Abstract
Introduction
Albumin administration in the critically ill has been the subject of some controversy. We investigated the use of albumin solutions in European intensive care units (ICUs) and its relationship to outcome.
Methods
In a cohort, multicenter, observational study, all patients admitted to one of the participating ICUs between 1 May and 15 May 2002 were followed up until death, hospital discharge, or for 60 days. Patients were classified according to whether or not they received albumin at any time during their ICU stay.
Results
Of 3,147 admitted patients, 354 (11.2%) received albumin and 2,793 (88.8%) did not. Patients who received albumin were more likely to have cancer or liver cirrhosis, to be surgical admissions, and to have sepsis. They had a longer length of ICU stay and a higher mortality rate, but were also more severely ill, as manifested by higher simplified acute physiology score (SAPS) II and sequential organ failure assessment (SOFA) scores than the other patients. A Cox proportional hazard model indicated that albumin administration was significantly associated with decreased 30-day survival. Moreover, in 339 pairs matched according to a propensity score, ICU and hospital mortality rates were higher in the patients who had received albumin than in those who had not (34.8 versus 20.9% and 41.3 versus 27.7%, respectively, both p < 0.001).
Conclusion
Albumin administration was associated with decreased survival in this population of acutely ill patients. Further prospective randomized controlled trials are needed to examine the effects of albumin administration in sub-groups of acutely ill patients.
Similar content being viewed by others
Introduction
Albumin administration in the critically ill is controversial and hotly debated, despite having been accepted and widely used for more than 50 years. A meta-analysis by the Cochrane group [1] published 5 years ago first put light to this fire, showing an increased mortality in patients treated with albumin in their analysis of 30 randomized controlled trials including 1,419 randomized patients. An accompanying editorial even suggested that, based on these results, "the administration of albumin should be halted" [2]. The Cochrane analysis was criticized by a later meta-analysis [3] because it excluded, for various reasons, several trials that had shown reduced mortality rates with albumin administration. When more studies were included into the meta-analysis, an adverse effect of albumin on mortality could no longer be demonstrated [3]. Both analyses, however, have the limitation that the inclusion criteria were very broad and the fluid regimen very different among the included trials. In a recent randomized controlled study (the Saline versus Albumin fluid Evaluation (SAFE) study) providing data on nearly 7,000 patients randomized to receive either albumin or normal saline as resuscitation fluid, there was no difference in outcome between the two groups [4].
While randomized controlled trials such as the SAFE study provide strong evidence for or against an intervention, epidemiological studies allowing for multivariable analyses can provide useful additional information on the current use of albumin and on associated outcomes. The Sepsis Occurrence in Acutely ill Patients (SOAP) study did exactly this to determine current intensive care unit (ICU) practice and the effects of that practice on outcomes for various topics, including administration of albumin.
Methods
Study design
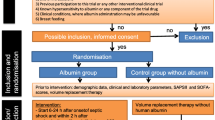
The SOAP study was a prospective, multicenter, observational study designed to evaluate the epidemiology of sepsis as well as other characteristics of ICU patients in European countries and was initiated by a working group of the European Society of Intensive Care Medicine. Institutional recruitment for participation was by open invitation from the study steering committee. As this epidemiological observational study did not require any deviation from routine medical practice, institutional review board approval was either waived or expedited in participating institutions and informed consent was not required. All patients older than 15 years admitted to the participating centers (see Acknowledgements below for a list of participating countries and centers) between 1 May and 15 May 2002 were included. Patients were followed up until death, hospital discharge, or for 60 days. Those who stayed in the ICU for less than 24 hours for routine postoperative observation were excluded.
Data management
Data were collected prospectively using preprinted case report forms. Detailed explanations of the aim of the study, instructions for data collection, and definitions for various important items were available for all participants via the Internet [5] before starting data collection and throughout the study period. The steering committee processed all queries during data collection.
