Abstract
Background:
Nab-paclitaxel–gemcitabine combination significantly improved overall survival over gemcitabine in metastatic pancreatic adenocarcinoma. A phase 1b trial was performed (ClinicalTrials.gov number, NCT01730222) to determine the recommended phase 2 dose (RP2D) of nab-paclitaxel in combination with cisplatin, capecitabine, and gemcitabine at fixed dose (800, 30, and 1250 mg m−2 every 2 weeks, respectively; PAXG regimen).
Methods:
Nab-paclitaxel doses were escalated from 100 (level one) to 125 (level two) and 150 mg m−2 (level three) every 2 weeks in cohorts of 3–6 patients with pathologically confirmed unresectable or borderline resectable pancreatic adenocarcinoma.
Results:
Between Dec 2012 and Apr 2014, 24 patients were enroled (3 at level one, 5 at level two, 16 at level three) and received 117 cycles of PAXG. No dose-limiting toxicity occurred and level three was the RP2D. At this dose, nab-paclitaxel dose-intensity was 91%. Worse per patient grade 3/4 toxicity were neutropenia 25/31%; fatigue 19%; anaemia and hand-foot syndrome 12%, nausea 6%, and febrile neutropenia 6%. A partial response (PR) was observed in 16 (67%) and stable disease (SD) in 8 patients (33%). Among 21 patients with a baseline positive positron emission tomography (PET) scan, a complete metabolic response was observed in 9 (43%), PR in 10 (48%), SD in 2. CA19-9 decreased by ⩾49% in all the 19 patients with elevated basal value. Six patients were resected after chemotherapy. Progression-free survival at 6 months (PFS-6) was 96%.
Conclusions:
The RP2D of nab-paclitaxel in the PAXG regimen was 150 mg m−2 every 2 weeks. The preliminary results are promising and warrant further exploration.
Similar content being viewed by others
Main
Pancreatic adenocarcinoma is a rare disease, but is the seventh leading cause of cancer death (GLOBOCAN, 2015). Only 15–20% of patients present with resectable disease, whereas the majority of patients have metastatic disease at diagnosis, and nearly one-third have involvement of regional main vessels.
Randomised trials in locally advanced or borderline disease have been often prematurely interrupted for poor accrual (Chauffert et al, 2008; Loehrer et al, 2011); thus the results have limited statistical strength. Therefore, standard of care for this stage of disease is still controversial.
Currently, chemoradiation and chemotherapy alone, or followed by chemoradiation, are regarded both as acceptable treatment options. Prospective trials, including patients with both locally advanced and metastatic disease treated with combination regimens failed to show any OS improvement over gemcitabine (Cunningham et al, 2009; Poplin et al, 2009; Colucci et al, 2010), with the notable exception of the PEFG regimen (cisplatin, epirubicin, 5-fluorouracil (5-FU), gemcitabine) that showed a significant progression-free survival (PFS) and OS improvement compared to gemcitabine monotherapy (Reni et al, 2005). PEFG was modified by substituting oral capecitabine for 5-FU, originating the PEXG regimen (Reni et al, 2012). The subsequent inclusion of docetaxel instead of epirubicin (PDXG regimen) reduced grade 3 and 4 neutropenia and improved radiological and biochemical responses, particularly in locally advanced disease (Reni et al, 2012). These results might be explained by the well-known synergism of taxanes with fluoropyrimidines increasing intratumour conversion of capecitabine into 5-FU through the promotion of intra-cellular activity of thymidine phosphorylase (Sawada et al, 1998). Furthermore, taxanes reduce multi-drug resistance proteins favoring cisplatin cytotoxicity (Maeda et al, 2004). These data have been further enriched by the findings of a significantly better outcome of stage 4 patients treated with nab-paclitaxel and gemcitabine compared with those receiving gemcitabine alone in a phase 3 trial (Von Hoff et al, 2013).
