Abstract
The constantly evolving and growing global health crisis, antimicrobial resistance (AMR), endangers progress in medicine, food production, and life expectancy. Limited data on population-level prevalence, including seasonal and temporal variations, hampers accurate risk assessment for AMR transmission, despite its paramount importance on both global and national fronts. In this study, we used quantitative real-time PCR (q-PCR) to analyze 123 antibiotic resistance genes (ARGs) and 13 mobile genetic elements (MGEs) in wastewater of a selected urban community. Sampling was conducted monthly over a 5-month period (December 2021–April 2022) to assess resistance diversity, temporal dynamics, co-abundance of ARGs, MGEs, and resistance mechanisms. Approximately 50% of the tested ARG subtypes were consistently detected in all months, with frequency ranging from 52 to 61% with maximum absolute abundance in the winter months (December and January). In co-abundance analysis, specific genes were clustered into modules, highlighting shared distribution patterns and functional associations among the ARGs and MGEs. Detected clinically significant genes (ndm-1 and cfiA) and other variants (blaoxy, aph, aacC, tet-35, tet M, tet-32) are capable of imparting resistance to 3rd and 4th generation (gen) β-lactam, aminoglycoside, tetracycline, and multidrug classes. These contribute significantly to core/persistent resistance. This study deepens our comprehension of temporal/seasonal fluctuations in ARG and MGE distribution, providing valuable evidence to guide AMR control policies and promote responsible antibiotic/antimicrobial use for preserving effectiveness.
Similar content being viewed by others
Introduction
As one of the top ten human health threats, AMR is anticipated to increase fatalities in the coming years, adversely affecting both the ecosystem and economy1,2,3. Human activities, such as antibiotic consumption and, discharge into the environment without proper treatment, have intensified the proliferation of antibiotic resistance (AR) in the environment4. The impact of these actions, coupled with insufficient data on resistance trends, particularly in densely populated areas, underscores the urgent necessity for enhanced urban resistance surveillance5. Such surveillance is crucial for defining resistance scope, developing interventions, and monitoring effectiveness in real-time to mitigate the spread of resistance. Studies have assessed the incidence of AR in urban systems, with a predominant emphasis on hospital discharges, riverine systems, and wastewater treatment plants (WWTPs)6,7,8,9. However, only a limited number of studies have addressed community-acquired resistance10,11. Furthermore, the temporal dynamics of resistance within urban locales, remain relatively underexplored and poorly understood11,12. Thus, it is imperative to conduct temporal studies across diverse geographical locations to ascertain the changes in resistance patterns with time. This is crucial as seasonal fluctuations exert a profound influence on antibiotic utilization, which fosters the proliferation of AR by the selection and spread of resistant bacteria13.
Aquatic systems (domestic wastewater, or sewage systems) influenced by both humans and animals have the potential ability to comprehend the dynamic infectious cycles of a diverse array of pathogens14,15. This also aids in the deeper understanding of the environmental landscape and sheds light on potential diseases that could arise in the times ahead10,16. From a surveillance standpoint, sewage offers a convenient way to sample a large population without the need for informed consent, addressing ethical concerns with minimal practical and logistical hurdles16,17. Specifically, sewage from urban communities is a viable option for monitoring purposes, propelled by the rise in the urban population and integration into sewer systems worldwide18. In addition, within the built environment, microbes have been implicated as potential sources of contagion, and the progression of certain conditions like allergies has been linked to escalating urbanization19.
Hence, our study employed a temporal strategy, utilizing sewage (wastewater-based epidemiology—WBE) to evaluate the prevalence, abundance, and dynamics of resistance in the chosen urban community over time. Culture-independent molecular method, quantitative real-time PCR (q-PCR) was employed (assessing 123 ARGs and 13 MGEs) to analyze the resistance, thereby enhancing accuracy, and minimizing false negatives. This non-intrusive sewage-based monitoring addresses AR in a One Health perspective, inasmuch the study site is intricately connected to all three aspects of it (human, animal, and environment). The integration of a One Health perspective enriches the study’s relevance, offering insights for community-oriented AR strategies, clinical decision-making, and early disease outbreak detection. This research bridges a crucial gap in understanding temporal resistance dynamics in urban environments, emphasizing the significance of ongoing surveillance in combating global antibiotic resistance. Moreover, understanding the site-specific distribution of distinct ARGs contributes to the comprehensive global atlas of AMR, encompassing its density, diversity, and dynamic profile.
Results and discussion
Diversity and abundance of ARGs
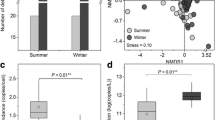
In our previous study conducted in this locale, 70% of the examined ARGs were positively detected. Nine out of 10 targeted ARG classes and 28 out of 52 antibiotics, were detected. Opportunistic pathogen such as Pseudomonas and human infection-causing microbe, Acinetobacter were also identified. This suggests the magnitude of resistance is quite high in the study site10. So, the current study was conducted in the same location to elucidate the temporal dynamics of ARGs. In this study, the intensity of resistance in the community was shown by the detection of resistance to 8 of the 9 major ARG classes tested (Table 1), which included β-lactams, tetracyclines, MLSBs, multidrugs, aminoglycosides, quinolones, sulfonamides, trimethoprims and chloramphenicols. Half of the targeted 123 ARG subtypes (genotypes) were detected in all the months, with detection frequency ranging from 52 to 61% (The Ct values of the analytical triplicates are presented in Supplementary Table 1). The number of genes detected varied from month-to-month, highest number found in March and the lowest number in December (March > February > April > January > December) (Table 1). Though the summer months (March and April) had the highest gene count (number of genes detected), winter exhibited the greatest absolute resistance. Throughout the 5 months, 49 genes are commonly detected termed as persistent /core resistance; many of these genes are from the β-lactam, followed by the multidrug, aminoglycosides, and MLSB classes (Fig. 1a and Supplementary Table 2). The absolute and relative abundance at the class level is represented in Fig. 1b (for class-level resistance, all detected gene copies were summed up within the class. Similarly, relative abundance (class level) was estimated by dividing the acquired absolute resistance by the number 16 S rRNA gene copies). The study area conferred maximum resistance to the aminoglycoside class followed by β-lactams, sulfonamides and trimethoprims. To classes of multidrug, MLSBs, and tetracycline, moderate resistance was observed. Resistance to chloramphenicols and quinolones classes was slightly lower and to vancomycin class resistance was not noticed. Wastewater characteristic parameters are presented in Supplementary Table 3.
