Abstract
We aimed to compare the reliability of bone scintigraphy (BS) and fluorine-18-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET)—derived parameters in the detection of active arthritis in 28-joint areas and evaluate the reliability of joint counts between BS and clinical assessment in patients with rheumatoid arthritis (RA). We enrolled 106 patients (67 in the development group and 39 in the validation groups) with active RA who underwent BS, 18F-FDG PET/computed tomography (CT), and clinical evaluation of disease activity. We compared the results of BS-derived joint assessment with those of PET-derived and clinical joint assessments. Subsequently we developed a disease activity score (DAS) using BS-positive joints and validated it in an independent group. The number of BS-positive joints in 28-joint areas significantly correlated with the swollen /tender joint counts (SJC/TJC) and PET-derived joint counts. A BS uptake score of 2 (strong positive) was significantly more sensitive compared with a BS uptake score of 1 (weak positive) in detecting a PET-positive joint among the 28-joints. After conducting multivariate analyses including erythrocyte sediment rate (ESR) and patient global assessment (PGA) in addition to BS-derived parameters, BS/DAS was obtained as follows: 0.056 × number of BS-positive joints in 28 joints + 0.012 × ESR + 0.030 × PGA. A significant correlation between BS/DAS and DAS28-ESR was confirmed in the validation group. Strong positive uptake of BS is sensitive and reproducible for the detection of active joints, and can complement the clinical assessment of disease activity in RA.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory joint disorder characterized by the synovial infiltration of active immune cells, which causes the destruction of cartilage, bone, and joint structures1. Joint counts performed by experienced physicians are considered crucial in the quantitative assessment of synovitis, which was included in the disease activity score (DAS) 28 for the measurement of RA activity2. However, joint counts are limited by an inherent lack of objectivity related to both operator’s factors and patient’s factors3,4, thereby increasing the need for more sensitive and reproducible tools to detect synovitis.
Although imaging modalities such as ultrasound (US) and magnetic resonance imaging (MRI) are more sensitive than clinical assessment for detecting joint inflammation5,6,7, it is difficult to assess systemic joint status in patients with RA with these tools8,9,10,11. Another limitation is the time-consuming nature of these imaging procedures. Recently, fluorine-18-fluorodeoxyglucose (FDG) positron emission tomography (PET)/computed tomography (CT) imaging provided important insights that helped in evaluating disease activity in patients with RA. The FDG PET/CT-derived joint count assessment is a highly reproducible and sensitive tool, and complements the clinical evaluations12. However, FDG PET/CT examinations have certain limitations including high levels of radiation exposure, use of expensive core facility, and high costs13,14,15.
Bone scintigraphy (BS), which has long been used in clinical settings for the assessment of inflamed joint distribution, has several advantages for evaluating systemic joints over US, MRI, and FDG PET/CT. BS provides whole-body joint imaging with much less radiation exposure compared with FDG PET/CT13 and is a potential tool for quantitative assessment of disease activity in a more affordable and safer way. However, no study has validated the usefulness of BS in the measurement of RA disease activity.
In this study, we aimed to validate the BS-derived quantitative parameters for RA disease activity by comparing BS-derived joint counts with PET-derived joint counts performed in 28-joints. First, BS-derived joint assessment was compared with PET-derived and clinical joint assessments. Subsequently, DAS was developed using BS-positive joints and validated it in an independent group.
