Abstract
To determine whether there is a link between serum albumin and mortality among participants in the elderly in Japan. This is a single-center,retrospective cohort study analysis of 253 old patients with dysphagia from Japan, conducted from January 2014 to January 2017. The primary outcome was mortality. We performed Cox regression analysis to compare the mortality between the two groups (divided by serum albumin = 3 g/dl). 253 patients were included in the analysis, of whom the number of serum albumin under 3 g/dl was 93. The log-rank test showed a significant longer mortality in the high group (serum albumin > = 3 g/dl) compared with the low group (median, 382 vs. 176 days, P < 0.0001). Cox regression analysis showed that unadjusted HR for the high group relative to the low group was 0.40 (95% CI: 0.29–0.57; P < 0.001). After adjusting 3 models in multivariable analysis, serum albumin was significantly associated with mortality. The adjusted HRs (95% CI) for total mortality rates were 0.46 (0.33–0.65), 0.66 (0.44–0.99) and 0.64 (0.42–0.97), from model 2 to model 4. There is negative association between serum albumin and mortality in Japanese old people with dysphagia.
Similar content being viewed by others
Introduction
Dysphagia, or disordered oropharyngeal swallowing, is a common finding in elderly persons1 whether are institutionalized or living in the community2,3, which is caused by age-related physiological changes in swallowing, including a decline of swallowing function and decreased digestive tract motility due to decreases in muscle mass and connective tissue elasticity4,5. Cicheroet6 reported a 25–30% prevalence among acute inpatients who underwent clinical screening for dysphagia. Dysphagia may lead to malnutrition and dehydration 5. It is a risky factor for pneumonia7 and stroke 8.
Serum albumin is a widely used routine clinical test and serves as a biomarker of inflammatory and nutritional status9,10,11, which is a reliable index of malnutrition. The effect of inflammation on albumin levels is responsible for much of the morbidity and mortality associated with hypoalbuminemia9. Some of the prior studies reported serum albumin was associated with chronic kidney disease and cardiovascular12,13,14, which is also a risky factor for dysphagia in elderly hip fracture surgery patients15. Hypoalbuminemia is strongly associated with mortality11, and is an independent determinant of poor outcome following acute ischemic stroke16.
Although some studies have shown that serum albumin is associated with many diseases, but few studies have revealed the association between serum albumin and mortality in elderly swallowing patients. A previous propensity-matched cohort study shows PEG (percutaneous endoscopic gastrostomy) is associated with a significantly longer survival time in older persons with dysphagia17. We perform a secondary analysis of the cohort study data to evaluate whether there is a link between serum albumin and mortality among participants in Japan.
Patients and methods
Study population and design
This study was a single-center, retrospective cohort study. Consecutive older patients with dysphagia who received PEG or TPN (total parenteral nutrition)18 between January 2014 and January 2017 in Japan. People who had advanced cancer or required a PEG for gastric decompression were excluded. Patients who had a PEG inserted before January 2014 were also excluded.
Because of the anonymous nature of the data, the requirement for informed consent was waived. All methods were performed in accordance with the relevant guidelines and regulations. The present study was approved by the Ethical Review Board of Miyanomori Memorial Hospital and was exempted from informed consent requirements owing to its retrospective design.
Procedures
The decision to select PEG feeding or TPN was made after sufficient discussion, including patients or their family and clinicians. Appropriate nutrition was administered based on clinical evaluation by clinicians. Clinical details were obtained from patients’ medical records including age, gender, height, weight, underlying diseases, and blood test results.
Laboratory assays
The blood test results were performed within 7 days before the start of PEG feeding or TPN. Body mass index (BMI) was calculated using the height and weight measured on admission. Daily calorie was investigated on the seventh day after the procedure in both groups.
Outcomes
The primary outcome was defined as mortality after the start of the procedure during the follow-up period.
Statistical analysis
All normally distributed and skewed continuous variables were described as mean (SD) or median (interquartile range [IQR]). Categorical variables were expressed as frequencies (%). Baseline characteristics are presented according to the serum albumin by 3 g/dl. Multivariable Cox regression analysis were adopted to assess the independent association between serum albumin and mortality. An extended Cox model approach was used for different covariates adjusted models. Survival curves were plotted by Kaplan–Meier analyses. These potential confounders were chosen on the basis of previous scientific literature, or a more than 10% change in effect estimates. All the analysis were performed with the statistical software packages R (http://www.R-project.org, The R Foundation) and Free Statistics software versions 1.2.
