Abstract
Solid malignancies are associated with the development of Pneumocystis jirovecii pneumonia (PJP). This study aimed to evaluate the risk factors for PJP among patients with lung cancer. This retrospective case-control study compared patients who had lung cancer with PJP (n = 112) or without PJP (n = 336) matched according to age, sex, histopathology, and stage. PJP definition was based on (i) positive PCR or direct immunofluorescence results for pneumocystis, (ii) clinical symptoms and radiological abnormalities that were consistent with a pneumonic process, and (iii) received targeted PJP treatment. The development of PJP was associated with radiotherapy (RTx), concurrent chemoradiotherapy (CCRTx), lymphopenia, and prolonged high-dose steroid therapy (20 mg of prednisolone equivalent per day for ≥3 weeks). Multivariate analysis revealed independent associations with prolonged high-dose steroid therapy (odds ratio [OR]: 1.96, 95% confidence interval [CI]: 1.06–3.63; p = 0.032) and CCRTx (OR: 2.09, 95% CI: 1.27–3.43; p = 0.004). Steroid use was frequently related to RTx pneumonitis or esophagitis (29 patients, 43.3%). Prolonged high-dose steroid therapy and CCRTx were risk factors for PJP development among patients with lung cancer. As these patients had a poor prognosis, clinicians should consider PJP prophylaxis for high-risk patients with lung cancer.
Similar content being viewed by others
Introduction
Pneumocystis jirovecii pneumonia (PJP) is an opportunistic infection caused by the fungus Pneumocystis jirovecii1. During 1980–2000, most PJP cases involved patients with acquired immunodeficiency syndrome (AIDS), although PJP has become common in non-human immunodeficiency virus (HIV)-infected cases because of improvements in AIDS treatment and more patients receiving immunosuppressive therapy2. However, non-HIV-infected patients with PJP have an overall mortality rate of approximately 35–55%3,4,5, compared to 10–20% among patients with AIDS6.
Hughes et al.7 reported that the incidence of PJP in acute lymphoblastic leukemia (ALL) ranged from 22% to 45%, depending on the chemotherapy used and the stage of leukemia. Another study also reported that without prophylaxis, PJP rates may approach 25% among patients with non-Hodgkin’s lymphoma8. In a recent study, PJP incidence of acute leukemia, chronic lymphocytic leukemia, and non-Hodgkin lymphoma was estimated to be >45 cases per 100,000 patient year, whereas PJP incidence of solid tumors was <25 cases per 100,000 patient-year9. Possible explanations of higher incidence of PJP in hematologic malignancies are related to high intensity of chemotherapy7 and severely impaired immune function10. After routine performance of prophylaxis using trimethoprim-sulfamethoxazole (TMP-SMX), incidence of PJP among patients with hematologic malignancies has shown remarkable decrease11.
Although the exact incidence of PJP in solid tumors still remains unknown, recent reports have reported PJP cases in lung cancer, which is the most common cause of solid malignancy-related death3,9,12. However, little is known about the risk factors for PJP development and who would benefit from PJP prophylaxis in lung cancer patients. Therefore, this study aimed to evaluate the risk factors for PJP among patients with lung cancer.
Patients and Methods
Study design and population
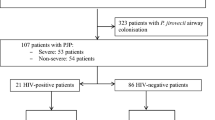
Electronic medical records from the Severance Hospital (a 2,500-bed tertiary referral hospital in South Korea) were searched to identify 3,877 patients with lung cancer who underwent surgery, chemotherapy (CTx), and/or radiotherapy (RTx) between January 2013 and December 2016. Among these patients, 311 patients had received treatment for PJP using intravenous and/or oral TMP-SMX (trimethoprim: 15–20 mg/kg/day, sulfamethoxazole: 75–100 mg/kg/day). However, cases were excluded if they had an unsatisfactory definition of PJP (n = 188), other cancers (n = 7), organ transplantation (n = 3), or HIV infection (n = 1). Thus, records from 112 patients with confirmed lung cancer and PJP were matched 1:3 with control patients (n = 336, lung cancer without PJP) according to age, sex, histopathology, and stage using exact match modeling (Fig. 1). Treatment modalities of lung cancer, including types of chemotherapy, were determined by relevant physician on a case-by-case basis, and treatment principles were based on national comprehensive cancer network (NCCN) guideline over study period13,14.
