that delays to diagnosis and treatment in males may lead to tuberculosis disease severity and death37. Supporting these findings, other studies suggested that compared to females, males are older and sicker when they seek health care3; they are more likely to be lost to follow-up and experience poor outcomes, including treatment failure and death19,37,38. The health-seeking delays in men may be explained by socioeconomic reasons such as the higher rates of employment in men and associated loss of income due to time lost while seeking tuberculosis health care38.
The assumed social mixing counterfactual scenario modestly influenced the tuberculosis incidence and mortality M:F ratios. In this scenario, social mixing proportions and contact rates were the same in men and women. The model estimated slight increases in tuberculosis incidence and mortality in females and declines in males, and the M:F ratios increased moderately. This is due to the higher contact rates in women that we assumed in the baseline scenario. However, in other studies where the social mixing patterns were assumed to be highly sex-assortative, sex disparities in tuberculosis increased20,22. This was mainly due to men having higher rates of social contact with other men who carry a higher tuberculosis prevalence and therefore further increasing the risk of transmission and the burden of tuberculosis among men20,22.
Our model suggests that removing an individual risk factor or equalising males' and females' health-seeking patterns, social contacts, or treatment outcomes at the current levels is insufficient to eliminate sex disparities. However, assuming the HIV epidemic was absent and all the other factors in males and females were the same, the tuberculosis incidence M:F ratios were reduced to 1.01. Some of the remaining differences may be due to other factors such as biological differences that we did not model. For mortality, the M:F ratio reduced to 0.93 (i.e., higher mortality in females). This is possibly because females’ ‘background’ mortality (deaths not related to HIV and tuberculosis, e.g., due to violence) is much lower than in males27,39; and therefore, more females survive to older ages than males. In our model we assumed tuberculosis mortality rates increase with age (Table 1), people in older age groups (55+ years) contribute disproportionately to tuberculosis mortality, and the majority are likely females. The lower female background mortality rates may also explain why in females compared to males, tuberculosis mortality may appear higher relative to background mortality27, although their absolute tuberculosis mortality risk is low.
Our analysis is strengthened by using a tuberculosis and HIV transmission model calibrated to several South African data sources. This dynamic model allowed us to quantify how HIV and ART affected the sex distribution of tuberculosis incidence and mortality over the 1990–2019 period. However, our study has several limitations. First, we did not include all the factors that may drive sex differences in tuberculosis, such as differences in biological susceptibility to tuberculosis disease5, occupational exposures such as mining, or incarceration40,41. Second, we did not model alcohol, smoking, undernutrition and diabetes dynamically; their effects depended on their prevalence in the population, with most of the prevalence estimates calculated from 2016 data7,30. The prevalence of these risk factors may have changed over time. Hence, the estimated PAFs (for 2019) may not accurately represent the historical effect of these risk factors on tuberculosis incidence. For instance, the prevalence of smoking has been on a declining trend42, and diabetes has risen over time43. Another limitation is that it is not clear whether these risk factors affect tuberculosis transmission, the incidence of tuberculosis disease or mortality. However, for simplicity, we have modelled only the effect of these risk factors on tuberculosis incidence. Lastly, we acknowledge the limitation that although some evidence suggests there are sex differences in latent tuberculosis infection (LTBI)44 we did not model sex differences in LTBI, this is partly due to the lack of South African based data on the prevalence of LTBI by sex.
In summary, men have consistently had higher tuberculosis incidence and mortality than women. The excess tuberculosis incidence and mortality in men highlights the need to make health services more accessible to men and address the structural barriers to their retention in tuberculosis and HIV care. Additionally, there is a need for effective interventions that reduce excessive alcohol consumption and tobacco smoking. Lastly, TB incidence can be reduced through better prevention and treatment of diabetes, especially in women45.
Data availability
All data generated or analysed during this study are included in this published article (and its Supplementary Information files).
References
World Health Organization. Global Tuberculosis Report, 2020. (2020).
Ledesma, J. R. et al. Global, regional, and national sex differences in the global burden of tuberculosis by HIV status, 1990–2019: Results from the Global Burden of Disease Study 2019. Lancet Infect. Dis. 3099, 1–20 (2021).
Horton, K. C., Macpherson, P., Houben, R. M. G. J., White, G. & Corbett, E. L. Sex differences in tuberculosis burden and notifications in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 21, 1–23 (2016).
Lienhardt, C. From exposure to disease: The role of environmental factors in susceptibility to and development of tuberculosis. Epidemiol. Rev. 23, 288–301 (2001).
Nhamoyebonde, S. & Leslie, A. Biological differences between the sexes and susceptibility to tuberculosis. J. Infect. Dis. 209, 1 (2014).
