Abstract
Environmental exposures interact with genetic factors has been thought to influence susceptibility of systemic lupus erythematosus (SLE) development. To evaluate the effects of environmental exposures on SLE, we conducted a population-based cohort study across Jiangsu Province, China, to examine the associations between the living environment including air and water pollution, population density, economic income level, etc. and the prevalence and mortality of hospitalized SLE (h-SLE) patients. A total of 2231 h-SLE patients were retrieved from a longitudinal SLE database collected by the Jiangsu Lupus Collaborative Group from 1999 to 2009. The results showed that: It existed regional differences on the prevalence of h-SLE patients in 96 administrative districts; The distribution of NO2 air concentration monitored by atmospheric remote sensors showed that three of the ultra-high-prevalence districts were located in the concentrated chemical industry emission area; h-SLE patient prevalence was positively correlated with the excessive levels of nitrogen in drinking water; The positive ratio of pericarditis and proteinuria was positively correlated with the prevalence of h-SLE patients and pollution not only induced a high h-SLE patient prevalence but also a higher mortality rate, which might be attributed to NOx pollution in the air and drinking water. In summary, our data suggested that NOx in air and drinking water may be one of the important predispositions of SLE, especially for patients with renal involvement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Systemic lupus erythematosus (SLE) is a multi-systemic chronic autoimmune disease with multifactorial etiology1. Evidence support that multiple factors contribute to SLE pathogenesis and clinical manifestations, including genetic susceptibility, environmental effects, and disturbances in both innate and adaptive immunity manifest2,3,4,5,6.
The possibility that virus may trigger SLE has been considered during the past 40 years7,8,9. Evidence for an environmental component in SLE arises from observations that the majority of lupus cases are idiopathic, drugs such as procainamide, hydralazine and other factors including smoking as well as UV light trigger lupus-like autoimmunity10,11,12, and the incomplete concordance between genetically identical twins13. Recently, environmental pollution has been threatening human health. The increased air pollutant concentration levels are positively correlated with the risk of SLE, NO2, SO2, CO, O3 and so on in the air are all considered to be potential risk factors for systemic inflammation in patients with SLE14. A nationwide population-based case–control study from Taiwan, China, support that the development of SLE was positively associated with NO2 exposure, but negatively with CO exposure15. Fernandes et al. explored the relationship between exposure to air pollutants and disease activities in 22 children with SLE (c-SLE), and found that exposure under PM10, NO2 and CO for about 2 weeks was a risk factor for c-SLE activity (SLEDAI-2K > 8), and moving average of the PM10 increased to 13.4 μg/m3 could increase the risk of SLEDAI-2K > 8 by 34%16. Alves et al. conducted a longitudinal panel study of 108 repeated measurements of 9 children with lupus for one year, and found that NO2 level was associated with decreased serum C3 levels17.
Pollution from drinking water sources has been proven to be the cause of SLE. Ingestion of NO3- can cause methemoglobinemia18, further, virus, bacteria, heavy metals, pesticide residues such as agricultural pesticides and antibiotics, industrial wastewater, agricultural non-point source pollution, domestic sewage and other pollutants entering the drinking water may increase the risk of SLE19,20. The comparative experimental analysis results of single chemicals in drinking water and the incidence of SLE all show a certain correlation21. The environment may be associated with epigenetic changes caused by exposure, increased oxidative stress, systemic inflammation and upregulation of inflammatory cytokines, and hormonal effects. Environmental agents can alter T cell gene expression through effects on DNA methylation, resulting in autoreactive T cells that promote autoimmunity22. Further, ERK pathway signaling is an important regulator of DNA methyltransferase 1 (DNMT1) that is decreased in hydralazine-treated T cells and in T cells from patients with idiopathic lupus23. Therefore, environmental agents that inhibit ERK signaling, its upstream regulator protein kinase C delta (PKC-d), or other conditions such as diet and aging, that impact DNMT1 activity may increase methylation-sensitive gene expression through epigenetic mechanisms to cause a lupus-like disease in genetically predisposed individuals24,25. All of these data support that environmental pollutants have proinflammatory effects and are therefore contributing to the generation of inflammation and autoimmunity.
However, the correlation between air and water pollutions and SLE development is still largely unknown, because it is difficult to rule out the living environment interference factors of each patient in the experimental group, and rare multi-center, large sample, systematic retrospective analysis was reported, which limit the effective and targeted solutions for the prevention of SLE prevalence induced by air and water pollutions. Here we investigated the living environment of 2231 hospitalized SLE (h-SLE) patients distributed in 96 administrative districts of 13 cities in Jiangsu Province, China, from 1999 to 2009, and analyzed the dataset for interrelations and mutual spatial occurrence to examine the relationship between the living environment including air and water pollution, population density, economic income level, etc. and the prevalence of h-SLE patients. Our data showed NOx in air and drinking water may be one of the important predispositions of SLE, especially for patients with renal involvement, while the economic and living standards had no effect on h-SLE patient prevalence distribution.
Materials and methods
Study population
A total of 2231 individuals were retrieved from a longitudinal SLE database collected by the Jiangsu Lupus Collaborative Group from 1999 to 2009. The distribution of the year of admission and diagnosis of 2231 patients, who were all hospitalized for the first time, was shown in Supplementary Fig. S1A,B, and more than 70% patients were initially diagnosed with SLE (Supplementary Fig. S1C), 44% patients were severe SLE (SLEDAI score > 14) patients (Supplementary Table S1). The demographic and clinical characteristics data of h-SLE patients was presented in Table 1 and Supplementary Table S2, and SLEDAI distribution of these patients was shown in Supplementary Fig. S1D.
