Abstract
The prevalence of obesity and metabolic syndrome increases in patients with type 1 diabetes mellitus (T1DM). In the general population this is linked with ectopic lipid accumulation in liver (HCL) and skeletal muscle (IMCL), representing hallmarks in the development of insulin resistance. Moreover, hepatic mitochondrial activity is lower in newly diagnosed patients with T1DM. If this precedes later development of diabetes related fatty liver disease is currently not known. This study aims to investigate energy metabolism in liver (kATP) and skeletal muscle (kCK) and its impact on HCL, IMCL, cardiac fat depots and heart function in 10 patients with long standing T1DM compared to 11 well-matched controls by 31P/1H magnetic resonance spectroscopy. HCL was almost 70% lower in T1DM compared to controls (6.9 ± 5% vs 2.1 ± 1.3%; p = 0.030). Also kATP was significantly reduced (0.33 ± 0.1 s−1 vs 0.17 ± 0.1 s−1; p = 0.018). In T1DM, dose of basal insulin strongly correlated with BMI (r = 0.676, p = 0.032) and HCL (r = 0.643, p = 0.045), but not with kATP. In the whole cohort, HCL was significantly associated with BMI (r = 0.615, p = 0.005). In skeletal muscle kCK was lower in patients with T1DM (0.25 ± 0.05 s−1 vs 0.31 ± 0–04 s−1; p = 0.039). No significant differences were found in IMCL. Cardiac fat depots as well as heart function were not different. Our results in patients with long standing T1DM show that HCL is lower compared to matched controls, despite reduced energy metabolism in liver and skeletal muscle.
Similar content being viewed by others
Introduction
The prevalence of obesity increases in patients suffering from type 1 diabetes mellitus (T1DM)1. Additionally, growing evidence suggests that liver and skeletal muscle are more insulin resistant in T1DM2. Obesity and insulin resistance represent two major features in the development of metabolic syndrome, which is associated with cardiovascular diseases and increased mortality in general population3.
Despite substantial reductions in the incidence of diabetes related comorbidities, including retinopathy and nephropathy, due to intensive diabetes treatment and better glycemic control4, overall mortality has remained substantially elevated even in patients with well controlled type 1 diabetes5. This increase in mortality is mainly due to cardiovascular diseases and is further enhanced with worsening of glycaemia5. Tight glycemic control in T1DM is mainly achieved by increasing daily insulin dose, which is closely linked with weight gain and thus might trigger metabolic disturbances6. Therefore, characterizing metabolic consequences of exogenous insulin therapy in patients with long standing T1DM is of utmost importance in order to detect future therapeutic targets to improve overall mortality.
In non-diabetic individuals, as well as in patients suffering from type 2 diabetes mellitus (T2DM), ectopic lipid deposition in liver and skeletal muscle represent hallmarks in the development of insulin resistance. However, data on the impact of ectopic fat accumulation for the development of insulin resistance in T1DM is conflicting. Whereas cross-sectional studies using ultrasound measurement techniques in 250 patients with T1DM suggest a prevalence of non-alcoholic fatty liver disease (NAFLD) up to 50%7,8, studies using proton magnetic resonance spectroscopy (1H MRS) showed a significantly lower hepatocellular lipid content (HCL) in obese patients with T1DM compared to non-diabetic control subjects9,10.
Alterations in mitochondrial activity might contribute to ectopic lipid accumulation in insulin sensitive tissues. Forward rates of skeletal muscle mitochondrial oxidative ATP turnover are reduced in insulin resistant individuals11 and correlate negatively with HCL12. Also, in the liver, insulin resistance relates to perturbed mitochondrial energy metabolism, since unidirectional flux through ATP synthase (FATP) is lower in T2DM13. Interestingly, hepatic mitochondrial activity seems to adapt to HCL in early stages of NAFLD, since respiratory capacity is significantly increased compared to lean controls. However, this hepatic mitochondrial flexibility is subsequently lost when liver disease progresses14,15. Recent evidence in newly diagnosed patients with T1DM suggests lower hepatic ATP synthesis, independently of HCL16. If these alterations precede later diabetes-related liver disease and represent a risk to develop NAFLD in later life is not known yet.