Results
Study participants and baseline characteristics
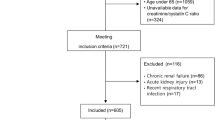
A total of 253 patients were included in the analysis, of whom the number of serum albumin below 3 g/dl was 93.Among them, there are 99 males and 154 females. 180 of whom underwent PEG feeding and 73 of whom underwent TPN. The median length of follow-up for censored cases was 601 days (range, 404–823 days). The mean age was 84.8 years old (SD 7.1) in low serum albumin group. The mean hemoglobin value was 9.8 g/dl (SD 1.9) in low serum albumin group. The median of survival time was 306 days. Baseline clinical and biochemical characteristics of participants were stratified by serum albumin (3 g/dl) in Table 1.
Kaplan–Meier curve
The Kaplan–Meier curve is illustrated in Fig. 1. The log-rank test shows a significantly longer mortality in the high group (serum albumin > = 3 g/dl) compared with the low group (median, 382 vs. 176 days, P < 0.0001).
Association between serum albumin and mortality in different models
Table 2 shows that unadjusted HR for the high group relative to the low group was 0.40 (95% CI: 0.29–0.57; P < 0.001). After adjustment in multivariable analysis in Table 2, serum albumin was significantly associated with mortality, so that survival time was longer in Alb ≥ 3 compared with Alb < 3 group. Furthermore, additional adjustment for age, sex, PEG, cerebrovascular diseases, severe dementia, neuromuscular diseases, aspiration pneumonia, chronic heart failure, total lymphocyte count (mm3), and c-reactive protein (mg/dl) did not substantially change the results. The adjusted HRs (95% CI) for total mortality rates were 0.46 (0.33–0.65), 0.66 (0.44–0.99) and 0.64 (0.42–0.97), from model 2 to model 4.
Discussion
In this study, we found that lower levels of serum albumin (< 3 g/dl) were associated with an increased risk of mortality. The association persisted after adjusting for different models. The elderly people are more likely to suffer malnutrition due to comprehensive factors, from physiological changes, such as appetite loss, changes in taste, depressive symptoms, to social and economic factors such as income, living circumstances and lifestyle19,20,21. Malnutrition in elderly was associated with higher mortality risk22 and poor Quality of life23.
Serum albumin, a protein which is synthesized in the liver24, is a marker of nutritional status of older people25,26. Serum albumin has antioxidative properties27 and low serum concentrations that have been suggested to be an indicator of inflammation, hypercoagulable states and liver disease28,29. The levels of serum albumin are associated with various diseases, although some studies do not provide direct evidence30, other studies report that a lower concentration of serum albumin is associated with cardiovascular mortality, acute respiratory distress syndrome , acute stroke, chronic kidney disease and other complications12,13,14,31,32. Indeed, a meta-analysis showed that hypoalbuminemia was an independent predictor of poor outcome33, which appeared to be independent of both nutritional status and inflammation. A study showed that low admission serum albumin was a prognostic determinant of 30 day case fatality and adverse functional outcome following acute ischemic stroke34. Meanwhile, high serum albumin has a protective effect on healthy older persons who do not have evidence of cytokine-mediated inflammation32.
On one hand, serum albumin may reflect the nutritional state of the human body. On the other hand, we can use proserum to supply the serum albumin when below 3 g/dl. Protein powders and a high protein diet was needed when the serum albumin was 3–4 g/dl. Albumin administration may improve organ function and in hypoalbuminemic critically ill patients35. However, results of the SOAP study16 showed ICU and hospital mortality rates were higher in patients who received albumin than those do not. Other two studies revealed the similar results, albumin using showed no benefit in outcome36,37. Further studies are needed to clarify the role of albumin in ICU patients.
The subgroup of PEG shows no differences in two groups (Supplementary Material Table 1). Previous studies have shown that enteral nutrition was associated with lower mortality rates38,39. Also there is no significant superiority of TPN feeding compared with PEG40,41. The FOOD study didn’t support a policy of early initiation of PEG feeding in dysphagic stroke patients42. There is strong evidence for not using enteral nutrition (EN) in the first week in dysphagic, and not using volitional nutrition support (VNS) in non-dysphagic stroke patients43.
There are some limitations to our study. First, subjects in this study were older people with dysphagia, thus limiting the generalizability of our findings. Some studies reported an inverse association between serum albumin and the incident CKD or CVD in middle-aged adults12,44,45. Because all the people in our study were over 50 years old, we could not predict the association of HSA and mortality in the middle aged people. Second, there is a possibility of a selection bias because we only had one measurement of serum albumin within 7 days of hospitalization, without follow-up measurements. We were unable to assess the effect of serum albumin levels at different time periods on outcomes. Third, this was a single-center study, and the size of sample is small, so a larger multicenter sample is needed to confirm this result. Fourth, this was a retrospective observational study, therefore, assignment to each group may have been biased. Information bias and unmeasured confounding could have influenced our results. Fifth, this study was conducted in elderly patients in Japan, it is uncertain whether it will be applicable in other countries, so more research evidences are needed.
