Abstract
Purpose
The AAMC has expanded its focus on healthcare disparities training during undergraduate medical education (UME). Currently, no standardized published curriculum dedicated to surgical disparity training exists. Therefore, our purpose was to develop, implement, and evaluate a novel Surgical Disparities Curriculum to equip medical students to recognize peri-operative disparities.
Methods
The Surgical Disparities Curriculum was developed based on the Surgical Disparity Framework created by the NIH-American College of Surgeons Summit on Health Disparity using Kern’s Model of Curriculum Development. The curriculum includes four components which are illustrated in Fig. 1: (1) a pre-session review of a journal article and multimedia adjunct highlighting one category within the framework, (2) a didactic session highlighting key elements of the state of surgical disparities and teaching the NIH-ACS framework, (3) a review of a clinical vignette and articles highlighting a framework factor, and (4) a discussion session applying all elements of the framework to disparities identified in pre-session materials, clinical vignette, and personal clinical experiences. The curriculum was administered at a single large academic institution to 223 third-year medical students. Curriculum evaluation was performed using Kirkpatrick’s Model of Training Evaluation and included post-participation surveys to evaluate participant reaction to the curriculum as well as pre- and post-course assessments to evaluate learning. Results were pooled and a Fisher’s exact test or independent samples t test was used for relevant analysis with p < 0.05 considered significant. Thematic analysis, using common word groupings, was also performed on post-survey comments.

Outline of novel Surgical Disparities Curriculum for Medical Students. Pre-session preparation includes a survey and a guided reading with a relevant journal article and a multimedia adjunct. Next is a didactic session that introduces a Surgical Disparities Framework established by the ACS in 2016 and gives students a background in the language of discussing disparities. Next is a clinical vignette that highlights a framework factor and several disparities of interest. This is followed by a guided discussion on the pre-session materials, the didactic component, and the clinical vignette within the framework accompanied by a discussion on how to apply the framework and identify and prevent disparities. This was followed by a post-session survey
Results
Participants stated they had prior dedicated training in recognizing health disparities integrated throughout the UME curriculum during pre-clinical (83%) and clinical (89%) experiences. Only 31% of students agreed surgical disparities had been discussed during their rotation prior to curriculum implementation. After curriculum participation, 90% of students endorsed an improved understanding of surgical disparities in healthcare and there was a 20% improvement in self-reported identification of peri-operative disparities from 68 to 88% (20% [CI 12–28%], p < 0.0001). Participation in the curriculum also resulted in knowledge acquisition with students scoring better (78% v 59% at baseline; p < 0.0001) on post-participation assessment.
Conclusion
The Surgical Disparities Curriculum provides a novel solution for bridging the gap in training medical students to recognize disparities in the care of surgical patients. Future work will be done to assess long-term retention and behavioral changes because of our intervention. In addition, we will be working on the translatability of our curriculum to other institutions with the goal of training clerkship students across the country to better recognize surgical disparities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical disparities describe differences in surgical disease burden, access to appropriate surgical treatment, and decisions regarding surgical interventions—all of which disproportionately impact socially disadvantaged populations, including those of a lower education and socioeconomic status [1,2,3,4]—which leads to disparate outcomes. Social determinants of health and healthcare disparities play a critical role in shaping these patient outcomes—with those patients of disadvantaged and marginalized communities [5] at an increased risk of chronic disease, mortality, morbidity, and worse post-operative outcomes [4, 6,7,8,9]. In fact, recent data show that up to eighty to ninety percent of healthcare outcomes can be attributed to social determinants of health—with medical care accounting for the paltry remainder [10]. Therefore, it is essential to address these healthcare disparities to improve healthcare outcomes in surgical patients. To do so, it is vital to equip our future physicians with the tools they need to identify and address peri-operative disparities. We have, therefore, created a novel Surgical Disparities Curriculum for medical student education to address this gap.
