Abstract
This cross-sectional study aimed to investigate the hypothesis that permanent capillary damage may underlie the long-term COVID-19 sequela by quantifying the retinal vessel integrity. Participants were divided into three subgroups; Normal controls who had not been affected by COVID-19, mild COVID-19 cases who received out-patient care, and severe COVID-19 cases requiring intensive care unit (ICU) admission and respiratory support. Patients with systemic conditions that may affect the retinal vasculature before the diagnosis of COVID-19 infection were excluded. Participants underwent comprehensive ophthalmologic examination and retinal imaging obtained from Spectral-Domain Optical Coherence Tomography (SD-OCT), and vessel density using OCT Angiography. Sixty-one eyes from 31 individuals were studied. Retinal volume was significantly decreased in the outer 3 mm of the macula in the severe COVID-19 group (p = 0.02). Total retinal vessel density was significantly lower in the severe COVID-19 group compared to the normal and mild COVID-19 groups (p = 0.004 and 0.0057, respectively). The intermediate and deep capillary plexuses in the severe COVID-19 group were significantly lower compared to other groups (p < 0.05). Retinal tissue and microvascular loss may be a biomarker of COVID-19 severity. Further monitoring of the retina in COVID-19-recovered patients may help further understand the COVID-19 sequela.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by severe acute respiratory syndrome coronavirus two (SARS-CoV-2). In December 2019, an outbreak of this respiratory disease emerged in Wuhan, China which was declared a pandemic in March 2020 and has affected many lives since then1. As of October 17, 2022, the total number of confirmed cases globally per the World Health Organization (WHO) is 621,797,133, with total deaths of 6,545,5612.
The virus affects multiple organ systems aside from the respiratory system3. The term “long COVID” was introduced only a few months after the outbreak, as patients reported various symptoms that persisted or developed even after recovery from the infection4. Douaud, et al.5 investigated brain changes associated with the virus, and one of their notable findings was a greater reduction in the global brain size. A systematic review performed by Castanares-Zapatero, et al.4 found that persistent inflammatory processes result in brain microglia activation, as well as pulmonary microvascular damage that may potentially lead to pulmonary hypertension. At the vascular level, the virus promotes an inflammatory state in the vascular endothelium, causing endotheliitis, ultimately leading to a prothrombotic state in the microcirculation6. López Reboiro, et al.7 suggested that von Willebrand factor (vWF) and lupus anticoagulant (LA), in addition to other molecules, play a crucial role in thrombogenesis induced by this virus. Obtaining serum measurements of vWF and LA may predict permanent endothelial damage, leading to long COVID sequelae such as neuropathic pain or neuropsychiatric issues.
In the eye, several works of literature reported various retinal findings after infection with the novel coronavirus. There is some evidence of vascular pathology associated with COVID-19 infection. The most commonly reported ocular manifestations were retinal hemorrhages and cotton wool spots, while the most common vision-threatening manifestation was retinal vein occlusion with macular edema, making this disease vasculopathic in nature8. Several case reports have also diagnosed paracentral acute middle maculopathy, a vasculopathy associated with deep retinal microvascular circulation, after COVID-19 infection using optical coherence tomography (OCT)9,10,11,12. These are all anecdotal case reports, and many of these patients likely had comorbidities that are not described fully in the papers.
OCT Angiography (OCTA) is a non-invasive imaging technique that provides three-dimensional visualization of the retinal vasculature by moving particles, such as erythrocytes13. Although OCTA has been used in assessing retinal vasculature in patients infected with COVID-1914,15,16,17,18,19,20,21,22,23,24,25,26,27, some of these studies included patients with systemic confounders, including hypertension and diabetes mellitus, which are known to affect the retinal microvasculature.
The purpose of this study was to investigate the retinal thickness, volume, and vessel density of patients who were diagnosed and recovered from COVID-19 using Spectral Domain OCT (SD-OCT) and OCTA and to compare findings with a control group who had not been infected. We aim to understand the natural course of the ocular findings of this disease. The patients included in this study were carefully selected and had no prior systemic disease that might alter the retinal microvascular architecture.