PJP Definition
PJP was considered present when the patient fulfilled three conditions. The first condition was a positive result for Pneumocystis jirovecii using either real-time PCR testing or direct immunofluorescence testing of spontaneous sputum, induced sputum, bronchoalveolar lavage (BAL), or tissue samples. The real-time PCR assay was performed with the AmpliSens Pneumocystis jirovecii-FRT PCR kit (Moscow, Russia), which is a qualitative test based on the endogenous control, the β-globin gene. Ten-microliter DNA samples were added in each reaction tubes. PCRs were performed on the Bio-Rad CFX-96 real-time PCR system (Bio-Rad, Hercules, CA) according to the manufacturer’s instruction. The second condition was the presence of lung infiltration during chest radiography or computed tomography (CT)10,15,16. The third condition was clinical symptoms of PJP and PJP treatment during their hospitalization. We defined the prophylaxis group as those without a PJP diagnosis who received medication to prevent PJP.
Data collection
Demographic and clinical data were collected through a chart review. The lowest total lymphocyte count was selected from the 2 weeks before the PJP diagnosis (PJP group) or during the follow-up period (control group), and lymphopenia was defined as <1,000 cells/µL17. The daily dosage of steroids was expressed in prednisolone equivalents, and the continuous maximum use of steroids was recorded as the cumulative steroid dose. We did not consider intermittent steroid use (e.g., as emesis prophylaxis during CTx), or steroid use that was stopped at >1 month before the PCP diagnosis, in order to more accurately account for the effect of steroid treatment on PJP development18. Steroid dosage during the last 2 weeks before the PJP diagnosis was compared to the dosage during the preceding weeks, and changes during the 2 last weeks were categorized as maintained, increased, tapered, or stopped17. Adjunctive steroid use during PJP treatment was defined a high-dose (≥60 mg/day prednisolone equivalent), low-dose (<60 mg/day prednisolone equivalent), or absent19. The 60-mg cut-off was selected because it was the lowest effective dose in controlled trials for HIV-infected patients with PJP1,20. RTx-induced pneumonitis was diagnosed based on the patients’ symptoms (low-grade fever, dry cough, dyspnea, or chest pain) and radiological manifestations21,22. Radiation-induced esophagitis was also defined based on clinical symptoms (dysphagia, odynophagia, and substernal discomfort)23. Data from chest radiography and CT were evaluated independently by one radiologist at the PJP diagnosis, and then independently confirmed by two of the authors (EH Lee, MS Park). Medical records related to risk factors for PJP development were studied until PJP development in PJP patients, whereas those in controls were studied until death, transfer to another hospital, or December 2016.
Statistical analysis
Normally distributed continuous variables were reported as mean ± standard deviation, while non-normally distributed variables were reported as median (range). Continuous variables were analyzed using the Student t-test or the Mann-Whitney test. Categorical variables were reported as number and percentage, and compared using the chi-square test or Fisher’s exact test. The independent risk factors for PJP development were evaluated using conditional logistic regression modeling based on the matched paired data, and the results were reported as odds ratios (ORs) and 95% confidence intervals (CIs). A two-tailed P-value of <0.05 was considered statistically significant. All analyses were performed using SAS software (version 9.4; SAS Inc., Cary, NC).
Ethics
The research protocol was approved by the Institutional Review Board (IRB) of Severance Hospital (IRB No. 4-2017-0431). The need for informed consent was waived due to the retrospective nature of the study. All methods were carried out in accordance with relevant guidelines and regulations.
