Abstract
Background
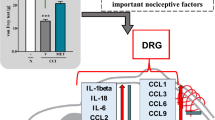
The G protein-coupled receptor 35 (GPR35), is considered important for nociceptive transmission, as suggested by accumulating evidence. This receptor was discovered in 1998; however, a lack of pharmacological tools prevented a complete understanding of its function and how to exploit it therapeutically. We studied the influence of CXCL17, kynurenic acid and zaprinast on nociceptive transmission in naïve and neuropathic mice. Additionally, we investigated the influence of kynurenic acid and zaprinast on morphine effectiveness in neuropathic pain.
Methods
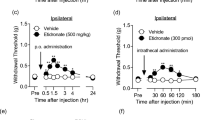
The chronic constriction injury (CCI) of the sciatic nerve in Swiss mice was performed. The CXCL17, kynurenic acid, zaprinast and morphine were injected intrathecally into naive and CCI-exposed mice at day 14. To evaluate tactile and thermal hypersensitivity, the von Frey and cold plate tests were used, respectively.
Results
Our results have shown, for the first time, that administration of CXCL17 in naïve mice induced strong pain-related behaviours, as measured by von Frey and cold plate tests. Moreover, we demonstrated that kynurenic acid and zaprinast diminished CXCL17-evoked pain-related behaviours in both tests. Kynurenic acid and zaprinast reduced thermal and tactile hypersensitivity developed by sciatic nerve injury and strongly enhanced the effectiveness of morphine in neuropathy.
Conclusions
Our study highlights the importance of GPR35 as a receptor involved in neuropathic pain development. Therefore, these results suggest that the modulation of GPR35 could become a potential strategy for the treatment of neuropathic pain.
Similar content being viewed by others
References
Kalso E, Edwards JE, Moore RA, McQuay HJ. Opioids in chronic non-cancer pain: systematic review of efficacy and safety. Pain 2004;112:372–80, doi: https://doi.org/10.1016/j.pain.2004.09.019.
Dworkin RH, O’Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc 2010;85:S3–14, doi: https://doi.org/10.4065/mcp.2009.0649.
Truini A, Garcia-Larrea L, Cruccu G. Reappraising neuropathic pain in humans—how symptoms help disclose mechanisms. Nat Rev Neurol 2013;9:572–82, doi: https://doi.org/10.1038/nrneurol.2013.180.
Lotfy Mohamed, Ashri NH, Khairy MM. Truncal neuralgia in diabetic patients: an ignored cause of abdominal pain. Edorium J Surg 2017;4:14–7, doi: https://doi.org/10.5348/S05-2017-19-OA-3.
Mika J, Zychowska M, Popiolek-Barczyk K, Rojewska E, Przewlocka B. Importance of glial activation in neuropathic pain. Eur J Pharmacol 2013;716:106–19, doi: https://doi.org/10.1016/j.ejphar.2013.01.072.
Popiolek-Barczyk K, Mika J. Targeting the microglial signaling pathways: new insights in the modulation of neuropathic pain. Curr Med Chem 2016;23:2908–28, doi: https://doi.org/10.2174/09298673236661606071.
Pabreja K, Dua K, Sharma S, Padi SSV, Kulkarni SK. Minocycline attenuates the development of diabetic neuropathic pain: possible anti-inflammatory and anti-oxidant mechanisms. Eur J Pharmacol 2011;661:15–21, doi: https://doi.org/10.1016/j.ejphar.2011.04.014.
Tang W, Lv Q, Chen X, Zou J, Liu Z, Shi Y. CD8 + T cell-mediated cytotoxicity toward schwann cells promotes diabetic peripheral neuropathy. Cell Physiol Biochem 2013;32:827–37, doi: https://doi.org/10.1159/000354485.
Zychowska M, Rojewska E, Przewlocka B, Mika J. Mechanisms and pharmacology of diabetic neuropathy — experimental and clinical studies. Pharmacol Rep 2013;65:1601–10, doi: https://doi.org/10.1016/S1734-1140(13)71521-4.
Zychowska M, Rojewska E, Pilat D, Mika J. The role of some chemokines from the CXC subfamily in a mouse model of diabetic neuropathy. J Diab Res 2015;2015:750182, doi: https://doi.org/10.1155/2015/750182.
