Abstract
Desflurane is known to have a larger vasodilatory effect than that of sevoflurane. However, its generalizability and effect size in actual clinical practice are yet to be proven. Patients aged ≥ 18 years who underwent noncardiac surgery under general anesthesia using inhalation anesthetics (desflurane or sevoflurane) were matched 1:1 by propensity score. The mean intraoperative perfusion index (PI) of each patient were compared between the two groups. Propensity score matching of 1680 patients in the study cohort identified 230 pairs of patients. PI was significantly higher in the desflurane group (median of paired difference, 0.45; 95% CI 0.16 to 0.74, p = 0.002). PI durations below 1.0 and 1.5 were significantly longer in the sevoflurane group. Mean arterial pressure (MAP) and durations of low MAP did not differ significantly between the two groups. Generalized linear mixed models revealed that the use of sevoflurane, mean MAP, mean heart rate, age, and duration of anesthesia had significant negative effects (lower PI), whereas mean age-adjusted minimum alveolar concentration of inhalation agent had a positive effect on PI (higher value). Intraoperative PI was significantly higher in patients administered desflurane than sevoflurane. However, the impact of the choice between desflurane and sevoflurane on intraoperative PI in this clinical setting was minimal.
Similar content being viewed by others
Introduction
Vascular tone is an essential factor for understanding organ perfusion1 and hemodynamic assessments2,3. Because organ perfusion does not depend solely on blood pressure, it is crucial to consider other parameters, such as vascular tone and regional perfusion4. Peripheral vascular tone and perfusion may be assessed by measuring the peripheral perfusion index (PI; or as PPI in some literature), a parameter derived from the pulse oximetry signal4,5,6. It represents the ratio of pulsatile to non-pulsatile components of the signal.
Inhalation anesthetics have vasodilatory effects7,8 and can improve microcirculation9. A recent randomized trial6 found that desflurane exerts a more potent vasodilatory effect than sevoflurane, as shown by higher PI and lower blood pressure. Although these findings were supported by the careful control of many possible confounders, such as comorbidities and stimulation intensity, the findings of that study may have limited generalizability to real-world clinical practice, in which such confounders cannot be controlled. Therefore, the present study retrospectively compared intraoperative PI in patients administered desflurane and sevoflurane as inhalation anesthetics.
Materials and methods
The study was conducted in accordance with the principles of the Declaration of Helsinki and the study protocol was approved by the Institutional Review Board of Chungnam National University Hospital (CNUH 2021-11-008) on 12 November 2021 with waiver for informed consent and registered at the Clinical Research Information Service, a clinical trial registry in South Korea (KCT0006766).
Study design
This retrospective cohort study included patients aged ≥ 18 years who underwent noncardiac surgery, including general, gynecological, otolaryngological, plastic, and urological surgery, under general anesthesia using inhalation anesthetics (desflurane or sevoflurane) and PI monitoring from February to August 2021 in a university hospital. Patients were excluded if clinical or vital data were missing, their vital records had interruptions, or if information was lacking regarding the inhalation agent, PI, or blood pressure (noninvasive or invasive arterial pressure). To account for the differences in their clinical characteristics, patients administered desflurane and sevoflurane were matched 1:1 by propensity score. This manuscript adheres to the applicable STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines10.
Data acquisition
All vital data were obtained from the prospective registry of the vital signs for surgical patients at Chungnam National University Hospital (CNUH IRB 2019-08-039), which uses a free data collection program (Vital recorder11 version 1.8, accessed at https://vitaldb.net, Seoul, Republic of Korea).
Other data collected from patient medical records included age, sex, body mass index (BMI), comorbidities (hypertension, diabetes, coronary artery disease, liver cirrhosis, chronic obstructive pulmonary disease, chronic renal impairment), Charlson comorbidity index, American Society of Anesthesiologists (ASA) physical status, type of surgery (general, gynecological, otolaryngological, plastic, or urological), emergency surgery, duration of anesthesia, intraoperative infusion of vasopressor (norepinephrine), intraoperative transfusion (red blood cells or fresh frozen plasma), intraoperative fluid input, and intraoperative opioid dose (remifentanil, μg kg–1 min–1).