Methods
Design
This cross-sectional, single-institution study was approved by the Institutional Review Board of the University of California San Diego in California, USA, and complied with the Health Insurance Portability and Accountability Act of 1996. All patients provided written informed consent as per institution protocol, and all the data that were collected were anonymized. Data collection and analysis were conducted according to the Principles of the Declaration of Helsinki.
Participants and patient selection
Participants in the study were subdivided into three groups: (1) Age-matched controls who never developed COVID-19; (2) Patients who received outpatient care after developing mild symptoms (fever and/or cough) and tested positive for COVID-19 by reverse transcription polymerase chain reaction (RT-PCR); (3) Patients who were seen at the University of California San Diego who were diagnosed COVID-19 positive by RT-PCR and required admission to intensive care for further management and respiratory support. Patients in subgroups 2 and 3 were diagnosed with COVID-19 between March 2020 and January 2022 and recovered from the infection, and were clinically stable upon participation in the study. Exclusion criteria were any of the following medical histories before getting infected with COVID-19: primary or secondary hypertension, diabetes mellitus type 1 or 2, hematologic disorders, any types of cancer, any cardiovascular or respiratory disease, ocular history of myopia (> 6 diopters), glaucoma, retinopathies including retinal detachment, retinal vascular disease, macular degeneration, central serous chorioretinopathy, diabetic retinopathy, recent ocular surgery within 6 months of evaluation, and media opacity (corneal, lens, or vitreous) that could affect the image quality of the scans. Participants were initially identified using structured queries of the electronic health record data warehouse (Epic SlicerDicer, Verona, WI, USA), and eligibility was confirmed with each participant via manual chart review and screening interviews regarding the aforementioned inclusion and exclusion criteria prior to study enrollment.
Examinations and procedures
Participants underwent a comprehensive ophthalmologic examination by trained retina specialists (AL, DK). This included obtaining the best-corrected visual acuity (BCVA) using the Early Treatment Diabetic Retinopathy Study (ETDRS) chart (a standard chart used for measuring visual acuity in ophthalmic research studies, even outside the context of diabetic retinopathy), intraocular pressure (VM), anterior segment examination using slit lamp biomicroscope, and dilated fundus examination using an indirect ophthalmoscope. To assess the macular thickness, volume and vasculature, SD-OCT and OCTA were performed using the Heidelberg HRA + OCT Spectralis System version 1.11.2.0 (Heidelberg Engineering, Heidelberg, Germany). OCT scan pattern were as follows: Number of B-scans = 512, Pattern Size = 3.1 × 3.1 mm/10° × 10°, Distance between B-Scans = 12 μm, ART images average = 7.
Retinal thickness and volume
Retinal thickness and volume were measured using the proprietary Heidelberg HRA + OCT Spectralis software. A thickness map of the central 3 mm of the macula with its corresponding ETDRS sectors was obtained. This map provided nine retinal thickness and volume measurements, which include: central subfield 1 mm, 1 mm inner superior/nasal/inferior/temporal, and 1 mm outer superior/nasal/inferior/temporal. The segmentation was carefully assessed by the investigators, trained retina specialists, before obtaining the numerical data. Inner retinal thickness and volume were computed from the difference of the following thickness map analyses: Inner retinal layer (ILM + ELM) − Outer nuclear layer (OPL + ELM) (Fig. 1).
SD-OCT measurement of inner retinal thickness and volume* computed from the difference between (A) (Inner retinal layer = ILM + ELM) and (B) (Outer nuclear layer = OPL + ELM). SD-OCT spectral domain-optical coherence tomography, ILM internal limiting membrane, ELM external limiting membrane, OPL outer plexiform layer. *values of thickness and volume are in μm and mm3, respectively.
