Abstract
Aim:
Purinergic signaling plays a major role in the enteric nervous system, where it governs gut motility through a number of P2X and P2Y receptors. The aim of this study was to investigate the P2Y receptor-mediated motility in rat longitudinal ileum preparations.
Methods:
Ileum smooth muscle strips were prepared from rats, and fixed in an organ bath. Isometric contraction and relaxation responses of the muscle strips were measured with force transducers. Drugs were applied by adding of stock solutions to the organ bath to yield the individual final concentrations.
Results:
Application of the non-hydrolyzable P2 receptor agonists α,β-Me-ATP or 2-Me-S-ADP (10, 100 μmol/L) dose-dependently elicited a transient relaxation response followed by a sustained contraction. The relaxation response was largely blocked by SK channel blockers apamin (500 nmol/L) and UCL1684 (10 μmol/L), PLC inhibitor U73122 (100 μmol/L), IP3 receptor blocker 2-APB (100 μmol/L) or sarcoendoplasmic Ca2+ ATPase inhibitor thapsigargin (1 μmol/L), but not affected by atropine, NO synthase blocker L-NAME or tetrodotoxin. Furthermore, α,β-Me-ATP-induced relaxation was suppressed by P2Y1 receptor antagonist MRS2179 (50 μmol/L) or P2Y13 receptor antagonist MRS2211 (100 μmol/L), and was abolished by co-application of the two antagonists, whereas 2-Me-S-ADP-induced relaxation was abolished by P2Y6 receptor antagonist MRS2578 (50 μmol/L). In addition, P2Y1 receptor antagonist MRS2500 (1 μmol/L) not only abolished α,β-Me-ATP-induced relaxation, but also suppressed 2-Me-S-ADP-induced relaxation.
Conclusion:
P2Y receptor agonist-induced transient relaxation of rat ileum smooth muscle strips is mediated predominantly by P2Y1 receptor, but also by P2Y6 and P2Y13 receptors, and involves PLC, IP3, Ca2+ release and SK channel activation, but is independent of acetylcholine and NO release.
Similar content being viewed by others
Introduction
A balance of contraction and relaxation of gastrointestinal (GI) smooth muscle cells is the physiological prerequisite for digestive and non-digestive motility. Numerous sympathetic fibers and particularly parasympathetic fibers innervate the smooth muscle and are known to be involved in coordinating the motility of large portions of the GI tract. However, there is an increasing interest in non-adrenergic non-cholinergic (NANC) neurotransmission, and the enteric nervous system (ENC) has been acknowledged to play a major role in governing smooth muscle motility1. Generally, nitric oxide (NO) and adenosine 5′ triphosphate (ATP) are thought to be key molecules in inhibitory NANC signaling, giving rise to hyperpolarization and relaxation of GI smooth muscle2,3,4. While NO leads to a long-lasting inhibition of smooth muscle motility, the available data on purinergic responses are less consistent, as both excitatory and inhibitory effects have been observed and seem to depend on the subtype and cellular location of P2 purinoceptors. In addition, species differences should also be considered2,3,4,5,6,7,8,9,10. Seven cloned ionotropic P2X receptors that combine heteromerically, as well as eight cloned metabotropic P2Y receptors, account for the large heterogeneity of purinoceptor-mediated effects11. Hence, P2 purinoceptors are intriguing target candidates for future therapies in conditions associated with GI dysmotility. However, development of these therapies is currently hampered by the lack of specific inhibitors for the majority of P2 receptors. Immunohistochemical data have demonstrated that ionotropic P2X2/P2X3 and metabotropic P2Y1/P2Y2 receptors are expressed on pre-junctional enteric neurons7,12, while smooth muscle cells are predominantly immunoreactive for P2Y1 receptors7. Moreover, there is a great consensus that the purinergic inhibitory junction potential and the corresponding relaxation are highly sensitive to MRS2179 and MRS2500, showing that the P2Y1 is the receptor type involved in purinergic nerve-mediated relaxation13,14,15. This finding has also been confirmed in P2Y1 knock-out (KO) mice16,17,18. Consistent with this differential expression, the ATP release and smooth muscle contraction from cholinergic fibers that are induced by the P2 agonist α,β-methylene ATP (α,β-Me-ATP) are mediated by pre-junctional P2Y and P2X receptor activation, respectively8. Post-junctional P2Y receptors, however, activate apamin-sensitive SK channels as a consequence of Ca2+ release from thapsigargin-sensitive stores and thus promote relaxation4,9,19,20. Recently, an elegant study tested the hypothesis that spontaneous hydrolysis products of ATP, such as ADP and adenosine, mediate the biphasic effects observed following ATP administration and found that ADP and adenosine were agonists of P2Y and adenosine A1 receptor, respectively, thereby having the opposite effects from ATP6.
In the present study, we tested the hypothesis that purinergic signaling is involved in the control of ileum motility in the rat and found that P2 receptor activation led to both transient relaxation and slow-onset sustained contraction of longitudinal segments of the rat ileum.
Materials and methods
Preparation of ileum smooth muscle strips
Male Sprague–Dawley rats (50–120 days old, 200–350 g, Charles River, Sulzfeld, Germany) were deeply anesthetized with diethyl ether and decapitated. All procedures conformed to the national and international guidelines on the ethical use of animals (European Council Directive 86/609/EEC) and were approved by local authorities (LALLF Mecklenburg-Vorpommern). The abdomen was incised, and the full length of the small intestine was removed. Ileum preparation was obtained by cutting a piece 10–15 cm in length from the ileocecal junction in the oral direction. This preparation was subsequently submerged into a dissection solution containing (in mmol/L) 120 NaCl, 4.5 KCl, 26 NaHCO3, 1.2 NaH2PO4, 1.6 CaCl2, 1.0 MgSO4, 0.025 Na2-EDTA, 5.5 glucose, and 5 HEPES (pH=7.4) at 4 °C and was further cut while submerged in the solution into 4–8 specimens of approximately 2 cm in length. Thin nylon threads were sutured to either end of these specimens to enable longitudinal fixation in the organ bath (Panlab ML0146/C, ADInstruments, Spechbach, Germany). The organ bath was filled with a buffer that contained (in mmol/L) 120 NaCl, 4.7 KCl, 2.5 CaCl2, 1.2 MgSO4, 30 NaHCO3, 0.5 Na2-EDTA, 5.5 glucose, 2 sodium pyruvate (pH=7.4) and was gassed with carbogen (95% O2 and 5% CO2).