This data demonstrate the degree of resistance in the community; yet, AR is intrinsic and pervasive in the environment, each ecosystem has a distinct set of dominant ARGs due to the influence of human activities, which enhances the diversity and complexity of ARGs occurrence20. ARGs prevalence has been reported in different urban aquatic systems where ~80% of the evaluated ARGs were identified21,22, which is slightly higher than our study site. As previously stated, anthropogenic activity, together with socioeconomic variables such as antibiotic usage, has major impact on ARGs prevalence; this explains the discrepancies in ARG incidence in the current study to previous reports16,23.
Resistance pattern
The absolute and relative abundance of ARGs is depicted in Fig. 2. Genes observed just once were eliminated, and those spotted in at least 4 months were shown in the heatmap (Supplementary Fig. 1 included absolute and relative abundance for all the tested genes).
Higher resistance
Aminoglycosides showed the highest resistance of all the classes that were found, with gene copies ranging from 9.47 × 104 to 6.94 × 104, with a mean of 7.92 × 104 copies/L. Resistance to β-lactam and sulfonamide and trimethoprim classes varied between 2.17 × 104 to 9.36 × 103 and 1.09 × 104 to 8.83 × 103 with an average of 1.42 × 104 and 9.79 × 103 copies/L, respectively. A total of 10 genes in the aminoglycoside class were targeted; 9 of them were found in the initial 2 months, 8 in 3rd, 7 in 4th and 5th months. The 3rd month had the highest number of genes detected (20) and the 5th month showed the lowest (15) of the targeted 23 genes in the β-lactam class. 18 (the second and fourth) genes were identified in 2 months and 16 in 1st month. In the sulfonamide and trimethoprim class, six genes were targeted; four of them were found in the 4 months and all five in the fifth. In all 5 months, the gene-level abundance of the classes of aminoglycoside, β-lactam, and sulfonamide and trimethoprim were dominated by aph, aadA1, strB, and aadA-02, blaOXY, fox5, blaCTXM-01, blaOXA-30, blaVEB, penA, dfrA, and sul2, respectively. The highest resistance to these classes in the study region is not unusual, owing to their detection over diverse aquatic habitats24,25. The genes of these groups like str, sul, blaOxy, and blaOXA are even considered as biomarkers for comprehending the dynamics of AR in the environment because of anthropogenic contamination26. Except aph and blaOXY, which are chromosomal encoded resistance genes, almost all genes of these classes are located on plasmids, integrons, transposons, and integrative conjugative elements27. As an outcome, the presence of these genes on MGEs accelerates the spread throughout bacterial populations via horizontal gene transfer (HGT). Furthermore, the phenomenon of cross-resistance is also responsible for the occurrence of these genes, as well as the genes associated with it, in greater concentrations. Given that, blaOXA gene is in the transposon (Tn21) between the aad gene (resistance) and its promoter, thus offering cross-resistance to other antibiotic classes such as aminoglycosides10.
Moderate resistance
The gene copies noted for the classes that impart moderate resistance, including multidrugs, MLSBs, and tetracyclines, were between 5.19 × 103 to 3.25 × 103, 4.66 × 103 to 1.94 × 103 and 3.20 × 103 to 2.07 × 103. The average absolute abundance of these classes is 4.47 × 103, 2.99 × 103 and 2.51 × 103, respectively. In the multidrug class, 15 genes were studied; all 15 genes were found in last 3 months, and 10, 13, and 12 genes during the initial 3 months. In the MLSBs class, 9 out of the 19 targeted genes were found in the 4th month and 8 genes in the reaming 4 months. Out of the targeted 21 genes in the tetracycline class, the highest number of genes found is only 13 (fourth) in 1st month, 9 genes were detected in the first 2 months and 11 (third) and 12 (fifth) genes in the next 2 months. The dominated genes of these three classes in the total study period are OprD, OprJ, mexF, acrA, acrR, mtrC, ere A, mefA, mphA, lnuB, ermT, tet PB, tet M, tetO, tetQ, tet (32), and tet(36).
Only the number of MDR genes in the moderately detected resistance classes is comparable with earlier studies in various urban aquatic systems21,28, whereas the abundance of MLSBs is greater and to tetracyclines is lower in contrast to other studies in urban environments25,29. Yet MLSBs are not found in urban contexts, they are frequently found in the effluents from livestock farms30. Their presence might be explained by the presence of neighboring animals and people in the study site. In addition, MLSBs are usually distributed on plasmids and transposons that allow them to spread quickly; this also explains their prevalence in the research region31. Regarding tetracyclines, the variations in tetracycline resistance indicate that biogeographical patterns of resistance may vary due to various ecological variables, such as environmental selection16.