Data were entered centrally by medical personnel using the SPSS v11.0 for Windows (SPSS Inc, Chicago, IL, USA). A sample of 5% of data was re-entered by a different encoder and revised by a third; a consistency of more than 99.5% per variable and 98.5% per patient were observed during the whole process of data entry. In cases of inconsistency, data were verified and corrected. Daily frequency tables were revised for all variables and the investigators were queried when data values were either questionable or missing for required fields. There was no data quality control at the data collection level.
Data collection on admission included demographic data and comorbidities. Clinical and laboratory data for the simplified acute physiology (SAPS) II score [6] were reported as the worst value within 24 hours after admission. Microbiological and clinical infections were reported daily as well as the antibiotics administered. A daily evaluation of organ function, based on a set of laboratory and clinical parameters according to the sequential organ failure assessment (SOFA) score [7], was performed, with the most abnormal value for each of the six organ systems (respiratory, renal, cardiovascular, hepatic, coagulation, and neurological) being collected on admission and every 24 hours thereafter. For a single missing value, a replacement was calculated using the mean value of the results on either side of the absent result. When the first or last values were missing the nearest value was carried backward or forward, respectively. When more than one consecutive result was missing, it was considered to be a missing value in the analysis. Overall, missing data represented less than 6% of collected data, and 2% of these values were replaced.
Definitions
Infection was defined as the presence of a pathogenic microorganism in a sterile milieu (such as blood, abscess fluid, cerebrospinal or ascitic fluid), and/or clinically documented infection, plus the administration of antibiotics. Sepsis was defined according to the American College of Chest Physicians/Society of Critical Care Medicine (ACCP/SCCM) consensus conference definitions, by infection plus two systemic inflammatory response syndrome (SIRS) criteria [8]. Organ failure was defined as a SOFA score >2 for the organ in question [9]. Severe sepsis was defined by sepsis plus at least one organ failure. Mean fluid balance was calculated as the total fluid balance during the ICU stay divided by the duration of ICU stay in days.
Statistical methods
Data were analyzed using SPSS v11.0 for Windows (SPSS Inc, Chicago, IL, USA). Descriptive statistics were computed for all study variables. The Kolmogorov-Smirnov test was used and stratified distribution plots were examined to verify the normality of distribution of continuous variables. Nonparametric tests of comparison were used for variables evaluated as not normally distributed. Difference testing between groups was performed using the two-tailed t test, Mann-Whitney U test, Chi square test, and Fisher exact test as appropriate. To determine the relative hazard of death due to albumin administration, a Cox proportional hazard model [10] was constructed with time to death, right censored at 30 days as the dependent factor and, as independent factors, age, sex, trauma, comorbidities on admission, SAPS II score on admission, the timing of onset of albumin administration, use of other colloids and blood products (red blood cells, fresh frozen plasma), and the mean fluid balance, the degree of organ failure assessed by the SOFA score, procedures (mechanical ventilation, pulmonary artery catheter, renal replacement therapy), and the presence of sepsis syndromes on admission in patients who did not receive albumin and at onset of albumin administration in those who did, were also included as independent variables. Covariates were selected and entered in the model if they attained a p value <0.2 on a univariate basis. Seven countries were included in the model, six being identified as a risk of decreased survival and one with a favorable prognosis compared with the others. A forward stepwise approach was performed. Only significant variables were retained in the final model. The time dependent covariate method [10] was used to check the proportional hazard assumption of the model; an extended Cox model was constructed, adding interaction terms that involve time (for example, time dependent variables) computed as the byproduct of time and individual covariates in the model (time*covariate); individual time dependent covariates were introduced one by one and in combinations in the extended model, none of which was found to be significant (Wald chi-square statistic). The Cox proportional hazard model was reconstructed, stratifying patients according to the presence or absence of trauma or severe sepsis.
