Abstract
Non-invasive cardiac output monitoring, via electrical biosensing technology (EBT), provides continuous, multi-parameter hemodynamic variable monitoring which may allow for timely identification of hemodynamic instability in some neonates, providing an opportunity for early intervention that may improve neonatal outcomes. EBT encompasses thoracic (TEBT) and whole body (WBEBT) methods. Despite the lack of relative accuracy of these technologies, as compared to transthoracic echocardiography, the use of these technologies in neonatology, both in the research and clinical arena, have increased dramatically over the last 30 years. The European Society of Pediatric Research Special Interest Group in Non-Invasive Cardiac Output Monitoring, a group of experienced neonatologists in the field of EBT, deemed it appropriate to provide recommendations for the use of TEBT and WBEBT in the field of neonatology. Although TEBT is not an accurate determinant of cardiac output or stroke volume, it may be useful for monitoring longitudinal changes of hemodynamic parameters. Few recommendations can be made for the use of TEBT in common neonatal clinical conditions. It is recommended not to use WBEBT to monitor cardiac output. The differences in technologies, study methodologies and data reporting should be addressed in ongoing research prior to introducing EBT into routine practice.
Impact statement
-
TEBT is not recommended as an accurate determinant of cardiac output (CO) (or stroke volume (SV)).
-
TEBT may be useful for monitoring longitudinal changes from baseline of hemodynamic parameters on an individual patient basis.
-
TEBT-derived thoracic fluid content (TFC) longitudinal changes from baseline may be useful in monitoring progress in respiratory disorders and circulatory conditions affecting intrathoracic fluid volume.
-
Currently there is insufficient evidence to make any recommendations regarding the use of WBEBT for CO monitoring in neonates.
-
Further research is required in all areas prior to the implementation of these monitors into routine clinical practice.
Similar content being viewed by others
Introduction
Hemodynamic monitoring
Cardiac output (CO) is considered a fundamental physiological parameter for diagnosis and guidance of therapy in various neonatal conditions1. Maintaining optimal perfusion and oxygenation is of prime importance in the neonatal intensive care unit (NICU). Comprehensive monitoring of various physiological variables is required, as low CO has been associated with increased morbidity, adverse neurodevelopmental outcome, and increased mortality2.
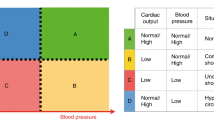
The circulatory system of neonates is significantly different from that of adults or children, as the neonatal population is a heterogeneous mix of gestational and postconceptional ages, with different degrees of cardiovascular maturation3. Indirect measures of CO, such as HR and blood pressure (BP), are inadequate for a comprehensive assessment of neonatal hemodynamic status4. Comprehensive hemodynamic monitoring, including CO, is thus an essential part of neonatal care to prevent adverse outcomes.
Cardiac output monitoring technology
CO measurement, via invasive techniques, e.g., intermittent pulmonary artery thermodilution and Fick’s method, are considered the gold standards for accurately determining CO in adults5. However, in neonates these methods are inappropriate6 as catheters are often too big and the invasiveness of these methods have been questioned7. Minimally invasive CO monitoring technologies encompass devices not requiring the insertion of a pulmonary artery catheter, e.g., pulse contour, pulse power analysis, partial gas re-breathing and transpulmonary ultrasound dilution8. Some of these technologies require the placement of an arterial line (pulse contour and pulse power analysis) and may need placement of a central venous line for calibration purposes6. These technologies have been poorly studied in the neonatal population whilst others are still under development (transpulmonary ultrasound dilution)9. Most other CO measurement methodologies in neonates offer only intermittent measurement values as they are labor, skill or technology intensive (transthoracic echocardiography (TTE) and cardiac magnetic resonance imaging)6.
Non-invasive CO monitoring technologies were therefore developed to overcome these challenges, offering fully non-invasive methods of monitoring stroke volume (SV) and CO. These included intermittent measurements via transcutaneous Doppler ultrasound (Ultrasound Cardiac Output Monitor and TTE) and continuous measurements via various electrical biosensing technologies (EBT) (bioimpedance (BI) and bioreactance (BR)).
For a new technology to be safely used in the clinical environment and to allow therapeutic decisions to be based upon it, it must be proven to be accurate and precise. A good agreement between a new and a reference technology is defined by a small bias (indicating a high accuracy), narrow limits of agreement (indicating a high precision) and a percentage error ≤30% (indicating technology interchangeability)10,11. Trending ability (change over time) should also be assessed to ensure that the new technology’s direction and magnitude of change is in line with that of the reference technology12.
Overview of EBT technology
The first type of non-invasive cardiac monitoring, rheocardiography, was developed in 1949 by Kedrov13 but only found popularity in 1966 when Kubicek re-designed it for use in the aerospace industry14. Since then, numerous iterations of this technology have become available in the healthcare industry, with methodologies measuring changes in whole body, segmental or thoracic impedance from which SV and hence CO is derived. Numerous nomenclatures are used—whole body electrical bioimpedance, thoracic electrical bioimpedance (TEB), electrical velocimetry, electrical cardiometry, impedance cardiometry, impedance cardiography, thoracocardiography, bioreactance and rheocardiography. These have subtle differences, often with proprietary algorithms and models to estimate SV and CO.
For EBT a high frequency, low amplitude electrical current is applied across the thorax (TEBT) or entire body (WBEBT). The resistance (impedance, Z0) to this electrical current varies between different tissues in the body, with the primary distribution being to the blood and extracellular fluid. This change in electrical current (∆Z0) over time (dZ0/dt) corresponds to SV, from which CO can be estimated.
EBT is divided into 2 broad categories: (1) bioimpedance (BI) which encompasses thoracic electrical velocimetry, electrical cardiometry, impedance cardiography as well as WBEBT, and (2) bioreactance (BR).
Significant differences exist between BI and BR15 (Table 1).
Thoracic electrical biosensing technology
Bioimpedance (BI)
Electrical velocimetry and electrical cardiometry
Electrical cardiometry (EC) is the method of non-invasive CO technology that utilizes the model of thoracic electrical velocimetry (EV) to determine SV and CO16. These are used by Aesculon™ and ICON™, manufactured by Osypka Medical GmbH, Germany (Fig. 1)
In EC, the change in impedance (∆Z0) is due to the degree of erythrocyte alignment in the aorta throughout the cardiac cycle. During diastole, as the aortic blood flow ceases, erythrocytes are randomly orientated and interfere with electrical conduction. During systole as the ventricles contract, the erythrocytes are forced to align parallel to pulmonary and aortic flow and the electrical current in the large vessels passes with less impedance, hence an increased conductivity in the absence of turbulent flow. These pulsatile changes in volume and thus in impedance, in relation to the cardiac cycle (∆Z0(t)), are used to calculate ejection/ flow time and thus SV.
EV estimates SV by means of the following equation17:
where SVTEB is SV estimated by TEB, CP is the patient constant (volume of electrically participating tissue, in ml), vFT is the mean blood velocity index (in s-1) during flow time (FT; measured in s). The EV model estimates SV based on the input of the patient’s body mass, an empiric means velocity index derived from a peak amplitude measurement assumed to be the peak aortic blood flow acceleration and a measurement of flow time.
Impedance cardiography (ICG) and electrical cardiometry (EC) are similar as both rely on periodical volumetric changes in the aorta to determine SV and CO. However, ICG and EC differ in the model applied to determine impedance measurements, specifically as to how the change in impedance is calculated. In ICG the change in impedance (conductivity) (ΔZ(t)) is solely attributed to the volumetric expansion of the ascending aorta due to the increase of volume within the aorta or due to its wall motion. The index of peak velocity of the volumetric change is used in ICG as compared to the index of peak acceleration in EV. EV includes direction of flow whereas ICG does not. In EV, volume changes also incorporate the alignment of erythrocytes18.
Bioreactance (BR)
In BR, another thoracic EBT method, it is assumed that blood flow changes are not only related to changes in impedance but also changes in capacitance (ability of biological tissue to store an electrical current) and inductance (biological tissue’s ability to store energy in a non-electrical form). BR therefore measures phase shift (φ) of an oscillating current as it traverses the thorax19. Four pairs of sensors, one electrode acting as a high frequency generator and the other as a receiver, are placed on either side of the thorax (Fig. 1). CO measurements are determined separately from each side of the body and the final CO is the average of the measurements.
BR uses the following formula to estimate SV20:
where C is a constant of proportionality, VET is ventricular ejection time, and dφ/ dtmax is the peak rate of change of the phase shift (Δφ). BR is used by the Reliant® and its newer version, Starling®, manufactured by Baxter, Deerfield, Illinois.
WBEBT
WBEBT is a derivative of ICG where the electrical current is passed through the whole body by the placement of electrodes on the radial aspect of the wrist and the posterior tibial area of the ankle (Fig. 1). With placement of the electrodes on the distal portions of the extremities, the low voltage current (30 K kHz AC current, 1.4 mA) passes through all major arteries and veins and the resistive portion of bioimpedance is measured.
The original NICaS monitor was upgraded to the NICaS 2004 Slim model in order to improve the accuracy and reliability of the CO, cardiac index (CI) results and their derivatives.
The various commercially available TEBT and WEBT technologies are summarized in Table 2.