Isometric contractions in vitro
After fixation in the organ bath, the ileum specimens were allowed to recover for at least 1 h before the experiments started. During this time, the organ bath temperature was raised from room temperature to 37 °C. The initial tension of the gut specimens within the organ bath was adjusted to yield a stable baseline tone. Briefly, the specimens were inserted and fixed with a mean force. Occasionally, the tissue displayed an increase or a decrease in baseline tone, which was abolished by re-adjustment of the baseline force. Before the start of the experiment, a stable baseline tone was achieved for at least 50 min. Under these conditions, both contractions and relaxations have been found to be very reproducible and to show low variance between different tissue specimens in previous studies21,22. Isometric contractions and relaxations of the smooth muscle strips induced by KCl or purinergic ligands were measured by force transducers (MLT0201, ADInstruments, Oxford, UK) and recorded with a bridge amplifier (ML224, ADInstruments) connected to an analog-to-digital converter (Powerlab 4/30, ADInstruments) and then analyzed by the Chart 5 software (ADInstruments).
α,β-Me-ATP, 2-methylthioadenosine-5′-diphosphate (2-Me-S-ADP), UCL1684, 2-aminoethoxydiphenylborane (2-APB), thapsigargin, U73122, pertussis toxin, MRS2211, MRS2179, MRS2578, MRS2500 and suramin were purchased from Tocris Bioscience (Bristol, UK). Apamin was obtained from Alomone Labs (Jerusalem, Israel). All other chemicals were obtained from Sigma-Aldrich (Taufkirchen, Germany). The application of drugs was performed by adding 100 μL of stock solution (α,β-Me-ATP, 2-Me-S-ADP, apamin, UCL1684, 2-APB, thapsigargin, U73122, pertussis toxin, MRS2211, MRS2179, MRS2578, MRS2500, suramin, tetrodotoxin) or 1000 μL of stock solution (KCl) to the organ bath (volume 25 mL) to yield the individual final concentration. The organ bath fluid was not corrected for osmolarity after the addition of KCl. However, the resulting increase in osmolarity was well tolerated by the preparations, and hyperosmotic control experiments with addition of the same amount of NaCl revealed relaxation of the smooth muscle rather than contraction21. Each gut preparation was tested with KCl for depolarization-induced contractions at the beginning and at the end of the experiment and was included in the study when the KCl-induced contraction at the end of the experiment was at least 50% of the initial response.
P2 receptor activation causes a transient relaxation and a sustained contraction. (A) At the beginning of each experiment, the ileum longitudinal smooth muscle strip was challenged by application of KCl to the organ bath at concentrations that reached 60 mmol/L, which produced a strong isometric peak contraction followed by a less pronounced sustained contraction, indicating stable recording conditions. After washout and recovery for 30 min, α,β-Me-ATP induced a transient relaxation and a sustained contraction (Aa and Ac). When the P2 receptor blocker suramin was present in the organ bath, both relaxation and contraction were abolished (Ab and Ad). At the end of the experiment, application of KCl again induced a contraction, which was similar to that at the beginning of the experiment. (B) The transient relaxation elicited by α,β-Me-ATP was dose-dependent and significantly inhibited by suramin (n=5–8 as indicated by numbers in brackets). (C) The sustained contraction by α,β-Me-ATP was also dose-dependent and significantly inhibited by suramin (n=5–8 as indicated by numbers in brackets). Mean±SEM. *P<0.05, **P<0.01.
Statistical analysis
All data are expressed as mean±SEM. Statistical comparison of drug effects was performed using ANOVA followed by Holm-Sidak post-hoc test for pairwise comparisons (Figure 2,3,4,5,6). If only two groups were being compared (Figure 1), the unpaired two-tailed Student's t-test was applied. Significant differences were assumed when the P value was less than 0.05.
P2 receptor-mediated relaxation relies on SK channel activation. (A) The transient relaxation induced by α,β-Me-ATP and by 2-Me-S-ADP (see arrows in Aa and Ab) was prevented by pre-application of 500 nmol/L apamin or 10 μmol/L UCL1684 (see asterisks in Aa and Ab). All traces in A are derived from individual smooth muscle specimens. (B) The transient relaxation induced by α,β-Me-ATP or by 2-Me-S-ADP was abolished by apamin and by UCL1684, indicating SK channel dependence (n=7–20 as indicated by numbers in brackets). (C) The sustained contraction elicited by both P2 receptor agonists was unaffected by apamin or UCL1684 (n=7–20 as indicated by numbers in brackets). Mean±SEM. *P<0.05.
P2 receptor-mediated relaxation involves Ca2+ release from internal stores. (A) The transient relaxation induced by α,β-Me-ATP and by 2-Me-S-ADP (see arrows in Aa and Ab) was prevented by pre-application of 100 μmol/L 2-APB or 1 μmol/L thapsigargin (see asterisks in Aa and Ab). All traces in A are derived from individual smooth muscle specimens. (B) The transient relaxation induced by α,β-Me-ATP and by 2-Me-S-ADP was significantly reduced by both 2-APB and thapsigargin, indicating the involvement of IP3 receptor-mediated Ca2+ release from internal stores (n=13–22 as indicated by numbers in brackets). (C) The sustained contraction induced by either P2 receptor agonist was unaffected by 2-APB and by thapsigargin (n=13–22 as indicated by numbers in brackets). *P<0.05.
P2 receptor-mediated relaxation is mediated by phospholipase C (PLC), but only partially involves inhibitory G proteins. (A) The transient relaxation by α,β-Me-ATP and by 2-Me-S-ADP (see arrows in Aa and Ab) was prevented by pre-application of 100 μmol/L U73122, but 40 ng/mL pertussis toxin blocked only the relaxation induced by 2-Me-S-ADP, but not that induced by α,β-Me-ATP (see asterisks in Aa and Ab). All traces in A are derived from individual smooth muscle specimens. (B) The transient relaxation induced by α,β-Me-ATP and by 2-Me-S-ADP was significantly reduced by U73122, indicating the involvement of PLC. Pertussis toxin significantly reduced the relaxation induced by 2-Me-S-ADP, indicating the involvement of inhibitory G proteins (n=5–16 as indicated by numbers in brackets). (C) The sustained contraction induced by 2-Me-S-ADP was significantly reduced by U73122, but contraction by α,β-Me-ATP was unaffected by either inhibitor (n=5–16 as indicated by numbers in brackets). Mean±SEM. *P<0.05.