Propensity scores [11] were obtained through forward stepwise logistic regression of patients' characteristics on albumin infusion status [11–14], that is, albumin administration as the dependent factor (Table 1). Variables were entered into the model and removed at a cutoff p value of 0.2. The propensity score was calculated as the probability based upon the final model. A greedy matching technique [15] was used to match individual patients who received albumin at any time with individual patients without albumin based on propensity scores. The best-matched propensity score was identical to five digits. Once a match was made, the control patient was removed from the pool. This process was then repeated using four-digit matching, then three-digit matching, and so on. The process proceeded sequentially to a single-digit match on propensity score. If a match was not obtained at this point, the patient who had received albumin was excluded. Baseline characteristics were compared between the two matched groups without comparing mortality and the process was repeated by adding interactions to the logistic regression model involving the unmatched covariates, including replacing it by its square or multiplying two unmatched covariates [12]. Kaplan Meier survival curves were plotted and compared using the signed Log Rank test in the propensity score matched pairs. Another Cox regression model was constructed as described above in the group of matched pairs involving the propensity score as a covariate. All statistics were two-tailed and a p value <0.05 was considered to be statistically significant.
Results
Of 3,147 patients, 354 (11.2%) received albumin and 2,793 (88.8%) did not. Figure 1 represents the proportion of patients who received albumin in the 14 most represented countries. In general, albumin administration was more commonly used in the south of Europe. Albumin was administered during the first 24 hours following admission in 157 (44.4%) of those who received it; only 34 patients (7.6%) received albumin after 7 days of admission.
Clinical data are presented in Table 2. Patients who received albumin had the same mean age, but were more likely to have cancer or liver cirrhosis, to be a surgical admission, and to have sepsis than the patients who did not receive albumin. They had a longer length of ICU stay and a higher ICU mortality rate (35 versus 16%, p < 0.001), but were also more severely ill, as manifested by higher SAPS II and SOFA scores than the other patients. At the onset of albumin administration (Table 3), these patients had a higher degree of organ dysfunction failure as manifested by higher SOFA scores and higher incidence of sepsis and invasive procedures (mechanical ventilation, pulmonary artery catheterization, and renal replacement therapy) compared with these factors on admission in patients who never received albumin during the ICU stay.
In the Cox proportional hazard model, albumin administration was independently associated with a lower 30-day survival (relative hazard 1.57, 95% confidence interval (CI) 1.11–2.22, p = 0.012; Table 4). Albumin remained an independent risk of lower 30-day survival when stratifying for trauma (n = 254) or severe sepsis (n = 765) (Table 5). Moreover, in 339 pairs matched according to a propensity score, ICU (34.8 versus 20.9%, p < 0.001) and hospital (41.3 versus 27.7%, p < 0.001) mortality rates were higher in patients who received albumin than in those who did not; the survival curves are shown in Figure 2. In these matched pairs, albumin administration was associated with a decreased 30-day survival in a multivariable Cox proportional hazard analysis (relative hazard 1.57, 95% CI 1.19–2.07, p = 0.001; Table 4). Table 6 shows the baseline characteristics of the propensity-matched patients on admission on the basis of age, gender, comorbidities, type of admission, SAPS II and SOFA scores, procedures, and sepsis syndromes. Propensity scores were also associated with a decreased 30-day survival, both in the whole population and in the matched pairs.
Discussion
In this observational study, patients who received albumin had higher ICU and hospital mortality rates than those who did not. This may be expected, as albumin administration is generally added to resuscitative fluids in very ill patients or patients with hypoalbuminemia and/or edema. Hypoalbuminemia itself is an independent predictor of an adverse outcome [16–18]. In the present study, patients who received albumin were also more severely ill, with a higher frequency of cancer, liver cirrhosis, and sepsis, and significantly higher SAPS II scores. Independent of albumin administration, these patients, therefore, had a higher risk of death than patients who did not receive albumin. We applied two different methods to control for these confounding factors. Firstly, we included the confounding variables in a Cox proportional hazard model. Secondly, we produced unbiased estimators of the effects of albumin administration on mortality rates by using a propensity analysis. In both analyses, the mortality rates after adjustment for confounding factors were still higher in patients who received albumin than in those who did not. Therefore, the administration of albumin was associated with higher mortality independent of those comorbid conditions included in our statistical models.