Patients and methods
Patients and study design
We enrolled 106 patients who had active joints and underwent BS evaluation at Kyungpook National University Hospital from December 2010 to February 2018 in our study. We diagnosed all patients with RA according to the American College of Rheumatology/European League Against Rheumatism criteria of 201016. This study comprised two groups: a development (n = 67) group, in which DAS was derived by both BS and FDG PET/CT, and a validation group (n = 39), in which the DAS was applied. At the time of BS evaluation, we assessed the clinical disease activity including swollen joint count (SJC), tender joint count (TJC), patient global assessment (PGA), erythrocyte sedimentation (ESR), and C-reactive protein (CRP). The clinical assessments of positive joint counts were examined in each patient by the rheumatologists (J.S.E., J.W.K., and N.R.K.) and a BS image analysis was performed by two nuclear medicine physicians (C.M.H. and I.C.). Nuclear medicine physicians were unaware of the clinical positive joint counts and disease activity of the patients. This study was approved by the Institutional Review Board (IRB) and Ethics Committee at Kyungpook National University Hospital (approval number 2018-05-032). The requirement for informed consent was waived by the IRB since the study involved a minimum risk to the enrolled patients and no identifiable information was used. All methods were performed in accordance with the relevant guidelines and regulations.
FDG PET/CT acquisition protocol and image analysis
A previous study demonstrated the FDG-PET/CT acquisition protocol12. All patients fasted more than 6 h, and the blood glucose levels of each patient before the FDG administration was < 150 mg/dL. PET/CT images were obtained from the skull vertex to the feet with the patient in supine position using a Reveal HiREZ 6-slice CT apparatus (CTI Molecular Imaging, Knoxville, TN, USA) 1 h after the intravenous injection of FDG (~ 5 MBq/kg body weight). First, a low-dose CT scan without contrast enhancement was obtained for attenuation correction, and all images were reconstructed using a 3.75-mm slice thickness at 2.5-mm increments. Then a three-dimensional-mode PET scan with a maximum spatial resolution of 6.5 mm was performed for 3 min per bed position. The PET images were reconstructed with a 128 × 128 matrix. When FDG uptake in the joint synovium was higher than normal regional tracer accumulation, the joints were considered positive for active arthritis. PET positive and negative joints were defined as scores 1 and 0, respectively. The volume of interest (VOI) for a PET-positive joint was placed on a joint synovium in PET images, and an iso-contour VOI including all voxels > 42% of the maximum was created; subsequently, the SUVmax value was automatically calculated. The SUVmax was obtained using following formula: maximum activity in the region of interest (MBq/mL) divided by injected dose (MBp)/body weight (g). PET28 was defined as the number of PET-positive joints among the 28-joints. Two experienced nuclear medicine physicians interpreted the PET/CT images and the interpretation of the PET/CT images was repeated 2 months later (by a nuclear medicine physician) or independently (two nuclear medicine physicians).
We previously developed a novel PET/DAS formula using PET/CT after conducting multivariate analyses including ESR and PGA in addition to PET-derived parameters12. PET/DAS was derived as 0.063 × PET28 + 0.011 × ESR + 0.030 × PGA.
BS acquisition protocol and image analysis
BS images were obtained 3–5 h after the injection of 740 MBq (20 mCi) of Tc-99m hydroxymethylene diphosphonate (HDP). A dual-headed gamma camera equipped with a high-resolution collimator (Infinia, GE, Milwaukee, WI, USA) was used to obtain anterior and posterior whole-body images, along with the static images of hands. The regions of interest (ROIs) were drawn around the 28-joints and a semi-quantitative analysis was performed in each joint and the results were compared with the reference backgrounds. For large joints including wrist joints and small joints, the left side of skull in the whole body image and right radius in the static image of the hand were used as a reference background, respectively. Then, the 28-joints of each patient were scored as 0–2 (0: negative, 1: weak positive, 2: strong positive; Supplementary Fig. S1). The visual interpretation of BS images was performed by two nuclear medicine physicians (C.M.H. and I.C.). The interpretation of the BS images was repeated 2 months later (C.M.H.) or independently (C.M.H. and I.C.). BSS28 was defined as the number of BS-positive joints among the 28-joints.