Cardiac output monitoring principles
Worldwide, 11% of all births are preterm with prematurity being the cause of 50% of all neonatal deaths21. With the growing number of surviving preterm neonates, at an ever-increasing younger gestational age22, the need for accurate monitoring is essential. The incidence of hemodynamic compromise is unknown as an exact definition is lacking. Often, blood pressure is the only parameter used and the definition of a “normal” blood pressure and the definition of hypotension is fraught with uncertainty23,24. Isolated, episodic clinical examination, vital signs and laboratory values are insufficient25 to assess a system that is in a continuous state of change, such as the neonate’s cardiovascular system26. For this reason, continuous, objective hemodynamic monitoring is essential.
Non-invasive CO monitoring offers the ability to continuously monitor several hemodynamic variables that provide insight into the changing dynamics of the preterm neonate’s cardiovascular system. By monitoring heart rate (HR), oscillometric blood pressure (BP) and peripheral saturation (SpO2) non-invasive CO monitors provide similar data to conventional vital signs monitor. In addition, these devices are able to provide SV, CO, total peripheral resistance, and thoracic fluid content (TFC), allowing estimation of global blood flow and cardio-pulmonary interaction. This may aid in determining the underlying pathophysiology of hemodynamic compromise.
The American College of Critical Care Medicine emphasizes the need for the early recognition of symptoms and the initiation of goal-orientated, time sensitive interventions to improve patient outcomes in neonatal shock. The guidelines also support the use of hemodynamic parameters, such as cardiac index (CO corrected for body surface area)27. In this regard, non-invasive CO monitoring may assist in the recognition of hemodynamic instability and shock, allowing the timely initiation of therapy and allowing therapeutic monitoring. The National Institute of Child Health and Human Development (NIHCD) has also emphasized the need for accurate, reliable and continuous methods to measure CO at the bedside whilst stating that TEBT-methods require validation28.
The use of hemodynamic monitoring in critically ill patients is reliant on the following principles: (1) no hemodynamic monitoring technique can improve outcome by itself; (2) monitoring requirements may vary over time and may depend on local availability and training; (3) there are no optimal hemodynamic values that are applicable to all patients; (4) variables should be combined and integrated; (5) CO is estimated but not measured; (6) monitoring hemodynamic changes over short periods of time is important; (7) continuous measurements of all hemodynamic variables is preferable and (8) non-invasiveness is not the only issue29.
Various theoretical, hardware, and patient-related factors must be considered when choosing a hemodynamic monitor (Table 3). Desirable characteristics of CO monitoring technologies are accuracy, precision, reproducibility, operator independence, rapid response time, continuous monitoring, ease of use and application, and cost effectiveness15. Currently, no such device exists for any patient population. The choice of CO monitor then depends on machine availability, patient characteristics, clinical situation, and practitioner preference30.
Clinical applications of EBT in neonatology
The Special Interest Group (SIG) on Non-invasive Cardiac Output Monitoring (NICOM) of the European Society for Paediatric Research (ESPR) deemed it necessary to provide guidance on the use of NICOM technology in the field of neonatology, based on literature up to January 2024.
Recommendations and suggestions are provided based on the available strength of evidence, as determined by the quality, quantity, and consistency of studies and evidence31. Recommendations were stated if there was strong evidence in the field (both positive or negative for strong or poor evidence), whereas suggestion was used based on less evidence.
Numerous studies in the neonatal setting have demonstrated the ease of use, non-invasiveness, and non-intrusiveness of the use of TEBT (supplementary data). These studies have shown changes in SV and CO in various clinical circumstances, physiological as well as pathophysiological, and during various medical and surgical interventions (supplementary data). Despite the probable lack of accuracy and precision of these devices, EBT may be able to provide additional, continuous monitoring that might be used in conjunction with traditional vital signs and monitoring aids (TTE).
TEBT to measure cardiac output
Numerous studies have reported on the agreement and accuracy of TEBT32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49 (supplementary data). Various narrative and meta-analyses have shown relative accuracy (low bias), poor precision (wide limits of agreements), and a high PE, indicative of non-interchangeability with TTE of EBT in neonates45,47,49,50,51. TEBT CO has poor correlation with TTE-derived RVO38 as compared to TTE-LVO.
TEBT has also been shown to have poor trending accuracy over the first 72 hours49 and first month45 after birth. TEBT has been shown to longitudinally track CO, enabling the identification of low CO post PDA ligation39, but bias may increase over time52.
TEBT has been compared to TTE in most neonatal research. No studies have been performed to compare TEBT to more accurate CO measuring methods, as many are difficult in neonates (cardiac MRI) or utilize inappropriate equipment (thermodilution). The utilization of TTE as a reference method remains problematic, as it is known to be inaccurate as compared to thermodilution1.
Machine learning has also been used to predict the subsequent 60 min of CO with good accuracy based on the first 300 min after its application53.
Recommendation
TEBT cannot accurately determine CO in neonatal care and is not interchangeable with TTE.
Its ability to longitudinally monitor CO may be clinically useful but requires further research prior to routine use.
TEBT to determine and monitor PDA management
PDA is a common occurrence in NICU and preterm neonates. Its natural history, management, and long-term follow-up remains a challenge54. Pharmacological management entails indomethacin, paracetamol (acetaminophen) and ibuprofen. Surgical ligation remains a viable option for unstable neonates.
Numerous studies have included PDA as a primary or secondary outcome in EBT studies (supplementary data). The presence of a PDA has been shown to affect the accuracy of TEBT measurements, as compared to TTE40,41,43,46,48. Hemodynamically non-significant PDA had low bias, wide LOA and an acceptable PE40 whilst a hemodynamically significant duct showed a large bias, wide LOA and an unacceptable PE40. In contrast, the ongoing NOAH trial (Noninvasive Objective Assessment of Hemodynamics in preterm infants) showed no difference in accuracy between measurements with or without a PDA, whether hemodynamically significant or not47. Increased TEBT-CO within the first 24 h after birth, and low BP, has been shown to predict a PDA requiring treatment55.
TEBT accuracy and precision has been shown to worsen over time in preterm neonates undergoing PDA ligation, but TEBT monitoring was able to determine CO patterns for those infants who developed post ligation cardiac syndrome requiring milrinone39. TEBT has also been used to demonstrate a drop in CO after PDA ligation (metal clip as well as suture ligation) with recovery at 24 and 48 h post-operative, influenced by birth weight and LA/Ao ratio56. Various studies have shown differing drops in CO post PDA ligation (25–73%), irrespective of type of closure56,57,58.
TEBT-monitored hemodynamic variables (CI) in medical vs surgical PDA management in ELBW infants59 showed a better tolerance of medical closure compared to surgical closure. TEBT may be able to identify CO differences in neonates who respond to medical therapy60.
Recommendation
TEBT measurements are affected by the presence of a PDA. TEBT should not be used to determine appropriate management strategies for PDA until further research has been performed.
TEBT may be helpful in monitoring longitudinal CO changes but requires further research prior to routine use.
TEBT to monitor transition
In order to recognize low flow states, leading to hemodynamic compromise, a baseline from which to work is required. TTE-LVO proposed lower limit is 150 ml/kg/min61 but values vary widely62. Attempts have been made to determine normal values for TEBT SV and CO42,44,63,64. Studies have used various technologies (BI, BR, and older versions of these) with varying values determined for CO and SV. Clinicians and researchers should therefore be cognizant that there may be technology-related differences in normal values.
Transition from an intra-uterine to an extra-uterine environment remains a time of extreme changes in cardiovascular and pulmonary systems. Preterm infants remain at risk of a failure in transition due to their immature myocardium and are at risk of poor contractility in combination with the sudden decrease in systemic vascular resistance4. Few technologies are available to either monitor hemodynamic changes in real-time for all changes associated with transition or to provide early intervention65.
Various studies have utilized TEBT during the transition period (supplementary data). Studies have examined the feasibility of using TEBT in the transitional period66,67,68. Despite claiming feasibility, studies have shown the difficulty in maintaining a good signal68,69.
Studies monitoring CO during the first 15 min after birth have inconsistent results. Studies have shown a decrease in CO over the first 10 min after birth whilst others have shown an increase with subsequent decrease over the first few minutes67,70,71. Similarly, studies have shown contradictory reasons for improved CO after birth. Some have shown that SV remained stable, suggesting that the CO changes were driven by an increase in HR67,68,70 whilst other studies have shown that CO increase was driven by SV increases rather than HR72,73. Data also showed possible sex-related differences in the transitional phase, with higher CO in male infants66,70. The effect of resuscitation (including positive pressure ventilation or cardiopulmonary resuscitation) on TEBT-derived CO and SV has not been evaluated.
In an older TEBT-methodology study66, TEBT parameters did not differ between infants born via vaginal or cesarean section delivery, whilst a newer study showed differences in SV variation (SVV) between term and late preterm infants born via cesarean section and normal vaginal delivery74.
An older TEBT methodology study showed the ability of TEBT to monitor CO and SV in infants of diabetic mothers, but showed no difference in CO or SV, despite infants presenting with cardiomegaly75.
TEBT has been used to determine CO changes during delayed cord clamping (DCC) showing contrasting effects on CO76,77,78,79.
Desaturations and/ or bradycardia events in preterm very low birth weight infants in the first 72 h after birth have been shown to decrease CO and increase SVR, but were influenced by antenatal doppler abnormalities, gestational age, and the presence of a hemodynamically significant PDA on the changes on CO. The investigators suggested a targeted and individualized approach for minimizing cerebral injury in preterm infants80.