With regard to the heart, cardiovascular disease is among the leading causes of death in T1DM. Whereas the overall rate of death from atherosclerosis and myocardial infarction constantly decreased during the last 10 years, no improvements were observed for death from heart failure17. In patients with T2DM excessive lipid accumulation within the myocardium (MYCL) is associated with diastolic dysfunction18. Moreover, not only MYCL, but also pericardial fat (PERI) might contribute to cardiac dysfunction directly by mechanical or paracrine effects19. In T1DM, only little is known on the impact of different cardiac fat depots on heart failure and alterations in cardiac geometry.
Therefore, the aim of this study was (i) to investigate tissue specific energy metabolism in insulin sensitive tissues in patients suffering from long-standing T1DM and (ii) to investigate its impact on ectopic lipid accumulation in liver, skeletal muscle and the heart compared to well matched healthy, non-diabetic controls.
Methods
10 patients with long-standing T1DM were compared to 11 sedentary, healthy controls well matched for age, sex and body mass index (BMI) (Table 1). T1DM patients were required to be on stable dosage of functional insulin therapy for at least 3 months prior to screening visit. The amount of prandial insulin demands and therefore the actual daily absolute insulin dose was highly variable. Therefore only the dose of basal insulin was used for calculations.
Exclusion criteria were evidence of cardiovascular disease, hypoglycemia unawareness or manifest end-organ damage, i.e. diabetic nephropathy, neuropathy or retinopathy.
The ethical committee of the Medical University of Vienna, Austria approved performing the experiments. Written informed consent was obtained from all participating subjects. This study was conducted in full conformance with the relevant guidelines and regulations, i.e. principles of the Declaration of Helsinki and the ICH-GCP guidelines. The study was registered at www.clinicaltrials.gov (NCT02023489).
Subjects were investigated under resting conditions in the morning after an overnight fast of at least ten hours and were asked to refrain from intensive physical training, to stop regular moderate exercise and to ingest an isocaloric diet (30 kcal/kg/day, carbohydrate/protein/fat: 55%/15%/30%) for three days prior to the MR measurements. In T1DM group, stable blood glucose values and the absence of hypoglycemia prior to the study days had to be documented.
On the first study day, subjects underwent 31P/1H magnetic resonance spectroscopy (MRS) of the liver and skeletal muscle, which was performed on a 7 T MR System (Magnetom, Siemens Healthineers, Erlangen, Germany) using a double-tuned (31 P/1 H) surface coil (Rapid Biomedical, Rimpar, Germany), with a diameter of 10 cm. The liver measurements were performed in the right lateral position with the right lobe of the liver positioned over the coil. For estimating hepatic mitochondrial activity (kATP) by 31P MRS, saturation transfer (ST) experiment was performed as described previously14. Concentrations of phosphor-containing hepatic metabolites were measured with 3D multi-voxel MRS based method for absolute quantification20. Hepatocellular lipid content was assessed with single-voxel 1H MRS using ultra-short echo time (TE = 6 ms) and calculated from ratios of summed area of methylene and methyl resonance to that of water following the individual T2 relaxation correction as per cent of total tissue MRS signal (water + methylene + methyl)21. The skeletal muscle measurements were performed in supine position with the calf muscle positioned over the same surface coil. Intramyocellular lipid content (IMCL) was measured in soleus muscle with single voxel 1H MRS using long echo time (TE = 280 ms) and calculated from ratios of area of IMCL methylene resonance to that of water following the individual relaxation correction as percentage of total tissue water MRS signal22. Unidirectional forward rates of oxidative ATP synthase (kATP) and creatine-kinase (kCK) were measured in the same setting with the 31P channel of the surface coil applying saturation transfer technique as described previously14.
On another study day, 1H MRI/MRS of the myocardium was performed on a 3 T Tim Trio System (Siemens Healthineers, Erlangen, Germany). All healthy control subjects underwent both MR measurements. In the T1DM group seven patients participated at cardiac 1H MRI/MRS. Myocardial lipid content (MYCL) was measured by ECG-gated single voxel localized 1H MRS, as described previously23. For cardiac MR visualization, analysis of heart function and pericardial fat from T1-weighted CINE MRI, ARGUS software (Siemens) was used. For pericardial fat (PERI), i.e. paracardial + epicardial adipose tissue, regions of interest were manually drawn along the borders of the fat surrounding the heart in three slices from the apex to the pulmonary trunk. The mean is given in square centimeters.