Statistical analysis
The baseline clinical data were expressed as means ± SD for continuous variables or as numbers and percentages for categorical variables. To compare BS and PET/CT in terms of the detection of active joints, the significant differences between variables were calculated using the chi-square test and Mann-Whitney test. The correlations between the BS-derived parameters and other disease activity measures were calculated using the Pearson’s correlation test, with Bonferroni’s correction. The intra-observer (the nuclear medicine physician, 2 month intervals) and inter-observer (between the two nuclear medicine physicians or between a nuclear medicine physician and rheumatologists) in the 28-joints counts were calculated using the Cohen κ-test and intraclass correlation coefficient (ICC). A kappa value of 0–0.20 was considered poor, 0.21–0.40 as fair, 0.41–0.60 as moderate, 0.61–0.80 as good, and 0.81–1.00 as excellent17,18. ICCs between the BSS28 and PET28, TJC28 in the development group were calculated using a two-way mixed-effects model and the Bland–Altman approach19.
For the development of DAS using BS, univariate and multivariate analyses were conducted using the linear regression model to evaluate the association among clinical factors, including BS-derived parameters, and disease activity measures in patients with RA. After the generation of BS/DAS, we calculated it for each patient in the validation group (n = 39). Pearson’s correlation test was utilized to compare the correlation between BS/DAS and DAS28-ESR. P values < 0.05 were considered significant. All statistical analyses were performed using SPSS version 19 software (IBM, Chicago, IL, USA) and GraphPad Prism version 5 (GraphPad, San Diego, CA, USA) was used to generate the graphics.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board at confirmed Kyungpook National University Hospital (2018-05-032).
Results
Baseline characteristics in the development and validation groups
We enrolled 86 patients with active RA in the development group (n = 67) and validation group (n = 39) who underwent BS, disease activity evaluation, and/or FDG-PET/CT at the same time. The mean ages of the development and validation groups at the time of disease evaluation were 68 and 67 years, respectively. The proportion of women was similar between the two groups. Additionally, the mean DAS28-ESR of the development and validation groups were 6.81 and 6.43, respectively, with all patients in both groups showing moderate to high disease activity. In both groups, 53 patients (79.1%) and 28 patients (71.8%) were naïve to disease-modifying antirheumatic drugs (DMARDs) (Table 1).
Correlations between BS-derived parameters and other disease activity measures in the development group
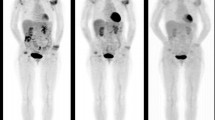
To compare the reliability of BS and PET/CT in the detection of active joints, the individual affected joints examined by BS, in terms of cumulative frequencies and percentages of involvement (Fig. 1A, B) of the individual joint, were expressed based on the positive joint counts and SUVmax on PET/CT (Fig. 1C). A BS uptake score of 2 was significantly more sensitive compared with a BS uptake score of 1 in detecting a PET-positive joint among the 28-joints (Fig. 1A, B). Thus we used the BS uptake score of 2 as a criterion for diagnosing a BS positive joint. At the time of BS and PET/CT evaluation, the clinical disease activity was assessed using SJC28, TJC28 and DAS28-ESR. To investigate the correlation between BSS28 and clinical disease activity, the BSS28 was compared with the clinical parameters including TJC28, SJC28 and DAS28-ESR. The BSS28 was significantly correlated with TJC28 (r = 0.483, p < 0.001), SJC 28 (r = 0.409, p = 0.001), and DAS28-ESR (r = 0.457, p < 0.001) (Fig. 2A–C). The BSS28 was also significantly correlated with PET28 (r = 0.643, p < 0.001) (Fig. 2D).