There continues to be a paucity in the recognition of disparities in surgical care, as evidenced by a 2016 American College of Surgeons survey which found that less than one in four surgeons make an effort to investigate disparities in their own surgical practice [6]. The majority reported that racial and ethnic disparities in care were primarily due to patient-level factors alone [6], further illustrating the lack of understanding of the often complex and multifactorial determinants of health that contribute to disparities [3]. Although the intersection of healthcare disparities and surgery is a relatively nascent topic, there has been a tremendous increase in research demonstrating the correlation between social determinants of health and surgical outcomes in the last decade [1, 4, 8, 11,12,13,14,15].
Despite this growing body of literature, surgical disparities continue to persist—highlighting the need to create solutions that identify and address surgical disparities in impactful ways that benefit patients and mitigate their increased risk for disability and death.
The first step to addressing disparities is understanding them. The American College of Surgeons developed a comprehensive framework in 2016 to better conceptualize disparities in surgical care by categorizing disparities into five factors including: patient factors, provider factors, system and access issues, clinical care and quality, and post-operative care and rehab [3]. By applying a comprehensive framework to identify and address surgical disparities, we can work toward more equitable and effective care for all patients [16].
Medical education plays a key role in training healthcare professionals to identify and address social determinants of health [17, 18]. Though the AAMC recommends that education on social determinants of health are included in medical school curricula [19], there are few known dedicated curricula regarding disparities in surgical care, and much of the education on healthcare disparities is limited to the pre-clinical years [20]. However, it is not enough to limit education on health disparities and inequities to discrete courses, but must be integrated into every facet of education from the pre-clinical years to bedside [19, 20] to have a discernable impact. Dedicated education is especially limited in the surgical clerkship of undergraduate medical education and, in addition, many medical students report being influenced by provider biases as a hidden impact of surgical education during the clerkship years [21], which highlights a significant need in combating disparities in the surgical sphere.
Currently, only a few examples of early piloted curricula exist, which are further detailed below. In an example of service learning, Janeway et al. describes a study where medical students spent time educating surgical inpatients about their surgical conditions, while simultaneously practicing how to screen for social determinants of health. Throughout their medical school career, students reported an increased confidence in both interacting with patients and assessing for social determinants of health [22]. Goodsell et al. describes an equity-focused module regarding disparities in prostate cancer which included preparatory material, a patient case, and an interactive discussion session. Post-tests after the intervention indicated that students reported an improvement in their knowledge and framing of surgical disparities [23]. Rhodin et al. examines a 10-month intervention where medical students followed the management of surgical oncology patients and spent time understanding the challenges faced by this population [24]. And finally, a group at the University of Pennsylvania was one of the first of their kind that instituted a longitudinal curriculum that spans a wide variety of surgical equity related topics to a voluntary group of medical students and residents and demonstrated an improved ability to advocate for surgical equity [25]. However, the group was only able to administer the curriculum on a voluntary basis and to a small cohort of twenty-four. Although these studies are good steps toward implementing disparity education in surgery, there remains a lack of a general Surgical Disparities Curriculum that has been implemented institution-wide. In addition, no curricula or studies have been evaluated on a long-term basis on improvement in graduate medical training or patient outcomes.
In this paper, we demonstrate how we have developed, implemented, and evaluated a novel general surgical disparities module that was integrated into the third-year clerkship. Our goal was to train medical students to be more comfortable in identifying and addressing the social determinants of health that contribute to the peri-operative disparities in surgical patients.
Methods
-
I.
Curriculum design and development: Our Surgical Disparities Curriculum was developed based on the Surgical Disparity Framework created at the American College of Surgeons in 2016 which illustrates five factors for framing and discussing surgical disparities. These five factors are: patient factors, provider factors, system and access issues, clinical care and quality, and post-operative care and rehab [3]. We used Kern’s Model of Curriculum Development [26], knowledge from resident and staff experiences, as well as influence from content area experts to design our curriculum.