Suggestion
TEBT may be able to monitor the transitional phase, but normal values are technology-specific and require further research. Signal quality may affect the efficacy of TEBT to monitor this period. Further studies should be performed in different gestational age brackets to determine the exact trend in CO and SV in the transitional period, and thus its application in detecting maladaptation.
TEBT for monitoring ventilation management
Positive pressure ventilation is known to affect hemodynamics by decreasing systemic venous return, increasing right ventricular load, decreasing pulmonary blood flow, and possibly leading to systemic compromise81. Hemodynamic monitoring during ventilation in neonates, especially if preterm, may be beneficial.
Numerous studies have shown the effect of various modes of ventilation on the accuracy of TEBT, as compared to TTE38,40,43,44,47,48 (supplementary data). Evidence is contradictory regarding the degree of bias and effect on precision48 and the effect on the interaction between ventilation and PDA40. Studies have shown the largest inaccuracies were during the use of high frequency ventilation with bias increasing with increasing complexity of ventilation (nCPAP, SIMV, and HFO)48.
No differences in TEBT-CO or SV were found when switching between pressure controlled and volume targeted ventilation in extremely low gestational age neonates82. TEBT-CO has been shown to decrease post-extubation, primarily due to changes in SV due to the presence of a PDA83.
In a term infant study, TEBT hemodynamic indices were shown not to differ between infants with and without respiratory distress84. Late preterm infants who received surfactant showed a higher increase in CO and SV compared to those who had not received surfactant during the transitional phase72.
In an older TEBT technology study, impedance (Z0) was shown to increase with a concomitant decrease in SV and CO during the development of a pneumothorax, suggesting the ability to use TEBT to monitor for pneumothoraces85.
Recommendation
TEBT cannot be used to monitor hemodynamics during invasive or non- invasive ventilation management. TEBT may be helpful in assessing longitudinal CO changes with ventilatory changes. More research is required in this area.
TEBT to monitor sepsis and septic shock
Sepsis-related cardiovascular dysfunction is varied in neonates depending on the level and progress of sepsis. SVR may be high or low depending on the level of vasodilation leading to hypotension, as well as producing varying levels of cardiac output86. EBT multi-parameter monitoring may therefore be helpful in neonatal sepsis.
TEBT monitoring of HR, SVR, and CO has been stated to facilitate inotrope choice in neonatal septic shock as well as monitor response to management87, although TTE confirmation was not obtained to confirm changes in TEBT measurements.
TEBT monitoring of the hemodynamic status during sepsis in late preterm infants showed that SV, CO, and CI increased on day 2 after the diagnosis of sepsis as compared to controls88. TTE was used for confirmatory measurements, with low bias, LOA, and PE based on CI measurements.
Recommendation
TEBT should not be used to diagnose or monitor management of septic shock in neonates. TEBT may be helpful in monitoring longitudinal CO changes during diagnosis and management of sepsis. More research is required before routine implementation.
TEBT to monitor red blood cell (RBC) transfusions
Preterm infants with symptomatic anaemia may have a high CO and the degree of anemia has been correlated with CO89. RBC transfusions may therefore alter CO and monitoring would be advantageous to ensure continued adequate perfusion.
Few studies utilizing TEBT during RBC transfusions have been performed (supplementary data). TEBT studies have shown contradictory effects on CO - no CO changes90 as well as significantly lower CO but not SV91.
Recommendation
TEBT should not be used to monitor RBC transfusions. TEBT may be helpful in monitoring longitudinal CO changes during and after RBC transfusions. More research is required prior to routine clinical use.
TEBT to predict outcome
Few studies are available correlating TEBT with neonatal outcome (supplementary data).
Infants with a birth weight <1250 g who had a low TEBT-CO on day 1 after birth followed by a significant increase on day 2 were shown to have a higher risk of developing IVH and/or NEC92,93. A larger increase in CO over the first 48 h after birth has been associated with early brain damage, represented by high grade IVH (IVH ≥ grade 2)94. TEBT-CO monitored after PDA ligation was found to not be associated with poorer neurodevelopmental outcome95.
TEBT was able to predict IVH in preterm infants at 6 h of age with moderate precision and sensitivity but poor specificity in a deep machine learning study96.
Recommendation
TEBT should not be used to predict neonatal outcomes. More research is required.
TEBT for monitoring therapeutic hypothermia
Perinatal asphyxia may lead to multi-component hemodynamic compromise – myocardial dysfunction, decreased contractility, reduced preload and afterload, pulmonary hypertension, myocardial ischaemia and decreased CO97. These effects may be exacerbated during the hypothermic or re-warming phases of therapeutic hypothermia. EBT may therefore be useful for continuous monitoring.
Few studies are available investigating the use of TEBT during therapeutic hypothermia (supplementary data).
CO was shown to decrease due to a trend towards a decrease in HR with no significant change in SV in the first 6 h of TH initiation98,99. CO has been shown to decrease during TH100 and increase during rewarming100,101. CO has been shown to differ between different grades of HIE in neonates undergoing TH. CO has been shown to be similar in control and mild HIE groups over the first 24 h after birth but differed significantly between mild and moderate HIE groups102.
Low SV has been associated with unfavorable outcome103 as well as being associated with an abnormal MRI103 in infants with HIE. An abnormal MRI in infants with HIE who underwent TH was also associated with lower CO and higher SVR92.
Recommendation
TEBT should not be used to guide clinical management during TH. TEBT may be helpful in monitoring longitudinal CO changes during TH, but more research is required.
TEBT to monitor cardiac and other surgery
Few studies have utilized TEBT during cardiac surgery (supplementary data).
TEBT-SV, monitored 72 h post-operatively after a TGA switch procedure, showed poor precision as compared to TTE52.
TEBT has been stated to be able to monitor CO during prostaglandin therapy and balloon atrial septostomy in hypoplastic left heart syndrome, whilst TTE was unable to provide CO values due to structural abnormalities104.
TEBT-CO did not change during application of different intrathoracic insufflation pressures required for thoracic surgery (trachea-esophageal fistula without cardiac defects)105.
Recommendation
TEBT should not be used to monitor neonates undergoing any form of surgery. There is poor and contradictory evidence for its use in this regard.
TEBT to monitor anesthesia in neonates
General as well as epidural anesthesia may compromise CO in neonates106,107. The association between neurological adverse outcomes and neonatal anesthesia remains controversial108. It may therefore be beneficial to monitor multiple hemodynamic parameters during neonatal anesthesia and surgery.
TEBT has been used in few neonatal studies in general anesthesia109,110,111 (supplementary data).
TEBT monitoring during induction of anesthesia showed a reduction in CI 1 min or more prior to changes in HR and systolic blood pressure110. During general anesthesia in children, including neonates, continuous TEBT monitoring showed that desaturations were associated with decreases in SV index (SVI) with no effect on CI109.
Etomidate induction in neonates/infants with congenital heart disease showed no CI changes111. CI also did not change pre and post caudal block in infants (including preterm infants) undergoing minor abdominal surgery112. The researchers acknowledged that TEBT should be considered as a trend monitor with limitations in measurement of acute hemodynamic changes and low flow states.
Recommendation
TEBT should not be used to monitor neonates undergoing anesthesia due to contradictory data. Hemodynamic monitoring during neonatal anesthesia and surgery is feasible and may provide insights into longitudinal hemodynamic changes. However, it is limited by the lack of evidence to determine acute changes. This requires more research prior to use in clinical practice.
TEBT for pharmacological monitoring
Hemodynamic monitoring has been used to quantify drug reactions112,113. Due to the possibility of various hemodynamic effects of medications on the neonate, this may improve safety and allow for patient-specific modifications in therapy.
Few and varying pharmacological studies have utilized TEBT (supplementary data).
Caffeine has been shown to decrease many prematurity-related diseases113. Neither routine nor early caffeine (<2 h of age) has been shown to affect CO as measured by TTE or TEBT114.
Sodium bicarbonate is often used in persistent metabolic acidosis with the assumption that resolution of acidosis may improve cardiac contractility115. TEBT-CO showed no improvement in CO during sodium bicarbonate administration despite cerebral and systemic vasodilatation116.
Intubation premedication (atropine, morphine/fentanyl, and cisatrucurium) showed no change in TEBT-CO as well as showing no association between changes in BP and CO56.
An interventional hemodynamic trial assessing the effectiveness of inhaled nitric oxide or milrinone for pulmonary hypertension was terminated early due to futility, but showed no differences in CO and SVR between treatment and placebo groups117.
Recommendation
TEBT should not be used to monitor hemodynamic parameters during or after any type of pharmacological management.
TEBT to monitor body position effects on CO
Few studies have utilized TEBT to determine CO changes during body position changes (supplementary data).
TEBT-CO and SV have been shown to decrease with an increase in SVR index (SVRI) in healthy term and preterm LBW infants when turned prone and to return to baseline when turned supine again118,119.
In infants with respiratory disorders, prone positioning has been shown to improve CO parameters in infants with RDS, but less so in infants with evolving BPD120.
Recommendation
TEBT may be able to be used for monitoring CO in various body positions but more research is required prior to routine implementation.
TEBT during neonatal transport
Very few studies have utilized TEBT during transport (supplementary data).
TEBT was shown to be feasible for ICU transports of neonatal and pediatric patient with transport itself not affecting the accuracy of TEBT121.
Recommendation
TEBT should not be used to monitor hemodynamics during transport due to a lack of evidence.