Comparison of positron emission tomography (PET) and bone scintigraphy (BS) in the detection of active joints. The frequencies (A), percentages (B) and the mean SUVmax (C) of PET positive joints were expressed according to BS scores in the affected individual joints among the 67 patients who underwent PET and BS. A total of 134 frequencies were observed for each joint. In total, 12 frequencies in knees were excluded in the analysis because those indicate the status of total knee replacement arthroplasty. When FDG uptake in the joint synovium was higher than normal regional tracer accumulation, the joints were considered positive for active arthritis. PET positive and negative joints were defined as scores 1 and 0, respectively. The 28-joints of each patient in BS were scored as 0–2 (0: negative, 1: weak positive, 2: strong positive). The BS uptake score of 2 was used as a criterion for diagnosing a BS positive joint. MCP, metacarpophalangeal joint; PIP, proximal interphalangeal joint; SUV, standardized uptake values. **p < 0.005; *p < 0.05
Correlation between positive findings in the joints assessed by PET, BS, and clinical assessment. The number of bone scintigraphy positive joints in 28-joints (BSS28) was significantly correlated with the tender joint counts in 28 joints (TJC28) (r = 0.483, p < 0.001) (A), the swollen joint counts in 28 joints (SJC28) (r = 0.409, p = 0.001) (B), DAS28-ESR (r = 0.457, p < 0.001) (C), and the number of PET-positive joints in 28 joints (PET28) (r = 0.643, p < 0.001) (D). Each symbol represents an individual data point, and the dotted lines represent the 95% confidence interval. The correlation coefficients and p values were calculated using the Pearson’s correlation test. ESR, erythrocyte sedimentation rate.
Reliability of joint counts between BSS28 and other disease activity measures in the development group
Kappa values between BS results and clinical assessments of the individual joints ranged from 0.033 to 0.457. However, these values indicated constant fair to moderate agreement, except for the knee and shoulder joints. The reliability values between BSS28 and SJC28/TJC28 assessed by ICCs at the patient level in 28-joints were 0.585 (95% confidence interval: 0.324–0.745) and 0.646 (0.424–0.783), respectively (Table 2). The reliability between BS and PET/CT for joint counts ranged from 0.194 to 0.703 by kappa values at the individual joint and 0.782 (0.646–0.866) by ICCs at the patient level in 28-joints, respectively. These reliability values were higher than those between BS results and clinical assessments (Table 2).
The level of reliability of the BSS28 in relation to the PET28 and TJC28 was further illustrated by the Bland–Altman plots. The mean differences between the BSS28 and PET28/TJC 28 were 0.46 and − 0.40, respectively. The majority of plots (62 of 67 (92.5%) and 64 of 67 (95.5%), respectively) were within the upper and lower limits of 2 SD (Fig. 3A, B).
Bland–Altman plot showing the interobserver reliability of assessment of the number of bone scintigraphy-positive joints in 28 joints (BSS28) in relation to PET positive joint count in 28-joints (PET28) (A) and the tender joint count in 28-joints (TJC28) (B). Mean between BSS28 and PET28 = average of the joint count as determined by the BSS28 and the joint count as determined by the TJC28. The mean differences between the BSS28 and PET28, and the BSS28 and TJC 28 were 0.46 and − 0.40, respectively, and the majority of plots (62 of 67 [92.5%] and 64 of 67 [95.5], respectively) were within the upper and lower limits of 2 SD (lines with asterisks).
When the intra-observer reliability of the nuclear medicine physician was evaluated, the kappa values at the individual joint showed moderate to excellent agreement, and the ICC values at the patient level showed an excellent reliability (0.938, 0.840–0.976). Furthermore, the ICC values of the inter-observer results (between two nuclear medicine physicians) were good in the 28-joints counts (0.830, 0.560–0.935) (Supplementary Table S1).
Development of the DAS using BS (BS/DAS)
For the development of BS/DAS, a linear regression model was used to analyze the BSS28 and DAS28-ESR. After conducting multivariate analyses including ESR or CRP, and PGA in addition to BSS28, the values of ESR or CRP, PGA, and BSS28 were independently associated with the DAS28-ESR/CRP (Supplementary Table S2). Using these parameters, the BS/DAS was derived based on the regression coefficients as the following formula:
Validation of the BS/DAS in the independent group
In the validation group, 28 patients were naïve to DMARDs, with 11 showing inadequate responses. Disease activities such as DAS28-ESR/CRP in the validation group were not significantly different from the development group (Table 1). The BS/DAS in the validation group were significantly correlated with DAS28-ESR (r = 0.806, p < 0.001) (Fig. 4). BS/DAS were also significantly correlated with the DAS28-CRP, TJC28, and SJC28 (Supplementary Table S3).