Intraoperative PI and heart rate (HR) were monitored continuously using a disposable oximeter sensor (Nellcor™ Neonatal-Adult SpO2 sensor, Covidien, Mansfield, MA, USA) and a patient monitor (Intellivue MX700 or MX800 [Philips, Boeblingen, Germany]) and recorded at a frequency of 1 Hz. Oximeter sensor was routinely attached to the index or third finger of the patient unless contraindicated or inaccessible. Blood pressure was measured continuously with an arterial catheter or intermittently at 5-min intervals using a noninvasive blood pressure cuff and recorded at a frequency of 1 Hz. Intra-arterial pressure was primarily used for analysis, if available. Data regarding inhalation anesthetics (agent type, end-tidal concentration [%]) were obtained from the anesthesia machines and recorded at a frequency of 0.2–0.25 Hz. All vital signs and records of inhalation agents were extracted as 10 s interval mean values. These data were filtered for errors in blood pressure, so that the mean arterial pressure (MAP) was > 20 mmHg and < 150 mmHg. To include periods only with proper administration of inhalation anesthetics in the analysis, a cut-off value of end-tidal concentration (the 25th percentile of the intraoperative end-tidal concentration) of the inhalation agent was determined for the vital records of each individual and filtered accordingly. For example, if the median intraoperative end-tidal concentration of sevoflurane was 1.3 volume % (25th to 75th percentile, 1.2% to 1.4%), then the cut-off was set at 1.2 volume % and only periods with end-tidal sevoflurane concentrations above this value were included in the analysis. Mean of PI values acquired for three minutes immediately before the initiation of the administration of inhalation anesthetics was considered baseline.
Outcome measures
The primary outcome was the mean intraoperative PI of each patient administered each inhalation agent. Other outcomes included the intraoperative durations at which the PI was below the thresholds of 0.5, 1, 1.5, and 2, mean HR, mean MAP, and the intraoperative durations at which MAP was below the thresholds of 50, 55, 60, 65, and 70 mmHg.
Statistics
The sample size was based on data available during the study period. All statistical analyses were performed using R software version 4.0.3 (R Project for Statistical Computing, Vienna, Austria). Propensity scores were calculated using a logistic regression model, in which the type of inhalation agent was considered a dependent variable and the clinical characteristics of patients, including age, sex, BMI, Charlson comorbidity index, ASA physical status (1–2 or > 2), comorbidities, type of surgery, and intraoperative variables (duration of anesthesia, vasopressor infusion, transfusion, intravenous fluid intake, opioid, mean age-adjusted minimum alveolar concentration [MAC] of the inhalation agent12, and the administered dose of opioid), were considered explanatory variables. Patients were matched by 1:1 nearest neighbor matching using a caliper width of 0.09 (0.25 \(\times\) the standard deviation [SD] of the propensity score) using the ‘MatchIt’ package13 in R software. The matching process included only those patients for whom we had complete records. The standardized mean difference was calculated to assess the balance between groups after matching, with a difference of < 0.1, indicating that the two groups were sufficiently balanced.
Continuous variables were reported as the mean ± SD or median (interquartile range [IQR]), depending on the results of the Shapiro–Wilk test. After the matching process, continuous variables were compared using paired Wilcoxon signed-rank tests14. Categorical variables were reported as numbers (%) and compared using chi-squared or Fisher’s exact tests. Statistical significance was set at a two-tailed p-value of < 0.05.
To identify factors affecting mean PI other than the inhalation agent, especially mean MAP and HR, a negative-binomial generalized linear mixed model was fitted. In that model, mean PI was considered a dependent variable; mean MAP, mean HR, inhalation agent, and the variables involved in the matching process were considered independent variables, and the matching identifier was considered a random effect. Because the dependent variable in the model could be reported only as a non-negative integer, the mean PIs were transformed as rounded values, expressed as 100 \(\times\) mean PI. The proper fitting of the model was assessed using the ‘Diagnostics for HierArchical Regression Models (DHARMa)’ package15.
