Abstract
Objective
To determine the validity of diagnostic hospital billing codes for complications of prematurity in neonates <32 weeks gestation.
Study Design
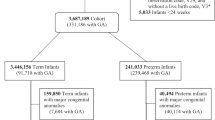
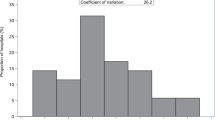
Retrospective cohort data from discharge summaries and clinical notes (n = 160) were reviewed by trained, blinded abstractors for the presence of intraventricular hemorrhage (IVH) grades 3 or 4, periventricular leukomalacia (PVL), necrotizing enterocolitis (NEC), stage 3 or higher, retinopathy of prematurity (ROP), and surgery for NEC or ROP. Data were compared to diagnostic billing codes from the neonatal electronic health record.
Results
IVH, PVL, ROP and ROP surgery had strong positive predictive values (PPV > 75%) and excellent negative predictive values (NPV > 95%). The PPVs for NEC (66.7%) and NEC surgery (37.1%) were low.
Conclusion
Diagnostic hospital billing codes were observed to be a valid metric to evaluate preterm neonatal morbidities and surgeries except in the instance of more ambiguous diagnoses such as NEC and NEC surgery.
Similar content being viewed by others
Data availability
Data used in the creation of the dataset contains potentially sensitive information and restrictions on sharing of this information is managed by the University of Iowa’s Institutional Review Board. The institutional point of contact for data request for this study is Nancy Weathers (Nancy-weathers@uiowa.edu).
References
Purisch SE, Gyamfi-Bannerman C, editors. Epidemiology of preterm birth. Seminars in perinatology; 2017: Elsevier.
Shapiro-Mendoza CK, Lackritz EM, editors. Epidemiology of late and moderate preterm birth. Seminars in Fetal and Neonatal Medicine; 2012: Elsevier.
Baron IS, Litman FR, Ahronovich MD, Baker R. Late preterm birth: a review of medical and neuropsychological childhood outcomes. Neuropsychol Rev. 2012;22:438–50.
World Health Organization. Preterm Birth 2018. https://www.who.int/news-room/fact-sheets/detail/preterm-birth.
Patel RM. Short-and long-term outcomes for extremely preterm infants. Am J Perinatol. 2016;33:318–28.
Waitzman NJ, Jalali A, Grosse SD, editors. Preterm birth lifetime costs in the United States in 2016: An update. Seminars in Perinatology; 2021: Elsevier.
Ducharme R, Benchimol EI, Deeks SL, Hawken S, Fergusson DA, Wilson K. Validation of diagnostic codes for intussusception and quantification of childhood intussusception incidence in Ontario, Canada: a population-based study. J Pediatrics. 2013;163:1073–9.e3.
Fleet JL, Dixon SN, Shariff SZ, Quinn RR, Nash DM, Harel Z, et al. Detecting chronic kidney disease in population-based administrative databases using an algorithm of hospital encounter and physician claim codes. BMC Nephrol. 2013;14:1–8.
Moll K, Wong HL, Fingar K, Hobbi S, Sheng M, Burrell TA, et al. Validating claims-based algorithms determining pregnancy outcomes and gestational age using a linked claims-electronic medical record database. Drug Saf. 2021;44:1151–64.
Juhl S, Hansen M, Fonnest G, Gormsen M, Lambaek I, Greisen G. Poor validity of the routine diagnosis of necrotising enterocolitis in preterm infants at discharge. Acta Paediatrica. 2017;106:394–8.
Ford JB, Roberts CL, Algert CS, Bowen JR, Bajuk B, Henderson-Smart DJ. Using hospital discharge data for determining neonatal morbidity and mortality: a validation study. BMC Health Serv Res. 2007;7:1–8.
Joseph K, Fahey J. Validation of perinatal data in the Discharge Abstract Database of the Canadian Institute for Health Information. Chronic Dis Inj Canada. 2009;29:96–100.
Hennessy S, Leonard CE, Freeman CP, Deo R, Newcomb C, Kimmel SE, et al. Validation of diagnostic codes for outpatient‐originating sudden cardiac death and ventricular arrhythmia in Medicaid and Medicare claims data. Pharmacoepidemiol Drug Saf. 2010;19:555–62.
Heintzman J, Bailey SR, Hoopes MJ, Le T, Gold R, O’Malley JP, et al. Agreement of Medicaid claims and electronic health records for assessing preventive care quality among adults. J Am Med Inform Assoc. 2014;21:720–4.
Beam KS, Lee M, Hirst K, Beam A, Parad RB. Specificity of international classification of diseases codes for bronchopulmonary dysplasia: an investigation using electronic health record data and a large insurance database. J Perinatol. 2021;41:764–71.
Knake LA, Ahuja M, McDonald EL, Ryckman KK, Weathers N, Burstain T, et al. Quality of EHR data extractions for studies of preterm birth in a tertiary care center: guidelines for obtaining reliable data. BMC pediatrics. 2016;16:1–8.
O’Malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health Serv Res. 2005;40:1620–39.
Tawfik DS, Gould JB, Profit J Perinatal risk factors and outcome coding in clinical and administrative databases. Pediatrics. 2019;143.