Retinal vessel density
Retinal vessel density was analyzed using the AngioTool software version 0.6a (National Institutes of Health, National Cancer Institute, Bethesda, MD, USA) from the acquisition of OCTA28. The parameters used were based on a previous study by Choi et al.29: threshold parameters = 30 and 255, vessel thickness = 5, removal of small particles = 80. Vessel density was defined as the percentage of area occupied by vessels inside the explant area. Vessel density measurements of the inner retinal layer provided were as follows: Nerve fiber layer vascular plexus (NFLVP), Superficial vascular plexus (SVP), Intermediate capillary plexus (ICP), and Deep capillary plexus (DCP) (Fig. S113).
Foveal avascular zone
To determine the area, circularity, and roundness of the foveal avascular zone (FAZ), the SVP slab from the OCTA data was analyzed using the proposed method by Shiihara, et al.30 using ImageJ version 1.53 k (National Institutes of Health, Bethesda, MD, USA). The FAZ was defined as the region within the SVP slab devoid of hyperreflective signal or flow at the center of the fovea. The border of the zone was manually drawn (FK) (Fig. S2). The parameters included in the FAZ analysis were the following: Area, Perimeter, Fit ellipse, and Feret’s diameter. A circularity value of 1.0 indicates that the FAZ is a perfect circle, and as the value decreases, the less circular or, the more elongated the FAZ is31. Roundness refers to the presence or absence of surface irregularities and also refers to the inverse of aspect ratio32. Computation for the circularity and roundness was based on the ImageJ manual31.
Statistical analysis
In the current study, retinal vessel density was measured by OCTA from each layer of the inner retina (retina above the outer nuclear layer), including NFLVP, SVP, ICP, and DCP. In addition, inner retinal thickness and retinal volume were also measured from the same area in multiple segments as nine standard ETDRS sectors within the central 10 degrees of the macula. Pooling of vessel density data from NFLVP to the other three layers created a bimodal distribution; therefore, vessel density data from NFLVP was analyzed separately from the other three layers. A bimodal distribution was also present for pooled volume data; therefore, pooled data from the inner five sectors were analyzed separately from the outer four sectors. A generalized linear mixed model was fitted with pooled vessel density (SVP, ICP, and DCP) as responses and location as a random effect nested in eye, patient, and COVID-19 group. Age and sex as covariates were adjusted in the model. A similar mixed model was used to analyze thickness and volume data. All analyses were performed using SAS software 9.4 (SAS Institute, NC, USA).
Results
A total of 20 patients infected with COVID-19 participated in the study. Thirteen patients developed mild COVID-19 symptoms and received outpatient care, and seven were hospitalized in the intensive care unit, hence considered severe. A control group of 11 healthy patients without COVID-19 was used for comparison and was labeled as normal. The demographics and ocular parameters are summarized in Table 1.
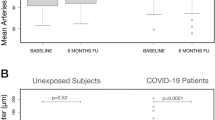
The analysis revealed that the mean vessel density of pooled data from the three inner retinal layers was significantly lower for severe COVID-19 patients (24.20, least square mean) than that of mild COVID-19 (26.18, p = 0.0057) and normal control patients (26.28, p = 0.004) (Fig. 2). Age and sex were adjusted for, but neither were significant factors. The vessel density of mild COVID-19 patients was not significantly different from that of normal participants (p = 0.87).
In this generalized linear mixed model, the least square means of the three COVID-19 levels were also compared within each retinal layer. The retinal vessel density of severe COVID-19 patients was significantly lower than that of mild COVID-19 and normal controls for ICP and DCP (p = < 0.05) (Fig. 3). Figure 4 represents an OCTA ICP and DCP scan of the normal and severe COVID-19 participants. No vessel density difference was seen among the three COVID-19 levels for SVP or NFLVP.
Representative OCTA images of the ICP (A,B) and DCP (C,D) slabs of normal participant (A,C) and severe COVID-19 participant (B,D) with their corresponding vessel densities (in percentage). OCTA optical coherence tomography angiography, ICP intermediate capillary plexus, DCP deep capillary plexus, COVID-19 coronavirus disease-19.
For inner retinal thickness data and volume data, similar analysis did not reveal significant difference between the three COVID-19 groups for the retinal thickness; however, pooled volume from the outer four standard ETDRS sectors revealed a significant lower mean volume for severe COVID-19 patients than the average volume of all patients (p = 0.02) (Fig. 5). The area of foveal avascular zone on OCTA was also analyzed, but no difference was found between the three COVID-19 groups.