Zychowska M, Rojewska E, Piotrowska A, Kreiner G, Nalepa I, Mika J. Spinal CCL1/CCR8 signaling interplay as a potential therapeutic target — evidence from a mouse diabetic neuropathy model. Int Immunopharmacol 2017;52:261–71, doi: https://doi.org/10.1016/j.intimp.2017.09.021.
Rojewska E, Zychowska M, Piotrowska A, Kreiner G, Nalepa I, Mika J. Involvement of macrophage inflammatory protein-1 family members in the development of diabetic neuropathy and their contribution to effectiveness of morphine. Front Immunol 2018;9:494, doi: https://doi.org/10.3389/fimmu.2018.00494.
Clark AK, Yip PK, Malcangio M. The liberation of fractalkine in the dorsal horn requires microglial cathepsin S. J Neurosci 2009;29:6945–54, doi: https://doi.org/10.1523/JNEUROSCI.0828-09.2009.
Clark AK, Malcangio M. Microglial signalling mechanisms: Cathepsin S and Fractalkine. Exp Neurol 2012;234:283–92, doi: https://doi.org/10.1016/j.expneurol.2011.09.012.
Abbadie C, Bhangoo S, De Koninck Y, Malcangio M, Melik-Parsadaniantz S, White FA. Chemokines and pain mechanisms. Brain Res Rev 2009;60:125–34, doi: https://doi.org/10.1016/j.brainresrev.2008.12.002.
Gao Y-J, Ji R-R. Chemokines, neuronal-glial interactions, and central processing of neuropathic pain. Pharmacol Ther 2010;126:56–68, doi: https://doi.org/10.1016/j.pharmthera.2010.01.002.
Kwiatkowski K, Piotrowska A, Rojewska E, Makuch W, Mika J. The RS504393 influences the level of nociceptive factors and enhances opioid analgesic potency in neuropathic rats. J Neuroimmune Pharmacol 2017;12:402–19, doi: https://doi.org/10.1007/s11481-017-9729-6.
Piotrowska A, Kwiatkowski K, Rojewska E, Slusarczyk J, Makuch W, Basta-Kaim A, et al. Direct and indirect pharmacological modulation of CCL2/CCR2 pathway results in attenuation of neuropathic pain — in vivo and in vitro evidence. J Neuroimmunol 2016;297:9–19, doi: https://doi.org/10.1016/j.jneuroim.2016.04.017.
Van Steenwinckel J, Reaux-Le Goazigo A, Pommier B, Mauborgne A, Dansereau M-A, Kitabgi P, et al. CCL2 released from neuronal synaptic vesicles in the spinal cord is a major mediator of local inflammation and pain after peripheral nerve injury. J Neurosci 2011;31:5865–75, doi: https://doi.org/10.1523/JNEUROSCI.5986-10.2011.
Zhang J, Shi XQ, Echeverry S, Mogil JS, De Koninck Y, Rivest S. Expression of CCR2 in both resident and bone marrow-derived microglia plays a critical role in neuropathic pain. J Neurosci 2007;27:12396–406, doi: https://doi.org/10.1523/JNEUROSCI.3016-07.2007.
Bhangoo SK, Ripsch MS, Buchanan DJ, Miller RJ, White FA. Increased chemokine signaling in a model of HIV1-associated peripheral neuropathy. Mol Pain 2009;5:48, doi: https://doi.org/10.1186/1744-8069-5-48.
Zhang Z-J, Dong Y-L, Lu Y, Cao S, Zhao Z-Q, Gao Y-J. Chemokine CCL2 and its receptor CCR2 in the medullary dorsal horn are involved in trigeminal neuropathic pain. J Neuroinflamm 2012;9:569, doi: https://doi.org/10.1186/1742-2094-9-136.
Zychowska M, Rojewska E, Piotrowska A, Kreiner G, Mika J. Microglial inhibition influences XCL1/XCR1 expression and causes analgesic effects in a mouse model of diabetic neuropathy. Anesthesiology 2016;125:573–89, doi: https://doi.org/10.1097/ALN.0000000000001219.