On the basis of this rational, a phase 1b trial was designed to determine the recommended phase 2 dose (RP2D) of nab-paclitaxel in combination with cisplatin, capecitabine, and gemcitabine (PAXG regimen).
Materials and Methods
Chemo-naive patients with 18–75 years, pathologic diagnosis of unresectable or borderline resectable pancreatic adenocarcinoma, without distant metastases and a Karnofsky Performance Status (KPS) ⩾70 were eligible for the study. The study was conducted at a single institution with a high-volume pancreatic surgery unit (Balzano et al, 2008). Tumours were considered unresectable or borderline resectable on the basis of the National Comprehensive Cancer Network (NCCN) definition (Tempero et al, 2012). The assignment of tumours to the unresectable or borderline resectable category was jointly performed by a dedicated radiologist (RN) and an experienced pancreatic surgeon (GB). Patients were required to have adequate bone marrow (leucocytes ⩾3500 mm−3, absolute neutrophil count ⩾1500 mm−3; platelet count ⩾100 000 mm−3; haemoglobin ⩾10 g dl−1), liver (total bilirubin ⩽2 mg dl−1; aspartate aminotransferase and alanine aminotransferase ⩽3 × upper limit of normal) and kidney function (serum creatinine ⩽1.5 mg dl−1) and the ability to swallow and absorb oral medications. Prior therapy for their cancer diagnosis, lactation or a positive pregnancy test, clinically significant cardiac disease, concurrent treatment with other experimental drugs, previous or concurrent malignancies at other sites with the exception of surgically cured carcinoma in situ of the cervix and basal or squamous cell carcinoma of the skin, and of other neoplasms without evidence of disease at least from 5 years, history of interstitial lung disease, of connective tissue disorders, or of psychiatric disabilities were all exclusion criteria. Written informed consent was obtained from all patients, and the study was approved by the Health Superior Institute and by the institutional Ethics Committee.
The trial was a single-arm phase 1 study to design a new treatment regimen. The primary endpoint was to determine the RP2D of nab-paclitaxel when used in combination with cisplatin, capecitabine, and gemcitabine (PAXG regimen). Secondary endpoints were OS, PFS, PFS at 6 months (PFS-6), response rate as defined by RECIST (Response Evaluation Criteria in Solid Tumours), carcinoma antigen 19-9 (CA19-9) response, and resectability rate. A standard 3+3 dose-escalation schema was used with preplanned cohort expansion at the maximum tolerated dose (MTD). Each treatment cycle consisted of a 28-day period with intravenous cisplatin administered at 30 mg m−2 on days 1 and 15, intravenous nab-paclitaxel on days 1 and 15, oral capecitabine at 1250 mg m−2 on days 1 through 28, intravenous gemcitabine at 800 mg m−2 on days 1 and 15 at a fixed-rate infusion (10 mg m−2 min−1). The dose of cisplatin, capecitabine, and gemcitabine was maintained fixed at any dose level cohort, whereas nab-paclitaxel dose was escalated from the starting dose level (DL1: 100 mg m−2) to DL2 (125 mg m−2), and DL3 (150 mg m−2). Dose-limiting toxicity (DLT) was defined as any of the following events attributable to the administered study drugs during the initial 4 weeks of treatment: grade ⩾4 neutropenia lasting 7 days or more; grade ⩾3 febrile neutropenia or fever of unknown origin⩾38.5 °C; grade 4 thrombocytopenia; grade 3 thrombocytopenia which required transfusions; grade ⩾3 nausea or vomiting; grade ⩾3 diarrhoea; any grade ⩾2 neurological toxicity; any grade ⩾3 toxicities or representing a shift by two grades from baseline (in case of abnormal baseline); failure to recover to grade ⩽1 toxicity (except alopecia) or to baseline values after delaying the initiation of next cycle by >2 weeks. Treatment was continued until documented progressive disease, unacceptable toxicity, patient’s refusal, medical decision or a maximum of six cycles whichever happened before. Surgery and/or chemoradiation after the end of chemotherapy were allowed but were not part of the phase Ib protocol and AE/activity reporting applies to chemotherapy alone.