In addition, our group performed a sub-analysis to compare mild versus severe COVID-19 patients while adjusting for the interval between the onset of COVID-19 symptoms and days to retinal imaging (SD-OCT and OCTA). The mean interval for mild and severe COVID-19 cases were 151 and 210, respectively. This was not significant and regression analysis revealed that the retinal vascular loss and thinning were not related to the examination interval between symptom onset of COVID-19 and imaging.
Discussion
Although the SARS-CoV-2 virus primarily affects the respiratory system, the virus has also been noted to exhibit endothelial and neurotropism and thus may infect and damage several organ systems8. COVID-19 has been associated with hypoxia and inflammation, which may lead to endothelial dysfunction and coagulation of the small and large vessels in the body33. The virus induces chronic oxidative stress in the endothelium, promoting hypercoagulability by releasing vWF. In addition, hypoxic vasoconstriction and direct cellular activation by viral transduction can lead to an increase in blood coagulation parameters34. Angiotensin-converting enzyme 2 (ACE2), a metalloproteinase, plays a key role in the SARS-CoV-2 infection as it mediates viral infection and participates in the renin–angiotensin–aldosterone system pathway and development of acute lung injury35. In relation to this, neurons and several retinal components, including retinal vascular endothelial cells, Müller cells, ganglion cells, and photoreceptor cells, contain ACE2 receptors. Therefore, retinal tissue, including vessels, may be involved in this infectious process36.
There are conflicting results regarding the retinal thickness and FAZ of patients who recovered from this virus. Some groups37,38 claimed that the central macular thickness in patients infected with COVID-19 was higher compared to normal controls, whereas other groups27,36,39 claimed that there was no difference. Our group compared the inner retinal thickness and volume of the central 3 mm of the macula and found a significant difference in the retinal volume of the outer third of the macula. This is a new finding since there were no available studies to compare retinal volume in COVID-19-recovered patients. Some groups18,20,23 also found that the FAZ is larger in patients who recovered from COVID-19 infection compared to normal controls; however, other groups14,15,21,22,24 found no difference. Our group found no significant difference between the three groups regarding the FAZ area, circularity, and roundness related to COVID-19 infection or severity.
Prior studies have used OCTA in COVID patients to determine whether retinal vessels are lost or damaged17,22. Vessel density has been related to several factors, one of which is age19, and the density of the retinal capillary vascular network decreases with older age40,41. In addition, co-morbidities such as diabetes and hypertension, which are known to be associated with severe COVID-19 infection, may also affect retinal vessels42,43. Our results showed a downward trend of vessel density as age increases, which is consistent among all groups and was corrected for in our analysis. Our results show that severe COVID patients demonstrated an 8% lower overall macular capillary vessel density compared with age-matched controls and those who developed mild COVID-19 symptoms. More particularly, an 8–11% decrease in vessel density was seen in the intermediate and deep capillary plexuses.
Several reports have shown a reduction in vessel density among patients who recovered from COVID-19. These studies noted a decrease in the superficial capillary plexus (SCP)15,16,17,18,19,21,22,23,24,26 and deep capillary plexus (DCP)16,17,21,22,23,26. Although these results are interesting, certain confounding variables were not accounted for. The severity of the disease or need for hospital admission compared to COVID-19 patients with mild disease was not carefully determined. In addition, some studies also included patients with prior systemic diseases such as hypertension and diabetes mellitus, which may affect the retinal vasculature before developing the COVID-19 infection, and hence, may skew the data. Our study involved careful enrollment of participants with no prior systemic disease (hypertension, diabetes mellitus, cancer, blood disorder), which may affect retinal vascularity and perfusion. Therefore, any effects on retinal vessel density could be more likely attributable to COVID-19 infection. Our group also carefully classified the patients into one of the two categories of recovered COVID-19 patients: those who developed mild symptoms and those who required intensive care admission and oxygen support. Our group found out that the severity of COVID-19 disease is associated with reduced retinal vessel density. Additionally, there was no statistically significant difference in the patient visit and imaging date between mild and severe COVID-19 groups.