Factors affecting TEBT measurements
TEBT-derived SV and CO have been shown to be variably affected by maternal and neonatal factors: maternal diabetes75, modes of delivery (normal vaginal deliveries vs caesarean section)66,74, sex70, gestational age groups42,43,44,45 and birth weight44,45,63. Older technologies have also suggested that severe tachycardia may affect accuracy33.
Volume expansion, phlebotomies, and hematocrit have been shown to affect TEBT32,122. In a study, using older technology, the thoracic segment length was also noted to significantly affect TEBT-CO measurements, with a 3-fold increase in CO depending on which thoracic segment length calculation was used122.
Electrode position has been shown to affect measurement parameters in bioimpedance body weight measurements38,64,123. It is unknown whether electrode position may affect CO parameters when measuring CO and SV. The accuracy of anthropometric measurements has also been shown to affect how TEBT monitors calculate CO, where for every 1 cm change in length resulted in an SV change of 1.8–36% for preterm infants and 1.6–2% for term infants. Also, for every 100 g in weight change/error, the SV changed 5–7.1% for preterm infants and 1.5–1.8% for term infants for all weight ranges124.
Although TEBT has been stated to be feasible in various studies34,44,121, signals could not be acquired within the first minute in DCC and resuscitation studies68,77 and could take up to 3 min to be acquired67. Only 2 studies have looked at signal quality during continuous use of TEBT and showed poor maintenance of high signal quality68,69 with improvement only when TEBT data were averaged over 1 minute68. Few studies have been performed in neonates to determine signal artefacts but movement artefacts in infants, with subsequent electrode detachment and data loss, have been documented125.
Electrode durability may also affect signal quality and therefore reliability of TEBT values, although inter-patient variability also exists39,45. TEBT sensor size and placement may pose limitations on placement of other monitoring electrodes34. No skin breakdown has been noted with TEBT sensors73, but prolonged placement, similar to ECG sensors, may cause skin irritation as the sensors are similar126.
Significant differences exist in commercially available technologies based on published algorithms17,18,20. Available data for normal and reference ranges for CO and SV differ between technologies42,63,73. Older algorithms have also suggested that hematocrit may influence accuracy127,128 but has not been assessed in the newer algorithms.
There is also ongoing debate as to the true origin of TEBT signals, theoretical thorax models, and the effects of respiratory and movement artefacts129. Device-specific knowledge and continued algorithm adaptation is required and may contribute to future computer-aided diagnoses130.
Recommendation
TEBT may be dependent on various technology-related factors. Anthropometric data should be accurately entered into the monitor and sensor placement should be constantly evaluated. Technology-specific and disease-specific normal/ reference ranges require further research.
TEBT to monitor thoracic fluid content
EBT monitors are mostly utilized for monitoring CO and SV, together with SVR. However, TFC is another parameter that is present for monitoring by EBT. TFC is the sum of extravascular, intravascular and intrapleural fluid. In neonates during the transition phase, in the absence of a hydrops or other significant edema, it can be assumed that intrapleural fluid is absent. Pulmonary blood flow increases dramatically from intra- to extra-uterine life stabilizing after a few minutes, when functional residual capacity has been established131. Therefore, with the intrapleural component being negligible and the intravascular component stabilizing within the first minutes after birth (assuming adequate lung recruitment), TFC equates to extravascular lung fluid in the neonate.
TFC has been used to predict outcomes in critically ill children132, monitor fluid responsiveness in children with shock133 as well as monitoring fluid overload during hemodyalisis134. Few such studies are available in neonates (supplementary data).
TFC reference ranges show increasing TFC values with increasing gestational age63. TFC has also been shown to decrease in the first 15 min after delivery74, as well as during the subsequent 72–96 h63,135.
A few studies have studied TEBT-derived TFC during respiratory distress in neonates136,137,138. TFC may be able to be used as a tool to predict respiratory distress at birth and persisting to 24 h137 as well as differentiate RDS and TTN136,138. TFC cut-off values have been determined for predicting mechanical ventilation and bronchopulmonary dysplasia139.
TFC has also been shown to differ significantly between preterm infants post-RBC transfusion, and non-transfused infants91,140. TFC has also been shown to be able to differentiate between infants with hsPDA and those with restrictive or closing PDA141.
Recommendation
TEBT may be helpful in assessing longitudinal TFC changes. However technological differences and lack of normative data require further research prior to routine clinical use.
WHOLE-BODY EBT
Few studies using WBEBT have been performed in neonates (supplementary data).
Accuracy studies of WBEBT, compared to TTE, in infants showed contradictory evidence of accuracy and precision142,143,144.
Few clinical studies have utilized WBEBT. WEBT-derived SI and CI were shown to increase with increasing PDA size in preterm infants145.
Recommendation
WBEBT should not be used in neonates for CO monitoring due to a lack of evidence of accuracy. Further research comparing WBEBT to a standard reference method should be performed.
EBT in research
Comparison of CO and SV using the current commercially available EBT devices is not possible, and the results are difficult to pool. Algorithmic differences exist between technologies146, equating to a need for technology-specific normative data.
Significant heterogeneity exists in data reporting. Measurement units for CO (ml/kg/min, l/min), SV (ml, ml/kg) and CI (ml/kg/min, ml/min/m2) differ. Data reporting should be standardized with consistent units of measurement, preferably indexed to weight, to enable better clinical interpretation and application.
Device accuracy analysis should be performed using Bland Altman not correlation statistics. Trending accuracy should be reported as polar plots not as correlation or changes between time points statistics. This would allow improved comparison of data across studies.
Numerous studies have used TEBT to longitudinally track hemodynamic variables but have used variable time periods, absolute changes, percentage changes as well as changes from baseline45,52,55,56,57,58,63,72,73,80,88,91,92,93,98,100,101,102,104. Future studies could utilize this technology to study longitudinal hemodynamic changes after interventions or for disease progression/improvement but require standardization of change parameters (i.e., changes from baseline) to allow individualization of management as well as improved comparison of study data. Longitudinal hemodynamic changes should be defined a priori. Consideration should be given to what may be clinically applicable changes from baseline (e.g., 20% change in CO from baseline) indicative of improvement or deterioration or response to therapy.
EBT-derived CO and SV can currently only be recommended in the context of research. Absolute value comparison of CO, SV, SVR, and TFC between studies cannot be recommended.
Discussion
EBT offers a non-invasive, minimal expertise required solution for hemodynamic monitoring of CO, SV, SVR, and TFC. With hemodynamic monitoring, the goal of early identification of systemic decompensation may be achievable, which may in turn, if adequately treated, improve neonatal outcomes. Non-invasive measurement of CO would be ideal in the NICU as it would enable continuous measurement of a parameter that reflects systemic perfusion. Numerous data have shown the inability of clinical and laboratory data to predict or timeously detect hemodynamic compromise in neonates25. Ensuring adequate CO, and thus systemic perfusion, may prevent numerous adverse outcomes6.
However, there are numerous limitations to the use of current EBT systems for routine use in clinical practice.
EBT, as compared to TTE, lacks accuracy and precision. TTE, commonly used in neonatology147,148, is itself inaccurate149 and does not represent a true reference standard for accuracy comparison. However, there are currently no better reference methods with which to determine EBT’s accuracy in neonates. Despite numerous studies regarding absolute accuracy of TEBT, only two studies have investigated trending accuracy and showed a poor trending ability. Future research should aim at determining a more accurate comparator for these devices to establish the true accuracy of EBT.
Many studies have reported hemodynamic parameters in various units of measurement. This should be standardized across research to enhance comparison and understanding as to applications in clinical practice (e.g., CO in ml/kg/min and SV in ml). Data analysis also varies with variable reporting methods, despite set standards for data reporting150,151. These methodological flaws also need to be addressed in future research.
In TTE, low CO has been defined62. However, due to the inaccuracies of EBT and varying technologies, this value may not be relevant. Further research is required to determine what TEBT- or WBEBT-values may represent a low CO requiring intervention. The use of the patient’s baseline measurements to determine individual variations and changes from baseline may be of more use, clinically, than absolute values. This requires more research.
The wide application of EBT, as well as ongoing research of use of TEBT in monitoring RBC transfusion for anemia45,152,153, respiratory disease monitoring154, ventilation monitoring155,156 and determining end-organ perfusion157, is a testament to the need for EBT-determined CO monitoring in neonates. However, the heterogenicity of studies consisting of infants of different gestation, postnatal age, birth weights, undergoing various physiological changes and pathophysiological processes and subjected to various interventions, contributes to the inability to determine normality and determine the effect of abnormality in these studies49,51. It also complicates the ability to accurately compare the accuracy of these devices. Although this would be representative of the “true state” of the neonates who most require CO monitoring, it complicates the ability of using these devices in routine practice. Research in the use of WBEBT in neonates is also ongoing, showing the continuing need for improved EBT technology and continuing need for non-invasive CO monitoring158.
Similar to problems encountered in NIRS monitoring159, this lack in accuracy may suggest that each patient (neonate) should be used as their own control, and changes from an individual baseline may provide information that could be used in clinical practice. Few neonatal studies have used changes from baseline to determine individual patient response to management or medical events80. One such paediatric study does exist106, which showed large ranges in intra-individual variability (46–56%) with changes from baseline varying between 62% and 126%. These changes may represent biological variability requiring an individualized approach to CO monitoring. This needs to be further researched with the inclusion of long-term outcomes to determine effects of physiology.
