Abstract
Background and aim
Following a stroke, around a quarter of people will have aphasia, a language disability. Aphasia can have a devastating long-term impact on a person’s psychological wellbeing, yet their language difficulties make it challenging to access mental health care. The Wellbeing In Stroke and Aphasia (WISA) study aims to evaluate the feasibility of setting up an accessible psychological service for people with aphasia.
Methods
The service will be open to people with post-stroke aphasia (n = 30) who live in the UK, are able to access the service either in the university clinic or via telehealth and are not currently receiving therapy from a mental health professional. Participants will be offered up to 8 therapy sessions over 6 months, either one-to-one, with family, or in a group. The intervention is Solution Focused Brief Therapy (SFBT), a brief psychological therapy, delivered by speech and language therapists with training in SFBT under the supervision of a stroke-specialist clinical psychologist. As part of this service, a protocol for addressing mental health care has been developed. Feasibility will be assessed by monitoring referral rates, therapy received, discharge processes, resource capability, costs, challenges, and adverse events. Patient-reported outcome measures collected pre and post intervention will assess mental wellbeing, mood, participation, and satisfaction with therapy and the service. A purposive sample will take part in in-depth interviews following therapy.
Discussion
Given the high levels of psychological distress in this client group, there is a need to investigate innovative ways to provide accessible and acceptable psychological support.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Around 25% of people who have a stroke will have aphasia, a communication disability that affects speaking, understanding, reading and writing [1]. It can have a devastating impact on a person’s identity and rates of depression are high, estimated to be between 43 and 70% [2]. Anxiety is also common with prevalence rates up to 44% [3]. People with aphasia are also at increased risk of having reduced social networks [4] and losing contact with friends [5].
In terms of the priorities of people with aphasia, research suggests they want therapy to address communication and also emotional wellbeing and increased life participation [6]. Yet in a UK survey of 1774 people after a stroke, only 20% felt they were given information, advice, and support in coping with the emotional aspects of the stroke [7]. Further, family members describe overwhelming shock, distress, and anxiety, yet are often not included in the rehabilitation process, nor have their own needs recognised by healthcare professionals [8, 9]. The James Lind Alliance in partnership with the UK Stroke Association recently conducted a Stroke Priority Setting Partnership exercise, consulting over 1400 people affected by stroke as well as healthcare professionals to establish priority areas for research and improvement within the stroke care pathway [10]. For rehabilitation and longer-term care, the number one priority identified was the psychological problems caused by stroke and how to address these.
People with post-stroke aphasia have higher rates of depression than those who do not have aphasia post stroke [11], yet often do not receive an equitable service. Healthcare professionals are concerned that services designed to support psychological wellbeing post stroke are not serving this client group well [12,13,14]. As mental health services rely on language, they are often perceived as inaccessible for people with aphasia, particularly severe aphasia [13]. Mental health professionals report finding it challenging to adapt psychological therapies for this client group [15]. Conversely, surveys of speech and language therapists (SLTs) carried out in the UK [12], Australia [16], South Africa [17], USA [18], New Zealand [19] and Ireland [20] have all found that SLTs, while able to facilitate successful conversations, often feel ill-equipped and lack confidence to address the emotional impact of the stroke; they perceive multiple barriers including a lack of training, supervision, management support, and time.
One way to support psychological recovery post stroke is collaborative working between mental health professionals and SLTs. The stepped or matched model of psychological care is recommended in UK stroke guidelines [21]. In this model, an individual is triaged into one of three levels depending on the severity of symptoms: Level 1, ‘sub-threshold’ or low level mood problems, commonly experienced post stroke; Level 2, mild to moderate symptoms of impaired mood that interfere with rehabilitation; Level 3, severe and persistent mood disorders. A person is then ‘matched’ with appropriate level of care and support. Within this model low level mood problems (Level 1) are within the remit of stroke-specialist healthcare professionals, such as allied health professionals and nurses, with suggested interventions including active listening and provision of information and advice. For mild-moderate mood problems (Levels 1 and 2), it may be appropriate for stroke-specialist healthcare professionals to provide brief psychological interventions provided they have training in this area and receive supervision, for example, receive regular support from a stroke-specialist clinical psychologist. For people with severe and persistent mood disorders (Level 3), it is recommended they receive intervention from a clinical psychologist and/or psychiatrist. SLTs potentially still have a role at Level 3 working with mental health professionals to facilitate successful conversations.
There is some evidence that psychological therapies can be successfully adapted for people with aphasia [22]. For example, there is evidence that behavioural activation therapy is effective in improving mood for people with aphasia [23], preliminary evidence that peer befriending can prevent mood problems [24], and ongoing research exploring diverse approaches including relaxation therapy and problem solving therapy (PRISM study, trial Id: ACTRN12620000209998). In terms of interventions that might be delivered by SLTs, there is evidence that it is feasible for SLTs to be trained and competent to deliver Solution Focused Brief Therapy (SFBT) [25]. SFBT is a brief psychological therapy that explores people’s resources and expertise and helps them to build on these to make positive changes in their everyday life [26]. The strongest evidence for the effectiveness of SFBT is with adults with depression [27]. A meta-analysis of SFBT in medical settings found a significant effect of SFBT (d = 0.34, p < 0.05) for health-related psychosocial outcomes [28]. Within stroke research, a trial reporting on 62 working-age people with mild-moderate first stroke found it effective in improving mood and lowering anxiety [29]. SFBT with people with aphasia was recently explored in the Solution Focused brief therapy In post-stroke Aphasia (SOFIA) feasibility trial. The SOFIA study found that it was feasible to adapt the approach for people with aphasia, including people with severe aphasia, and that they valued being able to explore their experiences, achievements, and hopes for the future [30]. The Wellbeing In Stroke and Aphasia (WISA) study builds on this work, exploring the practicalities and feasibility of setting up an innovative service offering SFBT as an accessible psychological therapy for people with aphasia, involving family members within therapy sessions as appropriate.