To our knowledge, this is the first study that used the Heidelberg Spectralis OCTA to analyze vessel density in carefully characterized patients recovering from COVID-19 and controls. This device subdivides the inner retinal layer into superficial, intermediate, and deep capillary plexus, unlike other OCTA devices, where the superficial and intermediate capillary plexuses are measured as one slab called the superficial plexus. This allows for more detailed phenotypic characterization. Our group found that the intermediate and deep capillary plexuses were significantly affected in COVID-19-infected patients. This may be because the inner layers of the retina have the highest sensitivity to hypoxic stress compared to the outer layers, which are more resistant to hypoxia44.
There are several limitations to our study. This study has a relatively small sample size per sub-group since our group excluded patients with systemic co-morbidities like hypertension and diabetes mellitus, which impacted our search for more available participants. This may limit the power to detect small differences between the categories and variables. Compared to retinal thickness and volume measurements, the overall vessel density in the central 3 mm of the macula was analyzed since calculation per ETDRS sector is unavailable. This may dilute regional changes in the macula. In future studies, it would be interesting to analyze OCTA using an ETDRS sector to understand if regional retinal structure correlates with changes in vascularity. Lastly, this is a cross-sectional study and retinal imaging and evaluation were done only once. A longitudinal evaluation of the parameters may be worth exploring in future studies, particularly given recent evidence that COVID-19 can have long-term effects throughout the body.
In conclusion, patients who recovered from COVID-19 after hospitalization showed a significant decrease in retinal tissue, including inner retinal volume and vessel density. Retinal volume and vessel density loss of this magnitude may not cause significant visual symptoms. However, this may be a biomarker for severe COVID or long COVID or COVID damage to the brain and other organs. OCT angiography is a non-invasive technique and can be performed on an undilated pupil. A high-quality exam by a trained operator is estimated to take around five to ten minutes per patient, hence the procedure is undemanding. Close monitoring and surveillance of the patients who recovered from COVID-19 should be considered to assess for long-term sequela of COVID-19 affecting the retina using this non-invasive imaging modality.
Data availability
All data in the current study are available from the corresponding author (WRF) upon reasonable request.
References
Patel, N. S. et al. Retrospective analysis of retinal imaging in COVID-19 positive patients at a tertiary eye care center. OPTH 15, 3727–3731 (2021).
World Health Organization, 2022. https://covid19.who.int/. Accessed 17 October 2022.
Pereira, L. A. et al. Retinal findings in hospitalised patients with severe COVID-19. Br. J. Ophthalmol. 106, 102–105 (2022).
Castanares-Zapatero, D. et al. Pathophysiology and mechanism of long COVID: A comprehensive review. Ann. Med. 54, 1473–1487 (2022).
Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604, 697–707 (2022).
López Castro, J. Post-COVID-19 Syndrome (PC19S): Chronic reactive endotheliitis and disseminated vascular disease. Acta Med. Port. 33, 859–859 (2020).
López Reboiro, M. L. et al. Role of lupus anticoagulant and von Willebrand factor in chronic reactive endotheliitis in COVID-19. J. Infect. 82, e27–e28 (2021).
Sen, S. et al. Retinal manifestations in patients with SARS-CoV-2 infection and pathogenetic implications: A systematic review. Int. Ophthalmol. 42, 323–336 (2022).
Padhy, S. K., Dcruz, R. P. & Kelgaonkar, A. Paracentral acute middle maculopathy following SARS-CoV-2 infection: The D-dimer hypothesis. BMJ Case Rep. 14, e242043 (2021).
Virgo, J. & Mohamed, M. Paracentral acute middle maculopathy and acute macular neuroretinopathy following SARS-CoV-2 infection. Eye 34, 2352–2353 (2020).
Naughton, A., Ong, A. Y., Gkika, T. & Downes, S. Bilateral paracentral acute middle maculopathy in a SARS-CoV-2-positive patient. Postgrad. Med. J. 98, e105–e106 (2022).