Sensitivity analysis
Because the results can be influenced by the selection of specific matched data sets, the primary outcomes were analyzed and model fitting was performed using two additional matched datasets.
Results
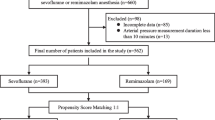
A total of 4210 patients underwent noncardiac surgery under general anesthesia, including inhalation of desflurane or sevoflurane and PI monitoring from February to August 2021. Of these patients, 2530 were excluded due to insufficient data. The remaining 1680 patients were subjected to 1:1 propensity score matching, yielding a total of 230 pairs (Fig. 1). Clinical characteristics before and after matching are summarized in Table 1, with all clinical characteristics after matching adequately balanced.
The outcomes according to the administered inhalation agents are summarized in Table 2 and Fig. 2. There was no significant difference in the baseline PI. The mean PI values were significantly higher in the desflurane (median 3.1 [IQR 2.0, 4.2]) than in the sevoflurane (median 2.6 [IQR 1.8, 3.8]) group after matching (median paired difference, 0.45; 95% CI 0.16 to 0.74, p = 0.002). PI durations below 1.0 and 1.5 were significantly longer in the sevoflurane group than in the desflurane group. MAP and all defined durations of low MAP did not differ significantly between the two groups after matching.
Box-and-whisker plot of mean perfusion index (PI) and kernel density plots of the duration of PIs below threshold stratified by the type of inhalation agent before (upper) and after (lower) the propensity score matching. Kernel density estimation is a non-parametric method of estimating the probability density function of a continuous random variable. The probability density function is used to specify the probability of the random variable falling within a particular range of the variable and the area under the entire curve is equal to one. Based on the presented kernel density plots, shorter durations of low PI values in patients administered desflurane than sevoflurane can be inferred.
The regression model showed that administration of sevoflurane, higher mean MAP, higher mean HR, older age, ASA > 2, longer duration of anesthesia, and certain type of surgery (general, gynecologic, and urologic surgery) had significant negative effects on mean PI (lower value), whereas chronic obstructive pulmonary disease and higher mean age-adjusted MAC of inhalation agent had significant positive effects on mean PI (higher value; Table 3). Specifically, the use of sevoflurane lowered the mean PI by 12.3%. In addition, a 10 mmHg increase in mean MAP and mean HR lowered mean PI by 5.3% and 6.1%, respectively. The relationship between mean MAP, mean heart rate, and mean PI stratified by the type of inhalation agent is shown in Fig. 3.
Effect of mean arterial pressure (MAP) and heart rate (HR) on perfusion index (PI) stratified by the type of inhalation agent. The plot presents the estimated marginal mean PI derived from the mixed-effects model. The shaded areas represent 95% confidence intervals of the estimated means. Note that the PI on the y-axis is multiplied by 100. BPM beat per minute.
The results of the sensitivity analysis are shown in Supplementary Materials 1 and 2. The result of the primary outcome was consistent in the additional datasets. Administration of sevoflurane, mean MAP, mean HR, age, and duration of anesthesia had significant negative effects on mean PI, whereas mean age-adjusted MAC of inhalation agent had significant positive effect on mean PI regardless of the dataset used.
Discussion
The present study was performed to assess generalizability of the findings from a previous clinical trial in a real-world data with propensity score matching. In line with the previous trial, the current study showed that PI was higher in patients receiving desflurane than in those receiving sevoflurane. In addition, the duration of low PI was longer in the sevoflurane group. However, the impact of the choice between desflurane and sevoflurane on intraoperative PI was minimal, median 0.45 and about 12% in the multivariable model, which has questionable clinical significance.