Watkins, R. E. & Plant, A. J. Does smoking explain sex differences in the global tuberculosis epidemic?. Epidemiol. Infect. 134, 333–339 (2006).
South Africa Demographic and Health Survey 2016. (2019).
Lönnroth, K., Williams, B. G., Stadlin, S., Jaramillo, E. & Dye, C. Alcohol use as a risk factor for tuberculosis—A systematic review. BMC Public Health 8, 289 (2008).
Al-Rifai, R. H., Pearson, F., Critchley, J. A. & Abu-Raddad, L. J. Association between diabetes mellitus and active tuberculosis: A systematic review and meta-analysis. PLoS ONE 12, 1–26 (2017).
Leung, C. C. et al. Lower risk of tuberculosis in obesity. Arch. Internal Med. 167, 1297–1304 (2007).
O’Leary, S. M. et al. Cigarette smoking impairs human pulmonary immunity to mycobacterium tuberculosis. Am. J. Respir. Crit. Care Med. 190, 1430–1436 (2014).
Rehm, J. et al. The relation between different dimensions of alcohol consumption and burden of disease: An overview. Addiction 105, 817–843 (2010).
Hegdahl, H. K., Fylkesnes, K. M. & Sandøy, I. F. Sex differences in HIV prevalence persist over time: Evidence from 18 countries in Sub-Saharan Africa. PLoS ONE 11, 1–17 (2016).
Osler, M. et al. Population-wide differentials in HIV service access and outcomes in the Western Cape for men as compared to women, South Africa: 2008 to 2018: a cohort analysis. J. Int. AIDS Soc. 23, 5–14 (2020).
Nanoo, A. et al. Nationwide and regional incidence of microbiologically confirmed pulmonary tuberculosis in South Africa, 2004–12: A time series analysis. Lancet Infect. Dis. 15, 1066–1076 (2015).
Hermans, S., Boulle, A., Caldwell, J., Pienaar, D. & Wood, R. Temporal trends in TB notification rates during ART scale-up in Cape Town: An ecological analysis. J. Acquir. Immune Defic. Syndrome 1988, 1–7 (2015).
Hermans, S., Cornell, M., Middelkoop, K. & Wood, R. The differential impact of HIV and antiretroviral therapy on gender-specific tuberculosis rates. Tropical Med. Int. Health 24, 454–462 (2019).
Zawedde-Muyanja, S. et al. Anti-retroviral therapy scale-up and its impact on sex-stratified tuberculosis notification trends in Uganda. J. Int. AIDS Soc. 22, 1–9 (2019).
Horton, K. C., Sumner, T., Houben, R. M. G. J., Corbett, E. L. & White, R. G. A Bayesian approach to understanding sex differences in tuberculosis disease burden. Am. J. Epidemiol. 187, 2431–2438 (2018).
Horton, K. C., Hoey, A. L., Béraud, G., Corbett, E. L. & White, R. G. Systematic review and meta-analysis of sex differences in social contact patterns and implications for tuberculosis transmission and control. Emerg. Infect. Dis. 26, 910–919 (2020).
Dodd, P. J. et al. Age- and sex-specific social contact patterns and incidence of mycobacterium tuberculosis infection. Am. J. Epidemiol. 183, 156–166 (2016).
Shaweno, D., Horton, K. C., Hayes, R. J. & Dodd, P. J. Assortative social mixing and sex disparities in tuberculosis burden. Sci. Rep. 11, 1–10 (2021).
Department of Health. The First National TB Prevalence Survey, South Africa 2018: Short report. (2021). https://doi.org/10.1080/1560221031000112230.
Uys, P., Marais, B. J., Johnstone-Robertson, S., Hargrove, J. & Wood, R. Transmission elasticity in communities hyperendemic for tuberculosis. Clin. Infect. Dis. 52, 1399–1404 (2011).
National Tuberculosis Management Guidelines. (2008).
National Tuberculosis Management Guidelines 2014. (2014).
Osman, M. et al. Mortality during tuberculosis treatment in South Africa using an 8-year analysis of the national tuberculosis treatment register. Sci. Rep. 11, 1–10 (2021).
den Boon, S. et al. High prevalence of tuberculosis in previously treated patients, Cape Town, South Africa. Emerg. Infect. Dis. 13, 1189–1194 (2007).
Johnson, L. F. & Dorrington, R. E. Thembisa version 4.3: A model for evaluating the impact of HIV/AIDS in South Africa. (2020).
Shisana O, Labadarios D, Rehle T, Simbayi L, Zuma K, Dhansay A, Reddy P, Parker W, Hoosain E, Naidoo P, Hogoro C, Mchiza Z, Steyn NP, Dwane N, Makoae M, Maluleke T, Ramlagan S, Zungu N, Evans MG, Jacobs L, F. M. The South African National health and Nutrition Examination Survey SANHANES-1. (2013).
