Abstract
Few studies have focused on frailty as a predictor of mortality and readmission among inpatients in the acute care setting, especially over long follow-up periods. We conducted this study to determine the impact of the frailty on subsequent mortality and readmission in this setting. This study was a prospective observational study conducted in the acute geriatric wards, with a three-year follow-up duration. We assessed frailty via the 36-item Frailty Index (FI), and a cut-off value of 0.25 was used to identify the presence or absence of frailty. We collected survival and readmission information through telephone interviews at 12, 24, and 36 months. We used the Cox regression model to examine the association between frailty and outcomes interested (death and readmission). The present study included 271 patients (mean age: 81.1 years old; 20.3% females), of whom 21.4% died during the 3-year follow-up period. One hundred and thirty-three patients (49.1%) were identified as being frail. The prevalence of frailty was similar in men and women (46.8% vs.58.2%, P = 0.130). Compared with non-frail patients, death and hospital readmission rates of frail patients were increased. Frailty was an independent predictor of 3-year death (adjusted hazard ratio (HR): 2.09; 95% confidence interval (CI): 1.20 to 3.63) and readmission (adjusted HR: 1.40; 95% CI: 1.04 to 1.88) after adjusting for several potential confounders. Frailty is prevalent among older inpatients and is a valuable predictor of 3-year mortality and hospital readmission in an acute care setting.
Similar content being viewed by others
Introduction
Frailty is defined as a geriatric syndrome or state, which is marked by increased vulnerability to even small stressors and decreased physiological reserve in old people1,2,3. The prevalence of frailty varies from 4.0–59.1% among community-dwelling older individuals4 and 19.0–75.6% nursing homes5, with high estimate variability stemming from differences between the assessment tools and the characteristics of populations in a given study. Previous studies that have specifically focused on the prevalence of frailty in acute care settings have estimated it to affect 33.5–68.5% (median) of older patients in this context6,7,8.
Numerous studies have conclusively demonstrated that frailty is a predictor for many adverse health outcomes, including disability, falls, delirium, hospitalization, and mortality up to 12 years follow up period6,9,10,11,12,13,14. However, the majority of these previous studies have focused on the association between frailty and mortality among community-dwelling older persons9,10,11 or residents in long-term care settings12,15, rather than on those in acute care settings.
Studies regarding the role of frailty in predicting adverse events in acute care settings have begun to emerge, as they can help formulate patient care plans and improve shared decision making regardless of how frailty is defined8,16,17,18,19,20. Of these studies, the most commonly used frailty assessment tools were the Frailty Index, the Clinical Frailty Scale, and the Fried Frailty Phenotype8. Recently, a large cohort study developed a hospital frailty risk score based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) diagnostic codes and found frailty was significantly associated with 30-day mortality (odds ratio: 1.71, 95% CI: 1.68 to 1.75) and 30-day readmission (1.48, 1.46 to 1.50)21. This hospital frailty risk score showed moderate agreement with the Frailty Index (Pearson’s correlation coefficient 0.41). These studies have thus demonstrated that frailty is an important prognostic factor when it comes to predicting adverse health outcomes in older patients in acute care settings. Notably, follow-up periods in these past studies have varied widely from 30 days to 12 months.
The value of frailty as a predictor longer-term adverse events has to date remained unclear in acute care settings. Furthermore, there are still some contradictory results with regard to how well frailty in predictive of readmission in such settings22,23,24,25 and data from non-Caucasian inpatient populations are scarce. Therefore, we designed this study to examine the prevalence of frailty as defined by frailty index in a Chinse patients of older inpatients in an acute care setting and to explore the value of frailty as a predictor of mortality and readmission for this population over a long-term (3-year) follow-up period.
Methods
Study design and patients
This study was a prospective observational study conducted in the Center of Gerontology and Geriatrics, West China Hospital, Sichuan University. All patients who were admitted to the ward in 2012 and provided formal consent were considered for inclusion in our study. We excluded those patients with severe disease because they did not complete the questionnaire or functional assessments required for this study. Trained volunteers (medical students) collected health-related variables using a pre-designed general questionnaire through face-to-face interviews within 48 hours of admission. We assessed the health-related and functional variables based on the status at admission. Before data collection, research staff trained all volunteers using investigation manuals, videos, and simulated patients. All volunteers passed a training test before participating in the formal investigation. We performed all methods in accordance with the relevant guidelines and regulations in the present study.