Results
Clinical characteristics and outcomes for PJP
The most common symptom of PJP was dyspnea (71.4%), followed by fever (27.7%) and cough (23.2%) (Table 1). The median respiratory symptom duration was 3 days (range: 1–20 days). Sixty-seven patients (59.8%) received steroids within 1 month before developing PJP. The most common reasons for steroid treatment were RTx complications like RTx pneumonitis or esophagitis (29 patients, 43.3%), relief of tumor infiltration symptoms (24 patients, 35.8%) such as increased intracranial pressure, bronchus obstruction, spinal cord compression and adrenal insufficiency (8 patients, 11.9%). Six patients (8.9%) received steroids because of exacerbated underlying lung disease. At the PJP diagnoses, 33 patients (49.3%) had a maintained dosage, 23 patients (34.3%) had a tapered dosage, and 11 patients (16.4%) had stopped steroid treatment. The most common findings were diffuse interstitial infiltrates during radiography (66.9%) and bilateral ground-glass attenuation during CT (66.3%). Focal consolidation and ground-glass opacities were also detected.
Table 2 shows treatment outcomes of PJP patients with lung cancer. All patients had received TMP-SMX, although 7 patients (6.3%) required second-line medication due to progression of PJP despite TMP-SMX therapy (primaquine and clindamycin in 6 cases, pentamidine in 1 case). Seventy-five patients (67%) received high-dose adjunctive steroids during PJP treatment, 26 patients (23.2%) received low-dose adjunctive treatment, and 11 patients (9.8%) did not receive adjunctive steroids. The median duration of PJP treatment was 13 days (range: 2–89 days), and 69 of the 112 patients (61.6%) died during PJP treatment (respiratory failure: 72.5%, cancer progression: 14.5%, and respiratory failure with cancer progression: 13.0%). Among the 69 deaths, 47 deaths (68.1%) involved a do-not-resuscitate and do-not-intubate order, and only 6 patients (8.7%) had a full code status.
Baseline characteristics of patients according to PJP status
Table 3 shows the clinical characteristics of the matched patients with and without PJP. The median patient age was 69 years (range: 42–88), and most patients were men (83%). The most frequent histopathological types were adenocarcinoma (46.4% vs. 49.4%), squamous cell carcinoma (36.6% vs. 35.7%), and small cell lung cancer (12.5% vs. 14.3%). Approximately 75% of the patients had stage IV lung cancer. More than 90% of the patients received CTx (94.6% vs. 92.6%), although the control group had a longer median CTx duration than the PJP group (123 days vs. 97 days). The types and frequency of chemotherapeutic agents showed no statistical difference between PJP group and control group. RTx or concurrent chemoradiation therapy (CCRTx) were more common in the PJP group, compared to the control group (RTx: 77.7% vs. 64.3%, p = 0.009; CCRTx: 39.3% vs. 21.7%, p < 0.001). Surgery was more common in the control group (11.6% vs. 23.8%, p = 0.006). The median daily steroid dose and proportion of steroid use were similar in the two groups (59.8% vs. 55.4%, p = 0.409). The median cumulative steroid dose tended to be higher in the PJP group (915 mg vs. 754 mg, p = 0.062) and the duration of steroid use was significantly longer in the PJP group (42 days vs. 26.5 days, p = 0.005). Patients with prolonged high-dose steroid use (20 mg of prednisolone equivalent per day for ≥3 weeks) were more common in the PJP group, compared to the control group (30 patients [26.8%] vs. 47 patients [14%], p = 0.002). The mean lymphocyte counts were 425/µL (range: 60–1,920/µL) in the PJP group and 540/µL (range: 10–2,730/µL) in the control group. The PJP group had a higher proportion of patients with lymphopenia (92% vs. 82.1%, p = 0.013). Only 30 of the 448 cases and controls (6.7%) received PJP prophylaxis, which was less frequent in the PJP group, compared to the control group (3 patients [2.7%] vs. 27 patients [8%], p = 0.049).