1.1 Aims
There are two main aims for the study: (1) Assess the feasibility of setting up and evaluating a service delivering an aphasia-accessible version of SFBT delivered by SLTs; (2) Explore how people with aphasia and their families experience the service, including their perceptions around acceptability and appropriateness of the service in meeting their needs. The overarching aim is that this study prepares the groundwork for establishing a long-term high quality, person-centred, and evidence-informed service that meets the needs of this population.
2 Methods
2.1 Design
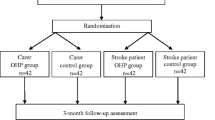
WISA is a pre-post study with nested qualitative research: there is no control arm nor randomisation, and all participants are offered SFBT. Figure 1 illustrates the flow of participants through the study. Participants will complete both baseline (Time 1) and post therapy assessments (Time 2, 6 months after Time 1); a purposive sample of people with aphasia and significant others will also take part in in-depth interviews (Time 2). The study is funded for 24 months from August 2023, and will be open to referrals for 12 months from December 2023. Participants will be in the study for approximately 6 months from baseline assessment.
The Template for Intervention Description and Replication (TIDieR) informed the description of the intervention [31] (see supplementary material). The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 statement [32] guided the writing of the study protocol, although as the study is evaluating the feasibility of setting up a novel service, not all items were applicable. Finally, many items from Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0) [33] were relevant and influenced the protocol.
2.2 Approvals
Ethical approval to conduct the study was granted by City, University of London, Senate Research Ethics Committee (ETH2223-1265). The research is being carried out following the guidelines of the ethics committee. The trial sponsor is City, University of London, and the study is funded by Sir Halley Stewart Trust (Grant 4175).
2.3 Participants: inclusion and exclusion criteria
Eligibility criteria comprise having aphasia, according to self-report and/or based on an SLT’s assessment, aged 18 years old or above, based in the UK, and able to access therapy sessions and complete assessments remotely via telehealth or in person at the university clinic.
Participants are eligible at any stage post stroke, and with any severity of aphasia, so long as they have capacity to consent (as assessed by the research team). They will also not be excluded based on their baseline score on the outcome measure assessing psychological distress, the General Health Questionnaire-12 (GHQ-12) [34]. If they are taking anti-depressants or receiving rehabilitation therapy, this will be recorded but will not be a reason for exclusion.
Each person with aphasia will be asked if they would like to nominate a significant other to take part in the study: someone they see/keep in contact with at least once a week, who is aged 18 years old or above, is based in the UK, and is able to access sessions either via telehealth or in clinic. People with aphasia can decide to take part in the study without nominating a significant other. Conversely, significant others can consent into the study without needing to attend therapy sessions.
People with aphasia will not be eligible for the service if they have not had a stroke or are currently receiving psychological or psychiatric intervention. Other exclusion criteria for both the person with aphasia and significant other are: lack capacity to give informed consent, diagnosis of dementia, severe co-morbidity or frailty (e.g., terminal cancer), non-fluent English speaker prior to the stroke (based on self/family report), severe uncorrected hearing or visual difficulties that could impact on their ability to engage in the therapy and assessments.
2.4 Setting
The intervention, assessment sessions and in-depth interviews will be conducted either via telehealth or in the university clinic. On a case-by-case basis participants may also be offered a one-off home visit to support them to set up online access if they live in London.
2.5 Recruitment and consent processes
Potential participants will learn about the service through a variety of potential routes including local and national stroke and aphasia charities, the university clinic, advertising the service through professional networks such as the British Aphasiology Society and local services, and through social media. The service will accept self-referrals and referrals from health and social care professionals, as well as from a family member or others who know the individual well, for example, volunteer coordinators.
Informed consent will be obtained from all participants. To ensure that each participant fully understands the study, participant information sheets and consent forms have been developed following standard aphasia-friendly principles, such as using short simple sentences, large font and white space, emboldening key words, and supporting key ideas with images. Potential participants will meet with a member of the research team to discuss the study prior to giving informed consent. They will be reassured that participating in the study is entirely voluntary, and that they can withdraw from the study at any time. During this initial session, an assessment will be made of their capacity to give fully informed consent. We will check that they can remember what the study is about and can understand the information. Where their capacity is uncertain, we will also ask three simple yes/no or forced alternative questions, to confirm they have understood key aspects of the study. This approach has been used in other aphasia studies [35, 36]. Where a person with aphasia elects to nominate a significant other, the significant other will receive a separate participant information sheet and consent form, as well as time to discuss the study.