Although a prospective, controlled randomized clinical trial is, of course, the optimal means of demonstrating cause and effect, epidemiological studies with adequate multivariable analysis can provide valuable information. A similar approach has been taken to show that aspirin administration may reduce complications after coronary artery bypass grafting [19]. One must, however, remember that a multivariable analysis cannot take all factors into account, so that other unidentified factors in the patients who received albumin may have influenced the results. Nevertheless, many factors, including comorbid diseases, were included in the analysis due to the epidemiological nature of this study. Regional factors may also influence results and, indeed, there were considerable regional variations, with albumin generally being used more commonly in the south of Europe; however, we corrected for regional differences in our multivariable model.
The SOAP study was not originally designed to specifically address questions regarding albumin administration in the ICU. This analysis, therefore, has some limitations in addition to those of a multivariable analysis. First, the indications for albumin administration were not recorded. Second, serum albumin levels were not measured and it thus remains unclear whether albumin levels were successfully corrected in patients treated with albumin. Indeed, there are data suggesting that the use of albumin in patients with hypoalbuminemia may be beneficial. In a recently published meta-analysis [16], nine studies addressing morbidity in critically ill patients after correction of hypoalbuminemia were identified. There was a trend towards reduced morbidity in patients where hypoalbuminemia was corrected (odds ratio 0.74; 95% CI 0.41–1.60). The meta-analysis also suggested that albumin levels need to reach more than 30 g/l before albumin replacement becomes effective [16]; only four of the nine studies achieved this goal. It should be pointed out that three of the four studies were undertaken in pediatric patients. Another recent meta-analysis noted a trend towards reduced morbidity in hypoalbuminemic patients who received albumin (relative risk 0.92; 95% CI 0.77–1.08) [20]. Nevertheless, it remains unproven whether an improvement in morbidity translates into an improvement in survival.
The reason for an increased mortality in patients who received albumin cannot be identified from our study. Albumin has well-recognized, potentially important functions in the critically ill, including maintenance of colloid oncotic pressure, binding capacity for drugs and other substances, and scavenging of oxygen free radicals [21]. Starling's principle may not appropriately reflect the microcirculation in critically ill patients, however, especially under conditions of capillary leakage, as may happen in sepsis or burns [22]. Other possible negative effects of albumin administration may include myocardial depression due to decreased ionic calcium [23], and impaired renal function [24, 25]. Furthermore, albumin has anti-thrombotic properties that might be detrimental in some patients [1, 26].
The recently completed, randomized controlled SAFE study [4] showed no differences in outcome in critically ill patients requiring fluid repletion who were treated with 4% albumin compared to those treated with saline. The SAFE study was without doubt a well-conducted study that answered adequately the question it asked, that is, that in a heterogeneous population of critically ill patients albumin does not seem to have harmful effects. However, albumin was given, often transiently, as part of a fluid challenge and a 4% albumin solution was used. Therefore, a number of patients received only small amounts of albumin that were unlikely to influence outcome.
Conclusion
Albumin may indeed be safe when used as a resuscitation fluid (as shown by the SAFE study), but our results suggest that it may not be safe all of the time in all critically ill patients. We believe further studies, such as the present, are needed to generate hypotheses and encourage further research to fully clarify the role of albumin in our ICUs.
Key messages
-
In this observational study of 3,147 patients, albumin administration was independently associated with a lower 30-day survival, using a Cox proportional hazard model.
-
Moreover, in 339 pairs matched according to a propensity score, ICU and hospital mortality rates were higher in patients who received albumin than in those who did not.
-
While albumin administration may be safe in patients requiring fluid for intravascular volume depletion, these results suggest it may not be harmless in all ICU patients.
Abbreviations
- CI:
-
confidence interval
- ICU:
-
intensive care unit
- SAFE:
-
saline versus albumin fluid evaluation
- SAPS:
-
simplified acute physiology score
- SOAP:
-
sepsis occurrence in acutely ill patients
- SOFA:
-
sequential organ failure assessment.