Kiguchi N, Maeda T, Kobayashi Y, Fukazawa Y, Kishioka S. Macrophage inflammatory protein-1β mediates the development of neuropathic pain following peripheral nerve injury through interleukin-1β up-regulation. Pain 2010;149:305–15, doi: https://doi.org/10.1016/j.pain.2010.02.025.
Kwiatkowski K, Piotrowska A, Rojewska E, Makuch W, Jurga A, Slusarczyk J, et al. Beneficial properties of maraviroc on neuropathic pain development and opioid effectiveness in rats. Prog Neurol-Psychopharmacol Biol Psychiatry 2016;64:68–78, doi: https://doi.org/10.1016/j.pnpbp.2015.07.005.
Maravillas-Montero JL, Burkhardt AM, Hevezi PA, Carnevale CD, Smit MJ, Zlotnik A. Cutting edge: GPR35/CXCR8 is the receptor of the mucosal chemokine CXCL17. J Immunol 2015;194:29–33, doi: https://doi.org/10.4049/jimmunol.1401704.
Divorty N, Mackenzie AE, Nicklin SA, Milligan G. G protein-coupled receptor 35: an emerging target in inflammatory and cardiovascular disease. Front Pharmacol 2015;6:, doi: https://doi.org/10.3389/fphar.2015.00041.
MacKenzie AE, Lappin JE, Taylor DL, Nicklin SA, Milligan G. GPR35 as a novel therapeutic target. Front Endocrinol (Lausanne) 2011;2:, doi: https://doi.org/10.3389/fendo.2011.00068.
Milligan G. Orthologue selectivity and ligand bias: translating the pharmacology of GPR35. Trends Pharmacol Sci 2011;32:317–25, doi: https://doi.org/10.1016/j.tips.2011.02.002.
Reggio PH, Shore DM. The therapeutic potential of orphan GPCRs, GPR35 and GPR55. Front Pharmacol 2015;6:1–22, doi: https://doi.org/10.3389/fphar.2015.00069.
Mackenzie AE, Milligan G. The emerging pharmacology and function of GPR35 in the nervous system. Neuropharmacology 2017;113:661–71, doi: https://doi.org/10.1016/J.NEUROPHARM.2015.07.035.
Zhao P, Lane TR, Gao HGL, Hurst DP, Kotsikorou E, Le L, et al. Crucial positively charged residues for ligand activation of the GPR35 receptor. J Biol Chem 2014;289:3625–38, doi: https://doi.org/10.1074/jbc.M113.508382.
Resta F, Masi A, Sili M, Laurino A, Moroni F, Mannaioni G. Kynurenic acid and zaprinast induce analgesia by modulating HCN channels through GPR35 activation. Neuropharmacology 2016;108:136–43, doi: https://doi.org/10.1016/j.neuropharm.2016.04.038.
Zimmermann M. Ethical guidelines for investigations of experimental pain in conscious animals. Pain 1983;16:109–10.
Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain 1988;33:87–107, doi: https://doi.org/10.1016/0304-3959(88)90209-6.
Mika J, Osikowicz M, Rojewska E, Korostynski M, Wawrzczak-Bargiela A, Przewlocki R, et al. Differential activation of spinal microglial and astroglial cells in a mouse model of peripheral neuropathic pain. Eur J Pharmacol 2009;623:65–72, doi: https://doi.org/10.1016/j.ejphar.2009.09.030.
Starnowska J, Costante R, Guillemyn K, Popiolek-Barczyk K, Chung NN, Lemieux C, et al. Analgesic properties of Opioid/NK1 multitarget ligands with distinct in vitro profiles in naive and chronic constriction injury mice. ACS Chem Neurosci 2017;8:2315–24, doi: https://doi.org/10.1021/acschemneuro.7b00226.
Mika J, Jurga AM, Starnowska J, Wasylewski M, Rojewska E, Makuch W, et al. Effects of chronic doxepin and amitriptyline administration in naïve mice and in neuropathic pain mice model. Neuroscience 2015;294:38–50, doi: https://doi.org/10.1016/j.neuroscience.2015.03.003.