2.6 Sample size and purposive sampling strategy
We will recruit 30 participants with aphasia and up to 30 significant others. We anticipate that this sample is adequate to inform uncertainties prior to setting up a longer-term service, allowing us to gather sufficient information on, for example, service data (e.g. referral routes), and therapy intervention data (e.g. number of sessions, how these are spaced); as well as record costs, challenges, and ideas for refining and improving the service. This size is commensurate with what is recommended for a feasibility trial, where similar feasibility questions are addressed [37].
We will purposively sample 10 participants with aphasia and five significant others to take part in in-depth interviews following the end of therapy. For interviews with participants with aphasia primary sampling criteria will be: severity of aphasia; mode of receiving therapy; baseline mood scores on the GHQ-12. Primary sampling criteria for significant others will be: relationship to person with aphasia; whether attended therapy. Secondary sampling criteria for both groups will be: age; gender; ethnicity. Purposive sampling will help to capture a diversity of views [38].
2.7 Intervention
The therapy is SFBT as trialled in the SOFIA study [25]; see supplementary material for full TIDieR checklist [31]. SFBT is a talk-based psychological intervention which previous research has shown can be adapted with communication supports for those with aphasia [25]. The therapy is highly individualised: it is led by what the participant believes will be a useful outcome, and within any specific session, therapist utterances follow from what the participant says. Nonetheless, it is anticipated that there will be consistency across all sessions in terms of the underlying assumptions. These include: the participant is expert in their own lives; that all participants have resources, talents, competencies and strengths, and the therapist’s role is to enable the participant to notice them; that a ‘solution’ may be brought about by small steps, hence a focus on noticing the everyday details of a person’s life; and that the therapist will hear and validate the participant’s account sufficiently to create a context where change can occur. The therapy will be offered by two aphasia-specialist SLTs who have received training in SFBT, as well as monthly clinical supervision and real time support as needed from a stroke-specialist clinical psychologist. The service will also facilitate regular therapist peer support and debriefing. Both therapists will be given the therapy manual created for the SOFIA study [36], and a practical guidebook to using the approach in healthcare settings including with people who have aphasia [26].
Participants will be able to elect whether to receive the therapy face-to-face in the university clinic or online (or a combination); individually or in a small group setting (where there is sufficient interest from other participants); and whether to include family members or friends within some or all the therapy sessions. The service is free to participants. Each session will be between 45 and 60 min long. Although SFBT is typically brief (3–5 sessions [39]) people with aphasia are likely to need additional sessions, as less material can be covered in each session due to their language disability [40]. The approach trusts that the client is the expert in determining how many sessions will be useful to them [26]. As such, the scheduling and number of sessions will be led by the participant, with an upper limit of eight sessions over 6 months to manage the demands on the service. There is no minimum number of sessions required to show adherence, as there is some evidence that SFBT can be effective as a single session intervention [41]. Where a participant elects to receive therapy in a group format, they will be offered a single one-to-one session, followed by seven group sessions, providing there is sufficient interest from other participants and resource capability.
2.8 Escalation of mental health care
The therapy within the WISA study is being delivered by SLTs not mental health professionals. Within the stepped care model of psychological care, the WISA service is providing a Level 1 or 2 intervention intended for people with mild to moderate mood problems [21]. There will be times when it is more appropriate for participants to receive more specialist or longer-term mental health care, for example, when they are at risk of self-harm, or have not responded to the WISA intervention. A detailed WISA protocol for triaging and escalating mental health care has been developed: it is anticipated this will be further refined during the study. The process of assessing risk, collaboratively developing safety plans, and escalating care may occur in any session within WISA and is considered an ongoing process rather than a one-off event.
Figure 2 illustrates the initial WISA triage process to identify psychologically vulnerable participants based on the screening tool trialled by Simm [42] on a stroke ward. The initial question has been shown to have good sensitivity and specificity as a screening tool in stroke [43]; follow up questions were informed by the work of Ellis, Ashmore [44] to support radiographers in identifying distress in oncology settings. The tool has been adjusted to use simpler language, and the WISA therapists will reframe or use total communication to enable comprehension of key concepts. This screening process will be used when a participant scores ≥ 3/12 on the GHQ-12 indicating psychological distress (either Time 1 or 2 assessment point); or when research staff have concerns (any stage in the study). Where this triage process demonstrates evidence of low mood/ hopelessness, the therapist will continue to the WISA risk assessment protocol which comprises four stages: (1) assess plans for self-harm; (2) assess history of self-harm; (3) have a RISK conversation exploring protective factors; (4) agree on a management plan, including whether to support someone to access Level 3 specialist mental health care. The RISK conversation (Resources; Increments; Sharing; Knowledge) [45] is a framework for exploring protective factors and increasing collaboration between healthcare professionals and participants when creating a safety plan. In all cases where there are concerns around a participant’s mental health, this will be discussed with the clinical psychologist supervisor.
Where a participant has been referred for more specialist mental health input, either directly or via their GP, the WISA therapist may have an extended role of supporting the mental health professional and person with aphasia to communicate successfully, and may continue to see the participant to support them through this process. Once the participant has established a therapeutic relationship with the mental health professional it is anticipated that they will discontinue WISA therapy. Unless there is a clinical reason not to, all participants will be invited to complete Time 2 assessments, even where they have been referred to more specialist provision.