Differential effects of MRS2179, MRS2500 and MRS2211 on P2 receptor-mediated relaxation. (A) While 50 μmol/L MRS2179 and 100 μmol/L MRS2211 prevented the transient relaxation induced by α,β-Me-ATP (see arrow and asterisks in Aa), these inhibitors had no effect on the 2-Me-S-ADP-induced relaxation (see arrows in Ab). All traces in A are derived from individual smooth muscle specimens. (B) The transient relaxation induced by α,β-Me-ATP was significantly reduced by MRS2179, MRS2500 or MRS2211. MRS2500 (1 μmol/L) also blocked the transient relaxation induced by 2-Me-S-ADP, indicating the involvement of P2Y1 receptors (n=6–18 as indicated by numbers in brackets). (C) The sustained contraction induced by α,β-Me-ATP was significantly reduced by MRS2179, MRS2500 or MRS2211. The contraction induced by 2-Me-S-ADP was significantly reduced only by MRS2179 (n=6–18 as indicated by numbers in brackets). Mean±SEM. *P<0.05.
Differential effects of MRS2179, MRS2211 and MRS2578 on P2 receptor-mediated relaxation. (A) While the transient relaxation induced by α,β-Me-ATP was abolished by co-application of 50 μmol/L MRS2179 and 100 μmol/L MRS221, it was unaffected by application of MRS2578 (see arrows and asterisk in Aa). In contrast, the transient relaxation induced by 2-Me-S-ADP was unaffected by co-application of MRS2179 and MRS2211, but was abolished by application of MRS2578 (see arrows and asterisk in Ab). All traces in A are derived from individual smooth muscle specimens. (B) The transient relaxation induced by α,β-Me-ATP, but not by 2-Me-S-ADP, was significantly reduced by co-application of MRS2179 and MRS2211, indicating the involvement of the P2Y1 and P2Y13 receptors. The transient relaxation induced by 2-Me-S-ADP was abolished by MRS2578, indicating the involvement of the P2Y6 receptor (n=8–16 as indicated by numbers in brackets). (C) The sustained contraction induced by α,β-Me-ATP was significantly reduced by co-application of MRS2179 and MRS2211, but the contraction induced by 2-Me-S-ADP was unaffected by any of the inhibitors (n=8–16 as indicated by numbers in brackets). Mean±SEM. *P<0.05.
Results
P2 receptor activation causes a transient relaxation and a sustained contraction
The aim of this study was to analyze the effect of P2 receptor signaling on the motility of the ileum longitudinal smooth muscle. To this end, we used α,β-Me-ATP as a non-hydrolyzable specific P2 receptor agonist. Figure 1A illustrates the experimental paradigm. At the beginning of the experiment, each gut preparation was challenged with a high concentration of KCl (60 mmol/L) for 10 min, and a strong depolarization-induced contraction was obtained in all cases (Figure 1A, leftmost traces). After the washout of KCl for at least 30 min, a single dose of α,β-Me-ATP was applied for 20 min using a randomly chosen concentration of 10 or 100 μmol/L (n=8 and 5; Figure 1A, middle traces). This agonist elicited a dose-dependent transient relaxation (100 μmol/L α,β-Me-ATP: −11.0±2.0 mN, n=5, Figure 1B) and a slow-onset, but sustained contraction (100 μmol/L α,β-Me-ATP: 13.8±5.7 mN, n=5), which was also dose-dependent (Figure 1C). We confined our experiment to a single dose of α,β-Me-ATP for each gut preparation, because preliminary experiments have shown that repeated applications of this agonist produce significant desensitization, as has also been reported previously23. Hence, after the washout of α,β-Me-ATP, we tested the effect of a high concentration of KCl solution again. This final depolarization-induced contraction (Figure 1A, rightmost traces) was as strong as that at the beginning of the experiment (100%±7% of initial KCl-response, n=25).
To demonstrate the P2 receptor-dependent nature of the α,β-Me-ATP-induced effects, we pre-applied the specific P2 receptor antagonist suramin (100 μmol/L; Figure 1Ab, d). This blocker was added to the organ bath 10 min prior to ATP application and almost abolished both relaxation (100 μmol/L α,β-Me-ATP: −1.2±0.6 mN, n=6, P<0.01, unpaired t-test) and contraction (100 μmol/L α,β-Me-ATP: 2.8±0.7 mN, n=6, P<0.05, unpaired t-test), hence providing evidence that P2 receptor-activation is the predominant mechanism of action of α,β-Me-ATP (Figure 1B, C). While α,β-Me-ATP has been reported to act primarily on P2X receptors24, we aimed to determine whether the P2 receptor-induced transient relaxation could also be achieved by 2-Me-S-ADP, a non-hydrolyzable agonist with preferential action on P2Y receptors. At a concentration of 10 μmol/L, this compound also produced transient relaxation (−6.7±0.9 mN, n=20) but less pronounced contraction (3.7±1.3 mN, n=20).
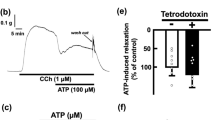
Intracellular cascade leading to P2 receptor-mediated relaxation and contraction
Because purinoceptors are localized to pre-junctional enteric neurons7,10,12, the effects of P2 receptor-mediated relaxation could be due to the inhibition of acetylcholine release or to the production of NO. However, atropine (1 μmol/L) had no effect on relaxation induced by α,β-Me-ATP (−10.1±0.6 mN, n=4) or by 2-Me-S-ADP (−6.8±2.0 mN, n=4, Table 1). The NO synthase blocker L-NAME (100 μmol/L) was also ineffective at reducing the relaxation induced by α,β-Me-ATP (−9.0±1.1 mN, n=15) or by 2-Me-S-ADP (−5.2±0.9 mN, n=8, Table 1). To inhibit the activity of all enteric nerve fibers, we pre-applied tetrodotoxin (TTX, 500 nmol/L) to the organ bath. Similarly to atropine and L-NAME, the relaxation induced by α,β-Me-ATP (−11.4±1.5 mN, n=9) or by 2-Me-S-ADP (−7.0±1.4 mN, n=10, Table 1) was not altered by TTX. In contrast, as previously published4,9,19,20, SK channel inhibition by apamin (0.5 μmol/L) or UCL1684 (10 μmol/L) abolished the relaxation induced by α,β-Me-ATP and by 2-Me-S-ADP (see asterisks in Figure 2Aa and 2Ab). Thus, P2 receptor-mediated relaxation was entirely due to SK channel-activation (0±0 mN for all, Figure 2B), while the contraction following purinergic stimulation did not involve these channels (Figure 2C).