Conclusions
Our results suggest that there is negative association between serum albumin and mortality in older people with dysphagia, implying we should pay more attention to the serum albumin levels of elderly patients, especially for hospitalized patients, monitor them regularly, and correct hypoproteinemia in time.
Data availability
The data are available at http://www.Datadryad.org/. which allows researchers to freely download the original data.
References
Lin, L. C. et al. Prevalence of impaired swallowing in institutionalized older people in Taiwan. J. Am. Geriatr. Soc. 50(6), 1118–1123 (2002).
Serra-Prat, M. et al. Oropharyngeal dysphagia as a risk factor for malnutrition and lower respiratory tract infection in independently living older persons: a population-based prospective study. Age Ageing 41(3), 376–381 (2012).
Kawashima, K., Motohashi, Y. & Fujishima, I. Prevalence of dysphagia among community-dwelling elderly individuals as estimated using a questionnaire for dysphagia screening. Dysphagia 19(4), 266–271 (2004).
Marik, P. E. & Kaplan, D. Aspiration pneumonia and dysphagia in the elderly. Chest 124(1), 328–336 (2003).
Ebihara, S. et al. Dysphagia, dystussia, and aspiration pneumonia in elderly people. J Thorac Dis 8(3), 632–639 (2016).
Cichero, J. A., Heaton, S. & Bassett, L. Triaging dysphagia: nurse screening for dysphagia in an acute hospital. J. Clin. Nurs. 18(11), 1649–1659 (2009).
Cabre, M. et al. Prevalence and prognostic implications of dysphagia in elderly patients with pneumonia. Age Ageing 39(1), 39–45 (2010).
Foley, N. C. et al. A review of the relationship between dysphagia and malnutrition following stroke. J Rehabil Med 41(9), 707–713 (2009).
Don, B. R. & Kaysen, G. Serum albumin: relationship to inflammation and nutrition. Semin. Dial. 6(17), 432–437 (2004).
Kim, S. & Kang, S. Serum albumin levels: a simple answer to a complex problem? Are we on the right track of assessing metabolic syndrome?. Endocrinol. Metab. (Seoul) 28(1), 17–19 (2013).
Friedman, A. N. & Fadem, S. Z. Reassessment of albumin as a nutritional marker in kidney disease. J. Am. Soc. Nephrol. 21(2), 223–230 (2010).
Ronit, A. et al. Plasma albumin and incident cardiovascular disease: results from the CGPS and an updated meta-analysis. Arterioscler. Thromb. Vasc. Biol. 40(2), 473–482 (2020).
Djousse, L. et al. Serum albumin and risk of myocardial infarction and all-cause mortality in the framingham offspring study. Circulation 106(23), 2919–2924 (2002).
Jiang, C. et al. U-shaped association between serum albumin and development of chronic kidney disease in general hypertensive patients. Clin. Nutr. 39(1), 258–264 (2020).
Byun, S. E. et al. The prevalence, risk factors and prognostic implications of dysphagia in elderly patients undergoing hip fracture surgery in Korea. BMC Geriatr. 19(1), 356 (2019).
Abubakar, S. et al. Low admission serum albumin as prognostic determinant of 30-day case fatality and adverse functional outcome following acute ischemic stroke. Pan. Afr. Med. J. 14, 53 (2013).
Masaki, S. & Kawamoto, T. Comparison of long-term outcomes between enteral nutrition via gastrostomy and total parenteral nutrition in older persons with dysphagia: a propensity-matched cohort study. PLoS ONE 14(10), e0217120 (2019).
Shigoka, H. et al. Comparison of modified introducer method with pull method for percutaneous endoscopic gastrostomy: prospective randomized study. Dig. Endosc. 24(6), 426–431 (2012).
de Morais, C. et al. Nutritional risk of European elderly. Eur. J. Clin. Nutr. 67(11), 1215–1219 (2013).
van Bokhorst-de, V. D. S. M. et al. Prevalence and determinants for malnutrition in geriatric outpatients. Clin. Nutr. 32(6), 1007–1011 (2013).
Amaral, T. F. et al. The economic impact of disease-related malnutrition at hospital admission. Clin. Nutr. 26(6), 778–784 (2007).
Cereda, E. et al. Nutritional screening and mortality in newly institutionalised elderly: a comparison between the geriatric nutritional risk index and the mini nutritional assessment. Clin. Nutr. 30(6), 793–798 (2011).
Rasheed, S. & Woods, R. T. Malnutrition and quality of life in older people: a systematic review and meta-analysis. Ageing Res. Rev. 12(2), 561–566 (2013).
Danesh, J. et al. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA 279(18), 1477–1482 (1998).
Zhang, Z. et al. Evaluation of blood biomarkers associated with risk of malnutrition in older adults: a systematic review and meta-analysis. Nutrients 9(8), 829 (2017).
Cabrerizo, S. et al. Serum albumin and health in older people: review and meta analysis. Maturitas 81(1), 17–27 (2015).