Measurement of NO2 concentration in Jiangsu
The ozone monitoring instrument (OMI) equipped with the AURA satellite was launched in 2004 to monitor NO2 concentration. The OMI detector has a spatial resolution of 13 km × 24 km, and could cover the world every day. We selected the average data of NO2 tropospheric column concentration in August 2005. Due to the complexity of the spatial resolution of the original raster data, we first converted the original raster data into points vector data in ARCGIS10.2, and then used Kriging space interpolation method for point vector data to obtain the spatial distribution map of NO2 concentration in Jiangsu Province, at the same time, the patient’s geographic coordinate information was used to project the patient onto the concentration distribution map, and then regional statistical analysis was used to calculate the NO2 concentration in each administrative district.
Measurement of Night light in Jiangsu
The first generation of luminous data is derived from the Operational Linescan System (OLS) carried by the Defense Meteorological Satellite Program (DMSP) in the last century, which has the world's longest time series data stock (1992–2013). The luminous radiation signal on the DMSP/OLS image is discretized into digital number values (DN value, range 0–63), and the area covered by a high DN value usually corresponds to an area with a higher level of human activity and economic development. We selected the 2003 DMSP/OLS image, and through related processing including cropping, denoising, got luminous distribution map in Jiangsu Province, and used the patient's geographic coordinate information to project the patients onto the concentration distribution map, and then used regional statistical analysis to calculate night light value in each administrative district.
Measurement of Water chemistry type in Jiangbei
Shi et al. investigated and discussed the characteristics and evolution of groundwater quality in the northern plains of Jiangsu Province on the basis of field data including 597 data collected in the 1980s and 1346 samples analyzed in the 2000s. We referred to the cation distribution map of the water chemical phase of the diving aquifer in the 2000s in the paper published by him, draw the distribution map of the cation water chemistry type in northern Jiangsu, and estimated the h-SLE patient prevalence of each type of water chemistry type based on the proportion of the element coverage area, and projected the patients to the water chemistry type distribution map.
Statistical analysis
Data statistics adopt district, classification and level statistics, and datasets were analyzed for interrelations and mutual spatial occurrence using statistical approaches including correlation analysis and significant difference analysis.
SPSS software version 22.0, GraphPad Prism version 8.0, Microsoft Excel version 2019 and Python version 3.7 were used for statistical analyses. Continuous data were expressed as means and standard deviations, whereas Categorical data were presented as a percentage. Non-normally distributed data were analyzed using the Mann–Whitney U-test. Categorical data were compared by means of the χ2 test. The prevalence and mortality of h-SLE patients conformed to the normal distribution after BOX-COX conversion and Shapiro–Wilk Test, and then divided the 96 administrative districts into 5 groups according to value of Night light, NO2 concentration, and population density, and assuming that each group was independent of each other, a multi-batch box-plot was used to compare and analyze the distribution shape, dispersion, and central tendency of different groups and different types of data. Correlations between the Night light value, NO2 concentration, and h-SLE patient prevalence were established using pearson correlation analysis and univariate regression analysis. Intergroup differences in Night light value, population density, NO2 concentration, water chemistry type was analyzed by one-way analysis of variance. The medical indicators were counted separately according to different h-SLE patient prevalence level and various indicators in districts of Jiangnan and Jiangbei were analyzed. P values of less than 0.05 were considered to be statistically significant.
Ethical considerations
The study complied with the ethical principles of the Declaration of Helsinki. Written informed consent was obtained from all patients. This study has been approved by the Ethics Committee of the Affiliated Drum Tower Hospital of Nanjing University Medical School.
Results
Environmental exposures might be triggering the development of h-SLE
The group difference analysis in Table1 showed that the two groups of patients in Jiangnan and Jiangbei did not show great differences in the demographic and clinical characteristics. To evaluate the population density of each administrative district and the distribution of h-SLE patients, we analyzed the density of 2231 individuals in 96 administrative districts of Jiangsu Province (Fig. 1A) and significant difference analysis of the h-SLE patient prevalence of population density (person/km2) group indicated that there was no significant difference in h-SLE patient prevalence among different groups (Fig. 1B). The highest prevalence of h-SLE patients appeared in Runzhou, Zhenjiang (26.6 cases per 100,000 people), and the lowest prevalence was in Sihong, Suqian (0.11 cases per 100,000 people), with a ratio of up to 240. Significant regional difference in patient prevalence suggested that environmental exposures might be crucial triggers for lupus. To reveal the relationships of environmental exposures and h-SLE incidence, we conducted a normalized analysis between the cases and the h-SLE patient prevalence in 96 administrative districts of Jiangsu Province (R2 = 0.62, Fig. 1C). 45 of the 96 districts fell outside the 0.2 × 0.2 area, supporting that the onset of lupus may be triggered by exposure to environmental factors. The 15 high-prevalence districts (> 5 cases per 100,000 people) were distributed in two different Zones I and II, among which, 3 ultra-high-prevalence districts (> 10 cases per 100,000 people) distributed in Zone II, Runzhou, Jingkou and Dantu, are all located in Zhenjiang, the south bank of the Yangtze River, where a large number of chemical enterprises are gathered, indicating that the exhaust emission of centralized chemical plants might participate in the development of SLE.