We next tested whether Ca2+ release from internal stores triggers SK channel activation. To this end, we used the IP3 receptor blocker 2-APB (100 μmol/L) and the sarcoendoplasmic reticulum ATPase (SERCA) inhibitor thapsigargin (1 μmol/L). Pre-treatment of ileum segment preparations with 2-APB caused a transient contraction followed by a persistent relaxation (not shown), which could be due to a brief activation of store-operated Ca2+ entry that is activated by 2-APB at concentrations below 10 μmol/L, but inhibited by higher concentrations25. Application of thapsigargin led to a pronounced but transient contraction (not shown), which has been shown to be correlated with a transient rise in cytosolic Ca2+ concentration following SERCA inhibition26. Therefore, smooth muscle preparations were allowed to equilibrate with these compounds before the agonists α,β-Me-ATP or 2-Me-S-ADP was added to the organ bath. As shown in representative traces in Figure 3A, both 2-APB and thapsigargin, prevented the purinergic agonist-induced transient relaxation (see asterisks in Figure 3Aa and Figure 3Ab). A series of independent experiments confirmed the significant reduction of the transient relaxation induced by α,β-Me-ATP (control: −9.0±1.2 mN, n=13; 2-APB: −0.2±0.1 mN, n=22, P<0.01; thapsigargin: −3.9±0.8 mN, n=15, P<0.01; Figure 3B) and by 2-Me-S-ADP (control: −9.0±0.7 mN, n=20; 2-APB: −0.2±0.2 mN, n=14, P<0.01; thapsigargin: −0.2±0.1 mN, n=17, P<0.01; Figure 3B). Interestingly, the purinergic agonist-induced contraction was not affected by these compounds (Figure 3C), indicating that Ca2+ influx through voltage-gated Ca2+ channels might be sufficient to trigger smooth muscle contraction. Indeed, co-application of thapsigargin and the L-type Ca2+ channel blocker verapamil (100 μmol/L) abolished the contraction (α,β-Me-ATP: 2.7±0.2 mN, n=2, P<0.05 versus control; 2-Me-S-ADP: 0.8±0.3 mN, n=9, P<0.01 versus control, data not shown). Collectively, our results so far indicate that Ca2+ release from internal stores and subsequent activation of SK channels are downstream mechanisms of purinergic agonist-induced relaxation.
Because IP3 receptor-mediated Ca2+ release is a consequence of phospholipase C (PLC) activation, we next tested the effect of the PLC inhibitor U73122 (100 μmol/L) on the relaxation induced by the P2 agonists α,β-Me-ATP and 2-Me-S-ADP (Figure 4). Both α,β-Me-ATP (control: −10.1±0.7 mN, n=9; U73122: −2.7±0.4 mN, n=16, P<0.01) and 2-Me-S-ADP (control: −8.3±0.8 mN, n=8; U73122: −1.0±0.1 mN, n=10, P<0.01) no longer stimulated relaxation of the ileum smooth muscle when PLC was inhibited prior to agonist administration (Figure 4B). Hence, PLC activation plays a crucial role in P2 receptor-mediated relaxation. With respect to purinergic contractions, U73122 did not affect α,β-Me-ATP-induced contraction, but significantly blocked the contraction by the P2Y-preferring agonist 2-Me-S-ADP (control: 5.6±1.3 mN, n=6; U73122: 1.4±0.6 mN, n=10, P<0.01; Figure 4C). These results indicate that P2Y receptor-mediated contraction requires PLC activation, while P2X receptor-mediated contraction may also be triggered by depolarization-induced Ca2+ influx via voltage-gated L-type Ca2+ channels. We therefore tested the effect of verapamil (100 μmol/L) on α,β-Me-ATP-induced contractions and observed a significant reduction (8.8±1.5 mN, n=6, P<0.05 versus control), but the contraction induced by the P2Y-preferring agonist 2-Me-S-ADP was not affected by inhibition of L-type Ca2+ channels (5.8±0.2 mN, n=4). These results suggest that P2Y receptor activation under normal circumstances does not substantially activate depolarization-induced Ca2+ influx.
P2Y receptors involved in purinergic relaxation and contraction
Heterotrimeric G proteins play a major role in PLC activation. In particular, the Gαq/11 and βγ-subunits of Gi/o proteins have been shown to recruit PLC and thereby lead to IP3 production27. Pertussis toxin (PTX), however, specifically interferes with Gi/o protein signaling and is thus a powerful tool to study this pathway28 and to discriminate between the Gαq/11 and βγ-subunit of Gi/o. Importantly, PTX (40 ng/mL) did not affect baseline motility, but had differential effects on purinergic relaxation. While this compound failed to block the α,β-Me-ATP-induced relaxation (see arrow in Figure 4Aa; −12.1±1.8 mN, n=5, Figure 4B), it significantly reduced the relaxing effect of 2-Me-S-ADP (see asterisk in Figure 4Ab; −3.1±0.8 mN, n=5, P<0.01, Figure 4B). In contrast, contractions induced by either agonist were largely unaffected by the PTX (Figure 4C). Together with our findings on PLC inhibition, these results suggest that α,β-Me-ATP-induced relaxation predominantly involves Gαq/11 activation, whereas PTX-sensitive Gi/o coupling is involved in 2-Me-S-ADP-induced relaxation.
Having ascertained that PLC activation is instrumental in relaxation induced by α,β-Me-ATP, as well as by 2-Me-S-ADP, we sought to identify the P2Y receptor(s) involved in this process. As shown in Figure 5, the P2Y1 receptor antagonists MRS2179 and MRS2500, as well as the P2Y13 receptor antagonist MRS2211, significantly reduced the α,β-Me-ATP-induced relaxation (see asterisks in Figure 5Aa; −2.2±0.5 mN, n=12 for MRS2179, 0±0 mN, n=6 for MRS2500, and −1.0±0.3 mN, n=11 for MRS2211; Figure 5B), but the 2-Me-S-ADP-induced relaxation was only reduced by MRS2500 (−2.0±1.0 mN, n=12). Moreover, the sustained contraction induced by α,β-Me-ATP was also significantly reduced by all three P2Y receptor antagonists (Figure 5C). These data demonstrate that α,β-Me-ATP not only activates P2X receptors but also is a potent P2Y1 and P2Y13 agonist. We therefore expected that co-application of MRS2179 and MRS2211 would almost abolish the α,β-Me-ATP-induced effects. This was indeed the case for both the relaxation (0±0 mN, n=8, Figure 6B; see asterisk in Figure 6Aa) and the contraction (2.2±0.2 mN, n=8, Figure 6C). However, the 2-Me-S-ADP-induced relaxation was not affected by co-application of MRS2179 and MRS2211 (−5.0±1.7 mN, n=8, Figure 6B), indicating that 2-Me-S-ADP probably involves receptors other than P2Y1 and P2Y13.