2.9 Outcomes
2.9.1 Feasibility and acceptability
To evaluate the feasibility of setting up the service we will monitor referral routes; information around the therapy (preferences for one-to-one versus group therapy, online versus in person; number of sessions and how these are spaced; discharge details including whether there was onward referral); costs of providing the service; rates of follow up and withdrawal; challenges and adverse events.
The feasibility of delivering the treatment as intended will also be assessed. To monitor and enhance treatment fidelity, therapists will complete a self-rating fidelity checklist after each session. This is a modified version of the checklist developed for the SOFIA study [36]. It lists the core assumptions expected to be present in all therapy sessions, as well as core and optional observable behaviours. It is intended that the reflective process of completing the checklist, along with regular clinical supervision, will enhance the likelihood that the intervention is being delivered as intended.
To evaluate acceptability, all participants and their nominated significant others will be supported to complete an aphasia-accessible version of the NHS Friends and Family Test (NHS FFT), a tool for evaluating patient experience and informing service improvement [46]. We will also assess participants’ satisfaction with therapy and therapeutic relationship using the Session Rating Scale (SRS) [47]. In addition, the in-depth interviews with people with aphasia (n = 10) and significant others (n = 5) will explore: their experiences of the therapy and the service including acceptability, and the extent to which the service is perceived as relevant and a good fit for their needs; the impact of receiving the service, if any; what psychological support they value post stroke; and suggestions for improving the service.
Feasibility and acceptability data will provide insight into how the service can best be configured should it be continued in the future. Progression criteria based on feasibility and acceptability outcomes are outlined below.
2.9.2 Profiling measure
In order to profile participants’ aphasia, the Frenchay Aphasia Screening Test (FAST) [48] will be conducted (baseline only).
2.9.3 Clinical outcomes
The rationale for collecting clinical outcome data is to assess the acceptability and appropriateness of the outcome measures (based on missing data and interview data) for evaluating the service, rather than to test a hypothesis of effectiveness, as well as to see how participant scores change over time. The following outcome measures will be collected: Warwick Edinburgh Mental Well-being Scale (WEMWBS) 14 item version, measuring mental well-being [49]; General Health Questionnaire-12 (GHQ-12) measuring psychological distress [34]; Communicative Participation Item Bank (CPIB) measuring communicative participation [50]. The chosen measures have either been developed specifically for adults with an acquired communication disability (CPIB) or have been previously used with people with aphasia with good evidence of accessibility and acceptability (GHQ-12, WEMWBS). All chosen measures have sound psychometric properties.
In addition, we will measure the extent to which participants achieve individual goals: participants will be supported to identify their initial goals, or ‘best hopes’, from therapy near the start of their therapy. Participants will rate themselves on a scale 0–10, where 10 indicates best hopes fully realised, 0 indicates the opposite, following the methodology used in a study of stammering and SFBT [51]. In the final therapy session, we will repeat the same scale to monitor progress on personal goals. Finally, a single-item anchor question assessing participant perspective on clinical relevance will be asked at Time 2 assessment [52].
2.9.4 Procedure for collecting outcome measures and conducting interviews
Outcome measures will be collected in face-to-face interviews, either in person or online, by research staff who are aphasia-specialist SLTs with experience of research processes. The presentation of measures will be modified to make them aphasia-accessible: participants will be able to read items as well as hear them; few items will be presented per page and key words will be emboldened; a practice item will be inserted at the start of questionnaires to familiarise participants with response options. The content, however, will not be changed to avoid affecting the measures’ psychometric properties.
At Time 2, research staff will be blinded to baseline assessment scores; however, as there is no control group they will be aware that the participant has been offered therapy. Time 2 assessments and in-depth interviews will not be completed by the treating therapist. However, goal attainment rating scales will be measured at the start and end of the therapy process.
2.10 Analyses
2.10.1 Quantitative analysis
We will provide a diagram displaying the flow of participants through the study. In line with CONSORT Item 13a [53], we will detail the number of participants who were referred and assessed for eligibility; recruited; received intervention (group or one-to-one); included in analysis. Additionally, as specified in CONSORT Item 13b [53], we will include the number of people who were excluded, withdrew, or were lost to follow up, with reasons why where possible.
For all descriptive statistics outlined below, we will calculate appropriate 95% confidence intervals. In terms of feasibility data we will analyse: (1) proportion who are eligible from those referred/expressed an initial interest; (2) proportion who consent of those eligible; (3) rate of consent per month; (4) how participants hear about the project/referral sources; (5) how quickly potential participants are seen for an initial information giving session following referral/initial expression of interest; (6) how quickly participants commence therapy following initial information giving session; (7) proportion of participants who withdraw or are lost to follow up (reasons why recorded where known); (8) proportion who are seen for post-therapy assessment at 6 months ± 2 weeks. We will also analyse: (9) proportion who elect to receive one-to-one therapy versus group therapy; (10) proportion who elect to receive therapy at the clinic, online or a combination; (11) proportion who invite a significant other into the therapy; (12) total number of therapy sessions each participant receives; (13) duration of therapy received (i.e. over how many months); (14) number of participants referred for more specialist mental health support; (15) frequency and nature of contact with mental health professionals; (16) number referred to services other than mental health. We will also collect and report intervention costs such as SLT time, clinical supervision, and SFBT training; and resources and capabilities of the service such as the number of sessions available per week.