Laboratory parameters were measured by routine lab methods at AKH Vienna (http://www.kimcl.at).
Based on previous data14,23,24 a sample size of 8 subjects per group was sufficient to detect clinically relevant differences in ectopic lipid content (IMCL ± 0.8%, HCL ± 4%, MYCL ± 0.2%) with alpha = 0.05 and beta = 0.2. Exploratory statistical analysis was performed using SPSS Version 24 (IBM, Armonk, NY, USA). Data is given as means ± standard deviation. Comparison between groups was performed by unpaired Student’s t-test. Correlation analysis was calculated with Pearson’s correlation coefficient (r). Level of statistical significance was set at α < 0.05.
Results
Baseline characteristics
T1DM and controls were of comparable age and BMI. HbA1c and fasting blood glucose was significantly higher in T1DM. Anthropometric characteristics and laboratory values are summarized in Table 1.
Hepatic energy- and lipid metabolism
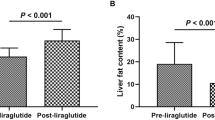
HCL was almost 70% lower in T1DM compared to controls (controls vs T1DM: 6.9 ± 5% vs 2.1 ± 1.3%, p = 0.030). kATP was significantly reduced by half in T1DM (controls vs T1DM: 0.33 ± 0.1 s−1 vs 0.17 ± 0.1 s−1, p = 0.018) (Fig. 1). No differences could be found in absolute concentrations of energy rich phosphate compounds (controls vs T1DM: γ-ATP = 3.2 ± 0.7 mmol/l vs 3.0 ± 0.4 mmol/l, p = n.s.; inorganic phosphate = 1.4 ± 0.3 mmol/l vs 1.4 ± 0.3 mmol/l, p = n.s.; phosphatidylcholine = 1.0 ± 0.3 mmol/l vs 1.2 ± 0.4 mmol/l, p = n.s., phosophoethanolamine = 1.43 ± 0.6 mmol/l vs 1.55 ± 0.5 mmol/l, p = n.s., NADH = 1.1 ± 0.2 mmol/l vs 1.1 ± 0.2 mmol/l, p = n.s). Dose of basal insulin strongly correlated with BMI (r = 0.676, p = 0.032) and HCL (r = 0.643, p = 0.045), while no significant associations were observed for kATP and concentrations of phosphate compounds. In the whole cohort, HCL was significantly associated with BMI (r = 0.615, p = 0.005).
Skeletal muscle energy- and lipid metabolism
No significant differences were found in soleus IMCL (0.50 ± 0.4% vs 0.88 ± 0.5%, p = 0.114). kCK was markedly reduced in T1DM (0.25 ± 0.05 s−1 vs 0.31 ± 0.04 s−1, p = 0.039). No differences in the basal levels of phosphorus-containing metabolites were found. In correlation analysis, there was no association found between age, BMI, insulin dose and IMCL or kCK. Skeletal muscle kCK correlated with hepatic kATP over the whole study cohort (r = 0.560, p = 0.020).
Myocardial lipid stores and heart function
No differences were observed for MYCL and PERI. Parameters of cardiac function were comparable in T1DM and healthy controls (Table 2). No significant correlations with diabetes duration, insulin dose and anthropometric characteristics were found.
Discussion
Recent evidence reports alterations in hepatic mitochondrial function in recently diagnosed T1DM with disease duration of about six months. It was suggested that these changes in energy metabolism might precede later diabetes-related liver disease16, which is not supported by our present data in patients with long term disease duration. In our group of patients with T1DM hepatic kATP is reduced as well. However, this is not linked with hepatic steatosis, since HCL was significantly lower in our population with long standing T1DM (25 ± 11 years) compared to the matched control group. This is in line with previous studies, showing that liver fat content is significantly lower in T1DM compared to non-diabetic controls9,10.
The link between lower rates of ATP synthesis rates together with lower HCL stands in sharp contrast to T2DM13,14,15. A possible explanation might be the unphysiological insulin delivery in T1DM. Ferranini et al. reported significantly higher insulin concentrations in the splanchnic region compared to peripheral tissue under fasting conditions in non-diabetic healthy subjects25. Whereas under physiological conditions pancreatic insulin is delivered directly to the liver, where approximately half of the insulin is extracted by first-pass effects, there is a relative increase in systemic insulin levels and low portal insulin concentrations following subcutaneous injection26. This relative lack of insulin in the splanchnic region might explain increased rates of endogenous glucose production during fasting conditions in patients with T1DM, despite higher hepatic insulin sensitivity9. Moreover, lower HCL might be explained by the loss of a physiological portal to peripheral insulin ratio in T1DM, as insulin is the main stimulator of de novo lipogenesis and ectopic triglyceride accumulation27.