Harris, D. & Haboubi, N. Malnutrition screening in the elderly population. J. R. Soc. Med. 98(9), 411–414 (2005).
Phillips, A., Shaper, A. G. & Whincup, P. H. Association between serum albumin and mortality from cardiovascular disease, cancer, and other causes. Lancet 2(8677), 1434–1436 (1989).
Folsom, A. R. et al. Serum albumin and risk of venous thromboembolism. Thromb. Haemost. 104(1), 100–104 (2010).
Law, M. R., Morris, J. K., Wald, N. J. & Hale, A. K. Serum albumin and mortality in the BUPA study: British united provident association. Int. J. Epidemiol. 23, 38–41 (1994).
Famakin, B. et al. Hypoalbuminemia predicts acute stroke mortality: paul coverdell georgia stroke registry. J. Stroke Cerebrovasc. Dis. 19(1), 17–22 (2010).
Reuben, D. B. et al. The prognostic value of serum albumin in healthy older persons with low and high serum interleukin-6 (IL-6) levels. J. Am. Geriatr. Soc. 48(11), 1404–1407 (2000).
Vincent, J. L. et al. Hypoalbuminemia in acute illness: is there a rationale for intervention? a meta-analysis of cohort studies and controlled trials. Ann. Surg. 237(3), 319–334 (2003).
Dubois, M. J. et al. Albumin administration improves organ function in critically ill hypoalbuminemic patients: a prospective, randomized, controlled, pilot study. Crit. Care Med. 34(10), 2536–2540 (2006).
Vincent, J. L. et al. Is albumin administration in the acutely ill associated with increased mortality? results of the SOAP study. Crit. Care 9(6), R745–R754 (2005).
Caironi, P. et al. Albumin replacement in patients with severe sepsis or septic shock. N. Engl. J. Med. 370(15), 1412–1421 (2014).
Finfer, S. et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N. Engl. J. Med. 350(22), 2247–2256 (2004).
Abe, K. et al. Long-term survival of patients receiving artificial nutrition in japanese psychiatric hospitals. Dement. Geriatr. Cogn. Dis. Extra 6(3), 477–485 (2016).
Tamiya, H. et al. Comparison of short-term mortality and morbidity between parenteral and enteral nutrition for adults without cancer: a propensity-matched analysis using a national inpatient database. Am. J. Clin. Nutr. 102(5), 1222–1228 (2015).
Bito, S., Yamamoto, T. & Tominaga, H. Prospective cohort study comparing the effects of different artificial nutrition methods on long-term survival in the elderly: Japan assessment study on procedures and outcomes of artificial nutrition (JAPOAN). JPEN J. Parenter. Enteral Nutr. 39(4), 456–464 (2015).
Roth, B. et al. Parenteral nutrition does not improve postoperative recovery from radical cystectomy: results of a prospective randomised trial. Eur. Urol. 63(3), 475–482 (2013).
Dennis, M. S., Lewis, S. C. & Warlow, C. Effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): a multicentre randomised controlled trial. Lancet 365(9461), 764–772 (2005).
Koretz, R. L. et al. Does enteral nutrition affect clinical outcome? a systematic review of the randomized trials. Am. J. Gastroenterol. 102(2), 412–429 (2007).
Bash, L. D. et al. Inflammation, hemostasis, and the risk of kidney function decline in the atherosclerosis risk in communities (ARIC) study. Am. J. Kidney Dis. 53(4), 596–605 (2009).
Erlinger, T. P. et al. Leukocytosis, hypoalbuminemia, and the risk for chronic kidney disease in US adults. Am. J. Kidney Dis. 42(2), 256–263 (2003).
Acknowledgements
The authors are very grateful to Jie Liu, PhD (Department of Vascular and Endovascular Surgery, Chinese PLA General Hospital), Qi lin Yang (Department of Critical Care, The Second Affiliated Hospital of Guangzhou Medical University) for his helpful review and comments regarding the manuscript.
Funding
Key disciplines of Traditional Chinese and Ethnic medicine in Guizhou province during the 14th Five-year Plan: Traditional Chinese Medicine pulmonary disease.
Author information
Authors and Affiliations
Contributions
G.L. and T.F. proposed and designed the study; G.L., X.Z. and T.F. wrote the main manuscript. X.H., Y.L., D.L. provided assistance in statistics and mapping. All authors were responsible for the critical revision of the manuscript and approval before the final version was submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, G., Zhou, X., Hou, X. et al. Association between serum albumin and mortality in Japan older people with dysphagia. Sci Rep 12, 12089 (2022). https://doi.org/10.1038/s41598-022-16010-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-16010-y
- Springer Nature Limited
This article is cited by
-
The effect of pre-operative carbohydrate loading in femur fracture: a randomized controlled trial
BMC Musculoskeletal Disorders (2022)