Hylden JLK, Wilcox GL. Intrathecal morphine in mice: a new technique. Eur J Pharmacol 1980;67:313–6, doi: https://doi.org/10.1016/0014-2999(80) 90515-4.
Fukui S, Schwarcz R, Rapoport SI, Takada Y, Smith QR. Blood-brain barrier transport of kynurenines: implications for brain synthesis and metabolism. J Neurochem 1991, doi: https://doi.org/10.1111/j.1471-4159.1991.tb03460.x.
Tuboly G, Tar L, Bohar Z, Safrany-Fark A, Petrovszki Z, Kekesi G, et al. The inimitable kynurenic acid: the roles of different ionotropic receptors in the action of kynurenic acid at a spinal level. Brain Res Bull 2015, doi: https://doi.org/10.1016/j.brainresbull.2015.02.001.
Zhang YQ, Ji GC, Wu GC, Zhao ZQ. Kynurenic acid enhances electroacupuncture analgesia in normal and carrageenan-injected rats. Brain Res 2003;966:300–7, doi: https://doi.org/10.1016/S0006-8993(02)04228-2.
Alkondon M, Pereira EFR, Todd SW, Randall WR, Lane MV, Albuquerque EX. Functional G-protein-coupled receptor 35 is expressed by neurons in the CA1 field of the hippocampus. Biochem Pharmacol 2015;93:506–18, doi: https://doi.org/10.1016/j.bcp.2014.12.009.
Berlinguer-Palmini R, Masi A, Narducci R, Cavone L, Maratea D, Cozzi A, et al. GPR35 activation reduces Ca2+ transients and contributes to the kynurenic acid-dependent reduction of synaptic activity at CA3-CA1 synapses. PLoS One 2013;8:, doi: https://doi.org/10.1371/journal.pone.0082180.
Cosi C, Mannaioni G, Cozzi A, Carlà V, Sili M, Cavone L, et al. G-protein coupled receptor 35 (GPR35) activation and inflammatory pain: studies on the antinociceptive effects of kynurenic acid and zaprinast. Neuropharmacology 2011;60:1227–31, doi: https://doi.org/10.1016/J.NEUROPHARM.2010.11.014.
Wang J, Simonavicius N, Wu X, Swaminath G, Reagan J, Tian H, et al. Kynurenic acid as a ligand for orphan G protein-coupled receptor GPR35. J Biol Chem 2006;281:, doi: https://doi.org/10.1074/jbc.M60350320022021-8.
Ohshiro H, Tonai-Kachi H, Ichikawa K. GPR35 is a functional receptor in rat dorsal root ganglion neurons. Biochem Biophys Res Commun 2008;365:, doi: https://doi.org/10.1016/j.bbrc.2007.10.197 344–8.
Taniguchi Y, Tonai-Kachi H, Zaprinast Shinjo K. A well-known cyclic guanosine monophosphate-specific phosphodiesterase inhibitor, is an agonist for GPR35. FEBS Lett 2006;580:5003–8, doi: https://doi.org/10.1016/j.febslet.2006.08.015.
Guo YJ, Zhou YJ, Yang XL, Shao ZM, Ou ZL. The role and clinical significance of the CXCL17-CXCR8 (GPR35) axis in breast cancer. Biochem Biophys Res Commun 2017;493:1159–67, doi: https://doi.org/10.1016/j.bbrc.2017.09.113.
Binti NAS, Amir M, Mackenzie AE, Boustani K, Hillier MC, Milligan G, et al. Evidence for the existence of a CXCL17 receptor distinct from GPR35., doi: https://doi.org/10.4049/jimmunol.1700884.
Park SJ, Lee SJ, Nam SY, Im DS. GPR35 mediates lodoxamide-induced migration inhibitory response but not CXCL17-induced migration stimulatory response in THP-1 cells; is GPR35 a receptor for CXCL17? Br J Pharmacol 2018;175:154–61, doi: https://doi.org/10.1111/bph.14082.
Mu X, Chen Y, Wang S, Huang X, Pan H, Li M. Overexpression of VCC-1 gene in human hepatocellular carcinoma cells promotes cell proliferation and invasion. Acta Biochim Biophys Sin (Shanghai) 2009;41:631–7.