In terms of outcome measures (GHQ-12, WEMWBS, CPIB), and individual goals, we will provide descriptive statistics for the entire population and by mode of delivery with mean and 95% confidence intervals plotted over time as appropriate. Descriptive statistics will also be used to analyse participants’ satisfaction with the service (NHS FFT) and therapy (SRS), and the single-item anchor question on clinical relevance.
Where participants are referred for more specialist mental health provision and commence alternative psychological/psychiatric treatment during their participation in WISA, we will still collect outcome data at Time 2 unless this is contra-indicated clinically. Initially, the full dataset will be summarised. Their data will then be excluded from the overall dataset and described separately.
In terms of treatment fidelity, we will report on: proportion of missing data on self-rating reflective checklists; and the proportion of sessions rated that delivered the core components of the approach. We will also provide descriptive statistics for the therapy components (both core and optional), detailed in the reflective checklists. This will enable us to compare the content of the intervention between WISA therapists, over time, and comparing people with severe versus mild-moderate aphasia.
Adverse events, adverse reactions, serious adverse events, serious adverse reactions and suspected unexpected serious adverse reactions will be summarised as counts of events and counts of people who have had events. We will also report the number of participants who have complete data at both baseline (Time 1) and Time 2.
2.10.2 Qualitative analysis
All interviews will be transcribed verbatim. We will use Framework Analysis [54] to analyse data collected during in-depth interviews, and also the qualitative responses to the NHS FFT [46]. Qualitative written reflections on the fidelity checklists, and the log of challenges by therapists will be analysed using qualitative content analysis [55]. Qualitative data will be reported according to the Standards for Reporting Qualitative Research Guidelines (SRQR) [56].
2.11 Progression criteria
The decision whether and how to continue the service will be considered by the study advisory groups, involving key stakeholders. It is anticipated these discussions will continue throughout the study, and that consideration will be given to ways to provide a continuous service as the current study ends. Discussions will take into account both qualitative and quantitative data, including four pre-specified criteria:
-
1.
Proportion of participants (with aphasia; significant others) who rate the service as ‘good’ or ‘very good’ on the NHS FFT: < 50% stop; 50–80% amend; > 80% go.
-
2.
Proportion of participants with aphasia who score 30/40 or above on the SRS (indicating satisfaction with therapy and therapeutic alliance): < 50% stop; 50–80% amend; > 80% go.
-
3.
Proportion of participants followed up at Time 2 assessment point: < 50% stop; 50–70% amend; > 70% go.
-
4.
Average number of participants recruited into the service per month: < 1: stop; 1: amend; ≥ 2 go.
2.12 Data management and monitoring
The main study database will be hosted at City, University of London (City), on City University One Drive, a secure network regularly backed up. Source data will be entered by authorised staff only with full audit trail. Database access will be restricted through passwords. Participants will be identified by their unique code (Participant Identification Number, PIN). Recordings of qualitative interviews will also be stored on the secure drive. During the transcription process, any information which could lead to the identification of a participant will be de-identified using pseudonyms, replacement terms and vaguer descriptors. We will seek consent to notify participants’ GPs that they are taking part in the study, however, we will not share their outcome data nor confidential information unless there are concerns around safety, or the participant has requested we do so.
There will be regular checks to monitor for completeness and accuracy of data collected and entered onto databases (including range and logic checks) as well as adherence to procedure (e.g. timeliness of visits). Variance from procedures and missing or incomplete data will be reported to co-investigators and the project steering group. Any significant amendments to the protocol will be communicated to all relevant authorities and advisory groups. There are no planned interim analyses.
2.13 Governance and advisory groups
The core research team of co-investigators will meet monthly, providing oversight, guidance and approving key decisions. They will consider progress of the study and participant and research staff welfare. There is also a project steering group (n = 3), consisting of academics and clinicians, including two SLTs and a clinical psychologist. They will meet three times during the study and will provide advice and support, for example, advising on any ethical issues which may arise. Adverse Events will be reported to both the co-investigators and the project steering group. Finally, there is a lived experience advisory group, consisting of three people living with stroke and aphasia, and one family member. They will meet four times during the study and advise on facilitating a positive participant experience, recruitment, making the service accessible, pathways for escalating care, involving family members, interview topic guides, interpreting results, and dissemination. All advisory groups will consider whether and how to continue the service beyond the end of the study.
2.14 Adverse events, ancillary and post-study care
As the service is offering a non-physical, non-invasive intervention, adverse events are considered unlikely. Research staff will document and report all adverse events. They will follow protocols for escalating care, according to whether the need is physical, social or psychological. In terms of ancillary care, all research staff are experienced SLTs trained in how to listen holistically to participants. In all sessions, whether initial information giving, assessment, therapy or interviews, the aim will be to enable a positive participant experience where they feel valued and respected. Towards the end of the therapy, the therapist will explore the participant’s hopes for after the therapy, which may include exploring ongoing supportive options. In terms of post-study support, all participants will be offered a final session with their therapist following the Time 2 assessment. This will be an opportunity to feed back on their progress, successes, address any persisting concerns around mood, and discuss onward plans. An aphasia-accessible final report will be shared with the participant.