Frailty assessment
In the present study, we constructed a frailty index (FI) using 36 health-related deficits/variables, according to a standard procedure26. All considered variables consisted of acute and chronic diseases present as diagnosed by an attending physician within 48 hours of admission (n = 12), sarcopenia assessed by research team according to the guidelines of the modified Asia Working Group for Sarcopenia (32), 14 items in Activities of Daily Living (ADL) or Instrumental ADL (IADL) items, and 9 symptoms including psychological and memory complaints. For binary variables, results were coded with a value of “1” indicating that the variable present and “0” indicating it was absent. For variables (ADL and IADL items) with 3 possible values, intermediate responses were coded as “0.5”. We did not include the BMI as a part of the frailty index in this study for the cutoff of BMI was inconsistent among Chinese people27,28,29. All items in the FI did not have missing data and were showed in Table 1. For each old individual, we calculated the FI as the sum of all score of present deficits divided by the total number of considered deficits (n = 36). Theoretically, the FI would be ranging between 0 and 1 as a continuous score. We chose 0.25 as cut-off point of the FI according to previous studies12,30,31,32,33,34.
Mortality and readmission information
We obtained mortality and readmission information for all patients through telephone interviews conducted at 12, 24, and 36 months from the baseline by trained research volunteers. We also confirmed the survival information based on records in the Death Registry of Sichuan province with the approval of local government. We recorded the death dates of patients who died during the follow-up period. For those patients who did not die during the follow-up period, we recorded the date of the last follow-up. For patients who were readmitted to the hospital more than one time during follow-up, we record the first date of readmission.
Co-variables
To assess the influence of variables not encoded directly in the frailty index, we also collected the following variables from the medical records systems and face-to-face interviews for each patient: age, sex, body mass index (BMI) as calculated by the body weight (Kg) divided by the square of the body height (m), systolic and diastolic blood pressure (SBP and DBP), education levels (illiteracy, primary school, secondary school, or advanced), previous occupations (intellectual work, light physical labor, heavy physical labor), living status (living alone or not), marriage status (married and living with spouse or not), lifestyle factors (smoking and alcohol consumption status).
Statistical analyses
All statistical analyses were performed using the SPSS Statistics for Windows, Version 17.0. Chicago: SPSS Inc., with P-values of <0.05 (two-tailed) indicating the presence of a statistically significant difference between the two groups. We presented the baseline characteristics of the patients by the frailty status (frailty and no frailty). We presented continuous variables and categorical variables as means ± standard deviations or numbers and proportions, respectively. We tested the differences between frailty and no frailty groups using independent Student’s t-tests or Chi-squared tests according to the types of variables. We used the Spearman correlation to assess the relationships between frailty index and age. We used the Cox regression models to estimate the hazard ratio (HR) and its 95% confidence interval (CI) of the frailty status as an independent variable in functions of increased risk of mortality and readmission. In adjusted model 1, we adjusted the general variables (age, sex, and education). In adjusted model 2, we adjusted several other potential confounders (P < 0.2, co-variables when compared among frailty and no frailty groups). We used the Kaplan–Meier method to plot the cumulative risk curves for death and readmission, and the differences between these curves were examined using the log-rank test.
Ethics
Research Ethics Committee in Sichuan University approved the performance of the study. We also obtained written informed consent all patients or their legal proxies before the study began.
Results
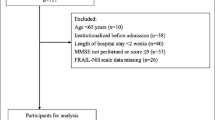
The characteristics of the study patients
A total of 313 patients agreed to participate in this study. We excluded 25 subjects due to severe disease because they did not complete the questionnaire or functional assessments required for this study. A total of 17 patients were lost due to failure to follow-up. We included 271 inpatients (55, 20.3% females) in the present study. The age of the patients ranging from 60 to 101 (mean: 81.1 ± 6.6 years). The maximum of FI is 0.69. The mean (standard deviation) and median FI scores of the patients were 0.26 (0.16) and 0.22, respectively. The 99th percentile of FI in this sample was 0.68. The FI follows an approximately normal distribution (Skewness = 0.671, standard error = 0.148; Kurtosis = −0.208, standard error = 0.295) and was positively related to age (r = 0.26, P < 0.001). According to the FI cutoff (0.25), 133 (49.1%) patients were identified as being frail.