Lee W-Y, Wang C-J, Lin T-Y, Hsiao C-L, Luo C-W. CXCL17, an orphan chemokine, acts as a novel angiogenic and anti-inflammatory factor. Am J Physiol Metab 2013;304:E32–40, doi: https://doi.org/10.1152/ajpendo.00083.2012.
Hiraoka N, Yamazaki-Itoh R, Ino Y, Mizuguchi Y, Yamada T, Hirohashi S, et al. CXCL17 and ICAM2 are associated with a potential anti-tumor immune response in early intraepithelial stages of human pancreatic carcinogenesis. Gastroenterology 2011;140:310–21, doi: https://doi.org/10.1053/J.GASTRO.2010.10.009e4.
Weinstein EJ, Head R, Griggs DW, Sun D, Evans RJ, Swearingen ML, et al. VCC-1, a novel chemokine, promotes tumor growth. Biochem Biophys Res Commun 2006;350:74–81, doi: https://doi.org/10.1016/J.BBRC.2006.08.194.
Zhang Z-J, Cao D-L, Zhang X, Ji R-R, Gao Y-J. Chemokine contribution to neuropathic pain: respective induction of CXCL1 and CXCR2 in spinal cord astrocytes and neurons. Pain 2013;154:2185–97, doi: https://doi.org/10.1016/j.pain.2013.07.002.
Piotrowska A, Rojewska E, Pawlik K, Kreiner G, Ciechanowska A, Makuch W, et al. Pharmacological blockade of CXCR3 by (±)-NBI-74330 reduces neuropathic pain and enhances opioid effectiveness — evidence from in vivo and in vitro studies. Biochim Biophys Acta 2018;1864:3418–37, doi: https://doi.org/10.1016/j.bbadis.2018.07.032S0925-4439:30281-3.
Zhang Q, Cao D-L, Zhang Z-J, Jiang B-C, Gao Y-J. Chemokine CXCL13 mediates orofacial neuropathic pain via CXCR5/ERK pathway in the trigeminal ganglion of mice. J Neuroinflamm 2016;13:183, doi: https://doi.org/10.1186/s12974-016-0652-1.
Montague K, Malcangio M. The therapeutic potential of targeting chemokine signalling in the treatment of chronic pain. J Neurochem 2017;141:520–31, doi: https://doi.org/10.1111/jnc.13927.
Burkhardt AM, Tai KP, Flores-Guiterrez JP, Vilches-Cisneros N, Kamdar K, Barbosa-Quintana O, et al. CXCL17 is a mucosal chemokine elevated in idiopathic pulmonary fibrosis that exhibits broad antimicrobial activity. J Immunol 2012;188:6399–406, doi: https://doi.org/10.4049/jimmunol.1102903.
Watkins LR, Hutchinson MR, Johnston IN, Maier SF. Glia: novel counter-regulators of opioid analgesia. Trends Neurosci 2005;28:661–9, doi: https://doi.org/10.1016/j.tins.2005.10.001.
Mika J. Modulation of microglia can attenuate neuropathic pain symptoms and enhance morphine effectiveness. Pharmacol Rep 2008;60:297–307, doi: https://doi.org/10.1080/15360280902901404.
Mika J, Obara I, Przewlocka B. The role of nociceptin and dynorphin in chronic pain: implications of neuro-glial interaction. Neuropeptides 2011;45:247–61, doi: https://doi.org/10.1016/j.npep.2011.03.002.
Marchand F, Perretti M, McMahon SB. Role of the immune system in chronic pain. Nat Rev Neurosci 2005;6:521–32, doi: https://doi.org/10.1038/nrn1700.
Moroni F, Cozzi A, Sili M, Mannaioni G. Kynurenic acid: a metabolite with multiple actions and multiple targets in brain and periphery. J Neural Trans 2012;119:133–9, doi: https://doi.org/10.1007/s00702-011-0763-x.
Bespalov AY, Beardsley PM, Balster RL. Interactions between N-methyl-d-aspartate receptor antagonists and the discriminative stimulus effects of morphine in rats. Pharmacol Biochem Behav 1998;507–17.