Ozsaygılı, C., Bayram, N. & Ozdemir, H. Cilioretinal artery occlusion with paracentral acute middle maculopathy associated with COVID-19. Indian J. Ophthalmol. 69, 1956 (2021).
Rocholz, R. et al. SPECTRALIS Optical Coherence Tomography Angiography (OCTA): Principles and Clinical Applications.
Savastano, M. C. et al. Retinal capillary involvement in early post-COVID-19 patients: A healthy controlled study. Graefes Arch. Clin. Exp. Ophthalmol. 259, 2157–2165 (2021).
Guemes-Villahoz, N. et al. Reduced macular vessel density in COVID-19 patients with and without associated thrombotic events using optical coherence tomography angiography. Graefes Arch. Clin. Exp. Ophthalmol. 259, 2243–2249 (2021).
Cetinkaya, T., Kurt, M. M., Cetinkaya, H. & Akpolat, C. Analysis of microvasculature in children recovered from COVID-19 using swept-source OCT/OCTA technology. Ocul. Immunol. Inflamm. https://doi.org/10.1080/09273948.2022.2054431 (2022).
Cetinkaya, T., Kurt, M. M. & Akpolat, C. Analysis of swept-source optical coherence tomography angiography measurement alterations in adult patients recovered from COVID-19. Clin. Exp. Optom. 105, 848–852 (2022).
Bilbao-Malavé, V. et al. Persistent retinal microvascular impairment in COVID-19 bilateral pneumonia at 6-months follow-up assessed by optical coherence tomography angiography. Biomedicines 9, 502 (2021).
Zapata, M. Á. et al. Retinal microvascular abnormalities in patients after COVID-19 depending on disease severity. Br. J. Ophthalmol. 106, 559–563 (2022).
Kal, M. et al. Retinal microvascular changes in COVID-19 bilateral pneumonia based on optical coherence tomography angiography. J. Clin. Med. 11, 3621 (2022).
Hazar, L. et al. Macular vessel density in patients recovered from COVID 19. Photodiagn. Photodyn. Ther. 34, 102267 (2021).
Cennamo, G. et al. Optical coherence tomography angiography features in post-COVID-19 pneumonia patients: A pilot study. Am. J. Ophthalmol. 227, 182–190 (2021).
Erogul, O. et al. Retinal microvascular morphology versus COVID-19: What to anticipate?. Photodiagn. Photodyn. Ther. 39, 102920 (2022).
Turker, I. C., Dogan, C. U., Dirim, A. B., Guven, D. & Kutucu, O. K. Evaluation of early and late COVID-19-induced vascular changes with OCTA. Can. J. Ophthalmol. 57, 236–241 (2022).
Naderi Beni, A. et al. Retinal findings of COVID-19 patients using ocular coherence tomography angiography two to three months after infection. Photodiagn. Photodyn. Ther. 38, 102726 (2022).
Abrishami, M. et al. Optical coherence tomography angiography analysis of the retina in patients recovered from COVID-19: A case-control study. Can. J. Ophthalmol. 56, 24–30 (2021).
Szkodny, D. et al. Retinal OCT findings in patients after COVID infection. JCM 10, 3233 (2021).
Zudaire, E., Gambardella, L., Kurcz, C. & Vermeren, S. A computational tool for quantitative analysis of vascular networks. PLoS ONE 6, e27385 (2011).
Choi, M., Kim, S.-W., Yun, C., Oh, J.-H. & Oh, J. Predictive role of optical coherence tomography angiography for exudation recurrence in patients with type 1 neovascular age-related macular degeneration treated with pro-re-nata protocol. Eye 37, 34–41 (2023).
Shiihara, H. et al. Objective evaluation of size and shape of superficial foveal avascular zone in normal subjects by optical coherence tomography angiography. Sci. Rep. 8, 10143 (2018).
Ferreira, T. & Rasband, W. ImageJ User Guide.
Takashimizu, Y. & Iiyoshi, M. New parameter of roundness R: Circularity corrected by aspect ratio. Prog. Earth Planet. Sci. 3, 2 (2016).