2.15 Dissemination
We will share the learning and findings from our study through social media, as well as the City Access—Aphasia Resources website (https://cityaccess.org) which is accessed by clinicians from across the world. We will also share results through writing academic articles, presenting at conferences, and hosting a dissemination event, where we will invite participants, therapists, charitable sector organisations and policy makers. Changes in clinical practice, attitudes or service provision will be assessed following the dissemination event through a Qualtrics survey.
3 Discussion
The WISA study is evaluating the feasibility of setting up an innovative service providing person-centred and accessible psychological therapy for people with aphasia. It will explore how people experience the service, and report on feasibility and clinical outcomes. These findings will be used to shape the future of the service beyond the end of the study.
People with aphasia can struggle to access mental health support due to their language difficulties particularly in the longer-term post stroke, and particularly those with more severe aphasia [13, 14]. Our previous research demonstrated that it is possible to adapt SFBT so that it works well for this client group, including people with severe aphasia [25]. The Aphasia Advisory Group for the SOFIA study advised there was an urgent need to develop a service to support the emotional wellbeing of people with aphasia, and that it should be responsive, accessible, and open to people at any stage post stroke. This informed the eligibility criteria, therapy formats offered, and inclusion of family members where this is the preference of the person with aphasia within the WISA study. The current service is also exploring the feasibility of offering SFBT both one-to-one and in a group setting. There is evidence that people with aphasia derive benefit from group therapy, as it fosters social connections and friendship [57], personal growth and self-acceptance [58]; and that SFBT can work well delivered in a group format with other client groups [59, 60]. The decision to offer the option of receiving therapy online was intended to increase accessibility for those unable to travel to the clinic.
In line with the stepped model of care, safeguards have been put in place for this to be a safe service and within the scope of practice of SLTs [21], with a protocol for escalating mental health care in a way that supports the wellbeing of both participants and therapists. Still, there are limitations to the service: it is unable to provide domiciliary care, nor offer Level 3 care for those with more severe distress, nor offer more than 8 therapy sessions. It is also only able to offer one psychological therapy approach, which may not suit all participants. Further, due to resource constraints, we are unable to assess maintenance of treatment perceptions and effects, for example, 3 months post intervention, which could have added additional information and insight.
In conclusion, the WISA study builds directly on previous research which found that people with aphasia value therapeutic interactions where they can share feelings and achievements, explore hopes, and ‘feel noticed and validated as people’ [30]. The WISA service aims to offer a safe, calm, and accepting space where people with aphasia are welcomed, feel heard and listened to, and where they can find hope for a way to live with their aphasia.
Data availability
There is no data associated with this protocol manuscript. We intend to share the anonymised dataset where explicit consent has been given by participants on completion of the study.
References
Flowers HL, et al. Poststroke aphasia frequency, recovery, and outcomes: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2016;97(12):2188–201. https://doi.org/10.1016/j.apmr.2016.03.006.
Kristo I, Mowll J. Voicing the perspectives of stroke survivors with aphasia: a rapid evidence review of post-stroke mental health, screening practices and lived experiences. Health Soc Care Comm. 2022;30(4):e898–908. https://doi.org/10.1111/hsc.13694.
Morris R, et al. Prevalence of anxiety in people with aphasia after stroke. Aphasiology. 2017;31(12):1410–5. https://doi.org/10.1080/02687038.2017.1304633.
Northcott S, Marshall J, Hilari K. What factors predict who will have a strong social network following a stroke? J Speech, Lang Hear Res. 2016;59(4):772–83. https://doi.org/10.1044/2016_JSLHR-L-15-0201.
Northcott S, Hilari K. Why do people lose their friends after a stroke? Int J Lang Commun Disord. 2011;46(5):524–34. https://doi.org/10.1111/j.1460-6984.2011.00079.x.
Wallace SJ, et al. Core outcomes in aphasia treatment research: an e-Delphi consensus study of international aphasia researchers. Am J Speech Lang Pathol. 2016;25(4S):S729–42. https://doi.org/10.1044/2016_AJSLP-15-0150.
Stroke Association, Feeling overwhelmed. Accessed in https://www.stroke.org.uk/resources/feeling-overwhelmed. 2015.
Howe T, et al. “You needed to rehab … families as well”: family members’ own goals for aphasia rehabilitation. Int J Lang Commun Disord. 2012;47(5):511–21. https://doi.org/10.1111/j.1460-6984.2012.00159.x.
Luker J, et al. Carers’ experiences, needs, and preferences during inpatient stroke rehabilitation: a systematic review of qualitative studies. Arch Phys Med Rehabil. 2017;98(9):1852–62. https://doi.org/10.1016/j.apmr.2017.02.024.
Stroke Association, Shaping stroke research to rebuild lives: the Stroke Priority Setting Partnership results for investment. 2021.
Zanella C, et al. Incidence of post-stroke depression symptoms and potential risk factors in adults with aphasia in a comprehensive stroke center. Top Stroke Rehabil. 2023;30(5):448–58. https://doi.org/10.1080/10749357.2022.2070363.