The correlation between BS/DAS and DAS28-ESR. BS/DAS (n = 39) was significantly correlated with DAS28-ESR (r = 0.806, p < 0.001). The correlation coefficient and p-value were derived by conducting the Pearson’s correlation test. BS bone scintigraphy, DAS disease activity score, ESR erythrocyte sedimentation rate.
Discussion
This study had two main results. First, the BS-derived joint assessment significantly correlated with clinical and PET/CT-derived joint counts, and its reliability was good for both clinical and PET/CT-derived findings. Second, we developed the disease activity formula, the BS/DAS, which is composed of the BSS28, levels of ESR, and the PGA. Additionally, the formula was confirmed in a validation group.
In our previous study, FDG-PET/CT could serve as a sensitive and reproducible method for assessing disease activity in patients with RA12. Although the radiation dose is reduced with more advanced scanners, an increase in radiation exposure is one of a major safety concern in this procedure15. In Korea, the average radiation doses of PET/CT and BS are 12.2 and 4.2 mSv, respectively, as estimated by a national survey14,15. Furthermore, the cost of conducting a PET/CT examination is high and this procedure required the use of accompanying facilities including the tracer production, so PET/CT study may not be possible in small to moderate sized facilities.
Therefore, the use of FDG PET/CT for evaluating disease activity in a routine clinical practice remains challenging. On the contrary, BS imaging for active joint count has much less radiation exposure than PET/CT imaging, while it provides similar reliable results in patients with RA. The correlation coefficient of a BS/DAS formula for representing DAS28-ESR in each patient in the validation group in this study is comparable to that of PET/DAS formula in a previous study (r = 0.806, p < 0.001 vs r = 0.843, p < 0.001, respectively)12.
BS is a highly sensitive diagnostic technique of nuclear imaging that uses a radiotracer to evaluate the distribution of active bone formation20. Solid tumors with high affinity for bone, metabolic bone diseases, and joint diseases such as chronic inflammatory arthritis and osteoarthritis (OA) are indications for BS evaluation20. BS has been used for the differential diagnosis of RA, OA, spondyloarthritis, and unclassified arthritis in the field of rheumatology21,22,23. Additionally our results show that joint count by BS evaluation is a reproducible method for assessing bone changes in the affected synovitis, with good reliability between observers, thus BS can be used for measuring disease activity in patients with RA. Therefore, this tool may help physicians worldwide who take care of RA patients, but without well-trained expertise or expensive facilities such as PET/CT. Moreover, as an objective tool for identifying arthritis in our study, BS may be applied for the differential diagnostic process of unclassified arthritis, which is important to estimate affected joints and their location. However, follow-up study is needed to clarify whether changes of BS uptake in patient with RA improve or remain after treatment.
Although previous studies on disease activity assessment using BS in patients with RA were limited, two reports showed a significant correlation between the regional uptake for large joints on BS and disease activity24,25. These studies did not evaluate 28-joints including small joints and did not compare the BS values with DAS28. According to the analysis of the affected joint in a large cohort with RA patients, tender joints were frequently observed in large joints, while swollen joints were frequently observed in the small joints of the hands26. Thus, evaluating large joints alone is not sufficient to represent the accurate disease activity. Furthermore, the reliability of BS for clinical assessment of large joints such as knee and shoulder joints was relatively lower than that of other joints in our study. Therefore, joint count based on the BS values of 28-joint areas including both small and large joints should provide a more objective parameter for disease activity assessment. Because it is important to determine the cut off value for BS score to assess for synovitis in patients with RA, we compared affected individual joints between BS scores and PET/CT examination. A BS uptake score of 2 was significantly more reliable than a BS uptake score of 1 in detecting PET-positive joint at 28 joints. Thus we used the BS uptake score of 2 as a criterion for BS positive joint.