Environmental exposures might be triggering the development of h-SLE. (A) Population density and distribution of h-SLE patients in Jiangsu Province (prepared by WQ in ArcMap 10.2, https://www.esri.com/zh-cn/arcgis/products/arcgis-pro/resources). (B) Significant difference analysis of the h-SLE patient prevalence of population density (person/km2) group. Level 0:230–560; Level 1: 560–700; Level 2: 700–1000; Level 3: 1000–2000; Level 4:2000–20,100. (C) Normalized relationship between the prevalence of h-SLE patients and the number of patient cases in Jiangsu Province, including 10 in the south of the Yangtze River and 5 in the north of the Yangtze River. The prevalence of h-SLE patients conformed to the normal distribution after BOX-COX conversion (λ = 0.053) and Shapiro–Wilk Test (P value: 0.186 > 0.05). Statistical analysis was performed with one-way ANOVA. *P < 0.05, ns not significant.
Relationship of the concentrated discharge of exhaust gas with the prevalence of h-SLE patients
Mostly, air and water pollution in Jiangsu Province were caused by exhaust emission from chemical enterprises. To assess the associations between air pollution and SLE, we analyzed the NO2 concentration distribution in Jiangsu Province, an indicator of air pollution, using OMI satellite atmospheric remote sensing data (Fig. 2A). It existed high h-SLE patient prevalence in areas with high NO2 concentration. The emission of NO2 in the 3 ultra-high-prevalence districts, Runzhou, Jingkou and Dantu, with only 23.2% of Zhenjiang area, accounting for 87.5% of the total city pollution emission. Among the high-prevalence districts in Nanjing, Xuanwu District was located in the industrial zone, and the concentrations of air pollutants including PM10, SO2 and NO2 were the highest; The annual average concentration of NO2 in Xuanwu and Gulou District was higher than the national environmental standard (0.04 mg/m3), and the maximum concentration of NO2 was 0.35 mg/m3 in Gulou, where mainly came from vehicle exhaust emission. Together, our data supported that the development of SLE was partially attributed to the concentrated discharge of exhaust gas from chemical plants or vehicle exhaust emission.
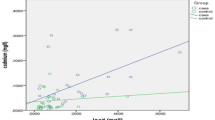
Association between the concentrated discharge of exhaust gas and the development of h-SLE. (A) NO2 concentration distribution in the air of Jiangsu Province in August 2005 (prepared by WQ in ArcMap 10.2, https://www.esri.com/zh-cn/arcgis/products/arcgis-pro/resources). (B) Normalized graph of h-SLE patient prevalence and air NO2 concentration in August 2005 in Jiangsu Province from 1999 to 2009. (C) Significant difference analysis of the prevalence of h-SLE patients in NO2 concentration group. Level 0:250–420; Level 1: 420–585; Level 2: 585–750; Level 3: 750–910; Level 4:910–1075. The prevalence of h-SLE patients conformed to the normal distribution after BOX-COX conversion (λ = 0.053) and Shapiro–Wilk Test (P value: 0.186 > 0.05). Statistical analysis was performed with one-way ANOVA. **P < 0.01, ***P < 0.001.
To further investigate the role of environmental exposures in the development of SLE, we made a normalized relationship chart between the NO2 concentration in the air and the h-SLE patient prevalence (Fig. 2B). Among the 15 high-prevalence districts of h-SLE patients, the air pollution in Jiangbei was lighter, for example, the NO2 normalization coefficients of Haizhou in Lianyungang, Yandu in Yancheng, and Huaian in Huai'an were all less than 0.2, and the NO2 normalization coefficient of Yunlong in Xuzhou was 0.47. In the low-prevalence districts with prevalence < 1, the normalized NO2 concentration in the air was < 0.8, with 6 points falling between 0.6 and 0.8, and significant difference analysis of the h-SLE patient prevalence of NO2 concentration group indicated that there was a threshold for air pollution-induced SLE disease (Fig. 2C), when the degree of air pollution was less than the threshold, the probability of induced SLE disease would be greatly reduced, and for areas with low air pollution, there should be other causes of SLE.
Relations of the concentrated discharge of exhaust water and the prevalence of h-SLE patients
Considering the sources of drinking water might be from polluted surface water or unpolluted groundwater, to evaluate the role of water pollution in h-SLE patient prevalence, we first analyzed the sources of drinking water in h-SLE patient high-prevalence districts (Supplementary Table S3), and found 5 out of 15 in the north of Yangtze River: Haizhou, Yandu, Tinghu, Huaian and Yunlong, were all from polluted surface water. For the other 4 high-prevalence districts in Wuxi City, the source of drinking water has been unified into Tai Lake since the 1970s, the nitrogen and phosphorus pollution in Tai Lake were serious because of the increasingly eutrophication, and the cross-sectional proportions of Class V and inferior Class V water quality were 15% and 85%, respectively, according to the China Hydrological Yearbook, from 1999 to 2009. However, for Yixing and Jiangyin in Wuxi, where the sources of drinking water were from Hengshan Reservoir and Yangtze River, respectively, the patient prevalence (2.2 cases per 100,000 people & 3.1 cases per 100,000 people) was much lower than that of Wuxi City from Tai Lake, suggesting that water pollution might play crucial role in the prevalence of SLE.