The heterogeneity of patient populations, diverse disease processes, and intra-individual variability may lend itself to the practice of precision medicine in neonatology, enabling precise and patient-specific tailored management of a disease160. TEBT may enable this approach, allowing for individualized hemodynamic management161. More research, however, is still required to overcome the current lack of accuracy and trending ability, lack of normal or reference ranges, and lack of data of what constitutes a clinically relevant change in baseline. TTE should be performed in all neonates where EBT is used, to determine cardiac anatomy, and function as well as to verify any changes in EBT.
Few neonatal studies are available showing that specific hemodynamic monitoring leads to improved outcome. This is also true of adult medicine162. Similar to adults, there is a need for disease-specific and process-specific research and clinical trials to use patient-centered outcomes to effectively monitor patients and rapidly detect instability. Some adult goal-directed fluid management continuous CO monitoring studies have shown decreased morbidities163, decreased cost164,165, no increase in costs163 and decrease in hospitalization and hospitalization-associated costs166. A systematic review showed that pre-operative hemodynamic optimization via various methods, was cost effective, would increase efficiency of health systems, and decrease the burden on public health systems156. No such studies have been performed in children or neonates. There may, therefore, be an economic advantage in using TEBT. Further research is required in this field.
Conclusion
EBT holds potential for CO monitoring and improvement in neonatal hemodynamic care. However, a lack of accuracy, lack of safety parameters (what EBT-CO is too low?), biological variability and diversity of reported research data negate the possibility for the recommendation of the use of EBT in routine clinical practice.
Further technical improvement and deeper understanding of technological algorithms are required. Further research is required before EBT can be recommended to be implemented into routine clinical practice.
EBT should currently only be used in research to determine accuracy, safety margins and long-term clinical outcomes based on these parameters.
Numerous research opportunities exist in EBT-determined hemodynamic monitoring (Table 4) and require attention prior to rolling out these monitors to routine practice.
References
Marik, P. E. Noninvasive Cardiac Output Monitors: A State-of The-art Review. J. Cardiothorac. Vasc. Anesthesia 27, 121–134 (2013).
Beausoleil, T. P., Janaillac, M., Barrington, K. J., Lapointe, A. & Dehaes, M. Cerebral oxygen saturation and peripheral perfusion in the extremely premature infant with intraventricular and/or pulmonary haemorrhage early in life. Sci. Rep. 8, 41598 (2018).
Vrancken, S. L., van Heijst, A. F. & de Boode, W. P. Neonatal hemodynamics: from developmental physiology to comprehensive monitoring. Front. Pediatr. 6, 1–15 (2018).
Azhibekov, T., Noori, S., Soleymani, S. & Seri, I. Transitional cardiovascular physiology and comprehensive hemodynamic monitoring in the neonate: relevance to research and clinical care. Semin. Fetal Neonatal Med. 19, 45–53 (2014).
Lee, A. J., Cohn, J. H. & Ranasinghe, J. S. Cardiac output assessed by invasive and minimally invasive techniques. Anesthesiol. Res. Pract. 2011, 475151 (2011).
McGovern, M. & Miletin, J. Cardiac output monitoring in preterm infants. Front. Pediatr. 6, 1–10 (2018).
Hadian, M. & Pinsky, M. R. Evidence-based review of the use of the pulmonary artery catheter: impact data and complications. Crit. Care 10, S8 (2006).
Kobe, J. et al. Cardiac output monitoring: technology and choice. Ann. Card. Anaesth. 22, 6–17 (2019).
Vrancken, S. L. et al. Estimation of extravascular lung water using the Transpulmonary Ultrasound Dilution (Tpud) method: a validation study in neonatal lambs. J. Clin. Monit. Comput. 30, 985–994 (2016).
Cecconi, M., Rhodes, A., Poloniecki, J., Della Rocca, G. & Grounds, R. M. Bench-to-bedside review: the importance of the precision of the reference technique in method comparison studies-with specific reference to the measurement of cardiac output. Crit. Care 13, 201 (2009).
Critchley, L. A. H. & Critchley, J. A. J. H. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J. Clin. Monit. Comput. 15, 85–91 (1999).
Critchley, L. A., Lee, A. & Ho, A. M. H. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth. Analg. 111, 1180–1192 (2010).
Kedrov, A. A. & Liberman, T. U. [Rheocardiography]. Klin. Med. 27, 40–46 (1949).
Kubicek, W. G., Karnegis, J. N., Patterson, R. P., Witsoe, D. A. & Mattson, R. H. Development and evaluation of an impedance cardiac output system. Aerosp. Med. 37, 1208–1212 (1966).
Jakovljevic, D. G., Trenell, M. I. & MacGowan, G. A. Bioimpedance and bioreactance methods for monitoring cardiac output. Best. Pract. Res. Clin. Anaesthesiol. 28, 381–394 (2014).
Electrical Cardiometry Technology (Ec) | Osypka Medical | Cardiotronic, <https://www.osypkamed.com/electrical-cardiometry-technology-ec> (
Us5735284a - Method and System for Non-Invasive Determination of the Main Cardiorespiratory Parameters of the Human Body - Google Patents, <https://patents.google.com/patent/US5735284A/en> (
Cybulski, G., Strasz, A., Niewiadomski, W. & Gasiorowska, A. Impedance cardiography: recent advancements. Cardiol. J. 19, 550–556 (2012).
Keren, H., Burkhoff, D. & Squara, P. Evaluation of a noninvasive continuous cardiac output monitoring system based on thoracic bioreactance. Am. J. Physiol. Heart Circ. Physiol. 293, 583–589 (2007).
Nguyen, L. S. & Squara, P. Non-invasive monitoring of cardiac output in critical care medicine. Front. Med. 4, 1–8 (2017).
Blencowe, H. et al. Born too soon: the global epidemiology of 15 Million preterm births. Reprod. Health 10, S2 (2013).
Larroque, B. et al. Survival of very preterm infants: epipage, a population based cohort study. Arch. Dis. Child. Fetal Neonatal Ed. 89, F139–F144 (2004).
Dempsey, E. M. & Barrington, K. J. Evaluation and treatment of hypotension in the preterm infant. Clin. Perinatol. 36, 75–85 (2009).
Wu, T. W. & Noori, S. Recognition and management of neonatal hemodynamic compromise. Pediatr. Neonatol. 62, S22–S29 (2021).
de Boode, W. P. Clinical monitoring of systemic hemodynamics in critically Ill newborns. Early Hum. Dev. 86, 137–141 (2010).
Tan, C. M. J. & Lewandowski, A. J. The transitional heart: from early embryonic and fetal development to neonatal life. Fetal Diagnosis Ther. 47, 373–386 (2020).
Davis, A. L. et al. American college of critical care medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit. Care Med. 45, 1061–1093 (2017).
Raju, T. N., Stevenson, D. K., Higgins, R. D. & Stark, A. R. Safe and effective devices and instruments for use in the neonatal intensive care units: nichd workshop summary. Biomed. Instrum. Technol. 43, 408–418 (2009).
Vincent, J. L. et al. Clinical review: update on hemodynamic monitoring - a consensus of 16. Crit. Care 15, 1–8 (2011).
Slagt, C., Breukers, R.-M. B. G. E. & Groeneveld, A. B. J. Choosing patient-tailored hemodynamic monitoring. Crit. Care 14 (2010).
Ebell, M. H. et al. Strength of Recommendation Taxonomy (Sort): a patient-centered approach to grading evidence in the medical literature - Pubmed. J. Am. Board Fam. Pract. 17, 59–67 (2004).
Costeloe, K., Stocks, J. & Godfrey, S. Cardiac output in the neonatal period using impedance cardiography. Pediatr. Res. 11, 1171–1177 (1977).
Tibballs, J. A comparative study of cardiac output in neonates supported by mechanical ventilation: measurement with thoracic electrical bioimpedance and pulsed doppler ultrasound. J. Pediatr. 114, 632–635 (1989).
Weisz, D. E., Jain, A., McNamara, P. J. & El-Khuffash, A. Non-invasive cardiac output monitoring in neonates using bioreactance: a comparison with echocardiography. Neonatology 102, 61–67 (2012).
Grollmuss, O. & Gonzalez, P. Non-invasive cardiac output measurement in low and very low birth weight: a method comparison. Front. Pediatr. 2, 16 (2014).
Noori, S., Drabu, B., Soleymani, S. & Seri, I. Continuous non-invasive cardiac output measurements in the neonate by electrical velocimetry: a comparison with echocardiography. Arch. Dis. Child. Fetal Neonatal Ed. 97, F340–F343 (2012).
Blohm, M. E. et al. Impedance cardiography (Electrical Velocimetry) and Transthoracic echocardiography for non-invasive cardiac output monitoring in pediatric intensive care patients: a prospective single-center observational study. Crit. Care 18, 603 (2014).
Song, R., Rich, W., Kim, J. H., Finer, N. N. & Katheria, A. C. The use of electrical cardiometry for continuous cardiac output monitoring in preterm neonates: a validation study. Am. J. Perinatol. 31, 1105–1110 (2014).
Weisz, D. E., Jain, A., Ting, J., McNamara, P. J. & El-Khuffash, A. Non-invasive cardiac output monitoring in preterm infants undergoing patent ductus arteriosus ligation: a comparison with echocardiography. Neonatology 106, 330–336 (2014).
Torigoe, T., Sato, S., Nagayama, Y., Sato, T. & Yamazaki, H. Influence of patent ductus arteriosus and ventilators on electrical velocimetry for measuring cardiac output in very-low/low birth weight infants. J. Perinatol. 35, 485–489 (2015).