Risk factors for PJP
In the univariate analyses (Table 4), PJP development was significantly associated with RTx (OR: 1.95, 95% CI: 1.18–3.25; p = 0.001), CCRTx (OR: 2.59, 95% CI: 1.58–4.25; p < 0.001), lymphopenia (OR: 2.68, 95% CI: 1.23–5.82; p = 0.013), and prolonged high-dose steroid therapy (OR: 2.49, 95% CI: 1.42–4.37); p = 0.002). PJP development was inversely but non-significantly associated with TMP-SMX prophylaxis (OR: 0.33, 95% CI: 0.10–1.09; p = 0.068). In the multivariate analyses, PJP development was independently associated with prolonged high-dose steroid therapy (OR: 1.96, 95% CI: 1.06–3.63; p = 0.032) and CCRTx (OR: 2.09, 95% CI: 1.27–3.43; p = 0.004). Surgery also was inversely associated with PJP development in the multivariate analysis (OR: 0.42, 95% CI: 0.22–0.79; p = 0.008), although this is likely because patients who were able to undergo surgery would be less likely to receive CTx or RTx for their early-stage cancer.
Discussion
Lung cancer is the most common cause of cancer death worldwide although the survival rate has improved due to the use of novel targeted therapies plus conventional therapies24. Disease progression itself may have influenced the prognosis and patient’s survival, infection and pneumonia are typically associated with poor prognoses among these immunocompromised patients25. Bacterial pneumonia is relatively common in this setting, compared to PJP, although recent studies have also indicated that PJP occurs among patients with solid malignancies, such as lung cancer3,26,27,28. Thus, the present study compared patients who had lung cancer with or without PJP, and the results revealed that prolonged high-dose steroid use and CCRTx were independent risk factors for developing PJP in this setting.
Long-term corticosteroid use is a known risk factor for developing PJP among non-HIV-infected patients29,30, which is likely related to their effects on T-cell immunity8. However, the present study detected a relatively small proportion of patients with steroid use and relatively low cumulative steroid dose in the PJP group, compared to the findings from previous studies12,18. This discrepancy may be related to differences in the definition of steroid use and other risk factors that might influence PJP development. For example, the present study excluded cases from the steroid use group if the steroid treatment was stopped at >1 month before the PJP diagnosis. In addition, we excluded cases with intermittent steroid use, and compared the maximum cumulative continuous steroid dose in the PJP and control groups. As a result, we did not detect a significant inter-group difference in daily steroid dose or cumulative maximum dose. However, when we categorized the patients according to daily steroid dose and duration, we found that a specific cut-off value (20 mg of prednisolone equivalent per day for ≥3 weeks) was independently associated with PJP development, although the area under the curve was low (0.568).
Previous studies have indicated that RTx could be a risk factor for PJP development5,31. In this study, univariate analysis revealed the RTx was associated with PJP development, this association was statistically insignificant in the multivariate analysis. Other reports have indicated that specific chemotherapeutic agents, such as fluorouracil, bleomycin, asparaginase, fludarabine, and gemcitabine, were associated with the risk of PJP development3,27,28,32. Patients who receive high-dose steroids with cytotoxic CTx or RTx could be even more vulnerable to PJP development28. In the current study, specific chemotherapeutic agents did not increase the risk of PJP, while CCRTx was significantly associated with PJP development in multivariate analysis (p = 0.004).
The present study revealed that most patients who developed PJP had decreased lymphocyte counts (median: 425/µL, range: 60–1,920/µL), which was a significant risk factor in the univariate analysis but not in the multivariate analysis. Mansharamani et al. have suggested that a cut-off value of 300 CD4+ cells/µL would include 91% of PJP cases among HIV-negative patients, which is a high-risk group, although 39–46% of individuals who received long-term corticosteroid therapy also had CD4+ counts of <300/µL33. Moreover, the accuracy of this biomarker is poorly characterized for non-HIV-infected patients, which limits its use in that population, although it is an accurate method for assessing PJP risk among patients with AIDS18,34.