Less resistance
The study area exhibited less resistance to chloramphenicols and quinolones, with mean gene copies of 1.98 × 103 and 5.33 × 102 correspondingly, with variations of 2.79 × 103 to 1.44 × 103 and 9.28 × 102 to 2.70 × 102. Out of the targeted eight genes in the quinolone class, five genes were found in the first month and six genes in the subsequent 4 months, whereas all the targeted 4 genes in the chloramphenicol class were found in the 5-month period. In these two classes, cmlA1, floR, oqxA, oqxB, qnr A, and qnr B are the dominant genes. Regardless of the less copy number, the number of tested to detected genes in the study site are more for both the chloramphenicols and quinolones classes (Table 1). CmlA1, a gene considered as a biomarker for antibiotic resistance in the environmental matrix, is one of the genes detected in high concentrations and is also more prevalent than the others studies32,33. The chloramphenicol class of resistance genes are all plasmid or transposon-encoded genes, and quinolone resistance genes act through quinolone resistance proteins34. This class of genes were often detected in wastewater and their existence on plasmids and transposons may have aided in their detection in the study area35,36.
Mobile genetic elements
The class-level and gene-level absolute and relative abundance of MGEs is represented in Figs. 1b and 3, respectively. In all 5 months, 11 MGEs were found in the 13 target MGE (5 integrons and 8 transposons), except intI2 in March and April. Integrons and transposons both reported gene copies ranging from 8.48 × 104 to 6.17 × 104 and 3.79 × 104 to 2.80 × 104 correspondingly. The mean gene copies for these two subtypes are 7.14 × 104 and 3.28 × 104. The gene-level dominance of the MGE group is by intI-1, intI-1(clinic), intI-1LC, tnpA-04, and tnpA-05. MGEs speed up the proliferation of ARGs in aquatic settings through HGT which is key mechanism for the extensive transmission of antibiotic resistance37. MGEs like intI-1, tnpA-04, and tnpA-05 are considered as anthropogenic contamination indicators since they contribute significantly in the spread of ARGs38. Many studies demonstrated that plasmids and class 1 integrons, co-localize with antibiotic resistance genes like sul 2, str B, and aadA39. The concurrent occurrence of both ARGs and MGEs with same frequency of detection pattern in the study site, adds to evidence of MGE’s role in ARG spread.
Co-abundance of ARGs and MGEs
ARGs and MGEs detected over a minimum period of 4 months were studied for the co-abundance (Fig. 4). The network has 71 nodes and 1660 edges, demonstrating a modularity of 0.248 and an average clustering coefficient of 0.701, signifying a modular structure. Based on the modularity, the network was divided into three modules (Module I, Module II, and Module III) with the largest, Module I, comprising 30 out of 71 nodes. The co-occurring ARG and MGE subtypes within each module are listed in Supplementary Table 4. lnuB, penA, mphA-02, cmlA1-01, mefA, blaVEB, str, oqxB 2, intI-1LC, and tetO-01 were the most densely connected nodes in Modules I, II, and III, serving as module hubs. Str, penA, dfrA, acrR-01, lnuB-01, tetO-01, cmlA1-01, oqxB 2, intI-1clinic, and IS613 emerge as highly interconnected as well as frequently detected genes within their respective classes. ARGs conferring resistance to the same antibiotics tended to cluster together within specific modules; for instance, MLSBs, tetracyclines, chloramphenicols, and MGEs in Module I, and β-lactam quinolones in Module II (Supplementary Table 4). This implies that they exhibited similar characteristics, such as distribution patterns or functional associations, indicating a shared fate. The categorization of a gene into a particular module is primarily determined by its functional role, interaction partners, and participation in specific biological processes, pathways, or functions40. Another plausible explanation for the abundance trends is that certain microbial taxa harbored these ARGs, and these taxa were found across various environments9.
Temporal variations in ARGs and MGEs
ARGs and MGEs variations are shown in the Fig. 5a, b. December, followed closely by January, exhibits the highest absolute abundance of ARGs overall (minimal disparity between these 2 months in terms of the cumulative sum of all ARG classes). During winter (Dec and Jan), robust resistance is observed to aminoglycoside, sulfonamide & trimethoprim, β-lactam, MLSB, and multidrug classes (Fig. 5b). In the subsequent month of February, resistance levels are moderate, while in the summer months (March and April), resistance reduced. The trend is reflected in the Tetracycline class, except for a minor peak observed in March. Chloramphenicol and Quinolone classes exhibit their highest detection in the winter month of January, maintaining consistent levels in February. In the summer months, detection levels for both classes declined. Moreover, MGE frequency exhibits a marked increase during winter months. There is a progressive decrease in MGE frequency from winter to summer, reflecting the pattern observed for ARGs in this study. This alignment in trends between MGEs and ARGs suggests a potential relationship or shared influencing factors governing their prevalence across seasons (Fig. 4).
