Abstract
Background
The goal of present investigation is to check the hypothesis that cardioprotective effect of polyunsaturated fatty acids (PUFAs) is mediated by influence on mRNA expression level of the FATP, IL-1ra and GJP43 through stimulation of PPARγ.
Methods
Animals obtained n-3 PUFAs orally during 4 weeks (0.1 ml/100 g b.w. per day) or during prenatal period. In experiments, isolated perfused hearts were subjected to 20-min regional ischemia and 40 min reperfusion. The hearts of newborn rats (2–3 days old) were used for isolated cardiomyocytes culture preparing. Culture cells underwent 30 min of anoxia followed by 60 min of reoxygenation. Using rtPCR the level of FATP, IL-1ra, GJP43 and BCL2 mRNA in isolated cardiomyocyte and hearts was evaluated.
Results
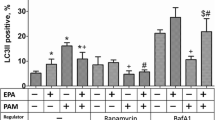
The data obtained indicate that in heart tissues from pups with prenatal n-3 PUFAs application the level of LA and DHA acids were increased in 3.6-fold and 2-fold correspondingly comparing to control. In adult hearts the level of DHA was increased in 1.4-fold, and the level of EPA—in 6.9-fold. We observed the increase in mRNA level of PPARγ-target genes: FATP in 2.25 times, and IL-1ra in 8.4 times. At the same time the level of mRNA of antiapoptotic gene BCL2 was increased in 2.13 times and Connexin-43 gene in 2.2 times after n-3 PUFAs application. These effects were accompanied by significantly improved cardiac function, and increase of living cardiomyocytes number at modeling of ischemia-reperfusion.
Conclusions
n-3 PUFAs application has cardioprotective effects and increases mRNA level of FATP, IL-1ra, GJP43, and BCL2 genes in culture of neonatal cardiomyocytes and in adult hearts.
Similar content being viewed by others
References
Fischer R, Dechend R, Qadri F, Markovic M, Feldt S, Herse F, et al. Dietary n-3 polyunsaturated fatty acids and direct renin inhibition improve electrical remodeling in a model of high human renin hypertension. Hypertension 2008;51:540–6.
Hulbert AJ, Turner N, Storlien LH, Else PL. Dietary fats and membrane function: implications for metabolism and disease. Biol Rev Camb Philos Soc 2005;80:155–69.
Nestel P, Shige H, Pomeroy S, Cehun M, Abbey M, Raederstorff D. The n-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid increase systemic arterial compliance in humans. Am J Clin Nutr 2002;76:326–30.
Calder PC. Omega-3 polyunsaturated fatty acids and inflammatory processes: nutrition or pharmacology. Br J Clin Pharmacol 2013;75:645–62.
Arnold C, Konkel A, Fischer R, Schunck WH. Cytochrome P450-dependent metabolism of omega-6 and omega-3 long-chain polyunsaturated fatty acids. Pharmacol Rep 2010;62:536–47.
Reiffel JA, McDonald A. Antiarrhytmic effects of omega-3 fatty acids. Am J Cardiol 2006;98:50–60.
Richardson ES, Iaizzo PA, Xiao YF. Electrophysiological mechanisms of the antiarrhythmic effects of omega-3 fatty acids. J Cardiovasc Transl Res 2011;4:42–52.
Zhang W, Hu X, Yang W, Gao Y. Omega-3 polyunsaturated fatty acid supplementation confers long-term neuroprotection against neonatal hypoxic-ischemic brain injury through anti-inflammatory actions. Stroke 2010;41:2341–7.
Wang C, Harris WS, Chung M, Lichtenstein AH, Balk EM, Kupelnick B, et al. n-3 Fatty acids from fish or fish-oil supplements, but not alpha-linolenic acid, benefit cardiovascular disease outcomes in primary- and secondary-prevention studies: a systematic review. Am J Clin Nutr 2006;84:5–17.
Pepe S, McLennan PL. Cardiac membrane fatty acid composition modulates myocardial oxygen consumption and postischemic recovery of contractile function. Circulation 2002;105:2303–8.
Khaire AA, Kale AA, Joshi SR. Maternal omega-3 fatty acids and micronutrients modulate fetal lipid metabolism: a review. Prostaglandins Leukot Essent Fatty Acids 2015;98:49–55.
Lee HS, Barraza-Villarreal A, Biessy C, Duarte-Salles T, Sly PD, Ramakrishnan U, et al. Dietary supplementation with polyunsaturated fatty acid during pregnancy modulates DNA methylation at IGF2/H19 imprinted genes and growth of infants. Physiol Genomics 2014;46:851–7.