Since insulin strongly stimulates ATP production28, basal rates of hepatic energy metabolism might be lower because of a relative lack of insulin in the splanchnic region. On the other hand, hepatic kATP might be decreased in connection with lower HCL in T1DM. Recent studies demonstrate lower ATP synthesis rates in the liver of lean, healthy controls compared to patients with NAFLD, reflecting mitochondrial flexibility in early stages of disease by increasing energy turnover in case of excessive substrate availability. This flexibility is subsequently lost, when liver disease progresses, resulting in inadequately reduced mitochondrial ATP turnover, despite higher HCL14,15.
With regard to skeletal muscle, similar to previous reports energy turnover is reduced in our patients with T1DM28,29. These alterations might be due to changes in circulating glucose and insulin concentrations. Moreover, insulin deficiency by short-term insulin deprivation prompted a decrease in muscle ATP production rates, but also at mitochondrial gene transcription levels30. In our cohort blood glucose values and HbA1c were significantly higher in T1DM compared to controls, probably indicating an at least temporary hypoinsulinemia, which could account for observed changes in skeletal muscles kCK.
There are conflicting results on IMCL in T1DM in the literature. Whereas others28 and we did not observe significant differences, IMCL was reported to be significantly higher in T1DM in earlier studies, similar to the insulin resistant state and T2DM31. These differences are most likely explained by long-term glucose control in investigated groups of patients, since IMCL was higher in T1DM with higher HbA1c, compared to our rather well controlled patient group.
The initiation of insulin therapy in patients with type 2 diabetes mellitus is associated with an acute increase in myocardial lipid stores32. However in contrast to this observation, with regard to the heart, neither ectopic or pericardial fat deposition nor cardiac function was different in T1DM. Our data is in line with previous publications of a large cohort of patients with T1DM participating in the diabetes control and complications trial (DCCT), in which cardiac geometry and function was normal33. Also, short-term hyperglycemic dysregulation after partial insulin deprivation for 24 hours had no effect on MYCL34. Thus, MYCL adapts differently in T1DM compared to insulin sensitive, healthy subjects, in which even in the absence of circulating free fatty acids an elevation in glucose concentrations significantly increased lipid deposition within the myocardium24. This could be explained by tracer studies reporting lower rates of glucose uptake into the myocardium under resting conditions in T1DM resembling cardiac insulin resistance. However, during hyperlipidemia and hyperinsulinemia, the heart is still able to adapt adequately to alterations in substrate availability indicating an intact metabolic flexibility35. Therefore, typical features of diabetic cardiomyopathy could not be found in T1DM.
This study has several limitations. First of all, the sample size is relatively small. However, according to sample size calculations based on our previous reports, the included number of patients was sufficient to observe assumed differences in hepatic energy metabolism14. Also for the assessment of ectopic lipid content in insulin sensitive tissue previous reports of our study group showed significant differences between groups of similar sample size due to the high sensitivity and low inter- and intraobserver variability of high resolution state of the art MRS techniques23,24. Moreover, we are not able to prove our hypothesis that the observed differences in hepatic energy metabolism and lipid content are because of a loss of the physiological portal to peripheral insulin ratio in T1DM during subcutaneous insulin therapy, since only peripheral blood samples were drawn at the study days.
Taken together, our results in patients with long standing T1DM show, that HCL is even lower compared to matched controls, despite lower hepatic and skeletal muscle energy metabolism. This might be explained by unphysiological portal to peripheral insulin ratio or by preserved metabolic flexibility. No differences in IMCL, cardiac fat depots and heart function could be found. Our findings are important for patients suffering from T1DM, as well as for treating physicians, since they indicate that NAFLD as well as cardiac steatosis is no clinically relevant long-term consequence of insulin therapy. Therefore, screening for sequelae of long standing T1DM should focus on well-established cardiovascular risk factors like diabetic nephropathy and LDL-cholesterol5 to reduce cardiovascular mortality.