In this study, ARGs were most abundant during the winter months, which aligns with findings from seasonal studies of aquatic habitats that also observed greater richness estimates in the winter41,42,43. Caucci et al. reported that the concentrations of ARGs in wastewater matched the temporal variations of outpatient antibiotic prescriptions in the city. Their 2-year evaluation on antibiotic prescriptions revealed that during the colder months, when temperatures dropped and infections by bacteria increased, there was a higher recommendation for antibiotics. Antibiotic consumption is a significant factor in the release of antibiotic-resistant bacteria into sewage through excretions. The selection of resistant bacteria can occur during or after antimicrobial therapy11. This finding provides an explanation for the observed strongest resistance in the winter months and its persistence until February in the study site. However, it is worth noting that other studies, such as those conducted by Jiao et al.33, and Zheng et al.9, have reported greater resistance during the summer. These studies attribute this finding to the more equitable distribution of microorganisms in the warmer season compared to the colder season, where bacterial activity is reduced44. The discrepancy between our research findings and these other studies can be attributed to the differences in climates. The average temperature recorded during the summer in those33 studies showing greater resistance is often like the average temperature reported during the winter in the present study site. Apart from temperature, other factors such as oxygen levels, organic carbon, and nitrogen can also influence the composition of the bacterial community45. Consequently, even minor environmental changes have the potential to impact specific taxa within the microbial community carrying ARGs, leading to fluctuations in ARG abundances. These variations in climate can result in diverse microbial dynamics, influencing the prevalence of ARGs and shaping the observed resistance patterns in various regions. In a related vein, the relationship between ARGs and MGEs identified in our study is supported by the findings of Lu and Zheng9,46. These studies reported a positive correlation between the detection patterns and incidence of ARGs and MGEs. The stress-induced SOS response, has been shown to enhance rates of genetic recombination and HGT by MGEs47. Interestingly, in the context of cold temperatures, it is suggested that they can promote the spread of ARGs by increasing cell competence and transformation, both of which are associated with the SOS response48. Therefore, these findings also imply that the cold/low temperatures in winter may be responsible for the high detection of MGEs and the associated ARGs at the study site.
Absolute vs relative abundance
The 16 S rRNA exhibited a similar pattern to the absolute abundance of ARGs and MGEs (Fig. 6). However, during the summer months, its copy number decreased significantly when compared with ARGs and MGEs. This substantial reduction in the 16 S rRNA copy number had an impact on the relative abundance of ARGs and MGEs, causing them to display an opposite trend compared to their absolute abundance. The Relative Standard Deviations (RSDs) of 16 S rRNA are higher compared to the absolute and relative abundances of ARGs and MGEs. This observation indicates that the number of bacteria is more prone to fluctuations than the resistance elements, providing evidence for the robust presence of resistance in the community. One more interesting observation in the study site is the detection of a greater number of ARGs (total ARGs detected in March is 76 and in December is 65) in summer months though the copy number of both 16 s r RNA and ARG is less in summer (Table 1). This observation can be attributed to the possibility that in March and April, although the copy number of bacteria reduced, which enabled the detection of other genes even in lower copy numbers due to the increased diversity of other bacterial species. This suggests that while December may have higher levels of 16 S rRNA gene copies, the bacterial community is less diverse, resulting in fewer detected genes related to antibiotic resistance. On the other hand, the more diverse bacterial community in March and April allows for the detection of a greater variety of genes, including those associated with antibiotic resistance, despite the reduced overall copy numbers of bacteria.
Persistence resistance and ARGs of emerging concern
The most concerning category for human health is defined as persistent resistance49, which refers to ARG subtypes present in all samples. This category includes 49 ARG subtypes (Fig. 1a and Supplementary Table 5) across 8 major types (Fig. 1a). The persistent resistance exhibits higher abundance compared to other ARGs within the same class (Fig. 2 and Supplementary Fig. 1). Specifically, it constitutes an average of 64–75% of the total ARG abundance. This aligns with earlier findings, where the core resistome represented an average of 70% of the total ARG abundance in the entire sample49,50. Furthermore, the ARGs of emerging like carbapenem resistant related genes to which treatment options are very limited such as ndm-1, blaVIM, blaOXA1/blaOXA-30, CTX-M which are usually found in the clinical settings were also found in the study site51.
Resistance to different generations of antibiotics
The detected ARG subtypes have the capacity to confer resistance to diverse classes of antibiotics spanning multiple generations. The Aph gene, detected in high copy numbers, was found to confer resistance to 1st (kanamycin, neomycin), 2nd (gentamicin), and 3rd (Tobramycin, amakicin) gen aminoglycosides. Genes aadA and str can provide resistance to 1st gen, aacC confers resistance to 2nd and 3rd gen aminoglycosides34. The prevalent in the β-lactams, blaoxy confers resistance to 3rd (aminopenicillins) and 4th (carboxypenicillins) gen penicillins, cephalosporins, and monobactams (aztreonam). Genes blaCTXM, blaOXA and fox 5 were identified to confer resistance to 2nd and 3rd gen penicillins and to aztreonam, cephamycins, and third-gen cephalosporins (ceftazidime). PenA and blaTEM were associated with resistance to penicillin, ceftriaxone, and 3rd gen aminopenicillins (ampicillin and amoxicillin). Clinically significant genes, ndm-1 (resistant to all β-lactams except aztreonam), and cfiA, (resistant to carbapenems (last-resort antibiotics)), were also found in the study site. In MLSBs, resistance to 1st and 2nd gen antibiotics was detected. Genes ereA, ermA, mefA, lnuB-01 can confer resistance to erythromycin and lincosamide (1st gen), while mphA-02 was linked to resistance against 1st gen erythromycin and 2nd gen roxithromycin. In the tetracycline class, variants capable of conferring resistance to 1st, 2nd, and 3rd gen tetracyclines were identified. Tet (35) and tet (36) were associated with resistance to 1st gen, tet M and tet O to 2nd gen and tet (32) was to 3rd gen (tigecycline) tetracyclines34.