The previous experimental study revealed that the use of desflurane result in mean 3.3 difference of PI compared with the use of sevoflurane and significant difference in blood pressure. However, the amount of PI difference was much lesser and no significant difference in blood pressure were noted depending on the inhalation agent in the current study. During dynamic intraoperative period, many factors such as various surgical stimulation, opioid use, and fluid and/or vasopressor administrations coexist and can interfere with the impact of inhalation agent on PI. Moreover, mixed population with various comorbidities and surgical procedure can surely be important confounding factors. As aforementioned factors cannot be completely controlled in a real-world setting, the findings in the current study would be more pragmatic than the previous one16,17. In other words, choice or switching between the two inhalation agents for the purpose of manipulating intraoperative PI seems impractical.
This study has several strengths. First, we used real-world data consisting of high-resolution vital records. The second strength was the use of a propensity score matching process, which resulted in a proper balance between the two groups. This process involves the consideration of various confounders, not only baseline characteristics but also intraoperative variables, including the mean MAC of the inhalation agent, opioid dose, and fluid intake. Third, the regression analysis after matching provides “double robustness”, complementing the findings of propensity score matching18. Fourth, further robustness was provided by sensitivity analysis using different sets of propensity score-matched patients. Fifth, a retrospective design using a dataset from a different institution may alleviate performance bias and generalizability could have been assessed.
The present study assumed PI is an indicator of vasodilation. Although this assumption is supported by several previous studies6,19,20,21,22, other studies suggest that PI also depends on cardiac output or stroke volume23,24,25. Considering relevant evidences altogether, it is more reasonable to consider PI as a combinational parameter dependent on various local and systemic factors26. Following this logic, the impact of inhalation agent on PI is more likely to be complex rather than simply reflecting vasodilation.
Other factors found to be consistently associated with mean PI in this study included mean MAP, mean HR, age, duration of anesthesia, and age-adjusted MAC. According to a recent review article26, PI is mainly determined by stroke volume and vascular tone. Increase of vascular tone and decrease of stroke volume can lead to reduced PI, and vice versa. In this context, the negative coefficient of mean MAP in the models indicate high vascular tone manifested as low PI with a given stroke volume. The negative coefficients of mean HR in the models may reflect decreased stroke volume and/or increased vascular tone, which is commonly accompanied by volume deficit and resultant increase of HR. In addition, the coefficient of mean age-adjusted MAC reflects positive dose–response relationship between inhalation agent and PI. However, these inferences should be considered hypothesis generating and needs further studies. Especially, caution is needed as those relationships between MAP, HR, and PI were not evaluated on an individual patient level with serial measurements.
Recent evidence has suggested that clinicians should pay attention not only to blood pressure but also to perfusion during surgery1,4,5,27. Because organ perfusion is not solely dependent on blood pressure, but is also affected by regional vascular tone, the suggestion that greater vasodilation and lower blood pressure arising from the use of desflurane may result in potential clinical harm requires careful reconsideration6. Because vasodilation and low blood pressure may exert opposite effects on organ perfusion, the net effect cannot be estimated simply. For example, the negative effect of desflurane-induced low blood pressure on organ perfusion may be counteracted by desflurane-induced vasodilation. Future studies should analyze these complicated net effects.
This study had several limitations. First, despite the availability of high-resolution vital records, only descriptive statistics (i.e. mean PI and MAP), rather than the original values, were included in the final analysis, except for the durations of low PI and MAP. Second, a large number of patients could not be included in the analysis because of the lack of vital recordings or detailed clinical information (mostly intraoperative remifentanil doses which were manually recorded). Although selection bias due to this issue cannot be excluded, these omissions were more likely to be random (missing at random) rather than systematic. Third, more detailed information, such as bolus use of a vasopressor (e.g. phenylephrine) and the total dose of infused norepinephrine, was not included in the analysis due to unreliable quality. Instead, the use of norepinephrine infusion was included in the analysis as a surrogate marker of considerable requirement of vasopressor because it is commonly adopted after repeated doses of phenylephrine. Fifth, subtle discrepancies in intraoperative management may exist among clinicians, some of whom may prefer either of the inhalation agents. This might have affected the results of the current study.