The percentage of frailty was similar in females and males (58.2% vs. 46.8%, X2 = 2.289, p = 0.130). Female had similar FI scores to those of male (0.28 ± 0.15 vs. 0.26 ± 0.16; t = −0.71, P = 0.479). Frail patients were older compared to non-frail patients (79.3 ± 7.6 vs. 82.8 ± 4.9; t = 4.48, p < 0.001). The frequency of married and live with spouse was lower in frail patients than in non-frail patients (67.7% vs. 79.7%, X2 = 5.08, P = 0.024). Table 2 shows the characteristics of the study patients by their frailty status (frailty or no frailty).
The relationship between frailty and all-cause mortality
Compared with non-frail patients, 3-year death rates of frail patients were significantly increased (28.6% vs. 14.5%, X2 = 7.98, P = 0.005). Table 3 shows the results of Cox regression models for frailty status, as a function of increased risk of death. Compared to the no frailty group, frail patients had a higher risk of death (hazard ratio: 2.18, 95% confidence interval (1.27 to 3.74), P = 0.005) than those who were not frail. After adjustment for age, sex, education levels, BMI, marital status, and alcohol intake, the model was stable and also found that frail subjects had a higher risk of death compared to the no frailty group (hazard ratio: 2.09, 95% confidence interval (1.20 to 3.63), P = 0.009). Figure 1 shows the cumulative risk curves for the death of the study patients by their frailty status at baseline, and these two curves differ significantly in the two groups (Log-rank P = 0.004).
The relationship between frailty and readmission
Compared with non-frail patients, readmission rates of frail patients were significantly increased (73.7% vs. 61.6%, X2 = 4.51, P = 0.034). Table 3 shows the results of Cox regression models for frailty status, as a function of increased risk of readmission. Compared to the patients without frailty, frail patients had a higher risk of readmission (hazard ratio: 1.45, 95% confidence interval (1.08 to 1.94), P = 0.013) than non-frail patients. After adjustment for age, sex, education levels, BMI, marital status, and alcohol intake, the model was stable and also found that frail subjects had a higher risk of readmission as compared to the no frailty group (hazard ratio: 1.40, 95% confidence interval (1.04 to 1.88), P = 0.026). Figure 2 shows the cumulative risk curves for readmission of the study patients according to their frailty status at baseline, and these two curves differ significantly in the two groups (Log-rank P = 0.011).
Discussion
In this study, we explored the prevalence of frailty and explored the relationship between frailty, mortality, and readmission in a population of older Chinse inpatients in an acute care setting. To the best of our knowledge, this is the first study to investigate the relationship between frailty, mortality, and readmission longitudinally in Chinese hospitalized older patients with a long-term (3-year) follow up duration. The present study showed that frailty was prevalent (49.1%) among older Chinese inpatients in acute geriatric wards. Frailty, as assessed by the Frailty Index, is a useful predictor of long-term death and readmission. This evidence indicates that we should consider frailty status when formulating health care plans for older inpatients.
A previous study with a large sample size (34,123 respondents) found that China has the lowest frailty prevalence than other countries (Ghana, India, Mexico, Russia and South Africa) among community-dwelling older persons35,36. The present study showed that the prevalence of frailty (49.1%) was similar to that identified by previous studies conducted in acute care settings in western countries (Europe, North America, Australia or New Zealand, 48.5%)8. Li and colleges previously used the FRAIL scale to define frailty and found that only 15.1% of patients with chronic diabetes in a geriatric ward met these criteria for frailty37. In our study, we chose a commonly used frailty index cut-off value (0.25) to define frailty in patients with acute conditions. This assessment methodology did influence the prevalence of frailty, potentially leading to a higher prevalence based on this definition for the FI captured more health-related information than FRAIL scale. The prevalence of frailty has varied massively in previous studies, ranging from 1.1–100% in studies conducted in western countries in acute care settings8. While it is difficult to compare frailty prevalence between studies due to variations in diagnostic methodology, our results suggest that unlike in community-dwelling older adults, older Chinese patients with acute illnesses have a similar prevalence of frailty as do those in other countries.
Some studies have suggested that frailty cannot be used as a predictor of readmission for those older patients with cirrhosis23 or idiopathic Parkinson’s disease38. In the two previous studies23,38, they recruited different patients and used different scales to define frailty with our present study. The reasons for these inconsistencies of the results were unclear and should be further investigated. Consistent with previous studies6,7,20,21,22,24,25,39,40, we found frailty to be a prognostic factor for mortality and readmission, independent of age, sex, and other potential confounders. Recently, Cesari and colleagues enrolled 4,488 patients aged 65 and older in 116 hospital wards in Italy between 2010 and 2016 and found that their 34-item frailty index was significantly predictive of 12-month mortality (HR 1.46, 95% CI 1.32–1.62) and in-hospital mortality after adjustment for age and sex39. Vidan and colleagues included 450 patients aged 79 and older and found frailty to be an independent predictor of 12-month readmission40. Our study extends these conclusions to a Chinese population and employs a more extended follow-up period (3 years).