Generally, Ca-type and Ca·Mg-type groundwater are defined as unpolluted, and Na-type or high-Na-type groundwater is defined as polluted due to the high content of Na+ in surface water. To further analyze the relations between drinking water sources and the development of h-SLE, we defined different types of water pollution according to the distribution of cations in shallow groundwater in the north of Jiangsu in 2000 (Fig. 3A)26. To normalize the relationship between the patient prevalence and patient cases, we classified drinking water sources in the north of Jiangsu as: surface water, surface water & groundwater, and groundwater (Fig. 3B). Considering that groundwater may be polluted by surface water, Ca·Mg-type groundwater that is not polluted and Na-type groundwater that may be polluted were classified. The prevalence of h-SLE patients was highest in SW (surface water) area, reaching 15.6 cases per 100,000 people; while the prevalence of h-SLE patients was significantly lower in ground water area, of which the lowest was only 0.73 cases per 100,000 people in Ca-type area (Fig. 3C), and there was a significant difference in h-SLE patient prevalence among the five different types of drinking water, especially between SW and Ca-type and Ca·Mg-type (P < 0.001) (Fig. 3D). The number of cases in Na·Ca-type & Na·Mg-type groundwater area was between 2.82 and 1.28 per 100,000, which might be related to a certain degree of pollution to groundwater with the presence of Na. Taken together, these data supported that the development of SLE was probably triggered by the concentrated discharge of exhaust water.
Relationship between the distribution of h-SLE patients and drinking water sources. (A) Distribution of groundwater chemistry types (2000s) and h-SLE patients in northern Jiangsu (prepared by WQ in Microsoft Excel 2019, referring to the cation distribution map of hydrochemical facies for the phreatic aquifer in the 2000s in the paper, https://doi.org/10.1007/s12665-015-4575-4). (B) Normalized relationship between the prevalence of h-SLE patients and the cases of h-SLE in different drinking water sources in northern Jiangsu. (C) Prevalence distribution of h-SLE patients with different chemical drinking water sources in Northern Jiangsu. (D) Significant difference analysis of the prevalence of h-SLE patients in water chemistry type. The prevalence of h-SLE patients conformed to the normal distribution after BOX-COX conversion (λ = 0.053) and Shapiro–Wilk Test (P value: 0.186 > 0.05). Statistical analysis was performed with one-way ANOVA. **P < 0.01, ***P < 0.001.
Correlations of pollution with clinical characteristics and mortality of h-SLE patients
Jiangsu Province is distributed in the two regions of Jiangnan and Jiangbei by Yangtze River with obvious difference in climatic conditions and patient prevalence. We next determined the correlations between different h-SLE patient prevalence in Jiangnan and Jiangbei and their clinical characteristics (Fig. 4, Supplementary Fig. S2, Supplementary Tables S4 and S5). We first made a correlation analysis on clinical characteristics (Supplementary Fig. S3), and found the correlation coefficient between proteinuria and anti-dsDNA antibodies was 0.074 (p = 0.0005), however, the correlation coefficient of proteinuria with pericarditis (r = 0.03, p = 0.1596), fever (r = -0.0043, p = 0.8379), rash (r = 0.034, p = 0.1098); Anti-dsDNA with Arthritis (r = 0.0085, p = 0.6883), fever (r = 0.03, p = 0.1614), rash (r = -0.014, p = 0.5081) and dropsy (r = 0.025, p = 0.9068), respectively, indicating the presence of statistically independent variables. The ratio of patient with proteinuria and pericarditis significantly increased with the increase of patients' prevalence (Fig. 4A,B), indicating that environment pollution might play a role in the development of lupus nephritis, the most common cause of morbidity and mortality for lupus. Further, as the patient prevalence increases, the ratio of patient with anti-double stranded DNA (anti-dsDNA) auto-antibodies, a disease activity indicator, also increased (Fig. 4D), suggesting that environment pollution might affect the disease status of h-SLE patients. However, the overall trends were not consistent among the different manifestations, no significant difference was observed for clinical manifestations including polyserositis, arthritis, fever, rash, dropsy, and so on, this may be affected by differences in individual immunity in the region and the high degree of heterogeneity of SLE, in addition, gender, age, organ involvement, and differences in the sensitivity and specificity of the biomarkers themselves also affected the trend of clinical manifestations27,28,29,30,31. Considering that NOx is the only common substance both in air and water pollution, and regardless of air or drinking water, the area with high NOx concentration has a high percentage of patients with pericarditis and proteinuria, our data gave us a hint that NOx in air and water pollution may be one of the main environmental triggers of SLE.
Proportion of clinical manifestation indicators of h-SLE patients with 5 prevalence levels in Jiangnan and Jiangbei. (A) Proteinuria. (B) Pericarditis. (C) Serositis. (D) Anti-dsDNA antibodies. The patient prevalence (cases per 100,000 people) was divided into 5 levels: level 0: prevalence < 2 (432 cases); level 1: 2 < prevalence < 3(443 cases); level 2: 3 < prevalence < 5(496 cases); level 3: 5 < prevalence < 10(503 cases); level 4: prevalence > 10(357 cases).