References
Cochrane Injuries Group: Human albumin administration in critically ill patients: systematic review of randomized controlled trials. BMJ 1998, 317: 235-240.
Offringa M: Excess mortality after human albumin administration in critically ill patients. Clinical and pathophysiological evidence suggests albumin is harmful. BMJ 1998, 317: 223-224.
Wilkes MM, Navickis RJ: Patient survival after human albumin administration. A meta-analysis of randomized, controlled trials. Ann Intern Med 2001, 135: 149-164.
Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, SAFE Study Investigators: A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 2004, 350: 2247-2256. 10.1056/NEJMoa040232
The SOAP Study[http://www.intensive.org/soap/index.cfm]
Le Gall JR, Lemeshow S, Saulnier F: A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 1993, 270: 2957-2963. 10.1001/jama.270.24.2957
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG: The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996, 22: 707-710.
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: Definitions of sepsis and multiple organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 1992, 20: 864-874.
Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter P, Sprung C, Colardyn FC, Blecher S: Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicentric, prospective study. Working group on "Sepsis-related problems" of the European Society of Intensive Care Medicine. Crit Care Med 1998, 26: 1793-1800.
Cox DR: Regression models and life tables. J R Stat Soc Ser B 1972, 34: 187-220.
Rosenbaum PR, Rubin DB: The central role of the propensity score on observational studies for causal effects. Biometrika 1983, 70: 41-55.
Rosenbaum PR, Rubin DB: Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc 1984, 79: 516-523.
D'Agostino RB Jr: Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998, 17: 2265-2281. 10.1002/(SICI)1097-0258(19981015)17:19<2265::AID-SIM918>3.0.CO;2-B
Rubin DB: Estimating causal effects from large data sets using propensity scores. Ann Intern Med 1997, 127: 757-763.
Gum PA, Thamilarasan M, Watanabe J, Blackstone EH, Lauer MS: Aspirin use and all-cause mortality among patients being evaluated for known or suspected coronary artery disease: A propensity analysis. JAMA 2001, 286: 1187-1194. 10.1001/jama.286.10.1187
Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM: Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg 2003, 237: 319-334. 10.1097/00000658-200303000-00005
Engelman DT, Adams DH, Byrne JG, Aranki SF, Collins JJ Jr, Couper GS, Allred EN, Cohn LH, Rizzo RJ: Impact of body mass index and albumin on morbidity and mortality after cardiac surgery. J Thorac Cardiovasc Surg 1999, 118: 866-873. 10.1016/S0022-5223(99)70056-5
Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF: Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg 1999, 134: 36-42. 10.1001/archsurg.134.1.36
Mangano DT, Multicenter Study of Perioperative Ischemia Research Group : Aspirin and mortality from coronary bypass surgery. N Engl J Med 2002, 347: 1309-1317. 10.1056/NEJMoa020798
Vincent JL, Navickis RJ, Wilkes MM: Morbidity in hospitalized patients receiving human albumin: a meta-analysis of randomized, controlled trials. Crit Care Med 2004, 32: 2029-2038. 10.1097/01.CCM.0000142574.00425.E9
Emerson TE Jr: Unique features of albumin: a brief review. Crit Care Med 1989, 17: 690-694.
Berger A: Why albumin may not work. BMJ 1998, 317: 240.
Kovalik SG, Ledgerwood AM, Lucas CE, Higgins RF: The cardiac effect of altered calcium homeostasis after albumin resuscitation. J Trauma 1981, 21: 275-279.
Moon MR, Lucas CE, Ledgerwood AM, Kosinski JP: Free water clearance after supplemental albumin resuscitation for shock. Circ Shock 1989, 28: 1-8.
Gore DC, Dalton JM, Gehr TW: Colloid infusions reduce glomerular filtration in resuscitated burn victims. J Trauma 1996, 40: 356-360.