There are certain limitations to our present study. First, we constructed our frailty index without using the same variables (70-item) employed in its original development study41. However, we constructed our frailty index according to a standard procedure and following the required criteria for variables selection26. Furthermore, the frailty index with 30 or more items have been shown to sufficiently capture frailty status and to be accurate for predicting adverse events, suggesting that our 36-item frailty index was sufficiently powerful26. We used 0.25 as the cut-off value for our frailty. This value has exhibited the strongest potential to predict adverse outcomes and is consistent with the results of the Fried Frailty phenotype and FRAIL scale32,33,34. Second, the number of patients in our study was smaller than many previous studies (n = 271), and we excluded patients with severe disease, which may have introduced a selection bias and thereby underestimated the prevalence of frailty. The small number of patients also limited our ability to perform subgroup analyses according to sex, different frailty levels and set more FI cut-off points. In addition, the small sample size may be the main reason for a wide 95% CI when we put FI in the Cox regression model as a continuous score. Third, we only included Chinese people (Han) in this study. Thus, we cannot extend the present conclusion to other ethnic groups or to other countries with medical care models distinct from those in China. Fourth, there were many pieces of missing data with regard to other potential confounders, such as income and physical activity levels, limiting our ability to adjust the model in light of these potential confounders. Additionally, the exposure of the studied patients to physiotherapy intervention during the ward stay as another possible confounder in the present study. Finally, the mean age of the patients in this study was 81 years. For such an old cohort, it is important to consider that a survival bias may be present when applying these findings.
Conclusions
Frailty (as assessed by frailty index) is a prevalent state among older inpatients and is valuable as a predictor of 3-year mortality and hospital readmission in acute care settings. Given the limitations of our study, prospective studies with larger sample sizes using other frailty assessment methods and conducted in other acute care settings are warranted to confirm these findings.
References
Clegg, A., Young, J., Iliffe, S., Rikkert, M. O. & Rockwood, K. Frailty in elderly people. Lancet 381, 752–762, https://doi.org/10.1016/S0140-6736(12)62167-9 (2013).
Fried, L. P. et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56, M146–156 (2001).
Fried, L. P., Ferrucci, L., Darer, J., Williamson, J. D. & Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 59, 255–263 (2004).
Collard, R. M., Boter, H., Schoevers, R. A. & Oude Voshaar, R. C. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 60, 1487–1492, https://doi.org/10.1111/j.1532-5415.2012.04054.x (2012).
Kojima, G. Prevalence of Frailty in Nursing Homes: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc 16, 940–945, https://doi.org/10.1016/j.jamda.2015.06.025 (2015).
Joosten, E., Demuynck, M., Detroyer, E. & Milisen, K. Prevalence of frailty and its ability to predict in hospital delirium, falls, and 6-month mortality in hospitalized older patients. BMC Geriatr 14, 1, https://doi.org/10.1186/1471-2318-14-1 (2014).
Vu, H. T. T. et al. Prevalence of frailty and its associated factors in older hospitalised patients in Vietnam. BMC Geriatr 17, 216, https://doi.org/10.1186/s12877-017-0609-y (2017).
Theou, O. et al. What do we know about frailty in the acute care setting? A scoping review. BMC Geriatr 18, 139, https://doi.org/10.1186/s12877-018-0823-2 (2018).
Shamliyan, T., Talley, K. M., Ramakrishnan, R. & Kane, R. L. Association of frailty with survival: a systematic literature review. Ageing Res Rev 12, 719–736, https://doi.org/10.1016/j.arr.2012.03.001 (2013).
Kojima, G. Frailty as a predictor of hospitalisation among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health 70, 722–729, https://doi.org/10.1136/jech-2015-206978 (2016).
Vermeiren, S. et al. Frailty and the Prediction of Negative Health Outcomes: A Meta-Analysis. J Am Med Dir Assoc 17, 1163 e1161–1163 e1117, https://doi.org/10.1016/j.jamda.2016.09.010 (2016).