Chess AC, Simoni MK, Alling TE, Bucci DJ. Elevations of endogenous kynurenic acid produce spatial working memory deficits. Schizophr Bull 2007;797–804, doi: https://doi.org/10.1093/schbul/sbl033.
Koola MM. Galantamine-memantine combination for cognitive impairments due to electroconvulsive therapy, traumatic brain injury, and neurologic and psychiatric disorders: kynurenic acid and mismatch negativity target engagement. Prim Care Companion CNS Disord 2018;20(2), doi: https://doi.org/10.4088/PCC.17nr02235.
Banerjee J, Alkondon M, Pereira EFR, Albuquerque EX. Regulation of GABAergic inputs to CA1 pyramidal neurons by nicotinic receptors and kynurenic acid. J Pharmacol Exp Ther 2012;500-9, doi: https://doi.org/10.1124/jpet.111.189860.
Elmslie KS, Yoshikami D. Effects of kynurenate on root potentials evoked by synaptic activity and amino acids in the frog spinal cord. Brain Res 1985;265-72, doi: https://doi.org/10.1016/0006-8993(85)90685-7.
Moroni F. Tryptophan metabolism and brain function: focus on kynurenine and other indole metabolites. Eur J Pharmacol 1999;375:87–100, doi: https://doi.org/10.1016/S0014-2999(99)00196-X.
Wu H-Q, Schwarcz R. Seizure activity causes elevation of endogenous extracellular kynurenic acid in the rat brain. Brain Res Bull 1996;39:155–62, doi: https://doi.org/10.1016/0361-9230(95)02087-X.
Majláth Z, Török N, Toldi J, Vécsei L. Memantine and kynurenic acid: current neuropharmacological aspects. Curr Neuropharmacol 2016;14:200–9, doi: https://doi.org/10.2174/1570159X14666151113123221.
Schwarcz R, Pellicciari R. Manipulation of brain kynurenines: glial targets, neuronal effects, and clinical opportunities. J Pharmacol Exp Ther 2002;303:1–10, doi: https://doi.org/10.1124/jpet.102.034439.
Pineda-Farias JB, Pérez-Severiano F, González-Esquivel DF, Barragán-Iglesias P, Bravo-Hernández M, Cervantes-Durán C, et al. The l -kynurenine-probenecid combination reduces neuropathic pain in rats. Eur J Pain 2013;17:1365–73, doi: https://doi.org/10.1002/j.1532-2149.2013.00305.x.
Näsström J, Karlsson U, Post C. Antinociceptive actions of different classes of excitatory amino acid receptor antagonists in mice. Eur J Pharmacol 1992;212:21–9, doi: https://doi.org/10.1016/0014-2999(92)90067-E.
Chapman V, Dickenson AH. Time-related roles of excitatory amino acid receptors during persistent noxiously evoked responses of rat dorsal horn neurones. Brain Res 1995;703:45–50, doi: https://doi.org/10.1016/0006-8993(95)01063-7.
Deng H, Hu H, He M, Hu J, Niu W, Ferrie AM, et al. Discovery of 2-(4-methylfuran-2(5 H)-ylidene)malononitrile and thieno[3,2- b]thiophene-2-carboxylic acid derivatives as G protein-coupled receptor 35 (GPR35) agonists. J Med Chem 2011;54:7385–96, doi: https://doi.org/10.1021/jm200999f.
Jenkins L, Brea J, Smith NJ, Hudson BD, Reilly G, Bryant NJ, et al. Identification of novel species-selective agonists of the G-protein-coupled receptor GPR35 that promote recruitment of β-arrestin-2 and activate G α13. Biochem J 2010;432:451–9, doi: https://doi.org/10.1042/BJ20101287.
Yang Y, Lu JYL, Wu X, Summer S, Whoriskey J, Saris C, et al. G-protein-coupled receptor 35 is a target of the asthma drugs cromolyn disodium and nedocromil sodium. Pharmacology 2010;86:1–5, doi: https://doi.org/10.1159/000314164.
Zhao P, Sharir H, Kapur A, Cowan A, Geller EB, Adler MW, et al. Targeting of the orphan receptor GPR35 by pamoic acid: a potent activator of extracellular signal-regulated kinase and -Arrestin2 with antinociceptive activity. Mol Pharmacol 2010;78:560–8, doi: https://doi.org/10.1124/mol.110.066746.