Ji J, Ling XB, Zhao Y, Hu Z, Zheng X, Xu Z, et al. A data-driven algorithm integrating clinical and laboratory features for the diagnosis and prognosis of necrotizing enterocolitis. PloS one. 2014;9:e89860.
Taylor LK, Travis S, Pym M, Olive E, Henderson-Smart DJ. How useful are hospital morbidity data for monitoring conditions occurring in the perinatal period? Aust NZ J Obstet Gynaecol. 2005;45:36–41.
Lebreton E, Crenn‐Hébert C, Menguy C, Howell EA, Gould JB, Dechartres A, et al. Composite neonatal morbidity indicators using hospital discharge data: A systematic review. Paediatr Perinat Epidemiol. 2020;34:350–65.
Centers for Disease Control and Prevention. ICD-10-CM International Classification of Diseases, Tenth Revision, Clinical Modification: Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/nchs/icd/icd-10-cm.htm.
Bancalari E, Jain D. Bronchopulmonary dysplasia: can we agree on a definition? Am J Perinatol. 2018;35:537–40.
Stoecklin B, Simpson SJ, Pillow JJ. Bronchopulmonary dysplasia: rationale for a pathophysiological rather than treatment based approach to diagnosis. Paediatr Resp Rev. 2019;32:91–7.
Isayama T, Shah PS. Need for an international consensus on the definition of bronchopulmonary dysplasia. Am J Resp Crit Care Med. 2019;200:1323–4.
Fallon SC, Kim ME, Hallmark CA, Carpenter JL, Eldin KW, Lopez ME, et al. Correlating surgical and pathological diagnoses in pediatric appendicitis. J Pediatr Surg. 2015;50:638–41.
Graber ML, Byrne C, Johnston D. The impact of electronic health records on diagnosis. Diagnosis. 2017;4:211–23.
Kusters CD, Chen ML, Follett PL, Dammann O. “Intraventricular”Hemorrhage and Cystic Periventricular Leukomalacia in Preterm Infants: How Are They Related? J Child Neurol. 2009;24:1158–70.
Kuban KC, Allred EN, Dammann O, Pagano M, Leviton A, Share J, et al. Topography of cerebral white-matter disease of prematurity studied prospectively in 1607 very-low-birthweight infants. J Child Neurol. 2001;16:401–8.
Neu J, Modi N, Caplan M, editors. Necrotizing enterocolitis comes in different forms: Historical perspectives and defining the disease. Seminars in Fetal and Neonatal Medicine; 2018: Elsevier.
Neu J. Necrotizing enterocolitis: the mystery goes on. Neonatology 2014;106:289–95.
Rehan V, Seshia M, Johnston B, Reed M, Wilmot D, Cook V. Observer variability in interpretation of abdominal radiographs of infants with suspected necrotizing enterocolitis. Clin Pediatr. 1999;38:637–43.
Overman RE Jr, Criss CN, Gadepalli SK. Necrotizing enterocolitis in term neonates: a different disease process? J Pediatr Surg. 2019;54:1143–6.
Kinstlinger N, Fink A, Gordon S, Levin TL, Friedmann P, Nafday S, et al. Is necrotizing enterocolitis the same disease in term and preterm infants? J Pediatr Surg. 2021;56:1370–4.
World Health Organization. International statistical classification of diseases and related health problems (11th ed.). Geneva: World Health Organization; 2019.
Swanson JR, Hair A, Clark RH, Gordon PV. Spontaneous intestinal perforation (SIP) will soon become the most common form of surgical bowel disease in the extremely low birth weight (ELBW) infant. J Perinatol. 2022;42:423–9.
Dzakpasu S, Joseph K, Huang L, Allen A, Sauve R, Young D, et al. Decreasing diagnoses of birth asphyxia in Canada: fact or artifact. Pediatrics 2009;123:e668–e72.
Hankins GD, Koen S, Gei AF, Lopez SM, Van Hook JW, Anderson GD. Neonatal organ system injury in acute birth asphyxia sufficient to result in neonatal encephalopathy. Obstet Gynecol. 2002;99:688–91.
Acknowledgements
We would like to thank Amy Castonguay and Allison Momany for their early work in developing the medical record validation protocols that eventually led to this work. We would also like to thank the Institute for Clinical and Translational Science (ICTS) Bioinformatics Core at the University of Iowa for creating the data repository used for this study. They were supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002537.
Funding
This research was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD102381). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
K.K.R. designed the study, performed statistical analysis, co-drafted the manuscript; P.J.H. co-drafted the manuscript; E.S., C.C., and N.W. collected data and provided critical input to the final draft of the manuscript. E.A.J., H.C., S.P.O., J.M.D., L.L.P., and E.E.R. assisted with conceptualization of the study and provided critical input to the final draft of the manuscript.
Corresponding author
Ethics declarations
COMPETING INTERESTS
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ryckman, K.K., Holdefer, P.J., Sileo, E. et al. The validity of hospital diagnostic and procedure codes reflecting morbidity in preterm neonates born <32 weeks gestation. J Perinatol 43, 1374–1378 (2023). https://doi.org/10.1038/s41372-023-01685-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01685-6
- Springer Nature America, Inc.