Despite the crucial role of RA disease activity measurement in detecting synovitis, clinical assessments of joint counts are not routinely performed in clinics because reliability of joint count assessments, considering both the intra-observer and inter-observer variabilities, needs to be explored further27. The intra-observer reliability of ICCs for the clinical assessment of joint counts by healthcare professionals ranged from 0.47 to 0.98 in both TJC and SJC28, whereas the reliability of kappa value at the joint level varied from fair to good in SJC29, thereby suggesting the inconsistent joint assessment in clinical practice. Furthermore, the range of inter-observer reliability assessed with the ICCs and the kappa value was dependent on the variation among study samples in finding a positive joint count (from 0.29 to 0.98, from poor to excellent, respectively)30,31. By contrast, joint counts by BS evaluation are a reproducible method for assessing synovitis, with excellent inter-observer and intra-observer reliability.
Surprisingly, when observing the ICC values of reliability between BS and PET/CT findings in 28-joints, the ICC between BSS28 and PET28 was 0.782 (0.646–0.866). Furthermore, the ICC values between BS28 and TJC28 were comparable to those between PET28 and TJC28 (0.646 and 0.728, respectively)12, implicating that the BSS28 and clinical assessments that were performed by experienced clinicians had a good reliability. We also developed a novel BS/DAS formula derived from the results of BS assessment alone, without using the results of joint assessment performed by experienced clinicians. This formula was confirmed in an independent validation group of RA patients. The BS/DAS, which may overcome the variability of clinical evaluation by joint assessors with diverse backgrounds, can complement the use of the DAS28-ESR and may provide similar results compared with more advanced modality such as PET/CT for evaluation of disease activity.
It was reported that US and MRI have the excellent capability in the evaluation of inflammatory arthritis, and their scores significantly correlated with DAS 28, proving their utility in the diagnosis and monitoring of patients with RA8,32,33. One study demonstrated that there was a powerful linear relationship between scores from MRI and PET/CT in the evaluation of arthritis, despite the fact that these modalities have different ways to identify synovitis7. Because FDG-PET/CT is considered as an excellent tool for evaluating inflammatory reaction in the joints, we assessed the utility of the BS in patients with RA. Given that the use of PET/CT in daily practice is challenging, this work can be a initial step (transversal study) before a clinical trial using BS to monitor the disease activity in patients with RA. Although US is easily accessible and has advantage of real-time examination and MRI has advantage of visualizing intra-osseous abnormality, they are time-consuming and have definite limitations in the evaluation of systemic joints33. On the contrary, PET/CT and BS images show the involvement of the whole joint pattern for synovial inflammation12,20. Especially, given the relative low cost and widespread availability of BS in an era of more advanced imaging tools, our findings could provide new insight into the BS evaluation in patients with RA.
There are two limitations in this study. First, BS reflects bone remodeling and uptakes in knee joints can be observed in patients with knee OA21, regardless of RA disease activity. Second, patients were enrolled at a single center, thus multicenter studies of BS validation are warranted to determine whether our findings are generalizable.
Conclusion
In conclusion, BS is a sensitive and reproducible method for the detection of active joints, and can complement the clinical assessment of disease activity in RA. Despite the availability of more advanced imaging modality such as PET/CT, considering their costs, and the radiation and sensitivity for evaluating active joints, BS may still be comparable to this advanced imaging method in terms of assessing disease activity in patients with RA. In the future, the incorporation of deep learning from BS images into computer-aided evaluation is promising for the assessment of disease activity in patient with RA.
Abbreviations
- RA:
-
Rheumatoid arthritis
- DAS:
-
Disease activity score
- US:
-
Ultrasound
- MRI:
-
Magnetic resonance imaging
- FDG:
-
Fluorodeoxyglucose
- PET:
-
Positron emission tomography
- CT:
-
Computed tomography
- BS:
-
Bone scintigraphy
- SJC:
-
Swollen joint count
- TJC:
-
Tender joint count
- PGA:
-
Patient global assessment
- ESR:
-
Erythrocyte sedimentation
- CRP:
-
C-reactive protein
- VOI:
-
Volume of interest
- HDP:
-
Hydroxymethylene diphosphonate
- ROI:
-
Regions of interest
- ICC:
-
Intraclass correlation coefficient
- DMARDs:
-
Disease-modifying antirheumatic drugs
- OA:
-
osteoarthritis
References
Harris, E. D. Jr. Rheumatoid arthritis. Pathophysiology and implications for therapy. N. Engl. J. Med. 322, 1277–89 (1990).