Pulimood TB, Park GR: Debate: Albumin administration should be avoided in the critically ill. Crit Care 2000, 4: 151-155. 10.1186/cc688
Acknowledgements
This study is endorsed by the European Society for Intensive Care Medicine, and supported by an unrestricted grant from Abbott, Baxter, Eli Lilly, GlaxoSmithKline and NovoNordisk.
Participants by country (listed alphabetically). Austria: University Hospital of Vienna (G Delle Karth); LKH Steyr (V Draxler); LKH-Deutschlandsberg (G Filzwieser); Otto Wagner Spital of Vienna (W Heindl); Krems of Donau (G Kellner, T Bauer); Barmherzige Bruede of Linz (K Lenz); KH Floridsdorf of Vienna (E Rossmann); University Hospital of Innsbruck (C Wiedermann); Belgium: CHU of Charleroi (P Biston); Hôpitaux Iris Sud of Brussels (D Chochrad); Clinique Europe Site St Michel of Brussels (V Collin); CHU of Liège (P Damas); University Hospital Ghent (J Decruyenaere, E Hoste); CHU Brugmann of Brussels (J Devriendt); Centre Hospitalier Jolimont-Lobbes of Haine St Paul (B Espeel); CHR Citadelle of Liege (V Fraipont); UCL Mont-Godinne of Yvoir (E Installe); ACZA Campus Stuivenberg (M Malbrain); OLV Ziekenhuis Aalst (G Nollet); RHMS Ath-Baudour-Tournai (JC Preiser); AZ St Augustinus of Wilrijk (J Raemaekers); CHU Saint-Pierre of Brussels (A Roman); Cliniques du Sud-Luxembourg of Arlon (M Simon); Academic Hospital Vrije Universiteit Brussels (H Spapen); AZ Sint-Blasius of Dendermonde (W Swinnen); Clinique Notre-Dame of Tournai (F Vallot); Erasme University Hospital of Brussels (JL Vincent); Czech Republic: University Hospital of Plzen (I Chytra); U SV Anny of Brno (L Dadak); Klaudians of Mlada Boleslav (I Herold); General Faculty Hospital of Prague (F Polak); City Hospital of Ostrava (M Sterba); Denmark: Gentofte Hospital, University of Copenhagen (M Bestle); Rigshospitalet of Copenhagen (K Espersen); Amager Hospital of Copenhagen (H Guldager); Rigshospitalet, University of Copenhagen (K-L Welling); Finland: Aland Central Hospital of Mariehamn (D Nyman); Kuopio University Hospital (E Ruokonen); Seinajoki Central Hospital (K Saarinen); France: Raymond Poincare of Garches (D Annane); Institut Gustave Roussy of Villejuif (P Catogni); Jacques Monod of Le Havre (G Colas); CH Victor Jousselin of Dreux (F Coulomb); Hôpital St Joseph & St Luc of Lyon (R Dorne); Saint Joseph of Paris (M Garrouste); Hôpital Pasteur of Nice (C Isetta); CHU Brabois of Vandoeuvre Les Nancy (J Larché); Saint Louis of Paris (J-R LeGall); CHU de Grenoble (H Lessire); CHU Pontchaillou of Rennes (Y Malledant); Hôpital des Hauts Clos of Troyes (P Mateu); CHU of Amiens (M Ossart); Hôpital Lariboisière of Paris (D Payen); CHD Félix Gyuon of Saint Denis La Reunion (P Schlossmacher); Hôpital Bichat of Paris (J-F Timsit); Hôpital Saint Andre of Bordeaux (S Winnock); Hôpital Victor Dupouy of Argentueil (J-P Sollet); CH Auch (L Mallet); CHU Nancy-Brabois of Vandoeuvre (P Maurer); CH William Morey of Chalon (J-M Sab); Victor Dupouy of Argenteuil (J-P Sollet); Germany: University Hospital Heidelberg (G Aykut); Friedrich Schiller University Jena (F Brunkhorst); University Clinic Hamburg-Eppendorf (A Nierhaus); University Hospital Mainz (M Lauterbach); University Hospital Carl Gustav Carus of Dresden (M Ragaller); Hans Sushemihl Krankenhaus of Emden (R Gatz); Vivantes-Klinikum Neukoelln of