Blohm, M. E., Hartwich, J., Obrecht, D., Kersten, J. F. & Singer, D. Effect of patent ductus arteriosus and patent foramen ovale on left ventricular stroke volume measurement by electrical velocimetry in comparison to transthoracic echocardiography in neonates. J. Clin. Monit. Comput. 31, 589–598 (2017).
Boet, A., Jourdain, G., Demontoux, S. & De Luca, D. Stroke volume and cardiac output evaluation by electrical cardiometry: accuracy and reference nomograms in hemodynamically stable preterm neonates. J. Perinatol. 36, 748–752 (2016).
Hsu, K.-H. et al. Electrical cardiometry to monitor cardiac output in preterm infants with patent ductus arteriosus: a comparison with echocardiography. Neonatology 112, 231–237 (2017).
Van Wyk, L., Smith, J., Lawrenson, J. & De Boode, W. P. W. P. W. P. Agreement of cardiac output measurements between bioreactance and transthoracic echocardiography in preterm infants during the transitional phase: a single-centre, prospective study. Neonatology 117, 271–278 (2020).
Lockhorst, C. Accuracy, reliability and applicability of electrical cardiometry for measuring cardiac output in critically Ill newborns. Masters thesis, Radboud UMC (2021). Available from https://essay.utwente.nl/88653/1/88653_Lokhorst_MA_TNW.pdf. Accessed on 15 May 2024
Xu, S. H., Zhang, J., Zhang, Y., Zhang, P. & Cheng, G. Q. Non-invasive cardiac output measurement by electrical cardiometry and M-mode echocardiography in the neonate: a prospective observational study of 136 neonatal infants. Transl. Pediatr. 10, 1757–1764 (2021).
Schwarz, C. E. et al. Agreement of cardiac output estimates between electrical cardiometry and transthoracic echocardiography in very preterm infants. Neonatology 119, 594–601 (2022).
Hassan, M. A., Bryant, M. B. & Hummler, H. D. Comparison of cardiac output measurement by electrical velocimetry with echocardiography in extremely low birth weight neonates. Neonatology 119, 18–25 (2022).
Van Wyk, L., Gupta, S., Lawrenson, J. & de Boode, W. P. Accuracy and trending ability of electrical biosensing technology for non-invasive cardiac output monitoring in neonates: a systematic qualitative review. Front. Pediatr. 10, 851850 (2022).
Mansfield, R. C. et al. Cardiac output measurement in neonates and children using noninvasive electrical bioimpedance compared with standard methods: a systematic review and meta-analysis. Crit. Care Med. 50, 126–137 (2022).
O’Neill, R., Dempsey, E. M., Garvey, A. A. & Schwarz, C. E. Non-invasive cardiac output monitoring in neonates. Front. Pediatr. 8, 614585 (2021).
Grollmuss, O., Demontoux, S., Capderou, A., Serraf, A. & Belli, E. Electrical velocimetry as a tool for measuring cardiac output in small infants after heart surgery. Intensive Care Med. 38, 1032–1039 (2012).
Muniru, I., Grobler, J. & Wyk, L. V. A Novel model for real-time monitoring of Ivh in preterm neonates using Non-Invasive Cardiac Output (Nicom) parameters and uber architecture for special event forecasting. The Global Health Network Collections https://doi.org/10.21428/3d48c34a.2406c195 (2023).
Evans, N. Preterm patent ductus arteriosus: a continuing conundrum for the neonatologist? Semin. Fetal Neonatal Med. 20, 272–277 (2015).
Katheria, V. et al. Early prediction of a significant patent ductus arteriosus in infants <32 weeks gestational age. J. Neonatal Perinat. Med. 11, 331–334 (2018).
Truong, L., Kim, J. H., Katheria, A. C., Finer, N. N. & Marc-Aurele, K. L. Haemodynamic effects of premedication for neonatal intubation: an observational study. Arch. Dis. Child. Fetal Neonatal Ed. 105, 123–127 (2020).
Lien, R., Hsu, K.-H., Chu, J.-J. & Chang, Y.-S. Hemodynamic alterations recorded by electrical cardiometry during ligation of ductus arteriosus in preterm infants. Eur. J. Pediatr. 174, 543–550 (2015).
Gatelli, I. F. et al. Electrical cardiometry in monitoring percutaneous closure of ductus arteriosus in preterm infants: a case study on five patients. Eur. J. Pediatr. 181, 2319–2328 (2022).
Rodríguez Sánchez de la Blanca, A., Sánchez Luna, M., González Pacheco, N., Arriaga Redondo, M. & Navarro Patiño, N. Electrical velocimetry for non-invasive monitoring of the closure of the ductus arteriosus in preterm infants. Eur. J. Pediatr. 177, 229–235 (2018).
Hsu, K. H. et al. Baseline cardiac output and its alterations during ibuprofen treatment for patent ductus arteriosus in preterm infants. BMC Pediatr. 19, 1–8 (2019).
Evans, N. & Kluckow, M. Early determinants of right and left ventricular output in ventilated preterm infants. Arch. Dis. Child. 74, 88–94 (1996).
de Waal, K. A. The methodology of doppler-derived central blood flow measurements in newborn infants. Int. J. Pediatr. 2012, 1–13 (2012).
Hsu, K. H. et al. Hemodynamic reference for neonates of different age and weight: a pilot study with electrical cardiometry. J. Perinatol. 36, 481–485 (2016).
Sexson, W. R., Gotshall, R. W. & Miles, D. S. Cardiothoracic variables measured by bioelectrical impedance in preterm and term neonates. Crit. Care Med. 19, 1054–1059 (1991).
Van Laere, D. et al. Monitoring circulation during transition in extreme low gestational age newborns: what’s on the horizon? Front. Pediatr. 6, 1–6 (2018).
Freyschuss, U., Noack, G. & ZetterstrÖM, R. Serial measurements of thoracic bioimpedance and cardiac output in healthy neonates after normal delivery and caeseran section. Acta Pediatr. 68, 357–362 (1979).
McCarthy, K. N. et al. Feasibility of non-invasive cardiac output monitoring at birth using electrical bioreactance in term infants. Arch. Dis. Child. Fetal Neonatal Ed. 106, 431–434 (2020).
Freidl, T. et al. Haemodynamic transition after birth: a new tool for non-invasive cardiac output monitoring. Neonatology 111, 55–60 (2016).
Schwarz, C. E., O’Toole, J. M., Livingstone, V., Pavel, A. M. & Dempsey, E. M. Signal quality of electrical cardiometry and perfusion index in very preterm infants. Neonatology 118, 672–677 (2021).
Baik-Schneditz, N. et al. Sex related difference in cardiac output during neonatal transition in term neonates. Cardiovasc. Diagnosis Ther. 11, 342–347 (2021).
Baik-Schneditz, N. et al. Cardiac output and cerebral oxygenation in term neonates during neonatal transition. Children 8, 439 (2021).
Cappelleri, A. et al. Myocardial function in late preterm infants during the transitional period: comprehensive appraisal with deformation mechanics and non-invasive cardiac output monitoring. Cardiol. Young. 30, 249–255 (2020).
Van Wyk, L., Smith, J., Lawrenson, J., Lombard, C. J. & de Boode, W. P. Bioreactance-derived haemodynamic parameters in the transitional phase in preterm neonates: a longitudinal study. J. Clin. Monit. Comput. 36, 861–870 (2022).
Metwalli, E. M., Eldin, Z. E., Aly, H., Soliman, R. M. & Massih, A. F. A. Hemodynamic trends in full term newborns versus late preterms during transition. Int. J. Health Sci. 6, 103–115 (2022).
Freyschuss, U., Gentz, J., Noack, G. & Persson, B. Circulatory adaptation in newborn infants of strictly controlled diabetic mothers. Acta Paediatr. Scandinavica 71, 209–215 (1982).
Soliman, R. M. et al. A randomized controlled trial of a 30- versus a 120-Second delay in cord clamping after term birth. Am. J. Perinatol. 41, 739–746 (2022).
Katheria, A. C., Truong, G., Cousins, L., Oshiro, B. & Finer, N. N. Umbilical cord milking versus delayed cord clamping in preterm infants. Pediatrics 136, 61–69 (2015).
Kagiya, A. et al. The evaluation of systolic time intervals and impedance cardiogram of neonates. Nippon Sanka Fujinka Gakkai zasshi 41, 601–608 (1989).
Katheria, A. et al. Neonatal resuscitation with an intact cord: a randomized clinical trial. J. Pediatrics 178, 75–80.e73 (2016).
Martini, S. et al. Cardiovascular and cerebrovascular responses to cardio-respiratory events in preterm infants during the transitional period. J. Physiol. 598, 4107–4119 (2020).
Bhombal, S. & Noori, S. Hemodynamic management in chronically ventilated infants. Semin. Fetal Neonatal Med. 24, 101038 (2019).
Bugiera, M., Szczapa, T., Sowińska, A., Roehr, C. C. & Szymankiewicz-Brȩborowicz, M. Cerebral oxygenation and circulatory parameters during pressure-controlled vs volume-targeted mechanical ventilation in extremely preterm infants. Adv. Clin. Exp. Med. 29, 1325–1329 (2020).
Rachel, M., Jan, M., Heather, C. & Jana, S. Non-invasive cardiac output monitoring before and after baby extubation – a feasibility study (Nicombabe Study). Early Hum. Dev. 170, 105605 (2022).