Prevoo, M. L. et al. Validity and reliability of joint indices. A longitudinal study in patients with recent onset rheumatoid arthritis. Br. J. Rheumatol. 32, 589–94 (1993).
Sokka, T. How should rheumatoid arthritis disease activity be measured today and in the future in clinical care?. Rheum. Dis. Clin. N. Am. 36, 243–57 (2010).
Tawakol, A., Unizony, S., Osborne, M. T., Massarotti, E. & Giles, J. T. Evolving use of molecular imaging in research and in practice. Arthritis Rheumatol. 71, 1207–10 (2019).
Mathew, A. J., Danda, D. & Conaghan, P. G. MRI and ultrasound in rheumatoid arthritis. Curr. Opin. Rheumatol. 28, 323–9 (2016).
Schmidt, W. A. et al. Colour Doppler ultrasonography to detect pannus in knee joint synovitis. Clin. Exp. Rheumatol. 18, 439–44 (2000).
Palmer, W. E. et al. Quantification of inflammation in the wrist with gadolinium-enhanced MR imaging and PET with 2-[F-18]-fluoro-2-deoxy-D-glucose. Radiology. 196, 647–55 (1995).
Naredo, E. et al. Assessment of inflammatory activity in rheumatoid arthritis: A comparative study of clinical evaluation with grey scale and power Doppler ultrasonography. Ann. Rheum. Dis. 64, 375–81 (2005).
Salaffi, F. et al. Inter-observer agreement of standard joint counts in early rheumatoid arthritis: A comparison with grey scale ultrasonography—A preliminary study. Rheumatology (Oxford). 47, 54–8 (2008).
Boer, A. C., Boeters, D. M. & van der Helm-van Mil, A. H. M. The use of MRI-detected synovitis to determine the number of involved joints for the 2010 ACR/EULAR classification criteria for Rheumatoid Arthritis—Is it of additional benefit?. Ann. Rheum. Dis. 77, 1125–9 (2018).
Fujimori, M. et al. Composite assessment of power Doppler ultrasonography and MRI in rheumatoid arthritis: a pilot study of predictive value in radiographic progression after one year. Br. J. Radiol. 91, 20170748 (2018).
Lee, S. J. et al. Development and validation of an (18) F-fluorodeoxyglucose-positron emission tomography with computed tomography-based tool for the evaluation of joint counts and disease activity in patients with rheumatoid arthritis. Arthritis Rheumatol. 71, 1232–40 (2019).
Valentin, J. Radiation dose to patients from radiopharmaceuticals (addendum 2 to ICRP publication 53). Ann. ICRP. 28, 1–126 (1998).
Valentin, J. Managing patient dose in multi-detector computed tomography(MDCT). ICRP Publication 102. Ann ICRP 37, 1–79, iii (2007).
Kwon, H. W. & Kim, J. P. Radiation dose from whole-body F-18 fluorodeoxyglucose positron emission tomography/computed tomography: Nationwide Survey in Korea. J. Korean Med. Sci. 31(Suppl 1), S69-74 (2016).
Aletaha, D. et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 62, 2569–81 (2010).
Landis, J. R. & Koch, G. G. The measurement of observer agreement for categorical data. Biometrics. 33, 159–74 (1977).
Shrout, P. E. & Fleiss, J. L. Intraclass correlations: uses in assessing rater reliability. Psychol. Bull. 86, 420–8 (1979).
Francq, B. G. & Govaerts, B. How to regress and predict in a Bland–Altman plot? Review and contribution based on tolerance intervals and correlated-errors-in-variables models. Stat. Med. 35, 2328–58 (2016).