Pretreatment evaluation with review of inclusion/exclusion criteria, medical and medication history, physical examination, surgical assessment for recectability, KPS assessment, laboratory tests and CA19-9 was performed for all patients ⩽14 days before enrolment. Radiological imaging by computed tomography (CT) was performed within 3 weeks before treatment initiation by a three-phase, high-resolution thorax and abdomen contrast-enhanced CT scan. An 18-fluorodeoxyglucose positron emission tomography (FDG-PET) scan was also performed at baseline whenever possible. Clinical evaluation and haematology panel were repeated at every drugs administration or whenever needed. Haematological and chemistry panel (CA19-9) were repeated on day 1 of every cycle. Radiographic disease assessment was performed every 8 weeks until disease progression using the revised RECIST (version 1.1) guidelines. A FDG-PET scan was repeated after two cycles and at the end of treatment. Metabolic response was assessed according to Weber’s criteria (Weber, 2005). Re-evaluation for surgical resectability was performed after four and six cycles. PFS was defined as the time from the day of treatment start to the disease progression or death (for any cause), whichever occurs first. OS was defined as the time interval between treatment start and the date of death, and censored at the date of the last study assessment. Best overall response was defined as the best response recorded from the start of treatment until disease progression.
Biochemical response was defined in relation to percentage of CA19-9 variation on nadir (minor value assessed while on treatment) with respect to basal value only in patients with CA19-9 level elevated (namely over superior normal laboratory level), after normalisation of serum bilirubin levels. Patients were classified as non-responders if CA19-9 variation was <50%; minor responders if CA19-9 variation was between 50 and 89%; major responders if CA 19-9 variation was >89% (Reni et al, 2009).
Safety was evaluated at the beginning of each treatment cycle based on patient-reported symptoms, physical examination findings, and clinical laboratory abnormalities. Toxicities were noted by grade and organ system using the National Cancer Institute Common Toxicity Criteria (CTC) (version 4.0), with the frequency and severity of all adverse events (grades 1–4) summarised descriptively. OS and PFS endpoints were measured according to the method of Kaplan and Meier.
Results
Between December 2012 and April 2014, 24 patients with unresectable or borderline resectable pancreatic ductal adenocarcinoma, were enroled. Patients’ characteristics are reported in Table 1. None of the patients enroled in the trial (three at DL1, five at DL2 and sixteen at DL3) experienced a DLT. Accordingly, DL3, which was expanded to obtain additional safety and efficacy information, was considered as RP2D. Both for the entire study cohort and for the RP2D, the median number of cycles was five (range: 3–6). One patient discontinued therapy due to disease progression at cycle five. One patient discontinued therapy due to poor subjective tolerance after 3.5 cycles; ten patients completed 6 months of therapy, whereas twelve patients discontinued treatment after 3–5 months due to medical decision, including four patients who were taken to surgery for resection and eight patients who were addressed to chemoradiation (Figure 1).
After eighty cycles at RP2D the dose-intensity was 90.5% for nab-paclitaxel (which was always administered at the planned dose but in two cycles in a single patient); 91% for cisplatin; 80.5% for gemcitabine with a dose reduction in 46% of cycles; and 75% for capecitabine. Chemoradiation, consisting of 44.25 Gy in fifteen fractions delivered with tomotherapy concomitant to capecitabine at 1250 mg m−2 daily was administered to all patients: at the end of chemotherapy to sixteen patients, after surgery to seven patients, and at time of recurrence in one patient. Sixteen patients (67%) experienced at least one grade 3–4 haematological and fifteen patients (60%) one grade 3–4 non-haematological adverse event at any point during therapy. Grade 3–4 neutropenia and grade 3 fatigue, neuropathy, anaemia, nausea, diarrhoea, hand-foot syndrome occurred in at least 5% of patients. Adverse events are summarised in Table 2. Granulocyte colony-stimulating factor was used in a single patient. No toxic death was observed.