Northcott S, et al. How do speech and language therapists address the psychosocial well-being of people with aphasia? Results of a UK on-line survey. Int J Lang Commun Disord. 2017;52(3):356–73. https://doi.org/10.1111/1460-6984.12278.
Northcott S, et al. Supporting people with aphasia to ‘settle into a new way to be’: speech and language therapists’ views on providing psychosocial support. Int J Lang Commun Disord. 2018;53(1):16–29. https://doi.org/10.1111/1460-6984.12323.
Baker C, et al. Stroke health professionals’ management of depression after post-stroke aphasia: a qualitative study. Disabil Rehabil. 2021;43(2):217–28. https://doi.org/10.1080/09638288.2017.1315181.
Strong KA, Randolph J. How do you do talk therapy with someone who can’t talk? Perspectives from mental health providers on delivering services to individuals with aphasia. Am J Speech-Lang Pathol. 2021;30(6):2681–92. https://doi.org/10.1044/2021_AJSLP-21-00040.
Sekhon JK, Douglas J, Rose ML. Current Australian speech-language pathology practice in addressing psychological well-being in people with aphasia after stroke. Int J Speech Lang Pathol. 2015;17(3):252–62. https://doi.org/10.3109/17549507.2015.1024170.
Nash J, et al. Psychosocial care of people with aphasia: practices of speech-language pathologists in South Africa. Int J Speech Lang Pathol. 2022;24(3):330–40. https://doi.org/10.1080/17549507.2021.1987521.
Hayashi H, et al. Perspectives of US speech-language pathologists on supporting the psychosocial health of individuals with aphasia. J Commun Disord. 2023;105:106365. https://doi.org/10.1016/j.jcomdis.2023.106365.
Gibson R, Purdy SC. How do speech language therapists in New Zealand perceive the psychological impact of communication difficulties? Speech, Lang Hear. 2014;17(2):116–22. https://doi.org/10.1179/2050572813Y.0000000026.
Manning MX, Cleary C, McCaughey C. How do speech and language therapists enact aphasia psychosocial support in Ireland? A cross-sectional online survey informed by normalization process theory. Int J Lang Commun Disord. 2023. https://doi.org/10.1111/1460-6984.12959.
NHS Improvement. Psychological care after stroke: improving stroke services for people with cognitive and mood disorders. Accessed in. http://www.nice.org.uk/2011.
Baker C, et al. A systematic review of rehabilitation interventions to prevent and treat depression in post-stroke aphasia. Disabil Rehabil. 2018. https://doi.org/10.1080/09638288.2017.1315181.
Thomas SA, et al. Communication and low mood (CALM): a randomized controlled trial of behavioural therapy for stroke patients with aphasia. Clin Rehabil. 2013;27(5):398–408. https://doi.org/10.1177/0269215512462227.
Hilari K, et al. Supporting wellbeing through peer-befriending (SUPERB) for people with aphasia: a feasibility randomised controlled trial. Clin Rehabil. 2021;35(8):1151–63. https://doi.org/10.1177/0269215521995671.
Northcott S, et al. Solution focused brief therapy in post-stroke aphasia (SOFIA): feasibility and acceptability results of a feasibility randomised wait-list controlled trial. BMJ Open. 2021;11(8):e050308. https://doi.org/10.1136/bmjopen-2021-050308.
Burns K, Northcott S. Working with solution focused brief therapy in healthcare settings: a practical guide. London: Routledge; 2022.
Gingerich WJ, Peterson LT. Effectiveness of solution-focused brief therapy: a systematic qualitative review of controlled outcome studies. Res Soc Work Pract. 2013;23(3):266–83. https://doi.org/10.1177/1049731512470859.
Zhang A, et al. The effectiveness of strength-based, solution-focused brief therapy in medical settings: a systematic review and meta-analysis of randomized controlled trials. J Behav Med. 2018;41(2):139–51. https://doi.org/10.1007/s10865-017-9888-1.
Wichowicz HM, et al. Application of solution-focused brief therapy (SFBT) in individuals after stroke. Brain Inj. 2017;31(11):1507–12. https://doi.org/10.1080/02699052.2017.1341997.
Northcott S, et al. “Now i am myself”: exploring how people with poststroke aphasia experienced solution-focused brief therapy within the SOFIA trial. Qual Health Res. 2021;31(11):2041–55. https://doi.org/10.1177/10497323211020290.
Hoffmann TC, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. https://doi.org/10.1136/bmj.g1687.
Chan AW, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–7. https://doi.org/10.7326/0003-4819-158-3-201302050-00583.
Ogrinc G, et al. SQUIRE 2.0 (S tandards for QU ality I mprovement R eporting E xcellence): revised publication guidelines from a detailed consensus process. J Contin Educ Nurs. 2015;46(11):501–7.
Goldberg D. The detection of psychiatric illness by questionnaire. London: Oxford University Press; 1972.
Hilari K, et al. Adjustment with aphasia after stroke: study protocol for a pilot feasibility randomised controlled trial for SUpporting wellbeing through PEeR befriending (SUPERB). Pilot Feasibility Stud. 2019;5(1):1–16. https://doi.org/10.1186/s40814-019-0397-6.