In contrast to the P2Y1 and P2Y13 receptor antagonists, the P2Y6 receptor antagonist MRS2578 completely blocked 2-Me-S-ADP-induced relaxation (−0.8±0.3 mN, n=8, Figure 6B; see asterisk in Figure 6Ab), but enhanced the contraction (10.7±1.1 mN, n=8). Furthermore, MRS2578 partially but significantly reduced the α,β-Me-ATP-induced relaxation. These data suggest that the α,β-Me-ATP-induced relaxation is preferentially mediated by the P2Y1 and P2Y13 receptors but may also involve other receptors, while the 2-Me-S-ADP-induced relaxation is mediated by P2Y6 receptor activation (Figure 6B).
Discussion
The aim of this study was to investigate the molecular mechanisms of P2Y receptor-mediated motility in longitudinal ileum preparations. The non-hydrolyzable P2 receptor agonists α,β-Me-ATP and 2-Me-S-ADP caused a transient relaxation and a more sustained contraction of rat ileum smooth muscle. Moreover, we found that the transient relaxation was mediated by P2Y receptor activation and involved PLC, IP3-dependent Ca2+ release from internal stores and subsequently SK-type Ca2+-activated K+ channels. In contrast, the P2 receptor-induced contraction was abolished by the combined inhibition of sarcoendoplasmic reticulum ATPase and L-type voltage-dependent Ca2+ channels.
P2 receptors are involved in purinergic motility of the rat ileum
The purinergic agonist α,β-Me-ATP was introduced as an inhibitor of ionotropic P2X receptors24,29. However, Kitajima and co-workers have demonstrated that the α,β-Me-ATP-induced rise in the intracellular Ca2+ in aortic smooth muscle cells is not entirely prevented by verapamil, which indicates the involvement of non-L-type voltage-dependent Ca2+ channels and/or intracellular Ca2+ release following P2Y receptor activation30. More recently, α,β-Me-ATP was demonstrated to activate the P2Y1 receptor in the murine and human colon31. Indeed, in our study, both α,β-Me-ATP-induced relaxation and contraction were significantly reduced by the P2Y receptor blockers MRS2179, MRS2211 and MRS2500 and were abolished by co-application of both antagonists, suggesting the involvement of P2Y rather than P2X receptors in the rat ileum. Moreover, MRS2578 application led to a significant reduction in α,β-Me-ATP-induced relaxation. This observation might indicate that either P2Y6 is involved in α,β-Me-ATP-induced relaxation or that P2Y1 is also inhibited by MRS2578. Importantly, α,β-Me-ATP-induced contraction was also significantly reduced by verapamil, indicating the involvement of L-type Ca2+ channels presumably activated via P2X-mediated depolarization.
Eight subtypes of P2Y receptors have been cloned so far, five of which (P2Y1, P2Y2, P2Y4, P2Y6, P2Y11) are coupled to the activation of PLC via Gq/11 proteins and the remainder of which (P2Y12, P2Y13, P2Y14) negatively regulate adenylate cyclase via Gi/o proteins but may also activate PLC via βγ-subunits11. While MRS2179 and MRS2500 are quite selective for P2Y132, MRS2211 has a high affinity for the P2Y13 receptor but a lower affinity for P2Y1 and P2Y12 receptors33,34. Thus, we conclude that α,β-Me-ATP-induced relaxation and contraction were mediated by the activation of the P2Y1 and P2Y13 receptors, but the experiments using MRS2500 point to P2Y1 receptors having the predominant role.
The other purinoceptor agonist used in this study, 2-Me-S-ADP, has been developed as a P2Y receptor-preferring agonist35. While 2-Me-S-ADP-induced relaxation was not affected by co-application of MRS2179 and MRS2211, it was abolished by MRS2578, a P2Y6 receptor-antagonist, indicating that this receptor subtype was sufficient to generate the 2-Me-S-ADP-induced relaxation. Intriguingly, MRS2211 applied alone led to the induction of increased relaxation by 2-Me-S-ADP, for as yet unknown reasons. In contrast, the contraction induced by 2-Me-S-ADP was not affected by any of the P2Y receptor antagonists used in this study and was thus mediated by purinergic receptors other than P2Y1, P2Y6, P2Y12 or P2Y13.
Morphological data on P2 receptor distribution in the gut are scarce. At least in the mouse ileum, smooth muscle cells were strongly immunoreactive for P2Y1 receptors7, and myenteric plexus neurons in the guinea-pig ileum were shown to express the P2Y6 and P2Y12 receptor36. However, interspecies differences are very likely, because α,β-Me-ATP-induced contractions of guinea-pig ileum were sensitive to the P2X1 receptor antagonist NF279 and the P2X receptor-preferring blocker PPADS37. This finding is in contrast to the present results using rat ileum, which point to a predominant P2Y receptor-mediated contraction following exposure to α,β-Me-ATP.
Another important issue is pre-junctional P2 receptor expression. In particular, it is known that α,β-Me-ATP application leads to neural fiber-mediated cholinergic contractions5, and altered ATP release from cholinergic fibers in response to pre-junctional P2Y receptor activation may have occurred in our preparations8. Therefore, we examined the P2Y receptor-induced transient relaxation following pre-incubation with atropine, L-NAME or TTX and found that at least the P2Y receptor-mediated relaxation was independent of acetylcholine or nitric oxide release from pre-junctional nerve fibers.
Intracellular signaling cascade following purinergic receptor activation
The pharmacological experiments in the present study showed that the transient relaxation induced by either α,β-Me-ATP or 2-Me-S-ADP was abolished by apamin or UCL1684, indicating that SK channel activation was instrumental in purinergic relaxation. Hence, we suggest that purinergic relaxation might be due to membrane hyperpolarization following SK channel activation. Consistent with this idea, the sustained contraction following application of the P2 receptor agonists was not sensitive to SK channel inhibition. Moreover, the transient relaxation induced by either agonist was significantly reduced by 2-APB, thapsigargin and U73122. These results indicate that activation of PLC and subsequent IP3-dependent Ca2+ release from internal stores were important steps in the intracellular pathway leading to purinergic relaxation, and these steps are upstream of SK channel activation. In agreement with previous reports4,9,19,20, we propose that a major pathway leading to purinergic relaxation involves P2Y1 receptor and PLC activation, followed by IP3-mediated Ca2+ release from internal stores and subsequent SK channel activation.