Resistance mechanism
The identified ARGs primarily employ five major resistance mechanisms: antibiotic inactivation (41.17%), antibiotic efflux (30.53%), antibiotic target protection (14.84%), antibiotic target alteration (8.12%), and antibiotic target replacement (5.32%) (Fig. 7). Within the class, the gene variants demonstrated diverse mechanisms, but primarily contributed to one or two major mechanisms. The inactivation mechanism was primarily driven by β-lactams, aminoglycosides, & MLSBs and efflux by multidrug and chloramphenicols. Protection was associated with tetracyclines and quinolones, while alteration was linked to MLSBs. Replacement was solely observed with sulfonamide and trimethoprims. The aminoglycoside (AG) class primarily employs the inactivation mechanism, a widespread resistance mechanism mediated by AG-modifying enzymes, including acetyltransferases (AAC), nucleotidyltransferases (ANT), and phosphotransferases (APH)52. These enzymes acetylate, adenylate, and phosphorylate open sites on aminoglycosides, rendering the antibiotic inactive53,54. The study site revealed the presence of resistance genes associated with these enzymatic modifications. Notably, plasmid or transposon-encoded O-phosphotransferases (Aph and strB) and O-nucleotidyltransferases (aadA and aadE) were prevalent, while gene cassette-borne acetyltransferases (aacC and aac) were less common. All β-lactam class gene variants predominantly utilize the inactivation mechanism, except for penA, which employs the alteration mechanism. In inactivation, resistance genes generate enzymes that make antibiotics inactive. Conversely, in the alteration mechanism, gene products modify antibiotic-binding targets in the cell wall, particularly the essential penicillin-binding proteins (PBPs)55. In the trimethoprim and sulfonamide class, detected genes operate via the replacement mechanism, where they substitute the antibiotic-binding target34. In the MLSBs class, resistance is conferred through three primary mechanisms: inactivation, alteration, and protection. The inactivation mechanism involves three enzymatic activities—erythromycin esterase (ere A), macrolide phosphotransferase (mphA-02), and lincosamide nucleotidyltransferase (lnuB-01, lnuB-02). Alteration is driven by genes like carB, ermA, ermB, ermT-01, and ermT-02, which employ ribosomal RNA methyltransferases to modify the antibiotic’s target binding site, reducing efficacy. The protection mechanism, associated with the gene mefA, shields the antibiotic’s target, conferring resistance34. In both multidrug and chloramphenicol classes, the prevalent resistance mechanism is efflux, except for the multidrug gene oprD, which utilizes the alteration mechanism. The efflux mechanism was further observed in some gene variants of tetracyclines (tetB-01, tetC-01, tetD-01, tetE, tetG-01, tetM-01, and tetPB-01) and quinolones (oqx A, oqxB 2) classes. In the same classes, protection (tet (32), tet (36)-01, tetO-01, tetQ, tetS, qnr A, qnr B, qnr S, and qnr S 2) and inactivation mechanism (tet (37), tet (34), tet (35)) were also observed34.
The study helps to understand the AR dynamics in an urban community over time. Seasons predominantly influenced the abundance/copy number of the gene, rather than their detection frequency. ARGs encoding resistance to aminoglycosides, sulfonamide & trimethoprims, and β-lactam resistance classes consistently demonstrated high resistance levels over the entire sampling period; which might be due to the extensive use of these antibiotic classes in both human medicine and veterinary. The persistent resistance in the community was characterized by widespread presence of all ARG classes, with β-lactams, multidrug, and aminoglycosides being the most prevalent. In the network analysis, the co-abundance of ARGs and MGEs within a single module indicates significant and robust correlations between them, suggesting a high likelihood of resistance transmission within the study site through gene transfer. This study acts as an early warning system for possible local and regional disease outbreaks. In addition, it adds valuable insights to the global repository of information on the density, diversity, and dynamics of resistance.
Methods
Study area and sampling strategy
An urban community (covering Tarnaka, Nacharam, and Lalaguda, ∼1.8 lakh population, 27 ± 2 MLD/day) in Hyderabad, Telangana, India, was selected as the study area based on insights from our previous study10. The study area contains two primary healthcare facilities but no agricultural activities, mass livestock farming, or antibiotic production. Sample collection was carried out according to the procedures described in ref. 56. Domestic wastewater samples were collected for a 5-month period from December (2021) to April (2022), i.e., from winter to the middle of the summer season. Sampling was carried out in the early hours (7.00 am to 8.30 am) of the morning at a depth of 0.5 m using grab sampling method near the end of the main drain (17.4308° N, 78.5595° E), which receives flow from the community’s 12 main lateral drains57. In sterile bottles, samples were collected in triplicates with a volume of 1 l each and quickly transported to the laboratory for analysis. Sample collection dates are represented in Supplementary Table 6.
Sample processing: wastewater characterization and DNA extraction
Prior to analysis, the triplicate samples were compounded and filtered using 150μm stainless steel mesh to remove the suspended particulates followed by wastewater characterization and ARGs quantification. pH has been measured using a multimeter probe (HANNA; HI5522). The measurements of COD (Chemical Oxygen Demand), TDS (Total Dissolved Solids), TSS (Total suspended solids), sulfates, nitrates and phosphates were carried out in accordance with established protocols58. The microbial biomass in water sample was collected by centrifuging the pre-filtered sample (100 mL) in sterile conditions for 10 min at 10,000 rpm. The supernatant was discarded and the pellet was washed thoroughly with PBS (phosphate buffer saline) two times. Genomic DNA extraction from the pellet was done by HiPurA® soil DNA purification kit (HIMEDIA HiGenoMB) following the manufacturers protocol. The DNA extraction quality was validated through 1% agarose gel electrophoresis, and its concentration was determined calorimetrically (Nanodrop 2000c; Thermo Scientific). Subsequently, it was stored at −20 °C until use10.