Kolappan, C. & Gopi, P. Tobacco smoking and pulmonary tuberculosis. Thorax 1, 964–966 (2002).
Corbett, E. L. et al. The growing burden of tuberculosis: global trends and interactions with the HIV epidemic. Arch. Intern. Med. 163, 1009–1021 (2003).
Onozaki, I. et al. National tuberculosis prevalence surveys in Asia, 1990–2012: An overview of results and lessons learned. Trop. Med. Int. Health https://doi.org/10.1111/tmi.12534 (2015).
Kubjane, M., Osman, M., Boulle, A. & Johnson, L. F. The impact of HIV and tuberculosis interventions on South African adult tuberculosis trends, 1990–2019: A mathematical modelling analysis. Int. J. Infect. Dis. https://doi.org/10.1016/j.ijid.2022.07.047 (2022).
Raftery, A. E. & Bao, L. Estimating and projecting trends in HIV/AIDS generalized epidemics using incremental mixture importance sampling. Biometrics 66, 1162–1173 (2010).
Pillay, Y. & Johnson, L. World AIDS day 2020: Reflections on global and South African progress and continuing challenges. South Afr. J. HIV Med. 22, 1–5 (2021).
Virenfeldt, J. et al. Treatment delay affects clinical severity of tuberculosis: A longitudinal cohort study. BMJ Open 4, 1–8 (2014).
Chikovore, J. et al. Missing men with tuberculosis : the need to address structural influences and implement targeted and multidimensional interventions. BMJ Glob. Health 21, 1 (2020).
Mathews, S. et al. The South African child death review pilot: A multiagency approach to strengthen healthcare and protection for children. S. Afr. Med. J. 106, 895–899 (2016).
Barboza, C. E. G., Winter, D. H., Seiscento, M., Santos, U. D. P. & Terra Filho, M. Tuberculosis and silicosis: Epidemiology, diagnosis and chemoprophylaxis. Jornal Brasileiro de Pneumologia 34, 959–966 (2008).
Telisinghe, L. et al. High tuberculosis prevalence in a South African prison: The need for routine tuberculosis screening. PLoS ONE 9, 1 (2014).
Janse van Rensburg, C. et al. Trends in smoking prevalence in South Africa for 1998 - 2014 - overcoming the challenge of multiple data sources. Tob. Induc. Dis. 16, 1 (2018).
Sahadew, N., Pillay, S. & Singaram, V. Diabetes in the Western Cape: an eight-year profile. J. Endocrinol. Metab. Diabetes South Afr 0, 1–6 (2021).
Ying Ting, W. et al. Gender disparities in latent tuberculosis infection in high-risk individuals: A cross-sectional study. PLoS ONE 9, 1 (2014).
Shirvani, T. et al. Community-based educational interventions for prevention of type II diabetes: A global systematic review and meta-analysis. Syst. Rev. 10. https://doi.org/10.1186/s13643-021-01619-3 (2021).
Acknowledgements
We thank Yogan Pillay, the South African National Department of Health and the National TB program for permitting us to use the electronic tuberculosis register data and thank Rory Dunbar for contributing to curating this data.
Funding
MK received training in research that was supported by the Fogarty International Center of the National Institutes of Health and the Eunice Kennedy Shriver National Institute of Child Health & Human Development (award number D43 TW010559), the South African Department of Science and Technology/National Research Foundation Centre of Excellence in Epidemiological Modelling and Analysis, and the International epidemiology Databases to Evaluate AIDS (National Institutes of Health, award number: UO1AI069924). LJ was supported by the Bill and Melinda Gates Foundation (award number: 019496). The content of this manuscript is solely the responsibility of the authors and does not represent the views of the funders. MC is supported by a grant from the National Institutes of Health (award number U01AI069924).
Author information
Authors and Affiliations
Contributions
M.K., L.J. and A.B. contributed to the study conceptualisation, analysis and interpretation of the results. L.J. and M.K. wrote the code for the mathematical model. M.C. contributed to the interpretation of results. M.O. curated the electronic tuberculosis register data and contributed to interpretation of results. M.K. wrote the first draft and all authors critically reviewed versions of the manuscript and agreed on the final version to be submitted for publication. All data used in this study were drawn from publicly available data sources which are described and reported in the supplementary material; all authors have access to the supplementary material.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kubjane, M., Cornell, M., Osman, M. et al. Drivers of sex differences in the South African adult tuberculosis incidence and mortality trends, 1990–2019. Sci Rep 13, 9487 (2023). https://doi.org/10.1038/s41598-023-36432-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-36432-6
- Springer Nature Limited