Van den Wyngaert, T. et al. The EANM practice guidelines for bone scintigraphy. Eur. J. Nucl. Med. Mol. Imaging. 43, 1723–38 (2016).
Kraus, V. B. et al. Association of bone scintigraphic abnormalities with knee malalignment and pain. Ann. Rheum. Dis. 68, 1673–9 (2009).
Kim, J. Y. & Choi, Y. Y. Bone scintigraphy in the diagnosis of rheumatoid arthritis: is there additional value of bone scintigraphy with blood pool phase over conventional bone scintigraphy?. J. Korean Med. Sci. 31, 502–9 (2016).
Duer, A., Ostergaard, M., Horslev-Petersen, K. & Vallo, J. Magnetic resonance imaging and bone scintigraphy in the differential diagnosis of unclassified arthritis. Ann. Rheum. Dis. 67, 48–51 (2008).
Kaya, M. et al. (99m)Tc-dextran scintigraphy to detect disease activity in patients with rheumatoid arthritis. Nucl. Med. Commun. 25, 597–601 (2004).
Park, H. M., Terman, S. A., Ridolfo, A. S. & Wellman, H. N. A quantitative evaluation of rheumatoid arthritic activity with Tc-99m HEDP. J. Nucl. Med. 18, 973–6 (1977).
Kanazawa, T., Nishino, J., Tohma, S. & Tanaka, S. Analysis of the affected joints in rheumatoid arthritis patients in a large Japanese cohort. Mod. Rheumatol. 23, 44–9 (2013).
Scott, D. L., Antoni, C., Choy, E. H. & Van Riel, P. C. Joint counts in routine practice. Rheumatology (Oxford). 42, 919–23 (2003).
Cheung, P. P., Gossec, L., Mak, A. & March, L. Reliability of joint count assessment in rheumatoid arthritis: A systematic literature review. Semin. Arthritis Rheum. 43, 721–9 (2014).
Marhadour, T. et al. Reproducibility of joint swelling assessments in long-lasting rheumatoid arthritis: influence on Disease Activity Score-28 values (SEA-Repro study part I). J. Rheumatol. 37, 932–7 (2010).
Walsh, C. A. et al. Consistency in assessing the Disease Activity Score-28 in routine clinical practice. Ann. Rheum. Dis. 67, 135–6 (2008).
Bellamy, N. et al. Rheumatoid arthritis antirheumatic drug trials. I. Effects of standardization procedures on observer dependent outcome measures. J. Rheumatol. 18, 1893–900 (1991).
Baker, J. F. et al. Development and validation of modified disease activity scores in rheumatoid arthritis: superior correlation with magnetic resonance imaging-detected synovitis and radiographic progression. Arthritis Rheumatol. 66, 794–802 (2014).
Carstensen, S. M. D., Terslev, L., Jensen, M. P. & Østergaard, M. Future use of musculoskeletal ultrasonography and magnetic resonance imaging in rheumatoid arthritis. Curr. Opin. Rheumatol. 32, 264–72 (2020).
Funding
This work was supported by the National Research Foundation of Korea Grants funded by the Korean Government (NRF-2019R1F1A1062038 and 2017R1A2B2008288) and was supported by Biomedical Research Institute grant, Kyungpook National University Hospital (2017).
Author information
Authors and Affiliations
Contributions
S.J.L. and Y.M.K. contributed to the design of the project interpretation and analysis of the data, and writing of the manuscript. C.M.H., I.C., B.C.A., J.S.E., N.R.K. and J.W.K. contributed to the collection and interpretation of data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, S.J., Hong, C.M., Cho, I. et al. Reappraisal of bone scintigraphy as a new tool for the evaluation of disease activity in patients with rheumatoid arthritis. Sci Rep 11, 21809 (2021). https://doi.org/10.1038/s41598-021-01104-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-01104-w
- Springer Nature Limited
This article is cited by
-
Use of Imaging in Axial Spondyloarthritis for Diagnosis and Assessment of Disease Remission in the Year 2022
Current Rheumatology Reports (2022)