It is important to note that smooth muscle cells may not be the only cell types involved in P2Y1 and SK channel-mediated purinergic relaxation. Recently, a new class of fibroblast-like cells expressing platelet derived growth factor receptor α (PDGFRα) have been described in the subepithelial layer of the gastrointestinal tract38. As has been demonstrated in both the murine detrusor muscle and colon, these cells express P2Y1 receptors coupled to SK channels, leading to purinergic inhibition39,40,41. Moreover, the effect of ATP was significantly reduced in PDGFRα-expressing cells from P2Y1-knockout mice, indicating a major role of P2Y1 in these cells40. It is therefore conceivable that these cells are also important mediators of purinergic relaxation in the rat ileum, which harbors SK3-expressing fibroblast-like cells that form gap junctions with smooth muscle cells42, as has recently been shown in the murine colon43. Another limitation of our study might be that purinergic receptors are also expressed in epithelial cells and hence are involved in secretory processes44,45,46. Therefore, we cannot exclude the possibility that purinoceptor activation-mediated secretion could have affected the relaxation and contraction in our preparations.
To further explore the subtype of the purinoceptor involved, we used pertussis toxin, which specifically and irreversibly inactivates Gi/o proteins. The G proteins not only inhibit adenylate cyclase but also activate PLC through their βγ-subunits47,48. Pertussis toxin can thus both stimulate adenylate cyclase and inhibit PLC28,49. In our study, pertussis toxin blocked 2-Me-S-ADP-induced relaxation, but had no effect on α,β-Me-ATP-induced relaxation. Because the effects of both agonists involved PLC signaling, the pertussis toxin data suggest that 2-Me-S-ADP involved the βγ-subunits of Gi/o proteins, whereas α,β-Me-ATP predominantly coupled to Gαq/11 proteins. As discussed above, α,β-Me-ATP-induced relaxation and contraction were mediated by P2Y1 and P2Y13 receptor activation. Because, according to the current knowledge, only P2Y1 is coupled to Gαq/1111, P2Y1 receptor-mediated motility fully compensated for the effects of both receptors under normal conditions. Thus, P2Y1 is a major purinoceptor on smooth muscle cells that governs rat ileum motility. In contrast, P2Y6 receptor inhibition abolished the relaxation induced by 2-Me-S-ADP, which was also largely pertussis toxin-sensitive. These data suggest that P2Y6 is not only coupled to Gq/11 as currently thought11 but also leads to Gi/o activation. Activation of different G protein species has previously been described for adenosine receptors50.
Purinergic contraction, however, was not affected by 2-APB or thapsigargin, suggesting that Ca2+ release from internal stores may not be involved in this process. Because 2-APB has been observed to interfere with store-operated Ca2+ entry25,51, this mechanism is not required. However, 2-Me-S-ADP-induced contraction, but not α,β-Me-ATP-induced contraction, was sensitive to U73122, indicating a potential role for PLC and subsequent intracellular Ca2+ signaling in mediating P2Y purinergic contraction for both motility responses, confirming previous reports52,53. In contrast, contraction induced by either agonist was abolished by co-application of the SERCA inhibitor thapsigargin and the L-type Ca2+ channel blocker verapamil. Thus, purinergic contraction might partially involve Ca2+ influx through voltage-gated Ca2+ channels, Ca2+ release from internal stores and other mechanisms downstream of PLC activation such as Rho kinase signaling54.
One potential caveat of our study might be that contractile activity measured in the longitudinal direction could be affected by epithelium-derived factors and/or by modulation via the electrically coupled circular layer of the smooth muscle. Although this possibility cannot be excluded, several observations argue against it. The ileum segments were closed on both ends by sutures to fix them in the organ bath. Thus, when the drug diffuses, it should first reach the outer longitudinal layer, while the inner circular layer and the epithelium should be reached much later. The latency between the administration of purinergic agonists (injection of 100 μL into 25 mL volume) and transient relaxation was approximately 8–10 s. Hence, we think that it is unlikely, albeit possible, that purinergic agonists exerted their effects indirectly by acting on the circular layer and/or the epithelium.
Another limitation of the present study is that pharmacological manipulation may activate multiple receptors, including extra-junctional ones, unlike electrical field stimulation (EFS) (which acts only on junctional receptors). EFS studies are required to confirm the findings made here.
Conclusion
In summary, our data provide evidence that P2Y receptor activation by α,β-Me-ATP or 2-Me-S-ADP leads to both Gq/11- and Gi/o-dependent and PLC-mediated IP3 production. While α,β-Me-ATP acts via P2X, P2Y1 and P2Y13 receptors, 2-Me-S-ADP activates both the P2Y1 and P2Y6 receptors. Overall, the P2Y1 receptor appears to be the major purinoceptor subtype involved in purinergic relaxation. Following PLC activation, IP3 is produced and activates the release of Ca2+ from internal thapsigargin-sensitive stores, which leads to the activation of SK channels. Because these channels sense the intracellular Ca2+ concentration, they give rise to a K+ outward current, leading to hyperpolarization and thus relaxation.
Author contribution
Felix MADER, Ludwig KRAUSE, and Tursonjan TOKAY performed the experiments; Timo KIRSCHSTEIN designed the study, performed the statistical analysis, and prepared the manuscript; Oliver W HAKENBERG and Rüdiger KÖHLING participated in the design of the study and prepared the manuscript. All authors read and approved the final manuscript.
References
Burnstock G . The journey to establish purinergic signalling in the gut. Neurogastroenterol Motil 2008; 20 Suppl 1: 8–19.
Benkó R, Undi S, Wolf M, Magyar K, Tóvölgyi Z, Rumbus Z, et al. P(2) purinoceptors account for the non-nitrergic NANC relaxation in the ratileum. Naunyn Schmiedebergs Arch Pharmacol 2006; 373: 319–24.
Wang GD, Wang XY, Hu HZ, Liu S, Gao N, Fang X, et al. Inhibitory neuromuscular transmission mediated by the P2Y1 purinergic receptor in guinea pig small intestine. Am J Physiol Gastrointest Liver Physiol 2007; 292: G1483–9.
Waseda K, Takeuchi T, Ohta M, Okishio Y, Fujita A, Hata F, et al. Participation of ATP in nonadrenergic, noncholinergic relaxation of longitudinal muscle of wistar rat jejunum. J Pharmacol Sci 2005; 97: 91–100.