To investigate the role of environmental pollution in mortality rate of h-SLE patients, we followed up h-SLE patients mainly in 2010 and 2015, the number of interviews was 1251 cases (survivors:1043, death:208), and the number of missing interviews in the survey was 980, accounting for 44% of the total number of patients. The death rate (24.7%) of level 4 (prevalence > 10 cases/100,000 people) was significantly higher than that of other levels (15.3% & 17.5% 14.5% & 14.2%, Supplementary Table S6), distributed in Runzhou (prevalence: 26.6), Jingkou (prevalence: 20.0), Binhu (prevalence: 13.0), Haizhou (prevalence:10.9) and Dantu (prevalence: 10.1). Among them, Runzhou, Jingkou and Dantu all belong to Zhenjiang City, a place for the concentrated emission of chemical plants, and Binhu, Wuxi, where the source of drinking water is eutrophic Tai Lake, had not only a high prevalence, but also a high mortality rate. Together, our data showed that the mortality rate was positively correlated with the prevalence of h-SLE patients, and pollution not only induced a high h-SLE patient prevalence but also a higher mortality rate.
Discussion
Our data demonstrated that h-SLE patient prevalence was highest in districts with severe air or drinking water pollution. The proportion of patients with pericarditis and proteinuria was positively correlated with the h-SLE patient prevalence, which might be attributed to the concentrated NOx contamination in the air and drinking water. It existed regional difference in the h-SLE patient prevalence, with the ratio of highest to lowest prevalence reaching 240. h-SLE high-prevalence districts also had high mortality rates and the prevalence of lupus nephritis, indicating that the prevalence and characteristics of SLE were related to the living environment, especially the concentrated discharge of air pollution and substandard drinking water.
Here we demonstrated that 6 out of 15 districts with high h-SLE patient prevalence were related to air pollution full of PM10, PM2.5, SO2, NOx, CO, O3, etc. In addition, the h-SLE prevalence was also related to the polluted drinking water sources, for example, drinking water source of four high-prevalence districts in Wuxi City is Tai Lake, in which excessive nitrogen and phosphorus cause serious eutrophication of the water body. The pollutants in drinking water are mainly nitrate nitrogen, ammonia nitrogen, potassium permanganate, phosphorus, COD, chloride, sulfide, etc.32, but the common feature is that the nitrate nitrogen exceeds the standard. NOx is a substance that coexists in air pollution and drinking water source pollution, indicating that whether it is air pollution or water pollution, NOx should be the culprit that induces the prevalence of SLE.
The mechanisms by which NOx participates in the pathogenesis of SLE still largely unknown. Carbon monoxide (NO) in the human body is derived from L-arginine and catalyzed by nitric oxide synthase33. The subtype of nitric oxide synthase-2 may be affected by oxidative stress and cytokines produced after inhalation of air pollutants34, and the acute effect of PM2.5 exposure on FeNO in c-SLE patients suggests that these patients have a higher degree of epithelial-mediated airway inflammation after exposure to fine particles35,36. Increasing evidence suggests that vascular effects such as estrogen increasing uterine arterial blood flow may be mediated by NO37. A multivariate analysis in Taiwan showed that NO2 exposure is positively correlated with the incidence of SLE, and this may be caused by chronic exposure to NO2, which may cause inflammation and increase the level of inflammatory factors such as interleukin-6 (IL-6)38. In vitro experiments showed that exposure under O3 and NO2 in the cultured nasal mucosa increase the production of pro-inflammatory cytokines tumor necrosis factor (TNF-α) and IL-6 by inducing an inflammatory cascade39,40, and TNF-α stimulates the production of other inflammatory molecules including IL-6, IL-6 in turn induces the production of IL-6 producing acute-phase proteins, including CRP and fibrinogen, thereby participating in autoimmune inflammation41,42. Studies have shown that as an active oxidant, peroxynitrite produced by nitric oxide (NO) and superoxide anion (O2·–) is oxidized by proteins and DNA damage (including DNA strand breaks and base modifications) effective triggers can activate the ribozyme poly ADP ribose polymerase (PARP), leading to energy expenditure and apoptosis/necrosis43,44. In chronic inflammatory diseases, the peroxynitrite formed by phagocytes may cause damage to DNA, generates new epitopes, leads to the production of autoantibodies, and participates in the development of autoimmune diseases such as SLE45. In addition, NOx stimulation leads to changes in biochemical epigenetic modifications, which may be a potential mechanism for the onset of SLE46, and NOx-mediated oxidative stress has been shown to inhibit T cell ERK pathway signaling, leading to DNA demethylation, immune gene upregulation, and self-response, and may cause SLE in genetically susceptible individuals47.