In conclusion, despite the lack of different effect of inhalation agents on MAP, the mean PI was significantly higher in patients administered desflurane than sevoflurane. However, the impact of the choice between desflurane and sevoflurane on intraoperative PI in this clinical setting was minimal which has questionable clinical significance.
Data availability
The data of the current study are available from the corresponding author on reasonable request.
References
Meng, L. Heterogeneous impact of hypotension on organ perfusion and outcomes: A narrative review. Br. J. Anaesth. https://doi.org/10.1016/j.bja.2021.06.048 (2021).
Slagt, C. et al. Cardiac output measured by uncalibrated arterial pressure waveform analysis by recently released software version 3.02 versus thermodilution in septic shock. J. Clin. Monit. Comput. 27, 171–177. https://doi.org/10.1007/s10877-012-9410-9 (2013).
Chin, J. H. et al. Unreliable tracking ability of the third-generation FloTrac/Vigileo™ system for changes in stroke volume after fluid administration in patients with high systemic vascular resistance during laparoscopic surgery. PLoS ONE 10, e0142125. https://doi.org/10.1371/journal.pone.0142125 (2015).
Foss, N. B. & Kehlet, H. Perioperative haemodynamics and vasoconstriction: Time for reconsideration?. Br. J. Anaesth. 123, 100–103. https://doi.org/10.1016/j.bja.2019.04.052 (2019).
Agerskov, M. et al. Association of the intraoperative peripheral perfusion index with postoperative morbidity and mortality in acute surgical patients: A retrospective observational multicentre cohort study. Br. J. Anaesth. 127, 396–404. https://doi.org/10.1016/j.bja.2021.06.004 (2021).
Ryu, K. H. et al. Comparison of vasodilatory properties between desflurane and sevoflurane using perfusion index: A randomised controlled trial. Br. J. Anaesth. 125, 935–942. https://doi.org/10.1016/j.bja.2020.07.050 (2020).
Iida, H., Ohata, H., Iida, M., Watanabe, Y. & Dohi, S. Isoflurane and sevoflurane induce vasodilation of cerebral vessels via ATP-sensitive K+channel activation. Anesthesiology 89, 954–960. https://doi.org/10.1097/00000542-199810000-00020 (1998).
Larach, D. R. & Schuler, H. G. Direct vasodilation by sevoflurane, isoflurane, and halothane alters coronary flow reserve in the isolated rat heart. Anesthesiology 75, 268–278. https://doi.org/10.1097/00000542-199108000-00015 (1991).
Cho, Y. J. et al. Microcirculation measured by vascular occlusion test during desflurane-remifentanil anesthesia is superior to that in propofol-remifentanil anesthesia in patients undergoing thoracic surgery: Subgroup analysis of a prospective randomized study. J. Clin. Monit. Comput. 31, 989–997. https://doi.org/10.1007/s10877-016-9937-2 (2017).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 147, 573–577. https://doi.org/10.7326/0003-4819-147-8-200710160-00010 (2007).
Lee, H.-C. & Jung, C.-W. Vital recorder—A free research tool for automatic recording of high-resolution time-synchronised physiological data from multiple anaesthesia devices. Sci. Rep. 8, 1527. https://doi.org/10.1038/s41598-018-20062-4 (2018).
Lerou, J. G. C. Nomogram to estimate age-related MAC. Br. J. Anaesth. 93, 288–291. https://doi.org/10.1093/bja/aeh186 (2004).
Ho, D., Imai, K., King, G. & Stuart, E. A. MatchIt: Nonparametric preprocessing for parametric causal inference. J. Stat. Softw. 42, 28. https://doi.org/10.18637/jss.v042.i08 (2011).
Austin, P. C. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat. Med. 27, 2037–2049. https://doi.org/10.1002/sim.3150 (2008).