References
Thorn, L. et al. Metabolic Syndrome in Type 1 Diabetes: Association with diabetic nephropathy and glycemic control (the FinnDiane study). Diabetes care 28, 2019–2024 (2005).
Bergman, B. C. et al. Features of hepatic and skeletal muscle insulin resistance unique to type 1 diabetes. The Journal of clinical endocrinology and metabolism 97, 1663–1672 (2012).
Pischon, T. et al. General and Abdominal Adiposity and Risk of Death in Europe. The New England Journal of Medicine 359, 2105–2120 (2008).
Group, T. D. S. R. Intensive Diabetes Treatment and Cardiovascular Disease in Patients with Type 1 Diabetes. The New England Journal of Medicine 353, 2643–2653 (2005).
Lind, M. et al. Glycemic control and excess mortality in type 1 diabetes. N Engl J Med 371, 1972–1982 (2014).
Cleland, S., Fisher, B., Colhoun, H., Sattar, N. & Petrie, J. Insulin resistance in type 1 diabetes: what is ‘double diabetes’ and what are the risks? Diabetologia 56, 1462–1470 (2013).
Targher, G. et al. Prevalence of non-alcoholic fatty liver disease and its association with cardiovascular disease in patients with type 1 diabetes. J Hepatol 53, 713–718 (2010).
Harman, D. J. et al. Prevalence and natural history of histologically proven chronic liver disease in a longitudinal cohort of patients with type 1 diabetes. Hepatology 60, 158–168 (2014).
Llaurado, G. et al. Liver fat content and hepatic insulin sensitivity in overweight patients with type 1 diabetes. The Journal of clinical endocrinology and metabolism 100, 607–616 (2015).
Perseghin, G. et al. Reduced intrahepatic fat content is associated with increased whole-body lipid oxidation in patients with type 1 diabetes. Diabetologia 48, 2615–2621 (2005).
Petersen, K. F., Dufour, S. & Shulman, G. I. Decreased insulin-stimulated ATP synthesis and phosphate transport in muscle of insulin-resistant offspring of type 2 diabetic parents. PLoS medicine 2, e233 (2005).
Szendroedi, J. et al. Lower fasting muscle mitochondrial activity relates to hepatic steatosis in humans. Diabetes care 37, 468–474 (2014).
Schmid, A. I. et al. Liver ATP synthesis is lower and relates to insulin sensitivity in patients with type 2 diabetes. Diabetes care 34, 448–453 (2011).
Valkovic, L. et al. Application of localized 31P MRS saturation transfer at 7T for measurement of ATP metabolism in the liver: reproducibility and first clinical application in patients with non-alcoholic fatty liver disease. Eur Radiol 24, 1602–1609 (2014).
Koliaki, C. et al. Adaptation of hepatic mitochondrial function in humans with non-alcoholic fatty liver is lost in steatohepatitis. Cell metabolism 21, 739–746 (2015).
Gancheva, S. et al. Variants in Genes Controlling Oxidative Metabolism Contribute to Lower Hepatic ATP Independent of Liver Fat Content in Type 1 Diabetes. Diabetes 65, 1849–1857 (2016).
Go, A. S. et al. Executive Summary: Heart Disease and Stroke Statistics–2013 Update: A Report From the American Heart Association. Circulation 127, 143–152 (2013).
Rijzewijk, L. J. et al. Myocardial steatosis is an independent predictor of diastolic dysfunction in type 2 diabetes mellitus. Journal of the American College of Cardiology 52, 1793–1799 (2008).
Wolf, P. et al. Pericardial- Rather than Intramyocardial Fat Is Independently Associated with Left Ventricular Systolic Heart Function in Metabolically Healthy Humans. PloS one 11, e0151301 (2016).
Pfleger, L. et al. Absolute quantification of hepatic metabolites using localized 31P MRS at 7T. In ESMRMB (2016).
Gajdosik, M. et al. Ultrashort-TE stimulated echo acquisition mode (STEAM) improves the quantification of lipids and fatty acid chain unsaturation in the human liver at 7 T. NMR Biomed 28, 1283–1293 (2015).
Klepochova, R. et al. Differences in Muscle Metabolism Between Triathletes and Normally Active Volunteers Investigated Using Multinuclear Magnetic Resonance Spectroscopy at 7T. Front Physiol 9, 300 (2018).