The characteristics of our patients with PJP and lung cancer were different from those of non-HIV-infected patients in other studies. The most common clinical symptom was dyspnea in the present study, and our patients’ respiratory symptoms tended to manifest quickly, which was also observed in previous studies12,35. However, the frequencies of fever and cough were relatively low in our study, compared to previous studies12,35. This discrepancy may be related to reduced immunity caused by CTx and/or RTx, which could mask signs of infection. The reported prognosis of PJP is poorer among non-HIV-infected patients, compared to HIV-infected patients36, although we observed a much higher mortality rate during PJP treatment (approximately 60%), compared to other studies conducted in non-HIV-infected patients5,35. In this current study, most patients received first-line TMP-SMX treatment and approximately 67% of the patients with PJP also received high-dose adjunctive steroids during their PJP treatment19. Thus, the poor prognosis may be related to the advanced lung cancer and/or the weakened general condition of patients who receive CTx and/or RTx before developing PJP. It is also possible that the large proportion of patients with do-not-resuscitate or do-not-intubate statuses was responsible for the relatively high mortality rate among our patients with lung cancer and PJP.
Among HIV-infected patients, TMP-SMX prophylaxis is highly effective for preventing PJP34. A recent meta-analysis also indicated that, among solid organ transplant recipients and patients with hematological malignancies, TMP-SMX treatment was associated with reductions in the occurrence of PJP (RR: 0.09, 95% CI: 0.02–0.32) and PJP-related mortality (RR: 0.17, 95% CI: 0.03–0.94), which suggests that PJP prophylaxis is warranted when adult patients have a >3.5% risk of PJP11. Several studies have indicated that solid malignancies are associated with an increased risk of PJP3,12,28,37, although there are no clinical data supporting the routine use of PJP prophylaxis for patients with solid tumors. The American Thoracic Society recommends considering prophylaxis when immunocompromised patients (including patients with solid tumors) receive prolonged high-dose corticosteroid treatment (20 mg of prednisolone equivalent per day for ≥4 weeks), although it acknowledges that this recommendation is based on a low level of evidence38. The present study also confirmed that PJP prophylaxis is not routine for patients with lung cancer, even for patients who are receiving prolonged high-dose steroid therapy. As PJP prophylaxis can significantly reduce mortality among patients with other diseases, it may be beneficial to provide PJP prophylaxis to high-risk patients with lung cancer. For example, prolonged high-dose steroid therapy and CCRTx were possible risk factors for PJP among patients with lung cancer, and the most common reason for steroid use was radiation-induced pneumonitis, which is relatively common after CCRTx (vs. RTx)21. Therefore, it seems reasonable to use PJP prophylaxis for patients who are receiving prolonged high-dose steroid treatment and CCRTx.
The present study has several limitations. First, the single-center retrospective design is associated with known risks of bias, and we were unable to collect exact information regarding symptom presentation or duration before the PJP diagnosis. Thus, our findings may not be generalized to other centers or patient populations. Second, proportion of surgery in PJP cases and controls are somewhat different, suggesting the possibility of inadequate cancer stage matching. Third, we used PCR and immunofluorescence data to diagnose PJP, and our data may include false-positive results, as a confirmed PJP diagnosis generally requires special microbiological staining of respiratory specimens39. However, non-HIV-infected patients have a lower overall organism burden40 compared to HIV-infected patients, and conventional staining methods might have provided lower sensitivity and false-negative results. A meta-analysis of PCR-based PJP diagnosis revealed a sensitivity of 99% and specificity of 92% among non-HIV-infected patients, and that 31.8% of patients with false-positive results had or subsequently developed PJP41. Thus, patients with a positive PCR result require careful follow-up and/or PJP treatment. Other reports have also suggested that PCR assays for PJP are sensitive and increase the diagnostic yield among non-HIV-infected immunocompromised patients16,42,43. Therefore, to reduce the likelihood of false-positive results, we only included patients with symptoms of acute pulmonary infiltrates, such as cough, dyspnea, and radiological abnormalities.