All patients were assessable for efficacy analyses and had a radiographically measurable disease. Sixteen patients (67%) had partial response according to RECIST criteria, whereas eight (33%) had stable disease. Among nineteen patients with elevated basal CA19-9 value, one was a CA19-9 non-responder (CA19-9 reduction=49%), ten (53%) had a CA19-9 minor response, and eight (42%) had a CA19-9 major response. Among five patients with normal basal CA19-9 value, one had elevated basal CA125 and one elevated basal CEA. Both patients had a nadir marker reduction >50%. A basal FDG-PET scan was performed in twenty-two patients. All but one was FDG avid. A complete metabolic response was observed in nine (43%), partial metabolic response in ten (48%), and a stable disease in two patients (9%). After chemotherapy, 17 patients remained unresectable by radiological criteria, whereas 7 patients were taken to surgery. In six cases (three borderline, three unresectable) resection was successfully performed, whereas one patient was found unresectable at surgical exploration: three had microscopically free surgical margins (R0) and three microscopically infiltrated margins (R1); four had negative nodes (N0) and two had positive nodes (N1).
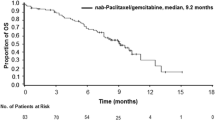
At time of report, all patients had disease progression; all patients but one were progression free at 6 months (PFS-6, 96%) and twelve (50%) were progression free at 1-year; median PFS was 12 months. Site of progression was local only in 3 patients; systemic only in 14 patients; both local and systemic in 6 patients and unknown in 1 patient. Noteworthy, the main site of recurrence was peritoneum (N=10), whereas liver metastases were observed only in 7 patients. Nineteen patients died of disease progression and five were alive at a median follow-up of 25 months (range: 22.2–28.9); mOS was 18.1 months; 1yOS and 2yOS were 83.3 and 29.2%, respectively. Efficacy results are summarised in Table 3.
Discussion
This phase 1 trial was designed to define the RP2D of nab-paclitaxel in combination with cisplatin, gemcitabine, and capecitabine as first-line treatment for patients with chemo-naive, borderline or unresectable pancreatic cancer. Overall, the four-drug combination was safely administered. None of the dose levels of nab-paclitaxel, which included the recommended dose of 150 mg m−2 in many other indications, was associated with toxicity consistent with MTD, and albeit the rate of grade 3–4 neutropenia (56%) and febrile neutropenia (6%) at the RP2D seems higher as compared to nab-paclitaxel–gemcitabine trial (38% and 3%) (Von Hoff et al, 2013), this may be related to small sample size of our series and appears acceptable in the neoadjuvant setting. Furthermore, despite the number of patients with a biliary stent (47% of those with tumour located in the pancreatic head) appears higher in our series as compared to the nab-paciltaxel–gemcitabine (40%) phase III trial (Von Hoff et al, 2013), only one patient experienced a febrile neutropenia. In addition, secondary endpoints analysis showed encouraging preliminary anti-tumour activity. In particular, results are numerically superior to those of our previous experience in a comparable patients population that was selected by the same team of surgeons, radiologists, and medical oncologists, and treated with other four-drug regimens, namely cisplatin, epirubicin, 5-fluorouracil, gemcitabine (PEFG), cisplatin, capecitabine, gemcitabine plus either epirubicin (PEXG) or docetaxel (PDXG) (Reni et al, 2005, 2009, 2012). Data should be considered with caution in view of the small cohort of patients enroled in this phase 1 trial at the RP2D. However, the PAXG regimen reported here obtained numerically superior results in terms of measurable response, disease control rate, mPFS and PFS at 6 months (vs 62.5–82.1%). The relevance of the observations should also be weighted in light of the high resectability rate of 25% obtained in spite of the fact that borderline resectability was present in only six patients at diagnosis. Albeit all patients recurred, OS at 1-year and 2-year (83.3 and 29.2%, respectively) are unusual in other prospective trials in this patients’ population (Table 4).