Krššák, M. et al. Insulin resistance is not associated with myocardial steatosis in women. Diabetologia 54, 1871–1878 (2011).
Winhofer, Y. et al. Short-term hyperinsulinemia and hyperglycemia increase myocardial lipid content in normal subjects. Diabetes 61, 1210–1216 (2012).
Ferrannini, E. et al. Splanchnic and renal metabolism of insulin in human subjects: a dose-response study. American Journal of Physiology 244, E517–E527 (1983).
Herring, R., Jones, R. & Russell-Jones, D. L. Hepatoselectivity and the evolution of insulin. Diabetes, obesity & metabolism 16, 1–8 (2014).
Brown, M. S. & Goldstein, J. L. Selective versus total insulin resistance: a pathogenic paradox. Cell metabolism 7, 95–96 (2008).
Kacerovsky, M. et al. Impaired insulin stimulation of muscular ATP production in patients with type 1 diabetes. Journal of internal medicine 269, 189–199 (2011).
Cree-Green, M. et al. Delayed skeletal muscle mitochondrial ADP recovery in youth with type 1 diabetes relates to muscle insulin resistance. Diabetes 64, 383–392 (2015).
Karakelides, H. et al. Effect of Insulin Deprivation on Muscle Mitochondrial ATP Production and Gene Transcript Levels in Type 1 Diabetic Subjects. Diabetes 56, 2683–2689 (2007).
Perseghin, G. et al. Insulin resistance, intramyocellular lipid content, and plasma adiponectin in patients with type 1 diabetes. American journal of physiology. Endocrinology and metabolism 285, 1174–1181 (2003).
Jankovic, D. et al. Effects of insulin therapy on myocardial lipid content and cardiac geometry in patients with type-2 diabetes mellitus. PloS one 7, e50077 (2012).
Genuth, S. et al. Effects of Prior Intensive Versus Conventional Therapy and History of Glycemia on Cardiac Function in Type 1 Diabetes in the DCCT/EDIC. Diabetes 62, 3561–3569 (2013).
Hammer, S. et al. Short-term hyperglycemic dysregulation in patients with type 1 diabetes does not change myocardial triglyceride content or myocardial function. Diabetes care 31, 1613–1614 (2008).
Peterson, L. R. et al. Fatty acids and insulin modulate myocardial substrate metabolism in humans with type 1 diabetes. Diabetes 57, 32–40 (2008).
Acknowledgements
The authors thank all participants for taking part at study related experiments. All authors substantially contributed to this work. P.W. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. M.K. has received research support from Sanofi and AstraZeneca as well as speaker and consulting fees from AstraZeneca, Novartis, Novo Nordisk, Lilly, Merck, Böhringer and Sanofi. A.L. received speaker and consulting fees from Lilly, Novo Nordisk and Sanofi. The other authors don’t have to report a potential conflict of interest. This study was in parts funded by grants from the Austrian Association of Endocrinology and Metabolism (ÖGES) to P.W., the Austrian National Bank (Nr. 13249 and 15363 to M. Krs.) and an unrestricted grant from Sanofi.
Author information
Authors and Affiliations
Contributions
P.W., Y.W., M. Krs. And M. Kre. had the initial idea and designed the study, supervised experimentation, analyzed the data, coordinated the project and wrote the manuscript; P.W., H.B., S.S., M.G., L.P. and P.F. recruited subjects, performed the study and conducted the experiments; C.H.A., S.T. and A.L. assisted in data interpretation and contributed to discussion.
Corresponding author
Ethics declarations
Competing Interests
M. Kre. has received research support from Sanofi and AstraZeneca as well as speaker and consulting fees from AstraZeneca, Novartis, Novo Nordisk, Lilly, Merck, Böhringer and Sanofi. A.L. received speaker and consulting fees from Lilly, Novo Nordisk and Sanofi. The other authors don’t have to report a potential conflict of interest. All other authors have nothing to declare.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wolf, P., Fellinger, P., Pfleger, L. et al. Reduced hepatocellular lipid accumulation and energy metabolism in patients with long standing type 1 diabetes mellitus. Sci Rep 9, 2576 (2019). https://doi.org/10.1038/s41598-019-39362-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-39362-4
- Springer Nature Limited