Despite its limitations, the present study also has several strengths. To the best of our knowledge, this is the first case-control study of PJP among patients with lung cancer. In addition, we matched the patients with PJP to a relatively large number of control patients, which provides a clearer perspective regarding the risk factors for PJP development among patients with lung cancer. Furthermore, our findings may be useful for identifying high-risk patients with lung cancer who should receive PJP prophylaxis. Nevertheless, multicenter randomized controlled trials are needed to examine the value of PJP prophylaxis in this setting.
Conclusion
In conclusion, the present study revealed that prolonged high-dose steroid therapy (20 mg of prednisolone equivalent per day for ≥3 weeks) and CCRTx were risk factors for PJP development among patients with lung cancer. These patients had a very poor prognosis. Furthermore, the most common reasons for the steroid treatment were CCRTx or RTx-induced pneumonitis. Therefore, clinicians should consider PJP prophylaxis for high-risk patients with lung cancer.
Data Availability
All datasets generated and analysed during this study are available from the corresponding author on reasonable request.
References
Thomas, C. F. Jr. & Limper, A. H. Pneumocystis pneumonia. N Engl J Med 350, 2487–2498, https://doi.org/10.1056/NEJMra032588 (2004).
Kovacs, J. A. & Masur, H. Evolving health effects of Pneumocystis: one hundred years of progress in diagnosis and treatment. Jama 301, 2578–2585, https://doi.org/10.1001/jama.2009.880 (2009).
Sepkowitz, K. A., Brown, A. E., Telzak, E. E., Gottlieb, S. & Armstrong, D. Pneumocystis carinii pneumonia among patients without AIDS at a cancer hospital. Jama 267, 832–837 (1992).
Mansharamani, N. G., Garland, R., Delaney, D. & Koziel, H. Management and outcome patterns for adult Pneumocystis carinii pneumonia, 1985 to 1995: comparison of HIV-associated cases to other immunocompromised states. Chest 118, 704–711 (2000).
Roblot, F. et al. Analysis of underlying diseases and prognosis factors associated with Pneumocystis carinii pneumonia in immunocompromised HIV-negative patients. Eur J Clin Microbiol Infect Dis 21, 523–531, https://doi.org/10.1007/s10096-002-0758-5 (2002).
Pulvirenti, J., Herrera, P., Venkataraman, P. & Ahmed, N. Pneumocystis carinii pneumonia in HIV-infected patients in the HAART era. AIDS Patient Care STDS 17, 261–265, https://doi.org/10.1089/108729103322108139 (2003).
Hughes, W. T. et al. Intensity of immunosuppressive therapy and the incidence of Pneumocystis carinii pneumonitis. Cancer 36, 2004–2009 (1975).
Sepkowitz, K. A., Brown, A. E. & Armstrong, D. Pneumocystis carinii pneumonia without acquired immunodeficiency syndrome. More patients, same risk. Arch Intern Med 155, 1125–1128 (1995).
Fillatre, P. et al. Incidence of Pneumocystis jiroveci pneumonia among groups at risk in HIV-negative patients. Am J Med 127(1242), e1211–1247, https://doi.org/10.1016/j.amjmed.2014.07.010 (2014).
Thomas, C. F. Jr. & Limper, A. H. Current insights into the biology and pathogenesis of Pneumocystis pneumonia. Nat Rev Microbiol 5, 298–308, https://doi.org/10.1038/nrmicro1621 (2007).
Green, H., Paul, M., Vidal, L. & Leibovici, L. Prophylaxis of Pneumocystis pneumonia in immunocompromised non-HIV-infected patients: systematic review and meta-analysis of randomized controlled trials. Mayo Clin Proc 82, 1052–1059, https://doi.org/10.4065/82.9.1052 (2007).
Bollee, G. et al. Clinical picture of Pneumocystis jiroveci pneumonia in cancer patients. Chest 132, 1305–1310, https://doi.org/10.1378/chest.07-0223 (2007).