Yoon MH, Jeong IC, Hong BB, Seong WJ, Sung SC, Kyung YY, et al. Lack of the nitric oxide-cyclic GMP-potassium channel pathway for the antinociceptive effect of intrathecal zaprinast in a rat formalin test. Neurosci Lett 2005;390:114–7, doi: https://doi.org/10.1016/j.neulet.2005.08.006.
Do Lee J, Jun IG, Choi YS, Im SH, Park JY. The antiallodynic effects of intrathecal zaprinast in rats with chronic constriction injury of the sciatic nerve. Korean J Pain 2009;22:16, doi: https://doi.org/10.3344/kjp.2009.22.1.16.
Southern C, Cook JM, Neetoo-Isseljee Z, Taylor DL, Kettleborough CA, Merritt A, et al. Screening β-arrestin recruitment for the identification of natural ligands for orphan G-protein-coupled receptors. J Biomol Screen 2013;18:599–609, doi: https://doi.org/10.1177/1087057113475480.
Szczudlik A, Dobrogowski J, Wordliczek J, Stępień A, Krajnik M, Leppert W, et al. Diagnosis and management of neuropathic pain: review of literature and recommendations of the Polish association for the study of pain and the Polish neurological society — part two. Neurol Neurochir Pol 2014;48:423–35, doi: https://doi.org/10.1016/j.pjnns.2014.11.002.
Szczudlik A, Dobrogowski J, Wordliczek J, Stępień A, Krajnik M, Leppert W, et al. Diagnosis and management of neuropathic pain: review of literature and recommendations of the Polish association for the study of pain and the Polish neurological society — part one. Neurol Neurochir Pol 2014;48:262–71, doi: https://doi.org/10.1016/j.pjnns.2014.07.011.
Pilat D, Piotrowska A, Rojewska E, Jurga A, Slusarczyk J, Makuch W, et al. Blockade of IL-18 signaling diminished neuropathic pain and enhanced the efficacy of morphine and buprenorphine. Mol Cell Neurosci 2016;71:114–24, doi: https://doi.org/10.1016/j.mcn.2015.12.013.
Yoon MH, Choi JI, Kim SJ, Kim CM, Bae HB, Chung ST. Synergistic antinociception between zaprinast and morphine in the spinal cord of rats on the formalin test. Eur J Anaesthesiol 2006;23:65–70, doi: https://doi.org/10.1017/S0265021505001791.
Heo BY, Kim CM, Jeong ST, Kim SJ, Il Choi J, Yoon MH. Antinociceptive effect of the intrathecal phosphodiesterase inhibitor, zaprinast, in a rat formalin test. Korean J Pain 2005;18:99, doi: https://doi.org/10.3344/kjp.2005.18.2.99.
Pilat D, Rojewska E, Jurga AM, Piotrowska A, Makuch W, Przewlocka B, et al. IL-1 receptor antagonist improves morphine and buprenorphine effi- cacy in a rat neuropathic pain model. Eur J Pharmacol 2015;764:240–8, doi: https://doi.org/10.1016/j.ejphar.2015.05.058.
Mika J, Wawrzczak-Bargiela A, Osikowicz M, Makuch W, Przewlocka B. Attenuation of morphine tolerance by minocycline and pentoxifylline in naive and neuropathic mice. Brain Behav Immun 2009;23:75–84, doi: https://doi.org/10.1016/J.BBI.2008.07.005.
Piotrowska A, Kwiatkowski K, Rojewska E, Makuch W, Mika J. Maraviroc reduces neuropathic pain through polarization of microglia and astroglia — evidence from in vivo and in vitro studies. Neuropharmacology 2016;108:207–19, doi: https://doi.org/10.1016/j.neuropharm.2016.04.024.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rojewska, E., Ciapała, K. & Mika, J. Kynurenic acid and zaprinast diminished CXCL17-evoked pain-related behaviour and enhanced morphine analgesia in a mouse neuropathic pain model. Pharmacol. Rep 71, 139–148 (2019). https://doi.org/10.1016/j.pharep.2018.10.002
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.pharep.2018.10.002