Detection and quantification of ARGs and MGEs
To assess the antibiotic resistivity, q-PCR (Light Cycler 96-Roche) was performed to a total of 136 primer sets including 123 ARGs, 13 MGEs (5 integrons and 8 transposons) and 1 16 S rRNA gene22,59. The rationale for selecting these genes is to ensure the representation of resistance to all major classes of antibiotics, as well as to align with the detection of these corresponding antibiotics in community wastewater as observed in our previous study10. The targeted 123 ARGs conferred resistance to widely used antibiotics like aminoglycosides (10), β-lactams (27), sulfonamide and trimethoprims (6), macrolide-lincosamide-streptogramin-B (19), quinolones (8), tetracyclines (21), multidrugs (19), vancomycins (9), and chloramphenicols (4). Primer/Oligonucleotides sequence and resistance mechanism were listed in Supplementary Table 722,59,60,61,62,63,64,65, and Supplementary Table 834. The PCR reaction volume is 10 μL; 5 μL-Master mix (TB Green premix Ex Taq II), 0.8 μL-each forward and reverse primer (10 μM), 1 μL-DNA template (5 ng) and 2.4 μL of nuclease-free PCR grade water. The reaction conditions of the PCR cycling program included: pre-incubation (95 °C, 5 min), 40 cycles of denaturation (95 °C, 15 s), annealing (60 °C, 60 s) and elongation (72 °C, 20 s) followed by melting curves (95 °C, 5 min and 65 °C, 1 min). The reactions were conducted in triplicates to ensure reproducibility, and a negative control with no template was included for comparison in each run to avoid any possible contamination. After amplification, the autogenerated melting curves and Ct values were exported to the LightCycler® 96 q-PCR software (V. 1.1) for analysis. For each primer set, Ct (threshold cycle) <28, and amplification of at least two of the three replicates with nearer Ct values and the same pattern of dissociation curve is considered as positive. The mean of the Ct values is used to calculate the gene copies, and the relative copy number is calculated by bringing its ratio to the 16 S rRNA gene using the following Eqs. (1) and (2)59.
Network analysis
To reduce the possibility of random coincidences, we examined co-abundance exclusively among prevalent ARGs and MGEs where, prevalence was defined as genes detected in at least 4 months. Using the R packages dplyr, Stringr, tidyverse, and tidyr, correlation, and statistical differences were analyzed. A correlation matrix was generated to illustrate the correlations in the network interface by computing all possible pair-wise Pearson’s rank correlations among the ARG and MGE subtypes66. A Pearson’s correlation coefficient (ρ) greater than 0.80 indicated a statistically significant correlation between the two items. To visualize the networks, a modular structure approach was employed with the Gephi interactive platform (version 0.10)67.
Data availability
All data generated or analyzed during this study are included in the main manuscript and Supplementary Information.
References
Nadimpalli, M. L. et al. Urban informal settlements as hotspots of antimicrobial resistance and the need to curb environmental transmission. Nat. Microbiol. 5, 787–795 (2020).
Wang, H. et al. Toxicity evaluation of β‐diketone antibiotics on the development of embryo‐larval zebrafish (Danio rerio). Environ. Toxicol. 29, 1134–1146 (2014).
World Health Organization. Antimicrobial Resistance: Global Report on Surveillance (World Health Organization, 2014).
Larsson, D. G. J. & Flach, C. F. Antibiotic resistance in the environment. Nat. Rev. Microbiol. 20, 257–269 (2022).
Singer, A. C., Shaw, H., Rhodes, V. & Hart, A. Review of antimicrobial resistance in the environment and its relevance to environmental regulators. Front. Microbiol. 7, 1728 (2016).
Gu, Q. et al. Characteristics of antibiotic resistance genes and antibiotic-resistant bacteria in full-scale drinking water treatment system using metagenomics and culturing. Front. Microbiol. 12, 798442 (2022).
Gupta, S., Graham, D. W., Sreekrishnan, T. R. & Ahammad, S. Z. Effects of heavy metals pollution on the co-selection of metal and antibiotic resistance in urban rivers in UK and India. Environ. Pollut. 306, 119326 (2022).
Buelow, E. et al. Hospital discharges in urban sanitation systems: long-term monitoring of wastewater resistome and microbiota in relationship to their eco-exposome. Water Res. 7, 100045 (2020).
Zheng, J. et al. High-throughput profiling of seasonal variations of antibiotic resistance gene transport in a peri-urban river. Environ. Int. 114, 87–94 (2018).
Javvadi, Y. & Mohan, S. V. Understanding the distribution of antibiotic resistance genes in an urban community using wastewater-based epidemiological approach. Sci. Total Environ. 868, 161419 (2023).
Joseph, S. M., Battaglia, T., Maritz, J. M., Carlton, J. M. & Blaser, M. J. Longitudinal comparison of bacterial diversity and antibiotic resistance genes in New York City sewage. mSystems 4, 10–1128 (2019).
Moges, F. et al. The growing challenges of antibacterial drug resistance in Ethiopia. J. Glob. Antimicrob. Resist. 2, 148–154 (2014).
Martinez, E. P. et al. Seasonality of antimicrobial resistance rates in respiratory bacteria: A systematic review and meta-analysis. PLoS ONE 14, e0221133 (2019).
Ekundayo, T. C., Swalaha, F. M. & Ijabadeniyi, O. A. Socioeconomic indices guided linear mixed-effects and meta-regression modelling of the temporal, global and regional prevalence of Helicobacter pylori in environmental waters: a class I carcinogen. J. Environ. Manag. 342, 118282 (2023).
Mohan, S. V., Hemalatha, M., Kopperi, H., Ranjith, I. & Kumar, A. K. SARS-CoV-2 in environmental perspective: occurrence, persistence, surveillance, inactivation and challenges. J. Chem. Eng. 405, 126893 (2021).