National Comprehensive Cancer Network (NCCN). Non-small cell lung cancer guidelines Available at, (http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#nscl) (2015).
National Comprehensive Cancer Network (NCCN). Small cell lung cancer guidelines Available at, (http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#nscl) (2015).
Alanio, A. et al. Real-time PCR assay-based strategy for differentiation between active Pneumocystis jirovecii pneumonia and colonization in immunocompromised patients. Clin Microbiol Infect 17, 1531–1537, https://doi.org/10.1111/j.1469-0691.2010.03400.x (2011).
Azoulay, E. et al. Polymerase chain reaction for diagnosing pneumocystis pneumonia in non-HIV immunocompromised patients with pulmonary infiltrates. Chest 135, 655–661, https://doi.org/10.1378/chest.08-1309 (2009).
Overgaard, U. M. & Helweg-Larsen, J. Pneumocystis jiroveci pneumonia (PCP) in HIV-1-negative patients: a retrospective study 2002–2004. Scand J Infect Dis 39, 589–595, https://doi.org/10.1080/00365540601150497 (2007).
Roblot, F. et al. Pneumocystis jirovecii pneumonia in HIV-negative patients: a prospective study with focus on immunosuppressive drugs and markers of immune impairment. Scand J Infect Dis 46, 210–214, https://doi.org/10.3109/00365548.2013.865142 (2014).
Pareja, J. G., Garland, R. & Koziel, H. Use of adjunctive corticosteroids in severe adult non-HIV Pneumocystis carinii pneumonia. Chest 113, 1215–1224 (1998).
Bozzette, S. A. et al. A controlled trial of early adjunctive treatment with corticosteroids for Pneumocystis carinii pneumonia in the acquired immunodeficiency syndrome. California Collaborative Treatment Group. N Engl J Med 323, 1451–1457, https://doi.org/10.1056/nejm199011223232104 (1990).
Zhang, X. J. et al. Prediction of radiation pneumonitis in lung cancer patients: a systematic review. J Cancer Res Clin Oncol 138, 2103–2116, https://doi.org/10.1007/s00432-012-1284-1 (2012).
Abid, S. H., Malhotra, V. & Perry, M. C. Radiation-induced and chemotherapy-induced pulmonary injury. Curr Opin Oncol 13, 242–248 (2001).
Baker, S. & Fairchild, A. Radiation-induced esophagitis in lung cancer. Lung Cancer (Auckl) 7, 119–127, https://doi.org/10.2147/lctt.s96443 (2016).
International Agency for Research on Cancer. Lung Cancer Estimated Incidence, Mortality and Prevalence Worldwide in 2012 Available at, http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx (2013).
Azoulay, E. et al. Acute respiratory distress syndrome in patients with malignancies. Intensive Care Med 40, 1106–1114, https://doi.org/10.1007/s00134-014-3354-0 (2014).
Teh, B. W. et al. Molecular diagnosis of Pneumocystis jirovecii in patients with malignancy: clinical significance of quantitative polymerase chain reaction. Med Mycol 52, 427–432, https://doi.org/10.1093/mmy/myt020 (2014).
Lingaratnam, S. M. et al. Pneumocystis jirovecii pneumonia associated with gemcitabine chemotherapy: experience at an Australian center and recommendations for targeted prophylaxis. Leuk Lymphoma 56, 157–162, https://doi.org/10.3109/10428194.2014.911861 (2015).
Worth, L. J. et al. An analysis of the utilisation of chemoprophylaxis against Pneumocystis jirovecii pneumonia in patients with malignancy receiving corticosteroid therapy at a cancer hospital. Br J Cancer 92, 867–872, https://doi.org/10.1038/sj.bjc.6602412 (2005).
Yale, S. H. & Limper, A. H. Pneumocystis carinii pneumonia in patients without acquired immunodeficiency syndrome: associated illness and prior corticosteroid therapy. Mayo Clin Proc 71, 5–13 (1996).