The relevance of the present data relies also on the homogeneous definition of resectability, which was performed in a single high-volume institution by the blinded assessment of experienced surgical and radiological teams, and the brief timeframe study period.
Overall, collection of pharmacodynamic information in pancreatic adenocarcinoma is very challenging. Tumour tissue is rarely available in pancreatic adenocarcinoma, and the collection of serial biopsies to study the effects of therapy during and after treatment is often limited by the risk linked to the anatomical site to biopsy. A functional characterisation of the response was therefore based on the prospective evaluation with FDG-PET (Chirindel et al, 2015) that can be viewed as a surrogate pharmacodynamic endpoint. A complete or partial FDG-PET response was observed in over 90% of patients, suggesting that the PAXG regimen could achieve a remarkable reduction of tumour metabolism consistent with the high rate of objective responses.
Recently, a few series of patients treated with original or modified FOLFIRINOX regimen (5-FU/leucovorin, irinotecan, and oxaliplatin) reported relevant results as well (Hosein et al, 2012; Blazer et al, 2015; Marthey et al, 2015). Although these data are in some cases preliminary, with short follow-up, and retrospective or observational, they support the concept that further prospective randomised studies of combination chemotherapy should be conducted in this setting.
Currently, the combination of nab-paclitaxel and gemcitabine is considered a standard therapy of metastatic pancreatic adenocarcinoma based on the significant survival improvement over single agent gemcitabine that was demonstrated in a large randomised phase III trial (Von Hoff et al, 2013). The 2-drug regimen has a manageable safety profile, and represents a suitable backbone for building more effective chemotherapy. Another phase 1 trial has tested the addition of capecitabine to nab-paclitaxel and gemcitabine in the AGX regimen in patients with metastatic pancreatic adenocarcinoma, but results were disappointing (Ko et al, 2012). The AGX regimen has several differences in respect to PAXG regimen reported here. The first is the presence of platinum in the PAXG. Platinum compounds are among the most active drugs for pancreatic cancer, and are used in first and second-line setting in the clinical practice. In addition, platinum compounds are synergistic with the other drugs in PAXG (Sawada et al, 1998; Maeda et al, 2004). Another relevant difference is the planned dose-intensity of nab-paclitaxel (75 vs 50 mg m−2 week−1 in AGX) and capecitabine (8750 vs 5250 mg m−2 week−1) that is substantially greater in PAXG, whereas that of gemcitabine is 20% lower (400 vs 500 mg m−2 week−1). Finally, the order of drug administration was different. In the PAXG regimen nab-paclitaxel is given before gemcitabine, as in the original phase 3 trial (Von Hoff et al, 2013), whereas in AGX the inverse sequence is used (Ko et al, 2012). Of note, pre-clinical studies showed that nab-paclitaxel decreases cytidine-deaminase levels (Freese et al, 2012), and increases the integration and interaction of gemcitabine-triphosphate with mRNA and favoring gemcitabine activity (Ricotti et al, 2003; Von Hoff et al, 2011).
In conclusion, the study proved the possibility of including nab-paclitaxel in the regimen and allowed to define the RP2D. An ongoing phase 2 trial is randomizing patients with unresectable, borderline resectable or metastatic pancreatic adenocarcinoma to receive the PAXG regimen or the standard nab-paclitaxel–gemcitabine combination.
Change history
26 July 2016
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Balzano G, Zerbi A, Capretti G, Rocchetti S, Capitanio V, Di Carlo V (2008) Effect of hospital volume on outcome of pancreaticoduodenectomy in Italy. Br J Surg 95: 357–362.