Ahmed Elmazzahy, E., Zoheir Elhouchi, S., Samir Khater, E. & Amin Ahmed, K. Electric cardiometry is not predictive of outcome in full-term newborns with respiratory distress: a single center study. Pediatr. Sci. J. 3, 91–97 (2023).
Noack, G. & Freyschuss, U. The early detection of pneumothorax with transthoracic impedaqnce in newborn infants. Acta Pædiatr. 66, 677–680 (1977).
Kharrat, A. & Jain, A. Hemodynamic dysfunction in neonatal sepsis. Pediatr. Res. 91, 413–424 (2022).
Gatelli, I. F. et al. Neonatal septic shock and hemodynamic monitoring in preterm neonates in a nicu: added value of electrical cardiometry in real-time tailoring of management and therapeutic strategies. Am. J. Perinatol. 39, 1401–1404 (2021).
Abdou, N. I. et al. Efficacy of electrical cardiometry in hemodynamic status monitoring of septic preterm neonates: a quasi experimental study. Res. Square (2023). Available at https://www.researchsquare.com/article/rs-2801297/v1. Accessed on 15 May 2024
Quante, M. et al. Effects of anaemia on haemodynamic and clinical parameters in apparently stable preterm infants. Blood Transfus. 11, 227–232 (2013).
Jain, D. et al. Cerebral oxygenation in preterm infants receiving transfusion. Pediatr. Res. 85, 786–789 (2019).
Weaver, B. et al. Hemodynamics and perfusion in premature infants during transfusion. AACN Adv. Crit. Care 29, 126–137 (2018).
Miletin, J., Semberova, J., Martin, A. M. A. M., Janota, J. & Stranak, Z. Low cardiac output measured by bioreactance and adverse outcome in preterm infants with birth weight less than 1250 G. Early Hum. Dev. 149, 105153 (2020).
Miletin, J. Low Cardiac Output in Extremely Low Gestation Age Neonates and Intraventricular Haemorrhage PhD thesis (University of Karlova, 2021).
Schwarz, C. E. et al. Electrical cardiometry during transition and short-term outcome in very preterm infants: a prospective observational study. Eur. J. Pediatr. 183, 1629–1636 (2024).
Hsu, K. H. et al. Cerebral hemodynamics and regional oxygen metabolism during ductus arteriosus ligation in preterm infants. Neonatology 119, 703–711 (2022).
Muniru, I. O., Grobler, J. & Van Wyk, L. Detecting intra ventricular haemorrhage in preterm neonates using lstm autoencoders. In Bioinformatics and Biomedical Engineering. IWBBIO 2023. Lecture Notes in Computer Science (Eds Rojas, I., Valenzuela, O., Rojas Ruiz, F., Herrera, L. J. & Ortuño, F.) 455–468 (Springer Verlag, Berlin, Germany, 2023)
Ovali, F. Hemodynamic changes and evaluation during hypoxic-ischemic encephalopathy and therapeutic hypothermia. 167, 105563 (2022).
Eriksen, V. R., Trautner, S., Hahn, G. H. G. H. & Greisen, G. Lactate acidosis and cardiac output during initial therapeutic cooling in asphyxiated newborn infants. PLoS ONE 14, 1–12 (2019).
Breatnach, C. The Assessment of Myocardial Performance and the Impact of Pathological Processes on Cardiac Adaptation in the Neonatal Population Using Functional Echocardiography PhD thesis, Royal College of Surgeons of Ireland, (2018).
Forman, E. et al. Noninvasive continuous cardiac output and cerebral perfusion monitoring in term infants with neonatal encephalopathy: assessment of feasibility and reliability. Pediatr. Res. 82, 789–795 (2017).
Wu, T. W., Tamrazi, B., Soleymani, S., Seri, I. & Noori, S. Hemodynamic changes during rewarming phase of whole-body hypothermia therapy in neonates with hypoxic-ischemic encephalopathy. J. Pediatr. 197, 68–74 (2018).
Garvey, A. A. et al. Non-invasive continuous cardiac output monitoring in infants with hypoxic ischaemic encephalopathy. J. Perinatol. 42, 1622–1629 (2022).
Balog, V. et al. Time series analysis of non-invasive hemodynamic monitoring data in neonates with hypoxic-ischemic encephalopathy. Front. Pediatr. 11, 1112959 (2023).
Gatelli, I. F., Vitelli, O., Chiesa, G., De Rienzo, F. & Martinelli, S. Noninvasive cardiac output monitoring in newborn with hypoplastic left heart syndrome. Am. J. Perinatol. 37, S54–S55 (2020).
Soaida, S. M., Hanna, M. G., Mahmoud, A. R. & Elmetwally, S. A. Electrical velocimetry (Icon cardiometry) assessment of hemodynamic changes associated with different inflation pressures during pediatric thoracoscopic surgery: a pilot study. Egypt. J. Cardiothorac. Anesth. 15, 3 (2021).
Falciola, V., Donath, S. M., Roden, E., Davidson, A. & Vutskits, L. Noninvasive cardiac output monitoring during anaesthesia and surgery in young children using electrical cardiometry: an observational study. Br J Anaesth. 128, e235–e238 (2022).
Triffterer, L. et al. An observational study of the macro- and micro-haemodynamic implications of epidural anaesthesia in children. Anaesthesia 72, 488–495 (2017).
Yu, D., Li, L. & Yuan, W. Neonatal anesthetic neurotoxicity: insight into the molecular mechanisms of long-term neurocognitive deficits. 87, 196–199 (2017).
King, M. R. et al. Age-related incidence of desaturation events and the cardiac responses on stroke index, cardiac index, and heart rate measured by continuous bioimpedance noninvasive cardiac output monitoring in infants and children undergoing general anesthesia. J. Clin. Anesth. 32, 181–188 (2016).
Coté, C. J. C. J. et al. Continuous noninvasive cardiac output in children: is this the next generation of operating room monitors? Initial Experience in 402 pediatric patients. Paediatr. Anaesth. 25, 150–159 (2015).
Dennhardt, N. et al. Effect of etomidate on systemic and regional cerebral perfusion in neonates and infants with congenital heart disease: a prospective observational study. Paediatr. Anaesth. 30, 984–989 (2020).
Beck, C. E. et al. Systemic and regional cerebral perfusion in small infants undergoing minor lower abdominal surgery under awake caudal anaesthesia: an observational study. Eur. J. Anaesthesiol. 37, 696–700 (2020).
Kua, K. P. & Lee, S. W. H. Systematic review and meta-analysis of clinical outcomes of early caffeine therapy in preterm neonates. Br. J. Clin. Pharmacol. 83, 180–191 (2017).
Katheria, A. C. et al. A pilot randomized controlled trial of early versus routine caffeine in extremely premature infants. Am. J. Perinatol. 32, 879–886 (2015).
Kimmoun, A., Novy, E., Auchet, T., Ducrocq, N. & Levy, B. Hemodynamic consequences of severe lactic acidosis in shock states: from bench to bedside. Crit Care. 19, 175 (2015).
Katheria, A. C. et al. Hemodynamic effects of sodium bicarbonate administration. J. Perinatol. 37, 518–520 (2017).
El-Khuffash, A. et al. The use of milrinone in neonates with persistent pulmonary hypertension of the newborn - a randomised controlled trial pilot study (Mint 1). J. Perinatol. 43, 168–173 (2023).
Wu, T. W., Lien, R. I., Seri, I. & Noori, S. Changes in cardiac output and cerebral oxygenation during prone and supine sleep positioning in healthy term infants. Arch. Dis. Child. Fetal Neonatal Ed. 102, F483–F489 (2017).
Ma, M. et al. Prone positioning decreases cardiac output and increases systemic vascular resistance in neonates. J. Perinatol. 35, 424–427 (2015).
Loi, B. et al. Respiratory and haemodynamic effects of 6h-pronation in neonates recovering from respiratory distress syndrome, or affected by acute respiratory distress syndrome or evolving bronchopulmonary dysplasia: a prospective, physiological, crossover, controlled. eClinicalMedicine 55, 101791 (2023).
Boet, A. et al. Basic hemodynamic monitoring using ultrasound or electrical cardiometry during transportation of neonates and infants. Pediatr. Crit. Care Med. 18, e488–e493 (2017).
Belik, J. & Pelech, A. Thoracic electric bioimpedance measurement of cardiac output in the newborn infant. J. Pediatr. 113, 890–895 (1988).
Toledo, L. F. M., Medeiros, T. R., Vieira, A. A. & Coca Velarde, L. G. Evaluation of the bioimpedance technique in newborns with a focus on electrode positioning: a prospective, randomized, crossover study. Nutr. Clin. Pract. 37, 1458–1463 (2022).
Healy, D. B., Dempsey, E. M., O’toole, J. M. & Schwarz, C. E. In-silico evaluation of anthropomorphic measurement variations on electrical cardiometry in neonates. Children 8, 936–936 (2021).
Iddawela, S. et al. Non-invasive cardiac output monitoring with electrical velocimetry after cardiac surgery in infants. Ann. R. Coll. Surg. Engl. 104, 583–587 (2022).
Anton, O. et al. Heart rate monitoring in newborn babies: a systematic review. Neonatology 116, 199–210 (2019).
Costeloe, K. L. et al. Short-term outcomes after extreme preterm birth in England: comparison of two birth cohorts in 1995 and 2006 (the Epicure Studies). BMJ 345, e7976 (2012).