Sepkowitz, K. A. Pneumocystis carinii pneumonia in patients without AIDS. Clin Infect Dis 17(Suppl 2), S416–422 (1993).
Mathew, B. S. & Grossman, S. A. Pneumocystis carinii pneumonia prophylaxis in HIV negative patients with primary CNS lymphoma. Cancer Treat Rev 29, 105–119 (2003).
Obeid, K. M. et al. Risk factors for Pneumocystis jirovecii pneumonia in patients with lymphoproliferative disorders. Clin Lymphoma Myeloma Leuk 12, 66–69, https://doi.org/10.1016/j.clml.2011.07.006 (2012).
Mansharamani, N. G., Balachandran, D., Vernovsky, I., Garland, R. & Koziel, H. Peripheral blood CD4+ T-lymphocyte counts during Pneumocystis carinii pneumonia in immunocompromised patients without HIV infection. Chest 118, 712–720 (2000).
Kaplan, J. E. et al. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep 58, 1–207; quiz CE201-204 (2009).
Nuesch, R., Bellini, C. & Zimmerli, W. Pneumocystis carinii pneumonia in human immunodeficiency virus (HIV)-positive and HIV-negative immunocompromised patients. Clin Infect Dis 29, 1519–1523, https://doi.org/10.1086/313534 (1999).
Rouyer, M., Stoclin, A. & Blanc, F. X. Pneumocystis pneumonia in HIV-negative adults. Rev Mal Respir 32, 985–990, https://doi.org/10.1016/j.rmr.2015.06.007 (2015).
Zahar, J. R. et al. Pneumocystis carinii pneumonia in critically ill patients with malignancy: a descriptive study. Clin Infect Dis 35, 929–934, https://doi.org/10.1086/342338 (2002).
Limper, A. H. et al. An official American Thoracic Society statement: Treatment of fungal infections in adult pulmonary and critical care patients. Am J Respir Crit Care Med 183, 96–128, https://doi.org/10.1164/rccm.2008-740ST (2011).
Cregan, P. et al. Comparison of four methods for rapid detection of Pneumocystis carinii in respiratory specimens. J Clin Microbiol 28, 2432–2436 (1990).
Limper, A. H. Alveolar macrophage and glycoprotein responses to Pneumocystis carinii. Semin Respir Infect 13, 339–347 (1998).
Lu, Y. et al. PCR diagnosis of Pneumocystis pneumonia: a bivariate meta-analysis. J Clin Microbiol 49, 4361–4363, https://doi.org/10.1128/jcm.06066-11 (2011).
Jiancheng, W. et al. Screening Pneumocystis carinii pneumonia in non-HIV-infected immunocompromised patients using polymerase chain reaction. Diagn Microbiol Infect Dis 64, 396–401, https://doi.org/10.1016/j.diagmicrobio.2009.04.009 (2009).
Wilson, J. W. et al. Pneumocystis jirovecii testing by real-time polymerase chain reaction and direct examination among immunocompetent and immunosuppressed patient groups and correlation to disease specificity. Diagn Microbiol Infect Dis 69, 145–152, https://doi.org/10.1016/j.diagmicrobio.2010.10.021 (2011).
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
E.H.L. and M.S.P. are responsible for the conception and design, the development of methodology, analysis and interpretation, and writing, review, and revision of the manuscript. Y.H.R. carried out the statistical analyses. E.Y.K., S.H.L., A.Y.L., J.H.S., S.Y.K., K.S.C., J.Y.J., Y.A.K., Y.S.K., J.C. contributed to the study concept and design, and acquisition, analysis, and interpretation of the data; All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, E.H., Kim, E.Y., Lee, S.H. et al. Risk factors and clinical characteristics of Pneumocystis jirovecii pneumonia in lung cancer. Sci Rep 9, 2094 (2019). https://doi.org/10.1038/s41598-019-38618-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-38618-3
- Springer Nature Limited