Blazer M, Wu C, Goldberg RM, Phillips G, Schmidt C, Muscarella P, Wuthrick E, Williams TM, Reardon J, Ellison EC, Bloomston M, Bekaii-Saab T (2015) Neoadjuvant modified (m) FOLFIRINOX for locally advanced unresectable (LAPC) and borderline resectable (BRPC) adenocarcinoma of the pancreas. Ann Surg Oncol 22: 1153–1159.
Chauffert B, Mornex F, Bonnetain F, Rougier P, Mariette C, Bouché O, Bosset JF, Aparicio T, Mineur L, Azzedine A, Hammel P, Butel J, Stremsdoerfer N, Maingon P, Bedenne L (2008) Phase III trial comparing intensive induction chemoradiotherapy (60 Gy, infusional 5-FU and intermittent cisplatin) followed by maintenance gemcitabine with gemcitabine alone for locally advanced unresectable pancreatic cancer. Definitive results of the 2000-01 FFCD/SFRO study. Ann Oncol 19: 1592–1599.
Chirindel A, Alluri KC, Chaudhry MA, Wahl RL, Pawlik TM, Herman JM, Subramaniam RM (2015) Prognostic Value of FDG PET/CT-derived parameters in pancreatic adenocarcinoma at initial PET/CT staging. AJR Am J Roentgenol 204: 1093–1099.
Colucci G, Labianca R, Di Costanzo F, Gebbia V, Cartenì G, Massidda B, Dapretto E, Manzione L, Piazza E, Sannicolò M, Ciaparrone M, Cavanna L, Giuliani F, Maiello E, Testa A, Pederzoli P, Falconi M, Gallo C, Di Maio M, Perrone F Gruppo Oncologico Italia Meridionale (GOIM), Gruppo Italiano per lo Studio dei Carcinomi dell’Apparato Digerente (GISCAD), Gruppo Oncologico Italiano di Ricerca Clinica (GOIRC) (2010) Randomized phase III trial of gemcitabine plus cisplatin compared with single agent gemcitabine as first-line treatment of patients with advanced pancreatic cancer: the GIP-1 study. J Clin Oncol 28: 1645–1651.
Cunningham D, Chau I, Stocken DD, Valle JW, Smith D, Steward W, Harper PG, Dunn J, Tudur-Smith C, West J, Falk S, Crellin A, Adab F, Thompson J, Leonard P, Ostrowski J, Eatock M, Scheithauer W, Herrmann R, Neoptolemos JP (2009) Phase III randomised comparison of gemcitabine versus gemcitabine plus capecitabine in patients with advanced pancreatic cancer. J Clin Oncol 27: 5513–5518.
Frese KK, Neesse A, Cook N, Bapiro TE, Lolkema MP, Jodrell DI, Tuveson DA (2012) nab-Paclitaxel potentiates gemcitabine activity by reducing cytidine deaminase levels in a mouse model of pancreatic cancer. Cancer Discov 2: 260–269.
GLOBOCAN (IARC). Section of Cancer Surveillance (2012) http://globocan.iarc.fr/Pages/fact_sheets_population.aspx (accessed on 26 September 2015).
Hosein PJ, Macintyre J, Kawamura C, Maldonado JC, Ernani V, Loaiza-Bonilla A, Narayanan G, Ribeiro A, Portelance L, Merchan JR, Levi JU, Rocha-Lima CM (2012) A retrospective study of neoadjuvant FOLFIRINOX in unresectable or borderline resectable locally advanced pancreatic adenocarcinoma. BMC Cancer 12: 1–7.
Ko AH, Truong TG, Kantoff E, Jones KA, Dito E, Ong A, Tempero MA (2012) A phase I trial of nab-paclitaxel, gemcitabine, and capecitabine for metastatic pancreatic cancer. Cancer Chemother Pharmacol 70: 875–881.