Hussain A, Nookaew I, Khoomrung S, Andersson L, Larsson I, Hulthen L, et al. A maternal diet of fatty fish reduces body fat of offspring compared with a maternal diet of beef and a post-weaning diet of fish improves insulin sensitivity and lipid profile in adult C57BL/6 male mice. Acta Physiol (Oxf) 2013;209:220–34.
Mennitti LV, Oliveira JL, Morais CA, Estadella D, Oyama LM, do Nascimento CM, et al. Type of fatty acids in maternal diets during pregnancy and/or lactation and metabolic consequences of the offspring. J Nutr Biochem 2015;26:99–111.
Radosinska J, Bacova B, Knezl V, Benova T, Zurmanova J, Soukup T, et al. Dietary omega-3 fatty acids attenuate myocardial arrhythmogenic factors and propensity of the heart to lethal arrhythmias in a rodent model of human essential hypertension. J Hypertens 2013;31:1876–85.
Radosinska J, Bacova B, Bernatova I, Navarova J, Zhukovska A, Shysh A, et al. Myocardial NOS activity and connexin-43 expression in untreated and omega-3 fatty acids-treated spontaneously hypertensive and hereditary hypertriglyceridemic rats. Mol Cell Biochem 2011;347:163–73.
Tribulova N, Seki S, Radosinska J, Kaplan P, Babusikova E, Knezl V, Mochizuki S. Myocardial Ca2+ handling and cell-to-cell coupling, key factors in prevention of sudden cardiac death. Can J Physiol Pharmacol 2009;87:1120–9.
Jump DB. N-3 polyunsaturated fatty acid regulation of hepatic gene transcription. Curr Opin Lipidol 2008;19:242–9.
Nakamura MT, Cheon Y, Li Y, Nara TY. Mechanisms of regulation of gene expression by fatty acids. Lipids 2004;39:1077–83.
Burdge G, Lillycrop K. Fatty acids and epigenetics. Curr Opin Clin Nutr Metab Care 2014;17:156–61.
Grygiel-Gorniak B. Peroxisome proliferator-activated receptors and their ligands: nutritional and clinical implications—a review. Nutr J 2014;13:13–7.
Zhukovska A, Shysh A, Bacova B, Radosinska J, Benova T, Viczenczova C, et al. Heart-protective effect of n-3 PUFA demonstrated in a rat model of diabetic cardiomyopathy. Mol Cell Biochem 2014;389:219–27.
Folch J, Lees M. Sloane Stanley GH: a simple method for the isolation and purification of total lipides from animal tissues. J Biol Chem 1957;226:497–509.
Reinecke H, Zhang M, Bartosek T, Charles EM. Survival, integration, and differentiation of cardiomyocyte grafts: a study in normal and injured rat hearts. Circulation 1999;100:193–202.
Nagibin VS, Dosenko VE, Pivovar SM, Moibenko AA. Fluorine-containing analog of diazoxide prevented of neonatal cardiomyocytes apoptosis during anoxia-reoxygenation. Fiziol Zh 2004;50:15–24.
Fabre A, Caspar-Bauguil S, Gaudart J, Mancini J, Garcia J, Mittaine M, et al. Antioxidant potential is correlated to ω6/ω3 ratio and Brasfield score in cystic fibrosis children. Int J Vitam Nutr Res 2013;83:325–34.
Tuncay E, Seymen AA, Tanriverdi E, Yaras N, Tandogan B, Ulusu NN, Turan B. Gender related differential effects of Omega-3E treatment on diabetes-induced left ventricular dysfunction. Mol Cell Biochem 2007;304:255–63.
Lin H, Mitasikova M, Dlugosova K, Okruhlicova L, Imanaga I, Ogawa K, et al. Thyroid hormones suppress epsilon-PKC signaling, downregulate connexin-43 and increase lethal arrhythmia susceptibility in nondiabetic and diabetic rat hearts. J Physiol Pharmacol 2008;59:271–85.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shysh, A.M., Nagibin, V.S., Kaplinskii, S.P. et al. N-3 long chain polyunsaturated fatty acids increase the expression of PPARγ-target genes and resistance of isolated heart and cultured cardiomyocytes to ischemic injury. Pharmacol. Rep 68, 1133–1139 (2016). https://doi.org/10.1016/j.pharep.2016.06.013
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.pharep.2016.06.013