Tabue-Teguo, M. et al. Frailty Index and Mortality in Nursing Home Residents in France: Results From the INCUR Study. J Am Med Dir Assoc 16, 603–606, https://doi.org/10.1016/j.jamda.2015.02.002 (2015).
Kojima, G. Frailty as a Predictor of Future Falls Among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc 16, 1027–1033, https://doi.org/10.1016/j.jamda.2015.06.018 (2015).
Kojima, G. Frailty Defined by FRAIL Scale as a Predictor of Mortality: A Systematic Review and Meta-analysis. J Am Med Dir Assoc 19, 480–483, https://doi.org/10.1016/j.jamda.2018.04.006 (2018).
Theou, O. et al. Frailty, Hospitalization, and Mortality in Residential Aged Care. J Gerontol A Biol Sci Med Sci 73, 1090–1096, https://doi.org/10.1093/gerona/glx185 (2018).
Scherer, J. S. & Swidler, M. A. Decision-making in patients with cancer and kidney disease. Adv Chronic Kidney Dis 21, 72–80, https://doi.org/10.1053/j.ackd.2013.07.005 (2014).
Tang, V. L. & Covinsky, K. Frailty and Surgical Decision Making. Ann Intern Med 165, 669–670, https://doi.org/10.7326/M16-1866 (2016).
Ethun, C. G. et al. Frailty and cancer: Implications for oncology surgery, medical oncology, and radiation oncology. CA Cancer J Clin 67, 362–377, https://doi.org/10.3322/caac.21406 (2017).
Kojima, G., Iliffe, S. & Walters, K. Frailty index as a predictor of mortality: a systematic review and meta-analysis. Age Ageing 47, 193–200, https://doi.org/10.1093/ageing/afx162 (2018).
Lin, S. M. et al. Comparison of 3 Frailty Instruments in a Geriatric Acute Care Setting in a Low-Middle Income Country. J Am Med Dir Assoc 19, 310–314 e313, https://doi.org/10.1016/j.jamda.2017.10.017 (2018).
Gilbert, T. et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet 391, 1775–1782, https://doi.org/10.1016/S0140-6736(18)30668-8 (2018).
Kahlon, S. et al. Association between frailty and 30-day outcomes after discharge from hospital. CMAJ 187, 799–804, https://doi.org/10.1503/cmaj.150100 (2015).
Tapper, E. B., Finkelstein, D., Mittleman, M. A., Piatkowski, G. & Lai, M. Standard assessments of frailty are validated predictors of mortality in hospitalized patients with cirrhosis. Hepatology 62, 584–590, https://doi.org/10.1002/hep.27830 (2015).
Li, Y. et al. Impact of frailty on outcomes after discharge in older surgical patients: a prospective cohort study. CMAJ 190, E184–E190, https://doi.org/10.1503/cmaj.161403 (2018).
Mathew, S. A., Gane, E., Heesch, K. C. & McPhail, S. M. Risk factors for hospital re-presentation among older adults following fragility fractures: a systematic review and meta-analysis. BMC Med 14, 136, https://doi.org/10.1186/s12916-016-0671-x (2016).
Searle, S. D., Mitnitski, A., Gahbauer, E. A., Gill, T. M. & Rockwood, K. A standard procedure for creating a frailty index. BMC Geriatr 8, 24, https://doi.org/10.1186/1471-2318-8-24 (2008).
Gu, Z. et al. Body mass index, waist circumference, and waist-to-height ratio for prediction of multiple metabolic risk factors in Chinese elderly population. Sci Rep 8, 385, https://doi.org/10.1038/s41598-017-18854-1 (2018).
Wang, F., Chen, Y., Chang, Y., Sun, G. & Sun, Y. New anthropometric indices or old ones: which perform better in estimating cardiovascular risks in Chinese adults. BMC Cardiovasc Disord 18, 14, https://doi.org/10.1186/s12872-018-0754-z (2018).
Zhang, J., Zhu, W., Qiu, L., Huang, L. & Fang, L. Sex- and Age-Specific Optimal Anthropometric Indices as Screening Tools for Metabolic Syndrome in Chinese Adults. Int J Endocrinol 2018, 1067603, https://doi.org/10.1155/2018/1067603 (2018).
Liu, Z. Y. et al. Association between serum beta2-microglobulin levels and frailty in an elderly Chinese population: results from RuLAS. Clin Interv Aging 12, 1725–1729, https://doi.org/10.2147/CIA.S142507 (2017).