Previous studies have suggested that economic development, economic income, and mental stress could be related to the progression of SLE48,49. In order to study the relationship between the h-SLE patient prevalence distribution and the economic development, we conducted a correlation analysis between the total night light observed with night light remote sensing in 2003 and the prevalence of h-SLE patients, night light remote sensing is highly related to economic development, the higher the brightness, the higher the degree of economic development, and the brightness can accurately reflect the economic development of the region and the average living standard of the people. Our data showed that there was no obvious correlation between the prevalence of h-SLE patients and the total night light (Supplementary Fig. S4A) and there was no significant difference in h-SLE patient prevalence among the five groups of Night light value (P > 0.05) (Supplementary Fig. S4B), for example, in Kunshan, Suzhou, where the total night light was the highest, the prevalence of h-SLE patients was very low. The normalized relationship between the amount of night light and h-SLE patient prevalence showed that there was no relationship between them (Supplementary Fig. S4C, R2 = 7 × 10–5). The analysis of the weighted value of night light in 16 districts showed that the night light value was not related to the prevalence of h-SLE patients (Supplementary Fig. S4D). To further confirm the role of economic level and living standard on the prevalence and mortality of h-SLE patients in 96 districts of Jiangsu province, we performed a statistical analysis of the effect of this inclusive difference between rural and urban areas on the prevalence of h-SLE (Supplementary Table S7 and Fig. S5), and found no significant difference in h-SLE patient prevalence between urban and rural areas except for the age (35.99 ± 12.79 & 34.41 ± 12.34, p = 0.0063) (Supplementary Table S7), which was consistent with the finding that there was no significant difference between night light values and h-SLE prevalence. In addition, there was no significant correlation between mortality and night light value and no significant difference in mortality between the groups divided by the night light values (Supplementary Fig. S4E,F). In conclusion, our data suggested that economic level and people's living standard were not the main causes of prevalence and mortality of h-SLE patients in the study area of Jiangsu Province. In our study, Jiangsu region rather than national or even worldwide patient data, hospitalized patients rather than all lupus patients, intercept selection bias of luminous data, and not yet reaching the threshold of triggering the disease of the economic level in Jiangsu province might contribute to the negative data between the prevalence and mortality of h-SLE patients and night light value.
In general, our data evaluated the relations between exposure under air and drinking water pollution and the h-SLE patient prevalence and mortality. We provided evidence that NOx in polluted air and drinking water may be one of the important predispositions of h-SLE, and pollution not only induced a high h-SLE patient prevalence but also a higher mortality rate, especially for patients with renal involvement. Limitations of the study are as followings: Firstly, our longitudinal database only enrolled hospitalized SLE patients in Jiangsu Province, lacking the outpatient samples, differences in the clinical manifestations of the two group patients (hospitalized patients & outpatients), including gender, age, organ involvement, disease activity and medications, might affect the data analysis. Secondly, some patients were diagnosed for the first time while some patients were in the course of the disease, and some inclusion biases might cause deviations in the results. Further limitations stem from a causality link, albeit biological plausible, cannot be proven yet due to lack of control group. Finally, the paper is more of a cross-sectional study from the perspective of geospatial and further longitudinal research is needed to confirm these findings and evaluate potential biological mechanisms.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Justiz Vaillant, A. A., Goyal, A., Bansal, P. & Varacallo, M. In StatPearls (2020).
Pan, Q. et al. Mechanistic insights into environmental and genetic risk factors for systemic lupus erythematosus. Am. J. Transl. Res. 11, 1241–1254 (2019).
Cui, Y., Sheng, Y. & Zhang, X. Genetic susceptibility to SLE: Recent progress from GWAS. J. Autoimmun. 41, 25–33. https://doi.org/10.1016/j.jaut.2013.01.008 (2013).
Qi, Y. Y., Zhou, X. J. & Zhang, H. Autophagy and immunological aberrations in systemic lupus erythematosus. Eur. J. Immunol. 49, 523–533. https://doi.org/10.1002/eji.201847679 (2019).
Geng, L. et al. Comprehensive expression profile of long non-coding RNAs in Peripheral blood mononuclear cells from patients with neuropsychiatric systemic lupus erythematosus. Ann. Transl. Med. 8, 349. https://doi.org/10.21037/atm.2020.03.25 (2020).
Geng, L. et al. MicroRNA-663 induces immune dysregulation by inhibiting TGF-beta1 production in bone marrow-derived mesenchymal stem cells in patients with systemic lupus erythematosus. Cell Mol. Immunol. 16, 260–274. https://doi.org/10.1038/cmi.2018.1 (2019).
Nelson, P., Rylance, P., Roden, D., Trela, M. & Tugnet, N. Viruses as potential pathogenic agents in systemic lupus erythematosus. Lupus 23, 596–605. https://doi.org/10.1177/0961203314531637 (2014).
Illescas-Montes, R., Corona-Castro, C. C., Melguizo-Rodriguez, L., Ruiz, C. & Costela-Ruiz, V. J. Infectious processes and systemic lupus erythematosus. Immunology 158, 153–160. https://doi.org/10.1111/imm.13103 (2019).
Pavlovic, M., Kats, A., Cavallo, M. & Shoenfeld, Y. Clinical and molecular evidence for association of SLE with parvovirus B19. Lupus 19, 783–792. https://doi.org/10.1177/0961203310365715 (2010).
Artinian, B. & Reesal, M. Procainamide-induced SLE and lymphoreticular disorders. Can. Med. Assoc. J. 110, 314 (1974).
Batchelor, J. R. et al. Hydralazine-induced systemic lupus erythematosus: Influence of HLA-DR and sex on susceptibility. Lancet 1, 1107–1109. https://doi.org/10.1016/s0140-6736(80)91554-8 (1980).
Wolf, S. J., Estadt, S. N., Gudjonsson, J. E. & Kahlenberg, J. M. Human and murine evidence for mechanisms driving autoimmune photosensitivity. Front. Immunol. 9, 2430. https://doi.org/10.3389/fimmu.2018.02430 (2018).
Xiang, Z., Yang, Y., Chang, C. & Lu, Q. The epigenetic mechanism for discordance of autoimmunity in monozygotic twins. J. Autoimmun. 83, 43–50. https://doi.org/10.1016/j.jaut.2017.04.003 (2017).
Farhat, S. C. et al. Air pollution in autoimmune rheumatic diseases: A review. Autoimmun. Rev. 11, 14–21. https://doi.org/10.1016/j.autrev.2011.06.008 (2011).