Mohapatra, S. N., Costeloe, K. L., & Hill, D. W. Blood resistivity and its implications for the calculation of cardiac output by the thoracic electrical impedance technique. Intensive Care Med. 3, 63–67 (1977).
Mansouri, S., Alhadidi, T., Chabchoub, S. & Salah, R. B. Impedance cardiography: recent applications and developments. Biomed. Res. 29, 3542–3552 (2018).
Chabchoub, S., Mansouri, S. & Salah, R. B. Signal processing techniques applied to impedance cardiography Icg signals - a review. J. Med. Eng. Technol. 46, 243–260 (2022).
Hooper, S. B., Polglase, G. R. & Roehr, C. C. Cardiopulmonary changes with aeration of the newborn lung. Paediatr. Respir. Rev. 16, 147–150 (2015).
Sumbel, L. et al. Thoracic Fluid Content (Tfc) measurement using impedance cardiography predicts outcomes in critically Ill children. Front. Pediatr. 8, 564902 (2021).
Awadhare, P. et al. Non-invasive cardiac output monitoring and assessment of fluid responsiveness in children with shock in the emergency department. Front. Pediatr. 10, 857106 (2022).
Wilken, M., Oh, J., Pinnschmidt, H. O., Singer, D. & Blohm, M. E. Effect of hemodialysis on impedance cardiography (Electrical Velocimetry) parameters in children. Pediatr. Nephrol. 35, 669–676 (2020).
Van Wyk, L., Smith, J., De Boode, W.-P. & Lawrenson, J. Non-Invasive Cardiac Output Monitoring in Preterm Neonates PhD thesis, Stellenbosch University, (2021).
Yoon, S. J. et al. Tools for assessing lung fluid in neonates with respiratory distress. BMC Pediatr. 22, 354 (2022).
Paviotti, G., De Cunto, A., Moressa, V., Bettiol, C. & Demarini, S. Thoracic fluid content by electric bioimpedance correlates with respiratory distress in newborns. J. Perinatol. 37, 1024–1027 (2017).
Bassiouny, M. R., Abdelhady, S. E. & Sobh, A. Thoracic fluid content in neonates presented with respiratory distress as a predictive tool for transient tachypnea of newborn. Am. J. Perinatol. 41, e109–e113 (2024).
Martini, S. et al. Prediction of respiratory distress severity and bronchopulmonary dysplasia by lung ultrasounds and transthoracic electrical bioimpedance. Eur. J. Pediatr. 182, 1039–1047 (2023).
Chakkarapani, A. A. et al. A comparison between electrical velocimetry and echocardiography on cardiac output measurement before and after packed TBC transfusion in extreme preterms by Bland Altman analysis in 32nd Annual Meeting of the European Society of Paediatric and Neonatal Intensive Care, Greece, 2023.
Martini, S. et al. Impact of patent ductus arteriosus on non-invasive assessments of lung fluids in very preterm infants during the transitional period. Eur. J. Pediatr. 182, 4247–4251 (2023).
Mansfield, R., Sathiyamurthy, S., Lees, C. & Banerjee, J. 1253 Noninvasive continuous stroke volume monitoring in term and late preterm neonates using whole body electrical bioimpedance: a clinical validation study. Arch. Dis. Child Fetal Neonatal. Ed. 106, A293–A294 (2021).
Banerjee, J. et al. Continuous non-invasive measurement of cardiac output in neonatal intensive care using regional impedance cardiography: a prospective observational study. Arch. Dis. Child Fetal Neonatal. Ed. 109, 450–455 (2023).
Beck, R., Milella, L. & Labellarte, C. Continuous non-invasive measurement of stroke volume and cardiac index in infants and children: comparison of impedance cardiography Nicas® Vs Cardioq® Method. La Clin. terapeutica 169, e110–e113 (2018).
Rafaeli Rabin, R., Rosin, I., Matitiau, A., Simpson, Y. & Flidel-Rimon, O. Assessing Patent Ductus Arteriosus (Pda) significance on cardiac output by whole-body bio-impedance. Pediatr. Cardiol. 41, 1386–1390 (2020).
Jakovljevic, D. G. et al. Comparison of Cardiac output determined by bioimpedance and bioreactance methods at rest and during exercise. J. Clin. Monit. Comput. 26, 63–68 (2012).
Roehr, C. C. et al. Investigating the European perspective of neonatal point-of-care echocardiography in the neonatal intensive care unit - a pilot study. Eur. J. Pediatr. 172, 907–911 (2013).
El-Khuffash, A., Herbozo, C., Jain, A., Lapointe, A. & McNamara, P. J. Targeted Neonatal Echocardiography (Tnecho) service in a canadian neonatal intensive care unit: a 4-year experience. J. Perinatol. 33, 1–4 (2013).
Wetterslev, M., Møller-Sørensen, H., Johansen, R. R. & Perner, A. Systematic review of cardiac output measurements by echocardiography vs. thermodilution: the techniques are not interchangeable. Intensive Care Med. 42, 1223–1233 (2016).
Odor, P. M., Bampoe, S. & Cecconi, M. Cardiac output monitoring: validation studies–how results should be presented. Curr. Anesthesiol. Rep. 7, 410–415 (2017).
Squara, P., Cecconi, M., Rhodes, A., Singer, M. & Chiche, J. D. Tracking changes in cardiac output: methodological considerations for the validation of monitoring devices. Intensive Care Med. 35, 1801–1808 (2009).
Chakkarapani, A. A. et al. Trends of Systemic Hemodynamic parameters measured by Electrical Velocimetry before, during, and after Packed RBC Transfusion in Extreme Preterms: A Single Centre Prospective Clinical Trial in 32nd Annual meeting of the European Society of Paediatric and Neonatal Intensice Care, Athens, Greece, 2023.
Chakkarapani, A. A. S. et al. A Decomposing Time Series Model Analysis of minute-to-minute data for the Effect of Packed Red Blood Cell Transfusion on Systemic Hemodynamics measured by Electrical Velocimetry in Extreme Preterms in Pediatric Academic Societies, Washington, 2023.
Van Wyk, L., Smith, J., Lawrenson, J., Lombard, C. J. & de Boode, W.-P. Bioreactance-derived thoracic fluid content (TFC) and respiratory distress in preterm infants in Joint European Neonatal Societies, Rome, Italy, 2023.
Weaver, B. S. PhD Thesis. Electrical Cardiometry during Mechanical Ventilation: An Exploratory Study. The Catholic University Of America, (2021). Available at https://www.proquest.com/docview/2622955510. Accessed on 15 May 2024.
DeBenedictis, N. & LaGamma, E. F. Continuous Hemodynamic Monitoring of Cardiac Output (CO) to Assess Extubation Readiness Characteristics in Very Low Birth Weight Infants in Pediatric Academic Societies, Washington, 2023.
Long, E. L. et al. Noninvasive Measurements of Cardiac Hemodynamic and Tissue Perfusion Indices in Normal Infants. Presentation 9 (Biostatistics Faculty Presentations). Available at https://digitalcommons.georgiasouthern.edu/biostat-facpres/92. Accessed on 15 May 2024.
Banerjee, J. Non-invasive Continuous Cardiac Output Monitoring in Preterm Infants Study. Available at https://clinicaltrials.gov/study/NCT04064177. Accessed on 15 May 2024.
Levy, P. T. et al. Near-infrared spectroscopy for perioperative assessment and neonatal interventions. Pediatr. Res. 90, 1–11 (2021).
Allegaert, K. & Simons, S. H. P. Editorial: precision medicine in neonates. Front. Pediatr. 9, 702760 (2021).
de Boode, W. P. Individualized hemodynamic management in newborns. Front. Pediatr. 8, 580470 (2020).
Pinsky, M. R. & Payen, D. Functional hemodynamic monitoring. Crit. Care 9, 566–572 (2005).
Jin, J., Min, S., Liu, D., Liu, L. & Lv, B. Clinical and economic impact of goal-directed fluid therapy during elective gastrointestinal surgery. Perioperative Med. 7, 22–30 (2018).
Sadique, Z., Harrison, D. A., Grieve, R., Rowan, K. M. & Pearse, R. M. Cost-effectiveness of a cardiac output-guided haemodynamic therapy algorithm in high-risk patients undergoing major gastrointestinal surgery. Perioperative Med. 4, 13 (2015).
Legrand, G., Ruscio, L., Benhamou, D. & Pelletier-Fleury, N. Goal-directed fluid therapy guided by cardiac monitoring during high-risk abdominal surgery in adult patients: cost-effectiveness analysis of esophageal doppler and arterial pulse pressure waveform analysis. Value Health 18, 605–613 (2015).
Benes, J., Zatloukal, J., Simanova, A., Chytra, I. & Kasal, E. Cost Analysis of the stroke volume variation guided perioperative hemodynamic optimization - an economic evaluation of the svvopt trial results. BMC Anesthesiol. 14, 40–48 (2014).
Funding
Open access funding provided by Stellenbosch University.
Author information
Authors and Affiliations
Consortia
Contributions
Conception and design: L.v.W., S.G.; acquisition of data: L.v.W., S.G.; drafting of article: L.v.W., S.G.; revision of article: all authors; approval of final manuscript: all authors. Large language models have not been used in this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Wyk, L., Austin, T., Barzilay, B. et al. A recommendation for the use of electrical biosensing technology in neonatology. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03369-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03369-z
- Springer Nature America, Inc.