Northcott S, et al. SOlution focused brief therapy in post-stroke aphasia (SOFIA trial): protocol for a feasibility randomised controlled trial. AMRC Open Res. 2019. https://doi.org/10.1268/amrcopenres.12873.2.
Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract. 2004;10(2):307–12. https://doi.org/10.1111/j.2002.384.doc.x.
Ritchie J, Lewis J, Elam G. Designing and selecting samples. In: Ritchie J, Lewis J, editors. Qualitative research practice: a guide for social science students and researchers. London: Sage; 2003.
Ratner H, George E, Iveson C. Solution focused brief therapy: 100 key points and techniques. In: Dryden W, editor. 100 key points series. Hove: Routledge; 2012.
Northcott S, et al. “Living with aphasia the best way I can”: a feasibility study exploring solution-focused brief therapy for people with aphasia. Folia Phoniatr Logop. 2015;67(3):156–67. https://doi.org/10.1159/000439217.
Iveson C, George E, Ratner H. Love is all around: a single session solution-focused therapy. In: Hoyt M, Talmon M, editors. Capturing the moment: single session therapy and walk-in services. London: Crown House; 2014. p. 325–48.
Simm R. The role of occupational therapists in supporting psychological wellbeing after stroke using a solution-focused psychological approach to mood assessment. Br J Occup Ther. 2013;76(11):503–6. https://doi.org/10.4276/030802213X13833255804630.
Watkins CL, et al. Evaluation of a single-item screening tool for depression after stroke: a cohort study. Clin Rehabil. 2007;21(9):846–52. https://doi.org/10.1177/0269215507079846.
Ellis T, Ashmore L, Bray D. Multidisciplinary radiographer-led review clinics–an example of implementation. J Radiother Pract. 2006;5(2):87–95. https://doi.org/10.1017/S1460396906000124.
Guyers M. Changing conversations in suicide risk management: a new model called RISK. Clin Psychol Forum. 2020;334:51.
NHS England, NHS England and NHS Improvement guidance: using the Friends and Family Test to improve patient experience. 2019.
Duncan BL, et al. The session rating scale: preliminary psychometric properties of a “working” alliance measure. J Brief Ther. 2003;3(1):3–12.
Enderby P, Wood V, Wade D. Frenchay aphasia screening test. Windsor: NFEW-Nelson; 1987.
Tennant R, et al. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. 2007;5:63. https://doi.org/10.1186/1477-7525-5-63.
Baylor C, et al. The communicative participation item bank (CPIB): item bank calibration and development of a disorder-generic short form. J Speech Lang Hear Res. 2013;56(4):1190–208. https://doi.org/10.1044/1092-4388(2012/12-0140.
Rodgers NH, et al. Using solution-focused principles with older children who stutter and their parents to elicit perspectives of therapeutic change. Perspect ASHA Special Interest Groups. 2020;5(6):1427–40.
Breitenstein C, et al. Operationalising treatment success in aphasia rehabilitation. Aphasiology. 2022. https://doi.org/10.1080/02687038.2021.2016594.
Eldridge SM, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016;2:64. https://doi.org/10.1186/s40814-016-0105-8.
Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess R, editors. Analysing qualitative data. London: Routledge; 1994.
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88. https://doi.org/10.1177/1049732305276687.
O’Brien BC, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51. https://doi.org/10.1097/ACM.0000000000000388.
Lanyon LE, Rose ML, Worrall L. The efficacy of outpatient and community-based aphasia group interventions: a systematic review. Int J Speech-Lang Pathol. 2013;15(4):359–74. https://doi.org/10.3109/17549507.2012.752865.
Attard MC, et al. Consumer perspectives on community aphasia groups: a narrative literature review in the context of psychological well-being. Aphasiology. 2015;29(8):983–1019. https://doi.org/10.1080/02687038.2015.1016888.
Dargan PJ, Simm R, Murray C. New approaches towards chronic pain: patient experiences of a solution-focused pain management programme. Br J Pain. 2014;8(1):34–42.
Schmit EL, Schmit MK, Lenz AS. Meta-analysis of solution-focused brief therapy for treating symptoms of internalizing disorders. Couns Outcome Res Eval. 2016;7(1):21–39. https://doi.org/10.1177/2150137815623836.
Acknowledgements
The authors would like to thank all the participants with aphasia and their families. They would also like to thank the research therapist, Nikki Atkins, and research assistant, Jean Rutter. We are also grateful to the Lived Experience Advisory Group and the Project Steering Group for their ongoing advice and support. Finally, we would like to thank City, University of London for use of the Roberta Williams Speech and Language Therapy centre, and to Sir Halley Stewart Trust for funding this work.
Author information
Authors and Affiliations
Contributions
SN led the study and drafted the manuscript; JI and SN co-authored the mental health protocol which forms part of the current manuscript; KJ has led on the statistical analysis; ST, KH and CB have all contributed significantly to the design and conduct of the study. All authors have critically reviewed the journal article and approved the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Northcott, S., Baker, C., Thomas, S. et al. Wellbeing in stroke and aphasia (WISA): protocol for a feasibility study setting up an accessible service offering psychological therapy to people with post-stroke aphasia. Discov Psychol 4, 107 (2024). https://doi.org/10.1007/s44202-024-00195-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44202-024-00195-6