Loehrer PJ Sr, Feng Y, Cardenes H, Wagner L, Brell JM, Cella D, Flynn P, Ramanathan RK, Crane CH, Alberts SR, Benson AB 3rd (2011) Gemcitabine alone versus gemcitabine plus radiotherapy in patients with locally advanced pancreatic cancer: an Eastern Cooperative Oncology Group trial. J Clin Oncol 29: 4105–4112.
Maeda S, Sugiura T, Saikawa Y, Kubota T, Otani Y, Kumai K, Kitajima M (2004) Docetaxel enhances the cytotoxicity of cisplatin to gastric cancer cells by modification of intracellular platinum metabolism. Cancer Sci 95: 679–684.
Marthey L, Sa-Cunha A, Blanc JF, Gauthier M, Cueff A, Francois E, Trouilloud I, Malka D, Bachet JB, Coriat R, Terrebonne E, De La Fouchardière C, Manfredi S, Solub D, Lécaille C, Thirot Bidault A, Carbonnel F, Taieb J (2015) FOLFIRINOX for locally advanced pancreatic adenocarcinoma: results of an AGEO multicentre prospective observational cohort. Ann Surg Oncol 22: 295–301.
Mukherjee S, Hurt CN, Bridgewater J, Falk S, Cummins S, Wasan H, Crosby T, Jephcott C, Roy R, Radhakrishna G, McDonald A, Ray R, Joseph G, Staffurth J, Abrams RA, Griffiths G, Maughan T (2013) Gemcitabine-based or capecitabine-based chemoradiotherapy for locally advanced pancreatic cancer (SCALOP): a multicentre, randomised, phase 2 trial. Lancet Oncol 14 (4): 317–326.
Poplin E, Feng Y, Berlin J, Rothenberg ML, Hochster H, Mitchell E, Alberts S, O’Dwyer P, Haller D, Catalano P, Cella D, Benson AB 3rd (2009) Phase III, randomized study of gemcitabine and oxaliplatin versus gemcitabine (fixed dose rate infusion) compared with gemcitabine (30-minute infusion) in patients with pancreatic carcinoma E6201: a trial of the Eastern Cooperative Oncology Group. J Clin Oncol 27: 3778–3785.
Reni M, Cordio S, Milandri C, Passoni P, Bonetto E, Oliani C, Luppi G, Nicoletti R, Galli L, Bordonaro R, Passardi A, Zerbi A, Balzano G, Aldrighetti L, Staudacher C, Villa E, Di Carlo V (2005) Gemcitabine versus cisplatin, epirubicin, fluorouracil, and gemcitabine in advanced pancreatic cancer: a randomised controlled multicentre phase III trial. Lancet Oncol 6: 369–376.
Reni M, Cereda S, Balzano G, Passoni P, Rognone A, Fugazza C, Mazza E, Zerbi A, Di Carlo V, Villa E (2009) Carbohydrate antigen 19-9 change during chemotherapy for advanced pancreatic adenocarcinoma. Cancer 115: 2630–2639.
Reni M, Cereda S, Balzano G, Passoni P, Rognone A, Zerbi A, Nicoletti R, Mazza E, Arcidiacono PG, Di Carlo V, Villa E (2009) Outcome of upfront combination chemotherapy followed by chemoradiation for locally advanced pancreatic adenocarcinoma. Cancer Chemother Pharmacol 64: 1253–1259.
Reni M, Cereda S, Rognone A, Belli C, Ghidini M, Longoni S, Fugazza C, Rezzonico S, Passoni P, Slim N, Balzano G, Nicoletti R, Cappio S, Doglioni C, Villa E (2012) A randomized phase II trial of two different 4-drug combinations in advanced pancreatic adenocarcinoma: cisplatin, capecitabine, gemcitabine plus either epirubicin or docetaxel (PEXG or PDXG regimen). Cancer Chemother Pharmacol 69: 115–123.
Ricotti L, Tesei A, De Paola F, Ulivi P, Frassineti GL, Milandri C, Amadori D, Zoli W (2003) In vitro schedule-dependent interaction between docetaxel and gemcitabine in human gastric cancer cell lines. Clin Cancer Res 9: 900–905.