Berlin (H Gerlach); University Hospital RWTH Aachen (D. Henzler); Kreisklinik Langen-Seligenstadt (H-B Hopf); GKH Bonn (H Hueneburg); Zentralklinik Bad Berka (W Karzai); Neuwerk of Moenchengladbach (A Keller); Philipps University of Marburg (U Kuhlmann); University Hospital Regensburg (J Langgartner); ZKH Links der Weser of Bremen (C Manhold); University Hospital of Dresden (M Ragaller); Universtiy of Wuerzburg (B Reith); Hannover Medical School (T Schuerholz); Universitätsklinikum Charité Campus Mitte of Berlin (C Spies); Bethanien Hospital of Moers (R Stögbauer); KhgmbH Schongau (J Unterburger); Greece: Thriassio Hospital of Athens (P-M Clouva-Molyvdas); Sismanoglion General Hospital of Athens (G Giokas); KAT General Hospital of Athens (E Ioannidou); G Papanikolaou General Hospital of Thessaloniki (A Lahana); Agios Demetrios of Thessaloniki (A Liolios); Onassis Cardiac Surgery Center of Athens (K Marathias); University Hospital of Ioannina (G Nakos); Tzanio Hospital of Athens (A Tasiou); Athens Gen Hosp Gennimatas (H Tsangaris); Hungary: Peterfy Hospital of Budapest (P Tamasi); Ireland: Mater Hospital of Dublin (B Marsh); Beaumont Hospital of Dublin (M Power); Israel: Hadassah Hebrew University Medical Center (C Sprung); Italy: Azienda Ospedaliera Senese o Siena (B Biagioli); S Martino of Genova (F Bobbio Pallavicini); Azienda Ospedaliera S Gerardo dei Tintori of Monza (A Pesenti); Osp Regionale of Saronno (C Capra); Ospedale Maggiore – University A Avogadro of Novara (F Della Corte); Osp Molinette of Torino (P P Donadio); AO Umberto I Ancona, Rianimazione Clinica (A Donati); Azienda Ospedaliera Universitaria Policlinico of Palermo (A Giarratano); San Giovanni Di Dio of Florence (T Giorgio); H San Raffaele IRCCS of Milano (D Giudici); Ospedale Di Busto Arsizio (S Greco); Civile Di Massa (A Guadagnucci); San Paolo of Milano (G Lapichino); S Giovanni Bosco Torino (S Livigni); Osp San Giovanni of Sesto (G Moise); S Camillo of Roma (G Nardi); Vittorio Emanuele of Catania (E Panascia); Hospital of Piacenza (M Pizzamiglio); Universita di Torino-Ospedale S Giovanni Battista (VM Ranieri); Policlinico Le Scotte of Siena (R Rosi); Ospedale Maggiore Policlinico IRCCS of Milano (A Sicignano); A Uboldo of Cernusco Sul Naviglio (M Solca); PO Civile Carrara of Massa (G Vignali); San Giovanni of Roma (I Volpe Rinonapoli); Netherlands: Boven IJ Ziekenhuis of Amsterdam (M Barnas); UMC St Radboud of Nijmegen (EE De Bel); Academic Medical Center of Amsterdam (A-C De Pont); VUMC of Amsterdam (J Groeneveld); Groningen University Hospital (M Nijsten); Waterlandziekenhuis of Purmerend (L Sie); OLVG of Amsterdam (DF Zandstra); Norway: Sentralsjukehuset i Rogaland of Stavanger (S Harboe); Sykehuset Østfold of Fredrikstad (S Lindén); Aker University Hospital of Oslo (RZ Loversustad); Ulleval University Hospitalof Oslo (H Moen); Akershus University Hospital of Nordbyhagen (N Smith-Erichsen); Poland: Paediatric University Hospital of Lodz (A Piotrowski); Central Clinic Hospital SLAM of Katowice (E Karpel); Portugal: Garcia de Orta of Almada (E Almeida); Hospital de St António dos Capuchos of Lisboa (R Moreno); Hospital de Santa Maria of Lisboa (A Pais-De-Lacerda); Hospital S Joao of Porto (JA Paiva); Fernado Fonseca of Masama (I Serra); São Teotonio Viseu (A Pimentel); Romania: Inst of Cardiovascular