Marchetti, M. COVID-19-driven endothelial damage: Complement, HIF-1, and ABL2 are potential pathways of damage and targets for cure. Ann. Hematol. 99, 1701–1707 (2020).
Sieiro-Santos, C. & López-Castro, J. Post-coronavirus disease syndrome and disseminated microthrombosis: The role of the von Willebrand factor and antiphospholipid antibodies. Clinics 76, e2784 (2021).
Liu, M., Zheng, B., Zhang, Y. & Li, J. Role and mechanism of angiotensin-converting enzyme 2 in acute lung injury in coronavirus disease 2019. Chronic Dis. Transl. Med. 6, 98–105 (2020).
Abrishami, M. et al. Spectral-domain optical coherence tomography assessment of retinal and choroidal changes in patients with coronavirus disease 2019: A case-control study. J. Ophthal. Inflamm. Infect. 12, 18 (2022).
Oren, B. et al. Quantitative assessment of retinal changes in COVID-19 patients. Clin. Exp. Optom. 104, 717–722 (2021).
Mavi Yildiz, A. et al. SD-OCT assessment of macular and optic nerve alterations in patients recovered from COVID-19. Can. J. Ophthalmol. 57, 75–81 (2022).
Fırat, M. & Kobat, S. How are central foveal and choroidal thickness affected in patients with mild COVID-19 infection?: Foveal and choroidal thicknesses with COVID-19. Bosn. J. Basic Med. Sci. https://doi.org/10.17305/bjbms.2021.5840 (2021).
Wang, Q. et al. Vascular density in retina and choriocapillaris as measured by optical coherence tomography angiography. Am. J. Ophthalmol. 168, 95–109 (2016).
Park, S. H. et al. Changes in the retinal microvasculature measured using optical coherence tomography angiography according to age. J. Clin. Med. 9, 883 (2020).
Lee, W. H. et al. Retinal microvascular change in hypertension as measured by optical coherence tomography angiography. Sci. Rep. 9, 156 (2019).
Di, G. et al. A morphological study of the foveal avascular zone in patients with diabetes mellitus using optical coherence tomography angiography. Graefes Arch. Clin. Exp. Ophthalmol. 254, 873–879 (2016).
Kaur, C. Hypoxia-ischemia and retinal ganglion cell damage. Clin. Ophthalmol. https://doi.org/10.2147/OPTH.S3361 (2008).
Acknowledgements
The authors would like to acknowledge the following: Multimodal Retina Image Alignment and Applications R01EY033847 (Freeman), UCSD Vision Research Center Core grant from the NEI P30EY022589, NIH grant R01EY016323 (Bartsch), NIH grant DP5OD29610 (Baxter), Foundation Fighting Blindness grant CD-GT-0918-0746-SE (Borooah), Nixon vision Foundation grant (Borooah), an unrestricted grant from Research to Prevent Blindness, NY (Freeman), and unrestricted funds from UCSD Jacobs Retina Center.
Author information
Authors and Affiliations
Contributions
F.G.P.K.—designed the study, acquired and analyzed the data, interpreted the data, drafted and revised the manuscript; A.W.—conceptualized and designed the study, acquired the data; M.C.—acquired the data; D.K.—acquired the data; A.L.—acquired the data; D.D.—acquired the data, revised the manuscript; C.G.—acquired the data; A.H.—acquired the data, revised the manuscript; V.M.—acquired the data; S.L.B.—analyzed the data, revised the manuscript; S.B.—analyzed the data, revised the manuscript; D.U.B.—acquired and analyzed the data; L.C.—analyzed the data and revised the manuscript; W.R.F.—conceptualized and designed the study, analyzed the data, revised the manuscript. All authors listed have contributed to the work and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kalaw, F.G.P., Warter, A., Cavichini, M. et al. Retinal tissue and microvasculature loss in COVID-19 infection. Sci Rep 13, 5100 (2023). https://doi.org/10.1038/s41598-023-31835-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-31835-x
- Springer Nature Limited