Hendriksen, R. S. et al. Global monitoring of antimicrobial resistance based on metagenomics analyses of urban sewage. Nat. Commun. 10, 1–12 (2019).
Bengtsson-Palme, J., Gunnarsson, L. & Larsson, D. J. Can branding and price of pharmaceuticals guide informed choices towards improved pollution control during manufacturing. J. Clean. Prod. 171, 137–146 (2018).
Baum, R., Luh, J. & Bartram, J. Sanitation: a global estimate of sewerage connections without treatment and the resulting impact on MDG progress. Environ. Sci. Technol. 47, 1994–2000 (2013).
Nicolaou, N., Siddique, N. & Custovic, A. Allergic disease in urban and rural populations: increasing prevalence with increasing urbanization. Allergy 60, 1357–1360 (2005).
Hu, H. W. et al. Diversity of herbaceous plants and bacterial communities regulates soil resistome across forest biomes. Environ. Microbiol. 20, 3186–3200 (2018).
Lai, F. Y., Muziasari, W., Virta, M., Wiberg, K. & Ahrens, L. Profiles of environmental antibiotic resistomes in the urban aquatic recipients of Sweden using high-throughput quantitative PCR analysis. Environ. Pollut. 287, 117651 (2021).
Yu, K. et al. Antibiotic resistome associated with microbial communities in an integrated wastewater reclamation system. Water Res. 173, 115541 (2020).
Zhao, R., Feng, J., Huang, J., Li, X. & Li, B. Reponses of microbial community and antibiotic resistance genes to the selection pressures of ampicillin, cephalexin and chloramphenicol in activated sludge reactors. Sci. Total Environ. 755, 142632 (2021).
Wasko, I., Kozińska, A., Kotlarska, E. & Baraniak, A. Clinically relevant β-lactam resistance genes in wastewater treatment plants. Int. J. Environ. Res. Public Health 19, 13829 (2022).
Khan, F. A., Söderquist, B. & Jass, J. Prevalence and diversity of antibiotic resistance genes in Swedish aquatic environments impacted by household and hospital wastewater. Front. Microbiol. 10, 688 (2019).
Cacace, D. et al. Antibiotic resistance genes in treated wastewater and in the receiving water bodies: a pan-European survey of urban settings. Water Res. 162, 320–330 (2019).
Amos, G. et al. The widespread dissemination of integrons throughout bacterial communities in a riverine system. ISME J. 12, 681–691 (2018).
Ho, J. Y. et al. Multidrug-resistant bacteria and microbial communities in a river estuary with fragmented suburban waste management. J. Hazard. Mater. 405, 124687 (2021).
Su, S. et al. Distribution of antibiotic resistance genes in three different natural water bodies-a lake, river, and sea. Int. J. Environ. Res. Public Health 17, 552 (2020).
Suzuki, S. et al. Macrolide resistance genes and mobile genetic elements in water ways from pig farms to the sea in Taiwan. J. Glob. Antimicrob. Resist. 29, 360–370 (2022).
Petinaki, E. & Papagiannitsis, C. Resistance of Staphylococci to Macrolides-Lincosamides-Streptogramins B (MLSB): Epidemiology and Mechanisms of Resistance, Staphylococcus aureus (IntechOpen, 2019).
Obayiuwana, A. & Ibekwe, A. M. Antibiotic resistance genes occurrence in wastewaters from selected pharmaceutical facilities in Nigeria. Water 12, 1897 (2020).
Jiao, Y. N. et al. Biomarkers of antibiotic resistance genes during seasonal changes in wastewater treatment systems. Environ. Pollut. 234, 79–87 (2018).
Alcock, B. P. et al. CARD 2023: expanded curation, support for machine learning, and resistome prediction at the Comprehensive Antibiotic Resistance Database. Nucleic Acids Res. 51, D690–D699 (2023).
Amin, M. B. et al. High prevalence of plasmid-mediated quinolone resistance (PMQR) among E. coli from aquatic environments in Bangladesh. PLoS ONE 16, e0261970 (2021).
Su, H. C. et al. Persistence of antibiotic resistance genes and bacterial community changes in drinking water treatment system: from drinking water source to tap water. Sci. Total Environ. 616, 453–461 (2018).
Gyles, C. & Boerlin, P. Horizontally transferred genetic elements and their role in pathogenesis of bacterial disease. Vet. Pathol. 51, 328–340 (2014).
Zheng, W., Huyan, J., Tian, Z., Zhang, Y. & Wen, X. Clinical class 1 integron-integrase gene–a promising indicator to monitor the abundance and elimination of antibiotic resistance genes in an urban wastewater treatment plant. Environ. Int. 135, 105372 (2020).
Conco, T. et al. Profiling of emerging pathogens, antibiotic resistance genes and mobile genetic elements in different biological wastewater treatment plants. J. Environ. Chem. Eng. 10, 107596 (2022).
Shapiro, J. T. et al. Multilayer networks of plasmid genetic similarity reveal potential pathways of gene transmission. ISME J. 17, 649–659 (2023).
Sun, S. et al. Temporal variations of antibiotic resistance genes in influents and effluents of a WWTP in cold regions. J. Clean. Prod. 328, 129632 (2021).
Schages, L., Wichern, F., Kalscheuer, R. & Bockmühl, D. Winter is coming–Impact of temperature on the variation of beta-lactamase and mcr genes in a wastewater treatment plant. Sci. Total Environ. 712, 136499 (2020).