Diseases of Bucharest (D Filipescu); Serbia and Montenegro: Military Medical Academy of Belgrade (K Jovanovic); Slovakia: SUSCH of Bratislava (P Malik); Slovenia: General Hospital of Novo Mesto (K Lucka); General Hospital of Celje (G Voga); Spain: Hospital Universitario Rio Hortega of Valladolid (C Aldecoa Alvarez-Santullano); Sabadell Hospital (A Artigas); Hospital Clinic of Barcelona (E Zavala, A Escorsell, J Nicolas); Virgen del Camino of Pamplona (JJ Izura Cea); Virgen de la Salud of Toledo (L Marina); 12 de Octubre of Madrid (J Montejo); Gregorio Maranon of Madrid (E Palencia); General Universitario de Elche (F Santos); Puerta del Mar of Cadiz (R Sierra-Camerino); Fundación Jiménez Díaz of Madrid (F Sipmann); Hospital Clinic of Barcelona (E Zavala); Sweden: Central Hospital of Kristianstad (K Brodersen); Stockholm Soder Hospital (J Haggqvist); Sunderby Hospital of Luleå (D Hermansson); Huddinge University Hospital of Stockholm (H Hjelmqvist); Switzerland: Kantonsspital Luzern (K Heer); Hirslanden Klinik Beau-Site of Bern (G Loderer); University Hospital of Zurich (M Maggiorini); Hôpital de la ville of La Chaux-de-Fonds (H Zender); United Kingdom: Western General Hospital of Edinburgh (P Andrews); Peterborough Hospitals NHS Trust of Peterborough (B Appadu); University Hospital Lewisham, London (C Barrera Groba); Bristol Royal Infirmary (J Bewley); Queen Elizabeth Hospital Kings Lynn (K Burchett); Milton Keynes General (P Chambers); Homerton University Hospital of London (J Coakley); Charing Cross Hospital of London (D Doberenz); North Staffordshire Hospital of Stoke On Trent (N Eastwood); Antrim Area Hospital (A Ferguson); Royal Berkshire Hospital of Reading (J Fielden); The James Cook University Hospital of Middlesbrough (J Gedney); Addenbookes of Cambridge (K Gunning); Rotherham DGH (D Harling); St Helier of Carshalton (S Jankowski); Southport & Formby (D Jayson); Freeman of Newcastle Upon Tyne (A Kilner); University Hospital of North Tees at Stockton on Tees (V Krishna-Kumar); St Thomas Hospital of London (K Lei); Royal Infirmary of Edinburgh (S Mackenzie); Derriford of Plymouth (P Macnaughton); Royal Liverpool University Hospital (G Marx); Stirling Royal Infirmary (C McCulloch); University Hospital of Wales, Cardiff (P Morgan); St George's Hospital of London (A Rhodes); Gloucestershire Royal Hospital (C Roberts); St Peters of Chertsey (M Russell); James Paget Hospital of Great Yarmouth (D Tupper-Carey, M Wright); Kettering General Hospital (L Twohey); Burnley DGH (J Watts); Northampton General Hospital (R Webster); Dumfries Royal Infirmary (D Williams)
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
JLV has received research grants from PPTA. The other authors declare that they have no competing interests.
Authors' contributions
JLV and YS participated in the design of the study. All authors contributed to data collection. YS performed the statistical analyses. JLV and YS drafted the manuscript. KR, CLS, HG, VMR revised the article. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Vincent, JL., Sakr, Y., Reinhart, K. et al. Is albumin administration in the acutely ill associated with increased mortality? Results of the SOAP study. Crit Care 9, R745 (2005). https://doi.org/10.1186/cc3895
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc3895