Hartig, F. DHARMa: Residual diagnostics for hierarchical (multi-level/mixed) regression models. http://florianhartig.github.io/DHARMa/ (2021).
de Lusignan, S., Crawford, L. & Munro, N. Creating and using real-world evidence to answer questions about clinical effectiveness. J. Innov. Health Inform. 22, 368–373. https://doi.org/10.14236/jhi.v22i3.177 (2015).
Sherman, R. E. et al. Real-world evidence—What is it and what can it tell us?. N. Engl. J. Med. 375, 2293–2297. https://doi.org/10.1056/NEJMsb1609216 (2016).
Stuart, E. A. Matching methods for causal inference: A review and a look forward. Stat. Sci. 25, 1–21. https://doi.org/10.1214/09-sts313 (2010).
Lima, A. P., Beelen, P. & Bakker, J. Use of a peripheral perfusion index derived from the pulse oximetry signal as a noninvasive indicator of perfusion. Crit. Care Med. 30, 1210–1213. https://doi.org/10.1097/00003246-200206000-00006 (2002).
Ginosar, Y. et al. Pulse oximeter perfusion index as an early indicator of sympathectomy after epidural anesthesia. Acta Anaesthesiol. Scand. 53, 1018–1026. https://doi.org/10.1111/j.1399-6576.2009.01968.x (2009).
Kus, A., Gurkan, Y., Gormus, S. K., Solak, M. & Toker, K. Usefulness of perfusion index to detect the effect of brachial plexus block. J. Clin. Monit. Comput. 27, 325–328. https://doi.org/10.1007/s10877-013-9439-4 (2013).
Sebastiani, A. et al. Perfusion index and plethysmographic variability index in patients with interscalene nerve catheters. Can. J. Anaesth. 59, 1095–1101. https://doi.org/10.1007/s12630-012-9796-3 (2012).
Corsini, I., Cecchi, A., Coviello, C. & Dani, C. Perfusion index and left ventricular output correlation in healthy term infants. Eur. J. Pediatr. 176, 1013–1018. https://doi.org/10.1007/s00431-017-2920-1 (2017).
Janaillac, M. et al. Correlations between near-infrared spectroscopy, perfusion index, and cardiac outputs in extremely preterm infants in the first 72 h of life. Eur. J. Pediatr. 177, 541–550. https://doi.org/10.1007/s00431-018-3096-z (2018).
Lian, H., Wang, X., Zhang, Q., Zhang, H. & Liu, D. Changes in perfusion can detect changes in the cardiac index in patients with septic shock. J. Int. Med. Res. 48, 300060520931675. https://doi.org/10.1177/0300060520931675 (2020).
Coutrot, M. et al. Perfusion index: Physical principles, physiological meanings and clinical implications in anaesthesia and critical care. Anaesth. Crit. Care Pain Med. 40, 100964. https://doi.org/10.1016/j.accpm.2021.100964 (2021).
Bakker, J. Clinical use of peripheral perfusion parameters in septic shock. Curr. Opin. Crit. Care 27, 269–273. https://doi.org/10.1097/mcc.0000000000000826 (2021).
Funding
This work was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI20C2088) and the research fund of Chungnam National University Hospital (2021-CF-022).
Author information
Authors and Affiliations
Contributions
Study concept and design: C.O., S.L., B.H.; Data analysis: C.O., B.S.; Statistical supervision: B.S.; Data collection: S.K., C.L.; Study supervision: Y.S.S., Y.K., Y.H.K.; Draft of the manuscript: C.O., S.L.; Revising the manuscript: S.H.Y., C.L., B.H.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oh, C., Lee, S., Song, BS. et al. Comparative effects of desflurane and sevoflurane on intraoperative peripheral perfusion index: a retrospective, propensity score matched, cohort study. Sci Rep 13, 2991 (2023). https://doi.org/10.1038/s41598-022-27253-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-27253-0
- Springer Nature Limited