Caucci, S. et al. Seasonality of antibiotic prescriptions for outpatients and resistance genes in sewers and wastewater treatment plant outflow. FEMS Microbiol. Ecol. 92, fiw060 (2016).
García-Armisen, T. et al. Seasonal variations and resilience of bacterial communities in a sewage polluted urban river. PLoS ONE 9, e92579 (2014).
Zhang, K. et al. Characterization of antibiotic resistance genes in drinking water sources of the Douhe Reservoir, Tangshan, northern China: the correlation with bacterial communities and environmental factors. Environ. Sci. Eur. 34, 56 (2022).
Lu, X. M. & Lu, P. Z. Seasonal variations in antibiotic resistance genes in estuarine sediments and the driving mechanisms. J. Hazard. Mater. 383, 121164 (2020).
Beaber, J., Hochhut, B. & Waldor, M. SOS response promotes horizontal dissemination of antibiotic resistance genes. Nature 427, 72–74 (2004).
Miller, J. H., Novak, J. T., Knocke, W. R. & Pruden, A. Elevation of antibiotic resistance genes at cold temperatures: implications for winter storage of sludge and biosolids. Lett. Appl. Microbiol. 59, 587–593 (2014).
Yin, X. et al. Exploration of the antibiotic resistome in a wastewater treatment plant by a nine-year longitudinal metagenomic study. Environ. Int. 133, 105270 (2019).
Munck, C. et al. Limited dissemination of the wastewater treatment plant core resistome. Nat. Commun. 6, 8452 (2015).
Pärnänen, K. M. M. et al. Antibiotic resistance in European wastewater treatment plants mirrors the pattern of clinical antibiotic resistance prevalence. Sci. Adv. 5, eaau9124 (2019).
Garneau-Tsodikova, S. & Labby, K. J. Mechanisms of resistance to aminoglycoside antibiotics: overview and perspectives. Medchemcomm 7, 11–27 (2016).
Mutuku, C., Gazdag, Z. & Melegh, S. Occurrence of antibiotics and bacterial resistance genes in wastewater: resistance mechanisms and antimicrobial resistance control approaches. World J. Microbiol. Biotechnol. 38, 152 (2022).
Poirel, L. et al. antimicrobial resistance in Escherichia coli. Microbiol. Spectr. 6, ARBA–0026 (2017).
Moya, B. et al. β-Lactam resistance response triggered by inactivation of a nonessential penicillin-binding protein. PLoS Pathog. 5, e1000353 (2009).
Kopperi, H. et al. Defining the methodological approach for wastewater-based epidemiological studies-Surveillance of SARS-CoV-2. Environ. Technol. Innovation 23, 101696 (2021).
Tharak, A. et al. Understanding SARS-CoV-2 infection and dynamics with long term wastewater based epidemiological surveillance. Int. J. Environ. Res. Public Health 19, 2697 (2022).
APHA. Standard Methods for the Examination of Water and Waste Water (American Public Health Association, 2017).
Chen, Y. et al. High-throughput profiling of antibiotic resistance gene dynamic in a drinking water river-reservoir system. Water Res. 149, 179–189 (2019).
Looft, T. et al. In-feed antibiotic effects on the swine intestinal microbiome. Proc. Natl. Acad. Sci. USA 109, 1691–1696 (2012).
Chen, Q. et al. Long-term field application of sewage sludge increases the abundance of antibiotic resistance genes in soil. Environ. Int. 92, 1–10 (2016).
Ouyang, W. Y., Huang, F. Y., Zhao, Y., Li, H. & Su, J. Q. Increased levels of antibiotic resistance in urban stream of Jiulongjiang River, China. Appl. Microbiol. Biotechnol. 99, 5697–5707 (2015).
Su, J. Q. et al. Antibiotic resistome and its association with bacterial communities during sewage sludge composting. Environ. Sci. Technol. 49, 7356–7363 (2015).
Zhu, Y. G. et al. Diverse and abundant antibiotic resistance genes in Chinese swine farms. Proc. Natl. Acad. Sci. USA 110, 3435–3440 (2013).
Liu, B. & Pop, M. ARDB—antibiotic resistance genes database. Nucleic Acids Res. 37, 443–D447 (2009).
Steele, J. A. et al. Marine bacterial, archaeal and protistan association networks reveal ecological linkages. ISME J. 5, 1414–1425 (2011).
Li, B. et al. Metagenomic and network analysis reveal wide distribution and co-occurrence of environmental antibiotic resistance genes. ISME J. 9, 2490–2502 (2015).
Acknowledgements
Y.J. wants to acknowledge the Department of Science and Technology (DST) for providing Inspire Fellowship for pursuing Doctoral Research. Y.J. sincerely thank J. Santosh Yadav (research scholar-CSIR-IICT), for his help in sample collection. Y.J. wish to acknowledge J. Lakshmi Bhavani (systems engineer-TCS) and J.S.S.D. Manikanta (product development engineer-Phenome People) for their help in the generation of heat maps. The authors wish to thank the Director, CSIR-IICT, Hyderabad, for support and encouragement in carrying out this work (Manuscript no. IICT/Pubs./2023/335).
Author information
Authors and Affiliations
Contributions
Yamini Javvadi: research methodology design, experiment work, original draft preparation, accountability, and resolving accuracy or integrity questions. Dr. S. Venkata Mohan: conceptualization, research methodology, supervision, original draft preparation, accountability, and resolving accuracy or integrity questions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Javvadi, Y., Mohan, S.V. Temporal dynamics and persistence of resistance genes to broad spectrum antibiotics in an urban community. npj Clean Water 7, 56 (2024). https://doi.org/10.1038/s41545-024-00349-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41545-024-00349-y
- Springer Nature Limited