Barthó L, Undi S, Benkó R, Wolf M, Lázár Z, Lénárd L Jr, et al. Multiple motor effects of ATP and their inhibition by P purinoceptor antagonist, pyridoxalphosphate-6-azophenyl-2′,4′-disulphonic acid in the small intestine of the guinea-pig. Basic Clin Pharmacol Toxicol 2006; 98: 488–95.
Duarte-Araújo M, Nascimento C, Timóteo MA, Magalhães-Cardoso MT, Correia-de-Sá P . Relative contribution of ecto-ATPase and ecto-ATPDase pathways to the biphasic effect of ATP on acetylcholine release from myenteric motoneurons. Br J Pharmacol 2009; 156: 519–33.
Giaroni C, Knight GE, Ruan HZ, Glass R, Bardini M, Lecchini S, et al. P2 receptors in the murine gastrointestinal tract. Neuropharmacology 2002; 43: 1313–23.
Matsuo K, Katsuragi T, Fujiki S, Sato C, Furukawa T . ATP release and contraction mediated by different P2-receptor subtypes in guinea-pig ileal smooth muscle. Br J Pharmacol 1997; 121: 1744–8.
Storr M, Franck H, Saur D, Schusdziarra V, Allescher HD . Mechanisms of alpha,beta-methylene atp-induced inhibition in rat ileal smooth muscle: involvement of intracellular Ca2+ stores in purinergic inhibition. Clin Exp Pharmacol Physiol 2000; 27: 771–9.
Zizzo MG, Mulè F, Serio R . Inhibitory purinergic transmission in mouse caecum: role for P2Y1 receptors as prejunctional modulators of ATP release. Neuroscience 2007; 150: 658–64.
Abbracchio MP, Burnstock G, Boeynaems JM, Barnard EA, Boyer JL, Kennedy C, et al. International Union of Pharmacology LVIII: update on the P2Y G protein-coupled nucleotide receptors: from molecular mechanisms and pathophysiology to therapy. Pharmacol Rev 2006; 58: 281–341.
Xiang Z, Burnstock G . P2X2 and P2X3 purinoceptors in the rat enteric nervous system. Histochem Cell Biol 2004; 121: 169–79.
Gallego D, Hernandez P, Clave P, Jimenez M . P2Y1 receptors mediate inhibitory purinergic neuromuscular transmission in the human colon. Am J Physiol Gastrointest Liver Physiol 2006; 291: G584–94.
Gallego D, Vanden Berghe P, Farre R, Tack J, Jimenez M . P2Y1 receptors mediate inhibitory neuromuscular transmission and enteric neuronal activation in small intestine. Neurogastroenterol Motil 2008; 20: 159–68.
Gallego D, Gil V, Aleu J, Martinez-Cutillas M, Clave P, Jimenez M . Pharmacological characterization of purinergic inhibitory neuromuscular transmission in the human colon. Neurogastroenterol Motil 2011; 23: 792–e338.
Gil V, Martinez-Cutillas M, Mane N, Martin MT, Jimenez M, Gallego D . P2Y(1) knockout mice lack purinergic neuromuscular transmission in the antrum and cecum. Neurogastroenterol Motil 2013; 25: e170–82.
Hwang SJ, Blair PJ, Durnin L, Mutafova-Yambolieva V, Sanders KM, Ward SM . P2Y1 purinoreceptors are fundamental to inhibitory motor control of murine colonic excitability and transit. J Physiol 2012; 590: 1957–72.
Gallego D, Gil V, Martinez-Cutillas M, Mane N, Martin MT, Jimenez M . Purinergic neuromuscular transmission is absent in the colon of P2Y(1) knocked out mice. J Physiol 2012; 590: 1943–56.
Blottière HM, Loirand G, Pacaud P . Rise in cytosolic Ca2+ concentration induced by P2-purinoceptor activation in isolated myocytes from the rat gastrointestinal tract. Br J Pharmacol 1996; 117: 775–80.
Pacaud P, Feolde E, Frelin C, Loirand G . Characterization of the P2Y-purinoceptor involved in the ATP-induced rise in cytosolic Ca2+ concentration in rat ileal myocytes. Br J Pharmacol 1996; 118: 2213–9.
Kirschstein T, Rehberg M, Bajorat R, Tokay T, Porath K, Köhling R . High K+-induced contraction requires depolarization-induced Ca2+ release from internal stores in rat gut smooth muscle. Acta Pharmacol Sin 2009; 30: 1123–31.
Kirschstein T, Dammann F, Klostermann J, Rehberg M, Tokay T, Schubert R, et al. Dopamine induces contraction in the proximal, but relaxation in the distal rat isolated small intestine. Neurosci Lett 2009; 465: 21–6.
Kasakov L, Burnstock G . The use of the slowly degradable analog, alpha, beta-methylene ATP, to produce desensitisation of the P2-purinoceptor: effect on non-adrenergic, non-cholinergic responses of the guinea-pig urinary bladder. Eur J Pharmacol 1982; 86: 291–4.
Bo XN, Burnstock G . High- and low-affinity binding sites for 3H]-alpha, beta-methylene ATP in rat urinary bladder membranes. Br J Pharmacol 1990; 101: 291–6.
Várnai P, Hunyady L, Balla T . STIM and Orai: the long-awaited constituents of store-operated calcium entry. Trends Pharmacol Sci 2009; 30: 118–28.
Ohata H, Kawanishi T, Kawanishi M, Uneyama C, Takahashi M, Momose K . Spontaneous oscillations of cytoplasmic free calcium ion concentration in cultured smooth muscle cells from guinea pig ileum. Jpn J Pharmacol 1993; 63: 83–91.
Sternweis PC, Smrcka AV . G proteins in signal transduction: the regulation of phospholipase C. Ciba Found Symp 1993; 176: 96–111.
Boyer J, Paterson A, Harden TK . G-protein-mediated regulation of phospholipase C Involvement of βγ subunits. Trends Cardiovasc Med 1994; 4: 88–95.
Schlicker E, Urbanek E, Göthert M . ATP, alpha,beta-methylene ATP and suramin as tools for characterization of vascular P2x receptors in the pithed rat. J Auton Pharmacol 1989; 9: 357–66.
Kitajima S, Ozaki H, Karaki H . The effects of ATP and alpha,beta-methylene-ATP on cytosolic Ca2+ level and force in rat isolated aorta. Br J Pharmacol 1993; 110: 263–8.