Liao, Q., Zheng, Z., Xiu, S. & Chan, P. Waist circumference is a better predictor of risk for frailty than BMI in the community-dwelling elderly in Beijing. Aging Clin Exp Res, https://doi.org/10.1007/s40520-018-0933-x (2018).
Malmstrom, T. K., Miller, D. K. & Morley, J. E. A comparison of four frailty models. J Am Geriatr Soc 62, 721–726, https://doi.org/10.1111/jgs.12735 (2014).
Theou, O., Brothers, T. D., Mitnitski, A. & Rockwood, K. Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. J Am Geriatr Soc 61, 1537–1551, https://doi.org/10.1111/jgs.12420 (2013).
Rockwood, K., Andrew, M. & Mitnitski, A. A comparison of two approaches to measuring frailty in elderly people. J Gerontol A Biol Sci Med Sci 62, 738–743 (2007).
Biritwum, R. B. et al. Prevalence of and factors associated with frailty and disability in older adults from China, Ghana, India, Mexico, Russia and South Africa. Maturitas 91, 8–18, https://doi.org/10.1016/j.maturitas.2016.05.012 (2016).
Siriwardhana, D. D., Hardoon, S., Rait, G., Weerasinghe, M. C. & Walters, K. R. Prevalence of frailty and prefrailty among community-dwelling older adults in low-income and middle-income countries: a systematic review and meta-analysis. BMJ Open 8, e018195, https://doi.org/10.1136/bmjopen-2017-018195 (2018).
Li, Y. et al. A Pilot Study of the FRAIL Scale on Predicting Outcomes in Chinese Elderly People With Type 2 Diabetes. J Am Med Dir Assoc 16, 714 e717–714 e712, https://doi.org/10.1016/j.jamda.2015.05.019 (2015).
Torsney, K. M. & Romero-Ortuno, R. The Clinical Frailty Scale predicts inpatient mortality in older hospitalised patients with idiopathic Parkinson’s disease. J R Coll Physicians Edinb 48, 103–107, https://doi.org/10.4997/JRCPE.2018.201 (2018).
Cesari, M. et al. Implementation of the Frailty Index in hospitalized older patients: Results from the REPOSI register. Eur J Intern Med, https://doi.org/10.1016/j.ejim.2018.06.001 (2018).
Vidan, M. T. et al. Prevalence and prognostic impact of frailty and its components in non-dependent elderly patients with heart failure. Eur J Heart Fail 18, 869–875, https://doi.org/10.1002/ejhf.518 (2016).
Rockwood, K. et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 173, 489–495, https://doi.org/10.1503/cmaj.050051 (2005).
Acknowledgements
The authors would like to thank all volunteers that worked on this study, the staff of the Center of Gerontology and Geriatrics in West China Hospital, Sichuan University, and all patients and their legal proxies for their cooperation in the present study. The present study was co-funded by the “National Natural Science Foundation of China” (No. 81601220) and the “Project of Science and Technology Bureau of China and Sichuan Province” (2017RZ0040 and 2017YFC0840101) and the “Science Foundation for Young Researchers of Sichuan University” (2017SCU11044). These funding agencies did not have a role in the study implementation.
Author information
Authors and Affiliations
Contributions
Qiukui Hao (Q.H.) conducted the data analysis and drafted the initial manuscript. Lixing Zhou (L.Z.), Ming Yang (M.Y.) and Biao Dong (B.D.) help with results interpretation and give critical comments for the manuscript. Birong Dong (B.R.D.) and Yuquan Wei (Y.Q.W.) secured funding for data collection and verified the analysis outcomes.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hao, Q., Zhou, L., Dong, B. et al. The role of frailty in predicting mortality and readmission in older adults in acute care wards: a prospective study. Sci Rep 9, 1207 (2019). https://doi.org/10.1038/s41598-018-38072-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-38072-7
- Springer Nature Limited
This article is cited by
-
The hospital frailty risk score as a predictor of readmission after ERCP
Surgical Endoscopy (2024)
-
Acute care models for older people living with frailty: a systematic review and taxonomy
BMC Geriatrics (2023)
-
Prediction of adverse health outcomes using an electronic frailty index among nonfrail and prefrail community elders
BMC Geriatrics (2023)
-
Network analysis of frailty indicators in hospitalized elderly patients: unveiling the role of depression and hemoglobin as core factors
Aging Clinical and Experimental Research (2023)
-
Associations of social isolation, social participation, and loneliness with frailty in older adults in Singapore: a panel data analysis
BMC Geriatrics (2022)