Tang, K. T. et al. Relationship between exposure to air pollutants and development of systemic autoimmune rheumatic diseases: A nationwide population-based case-control study. Ann. Rheum. Dis. 78, 1288–1291. https://doi.org/10.1136/annrheumdis-2019-215230 (2019).
Fernandes, E. C. et al. Exposure to air pollutants and disease activity in juvenile-onset systemic lupus erythematosus patients. Arthritis Care Res. (Hoboken) 67, 1609–1614. https://doi.org/10.1002/acr.22603 (2015).
Alves, A. G. F. et al. Influence of air pollution on airway inflammation and disease activity in childhood-systemic lupus erythematosus. Clin. Rheumatol. 37, 683–690. https://doi.org/10.1007/s10067-017-3893-1 (2018).
Sadeq, M. et al. Drinking water nitrate and prevalence of methemoglobinemia among infants and children aged 1–7 years in Moroccan areas. Int. J. Hyg. Environ. Health 211, 546–554. https://doi.org/10.1016/j.ijheh.2007.09.009 (2008).
Parks, C. G. & De Roos, A. J. Pesticides, chemical and industrial exposures in relation to systemic lupus erythematosus. Lupus 23, 527–536. https://doi.org/10.1177/0961203313511680 (2014).
Lu-Fritts, P. Y. et al. Association of systemic lupus erythematosus with uranium exposure in a community living near a uranium-processing plant: A nested case-control study. Arthritis Rheumatol. 66, 3105–3112. https://doi.org/10.1002/art.38786 (2014).
Kilburn, K. H. & Warshaw, R. H. Prevalence of symptoms of systemic lupus erythematosus (SLE) and of fluorescent antinuclear antibodies associated with chronic exposure to trichloroethylene and other chemicals in well water. Environ. Res. 57, 1–9. https://doi.org/10.1016/s0013-9351(05)80014-3 (1992).
Somers, E. C. & Richardson, B. C. Environmental exposures, epigenetic changes and the risk of lupus. Lupus 23, 568–576. https://doi.org/10.1177/0961203313499419 (2014).
Strickland, F. M., Li, Y., Johnson, K., Sun, Z. & Richardson, B. C. CD4(+) T cells epigenetically modified by oxidative stress cause lupus-like autoimmunity in mice. J. Autoimmun. 62, 75–80. https://doi.org/10.1016/j.jaut.2015.06.004 (2015).
Li, Y., Gorelik, G., Strickland, F. M. & Richardson, B. C. Oxidative stress, T cell DNA methylation, and lupus. Arthritis Rheumatol. 66, 1574–1582. https://doi.org/10.1002/art.38427 (2014).
Sunahori, K. et al. The catalytic subunit of protein phosphatase 2A (PP2Ac) promotes DNA hypomethylation by suppressing the phosphorylated mitogen-activated protein kinase/extracellular signal-regulated kinase (ERK) kinase (MEK)/phosphorylated ERK/DNMT1 protein pathway in T-cells from controls and systemic lupus erythematosus patients. J. Biol. Chem. 288, 21936–21944. https://doi.org/10.1074/jbc.M113.467266 (2013).
Shi, X. et al. Characterization of the regional groundwater quality evolution in the North Plain of Jiangsu Province, China. Environ. Earth Sci. 74, 5587–5604 (2015).
Mok, C. C. Biomarkers for lupus nephritis: A critical appraisal. J. Biomed. Biotechnol. 2010, 638413. https://doi.org/10.1155/2010/638413 (2010).
Soliman, S. & Mohan, C. Lupus nephritis biomarkers. Clin. Immunol. 185, 10–20. https://doi.org/10.1016/j.clim.2016.08.001 (2017).
Ryu, S., Fu, W. & Petri, M. A. Associates and predictors of pleurisy or pericarditis in SLE. Lupus Sci. Med. 4, e000221. https://doi.org/10.1136/lupus-2017-000221 (2017).
Ramirez Sepulveda, J. I. et al. Sex differences in clinical presentation of systemic lupus erythematosus. Biol. Sex Differ. 10, 60. https://doi.org/10.1186/s13293-019-0274-2 (2019).
Ikushima, H. et al. Severe pleuritis and pericarditis associated with very-late-onset systemic lupus erythematosus. J Gen Fam Med 19, 53–56. https://doi.org/10.1002/jgf2.157 (2018).
Hryhorenko, L., Shchudro, S., Shevchenko, A., Rublevska, N. & Zaitsev, V. Prevalence of diseases among adolescent population in dnepropetrovsk region (ukraine), correlated with drinking water quality deterioration. Georgian Med. News 11, 91–96 (2017).
Sawano, M. Demonstration and quantification of the redistribution and oxidation of carbon monoxide in the human body by tracer analysis. Med. Gas Res. 6, 59–63. https://doi.org/10.4103/2045-9912.184598 (2016).
Zhu, X. M. et al. PM2.5 induces autophagy-mediated cell death via NOS2 signaling in human bronchial epithelium cells. Int. J. Biol. Sci. 14, 557–564. https://doi.org/10.7150/ijbs.24546 (2018).
Shi, J. et al. Association between fine particulate matter chemical constituents and airway inflammation: A panel study among healthy adults in China. Environ. Res. 150, 264–268. https://doi.org/10.1016/j.envres.2016.06.022 (2016).