Sawada N, Ishikawa T, Fukase Y, Nishida M, Yoshikubo T, Ishitsuka H (1998) Induction of thymidine phosphorylase activity and enhancement of capecitabine efficacy by taxol/taxotere in human cancer xenografts. Clin Cancer Res 4: 1013–1019.
Sherman WH, Chu K, Chabot J, Allendorf J, Schrope BA, Hecht E, Jin B, Leung D, Remotti H, Addeo G, Postolov I, Tsai W, Fine RL (2015) Neoadjuvant gemcitabine, docetaxel, and capecitabine followed by gemcitabine and capecitabine/radiation therapy and surgery in locally advanced, unresectable pancreatic adenocarcinoma. Cancer 121 (5): 673–680.
Tempero MA, Arnoletti JP, Behrman SW, Ben-Josef E, Benson AB 3rd, Casper ES, Cohen SJ, Czito B, Ellenhorn JDI, Hawkins WG, Herman J, Hoffman JP, Ko A, Komanduri S, Koong A, Ma WW, Malafa MP, Merchant NB, Mulvihill SJ, Muscarella P 2nd, Nakakura EK, Obando J, Pitman MB, Sasson AR, Tally A, Thayer SP, Whiting S, Wolff RA, Wolpin BM, Freedman-Cass DA, Shead DA (2012) Pancreatic adenocarcinoma, version 2.2012: featured updates to the NCCN guidelines. J Natl Compr Canc Netw 10: 703–713.
Von Hoff DD, Ramanathan RK, Borad MJ, Laheru DA, Smith LS, Wood TE, Korn RL, Desai N, Trieu V, Iglesias JL, Zhang H, Soon-Shiong P, Shi T, Rajeshkumar NV, Maitra A, Hidalgo M (2011) Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: a phase I/II trial. J Clin Oncol 29: 4548–4554.
Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF (2013) Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 369: 1691–1703.
Weber WA (2005) Use of PET for monitoring cancer therapy and for predicting outcome. J Nucl Med 46: 983–995.
Acknowledgements
Celgene provided funding for the study with an unrestricted grant and the supply of the drug. We thank all the patients who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
This work was supported by Celgene, which provided funding for the study with an unrestricted grant and the supply of the drug. MR discloses: advisory role for Celgene, Boehringer Ingelheim, Genetech, Lilly, Merck Serono, Baxalta; research funding to his institution from Celgene, PharmaMar, and Novartis; expenses reimbursement from Celgene. GB discloses: advisory role for Celgene. MF discloses: research funding to his institution from Novartis. LG discloses: consulting or advisory role for Roche, Pfizer, GlaxoSmithKline, Synthon, Taiho Pharmaceutical, AstraZeneca, Genomic Health, Merck Sharp & Dohme, Boehringer Ingelheim, Tiziana Pharma, Synaffix, and Celgene; patents/royalties/other intellectual property with Roche. All other authors disclose no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Reni, M., Balzano, G., Zanon, S. et al. Phase 1B trial of Nab-paclitaxel plus gemcitabine, capecitabine, and cisplatin (PAXG regimen) in patients with unresectable or borderline resectable pancreatic adenocarcinoma. Br J Cancer 115, 290–296 (2016). https://doi.org/10.1038/bjc.2016.209
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2016.209
- Springer Nature Limited
Keywords
This article is cited by
-
Synchronous double primary malignancies of the pancreatic body and extrahepatic bile duct treated with pancreatoduodenectomy and splenic artery resection following neoadjuvant chemotherapy with gemcitabine plus nab-paclitaxel: a case report
Surgical Case Reports (2022)
-
Time to CA19-9 nadir: a clue for defining optimal treatment duration in patients with resectable pancreatic ductal adenocarcinoma
Cancer Chemotherapy and Pharmacology (2020)