Martínez-Cutillas M, Gil V, Gallego D, Mañé N, Clavé P, Martín MT, et al. α,β-meATP mimics the effects of the purinergic neurotransmitter in the human and rat colon. Eur J Pharmacol 2014; 740: 442–54.
Boyer JL, Mohanram A, Camaioni E, Jacobson KA, Harden TK . Competitive and selective antagonism of P2Y1 receptors by N6-methyl 2′-deoxyadenosine 3′,5′-bisphosphate. Br J Pharmacol 1998; 124: 1–3.
Kim YC, Lee JS, Sak K, Marteau F, Mamedova L, Boeynaems JM, et al. Synthesis of pyridoxal phosphate derivatives with antagonist activity at the P2Y13 receptor. Biochem Pharmacol 2005; 70: 266–74.
Von Kügelgen I . Pharmacological profiles of cloned mammalian P2Y-receptor subtypes. Pharmacol Ther 2006; 110: 415–32.
Sak K, Webb TE . A retrospective of recombinant P2Y receptor subtypes and their pharmacology. Arch Biochem Biophys 2002; 397: 131–6.
Xiang Z, Burnstock G . Distribution of P2Y6 and P2Y12 receptor: their colocalization with calbindin, calretinin and nitric oxide synthase in the guinea pig enteric nervous system. Histochem Cell Biol 2006; 125: 327–36.
Benkó R, Undi S, Wolf M, Barthó L . Effects of acute administration of and tachyphylaxis to alpha,beta-methylene ATP in the guinea-pig small intestine. Basic Clin Pharmacol Toxicol 2005; 97: 369–73.
Kurahashi M, Nakano Y, Peri LE, Townsend JB, Ward SM, Sanders KM . A novel population of subepithelial platelet-derived growth factor receptor α-positive cells in the mouse and human colon. Am J Physiol Gastrointest Liver Physiol 2013; 304: G823–34.
Lee H, Koh BH, Peri LE, Sanders KM, Koh SD . Functional expression of SK channels in murine detrusor PDGFR+ cells. J Physiol 2013; 591: 503–13.
Lee H, Koh BH, Peri LE, Sanders KM, Koh SD . Purinergic inhibitory regulation of murine detrusor muscles mediated by PDGFRα+ interstitial cells. J Physiol 2014; 592: 1283–93.
Baker SA, Hennig GW, Ward SM, Sanders KM . Temporal sequence of activation of cells involved in purinergic neurotransmission in the colon. J Physiol 2015; 593: 1945–63.
Fujita A, Takeuchi T, Jun H, Hata F . Localization of Ca2+-activated K+ channel, SK3, in fibroblast-like cells forming gap junctions with smooth muscle cells in the mouse small intestine. J Pharmacol Sci 2003; 92: 35–42.
Kurahashi M, Mutafova-Yambolieva V, Koh SD, Sanders KM . Platelet-derived growth factor receptor-α-positive cells and not smooth muscle cells mediate purinergic hyperpolarization in murine colonic muscles. Am J Physiol Cell Physiol 2014; 307: C561–70.
O'Mullane LM, Cook DI, Dinudom A . Purinergic regulation of the epithelial Na+ channel. Clin Exp Pharmacol Physiol 2009; 36: 1016–22.
Christofi FL, Wunderlich J, Yu JG, Wang YZ, Xue J, Guzman J, et al. Mechanically evoked reflex electrogenic chloride secretion in rat distal colon is triggered by endogenous nucleotides acting at P2Y1, P2Y2, and P2Y4 receptors. J Comp Neurol 2004; 469: 16–36.
Köttgen M, Löffler T, Jacobi C, Nitschke R, Pavenstädt H, Schreiber R, et al. P2Y6 receptor mediates colonic NaCl secretion via differential activation of cAMP-mediated transport. J Clin Invest 2003; 111: 371–9.
Chan JS, Lee JW, Ho MK, Wong YH . Preactivation permits subsequent stimulation of phospholipase C by G(i)-coupled receptors. Mol Pharmacol 2000; 57: 700–8.
Murthy KS, Zhou H, Huang J, Pentyala SN . Activation of PLC-δ1 by Gi/o-coupled receptor agonists. Am J Physiol Cell Physiol 2004; 287: C1679–87.
Zhou H, Murthy KS . Distinctive G protein-dependent signaling in smooth muscle by sphingosine 1-phosphate receptors S1P1 and S1P2. Am J Physiol Cell Physiol 2004; 286: C1130–8.
Jacobson KA, Gao ZG . Adenosine receptors as therapeutic targets. Nat Rev Drug Discov 2006; 5: 247–64.
Bootman MD, Collins TJ, Mackenzie L, Roderick HL, Berridge MJ, Peppiatt CM . 2-Aminoethoxydiphenyl borate (2-APB) is a reliable blocker of store-operated Ca2+ entry but an inconsistent inhibitor of InsP3-induced Ca2+ release. FASEB J 2002; 16: 1145–50.
Tanaka N, Kawasaki K, Nejime N, Kubota Y, Nakamura K, Kunitomo M, et al. P2Y receptor-mediated Ca2+ signaling increases human vascular endothelial cell permeability. J Pharmacol Sci 2004; 95: 174–80.
Weng JY, Hsu TT, Sun SH . Functional characterization of P2Y1 versus P2X receptors in RBA-2 astrocytes: elucidate the roles of ATP release and protein kinase C. J Cell Biochem 2008; 104: 554–67.
Tanaka N, Nejime N, Kubota Y, Kagota S, Yudo K, Nakamura K, et al. Myosin light chain kinase and Rho-kinase participate in P2Y receptor-mediated acceleration of permeability through the endothelial cell layer. J Pharm Pharmacol 2005; 57: 335–40.
Acknowledgements
The authors wish to thank Katrin PORATH, Tina SELLMANN and Hanka SCHMIDT for excellent technical assistance. This research was supported by a grant from the Medical Faculty of the University of Rostock to Timo KIRSCHSTEIN.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mader, F., Krause, L., Tokay, T. et al. P2Y receptor-mediated transient relaxation of rat longitudinal ileum preparations involves phospholipase C activation, intracellular Ca2+ release and SK channel activation. Acta Pharmacol Sin 37, 617–628 (2016). https://doi.org/10.1038/aps.2015.137
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2015.137
- Springer Nature Singapore Pte Ltd.
Keywords
This article is cited by
-
The P2Y1 receptor in the colonic myenteric plexus of rats and its correlation with opioid-induced constipation
BMC Gastroenterology (2024)