Deerojanawong, J., Leartphichalak, P., Chanakul, A., Sritippayawan, S. & Samransamruajkit, R. Exhaled nitric oxide, pulmonary function, and disease activity in children with systemic lupus erythematosus. Pediatr. Pulmonol. 52, 1335–1339. https://doi.org/10.1002/ppul.23742 (2017).
Ramsay, B., Johnson, M. R., Leone, A. M. & Steer, P. J. The effect of exogenous oestrogen on nitric oxide production in women: A placebo controlled crossover study. Br. J. Obstet. Gynaecol. 102, 417–419. https://doi.org/10.1111/j.1471-0528.1995.tb11296.x (1995).
Jung, C. R., Chung, W. T., Chen, W. T., Lee, R. Y. & Hwang, B. F. Long-term exposure to traffic-related air pollution and systemic lupus erythematosus in Taiwan: A cohort study. Sci. Total Environ. 668, 342–349. https://doi.org/10.1016/j.scitotenv.2019.03.018 (2019).
Panasevich, S. et al. Interaction between air pollution exposure and genes in relation to levels of inflammatory markers and risk of myocardial infarction. BMJ Open 3, e003058. https://doi.org/10.1136/bmjopen-2013-003058 (2013).
Hu, X. et al. Inflammatory and oxidative stress responses of healthy adults to changes in personal air pollutant exposure. Environ Pollut 263, 114503. https://doi.org/10.1016/j.envpol.2020.114503 (2020).
Panasevich, S. et al. Associations of long- and short-term air pollution exposure with markers of inflammation and coagulation in a population sample. Occup. Environ. Med. 66, 747–753. https://doi.org/10.1136/oem.2008.043471 (2009).
Geng, L. et al. Reduced Let-7f in bone marrow-derived mesenchymal stem cells triggers Treg/Th17 imbalance in patients with systemic lupus erythematosus. Front. Immunol. 11, 233. https://doi.org/10.3389/fimmu.2020.00233 (2020).
Sawa, T., Akaike, T. & Maeda, H. Tyrosine nitration by peroxynitrite formed from nitric oxide and superoxide generated by xanthine oxidase. J. Biol. Chem. 275, 32467–32474. https://doi.org/10.1074/jbc.M910169199 (2000).
Dantzer, F. et al. Poly(ADP-ribose) polymerase-1 activation during DNA damage and repair. Methods Enzymol. 409, 493–510. https://doi.org/10.1016/S0076-6879(05)09029-4 (2006).
Ahmad, R., Rasheed, Z. & Ahsan, H. Biochemical and cellular toxicology of peroxynitrite: Implications in cell death and autoimmune phenomenon. Immunopharmacol. Immunotoxicol. 31, 388–396. https://doi.org/10.1080/08923970802709197 (2009).
Iriyoda, T. M. V. et al. Reduction of nitric oxide and DNA/RNA oxidation products are associated with active disease in systemic lupus erythematosus patients. Lupus 26, 1106–1111. https://doi.org/10.1177/0961203317692436 (2017).
Gorelik, G. & Richardson, B. Aberrant T cell ERK pathway signaling and chromatin structure in lupus. Autoimmun. Rev. 8, 196–198. https://doi.org/10.1016/j.autrev.2008.07.043 (2009).
Teixeira, R. C. A., Borba Neto, E. F., Christopoulos, G. B. & Sato, E. I. The influence of income and formal education on damage in brazilian patients with systemic lupus erythematosus. J. Clin. Rheumatol. 23, 246–251. https://doi.org/10.1097/RHU.0000000000000541 (2017).
Roussou, E., Iacovou, C., Weerakoon, A. & Ahmed, K. Stress as a trigger of disease flares in SLE. Rheumatol. Int. 33, 1367–1370. https://doi.org/10.1007/s00296-011-2292-1 (2013).
Acknowledgements
The authors thank all those members of Jiangsu Lupus Collaborative Group who followed up the patients and helped data collection. They acknowledge the Cinkate Corp for helping build and manage their lupus database. The work was supported by National Key R&D Program of China (2020YFA0710800), the Major International (Regional) Joint Research Project (No.81720108020), National Natural Science Foundation of China (No. 81871283, 81501347, 81373198, 81471533, 81370730, and 81273304) and Nanjing Medical Science and technique Development Foundation (JQX20004).
Author information
Authors and Affiliations
Contributions
J.C., W.Q. and Li.S. collected data and analyzed results, Js.C. and L.G. wrote the manuscript. W.K., F.W., W.P., L.L., M.W., F.D., H.H., X.D., H.W., Y.Z., X.Q., M.W., J.W., J.Tao., J.Tan., Z.D., M.Z., J.Li., J.Liang and X.F. acquired clinical data. L.G. and L.S. designed the study and supervised the project. All authors made substantial intellectual contributions to conception of the work, the interpretation of data and approval of the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, J., Qu, W., Sun, L. et al. The relationship of polluted air and drinking water sources with the prevalence of systemic lupus erythematosus: a provincial population-based study. Sci Rep 11, 18591 (2021). https://doi.org/10.1038/s41598-021-98111-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-98111-8
- Springer Nature Limited
This article is cited by
-
Air pollution exposure and auto-inflammatory and autoimmune diseases of the musculoskeletal system: a review of epidemiologic and mechanistic evidence
Environmental Geochemistry and Health (2023)