-
A.
Problem identification: [26]: Our surgery resident DEI (diversity, equity, and inclusion) committee determined a need for the curriculum from informal medical student requests and faculty feedback. Although students received education in their pre-clinical years at this institution, no formal education in surgical disparities existed. In addition, no formal discussion about healthcare disparities was present in the surgical clerkship.
-
B.
Targeted needs assessment [26]: A formal pre-session survey was given to highlight the targeted need for helping our medical students to identify disparities in the peri-operative care of their patients. Students were asked if they felt comfortable identifying disparities in the care of their peri-operative patients and furthermore if disparities had been discussed in their clerkship thus far.
-
C.
Goals and objectives [26]: The DEI resident committee met and clarified three overarching short- and long-term goals: (1) to train future physician and surgeons to recognize how surgical disparities impact the patients they serve, (2) to reinvigorate humanism in the care of surgical patients through a better understanding of surgical disparities, and (3) affect long-term patient outcomes through improved recognition and mitigation of surgical inequities.
-
D.
Educational strategies [26]: Resident members of the DEI committee met with faculty leaders in medical student education to formulate the design of the curriculum. Our institution has a collection of recorded cases taken from a series of disparity-related morbidity and mortality conferences begun by our institution as a first step to recognizing and mitigating disparities in surgery [27]. The recorded cases and clinical scenarios were divided into the different framework factors described by the ACS Surgical Disparity Framework [3]. To start with, three modules were created to pilot the curriculum. This was based on the availability of resident and staff expertise and materials to create the module. Currently the creation of more modules that highlight each of the framework categories is underway. The modules created, thus, far are better visualized in Table 1. The curriculum included in these modules include four key components: (1) a pre-session review of a journal article and multimedia adjunct highlighting one category within the framework, (2) a standardized didactic session reviewing the NIH-ACS approved framework for surgical disparities [3], (3) a review of a clinical vignette highlighting a surgical disparity, and (4) a discussion session applying the framework to disparities identified in pre-session materials, clinical vignette, and personal clinical experiences. The details of the curriculum design are further elucidated below:
-
i.
Pre-session survey: Prior to the session, a survey was sent via email asking students to describe their current experiences with education on healthcare disparities, their experiences in identifying healthcare disparities in their surgical patients, and knowledge questions about surgical disparities and the Surgical Disparities Framework. Students were then allowed to choose one of the three specific modules detailed above in Table 1. The module with the most votes was the one given during the session. Students were then given the associated academic journal article and multimedia adjunct such as a video, a news source, or book chapter related to the scenario to read prior to attending the session. The pre-test survey is available to be viewed in the Supplementary Information.
-
ii.
Didactic session: This was the first part of the in-person session. This 10-min didactic session was intended to be a primer on the state of surgical disparities. We started with a brief review of the basic vocabulary, definitions, and concepts of healthcare disparities as it relates specifically to surgical disease and management. In addition, we give an overview on the state of disparity research and education in surgery and introduce the conceptual framework for recognizing and discussing surgical disparities which was established by the ACS in 2016. The framework contains five factors: patient factors, provider factors, system and access issues, clinical care and quality, and post-operative care and rehab [3] which were canvassed in detail and specific examples of each factor in the surgical setting were discussed.
-
iii.
Clinical vignette: A 5–6-min presentation of a clinical vignette was adapted from one of our morbidity and mortality conferences [27] and played. The vignette highlighted the disparity factor that the students chose to focus on discussing in their pre-session survey.
-
iv.
Discussion and application: The remainder of the session is a guided discussion where the framework was used to discuss the article, the multimedia adjunct, the clinical vignette, and finally bring in clinical experiences the students had faced so far in the first half of their clerkship. The academic journal article was discussed first using the PICO (patient, intervention, comparison, outcome) framework [33] as an acronym to better understand the article by working through identifying the patient or problem, the intervention, the comparison(s) of interest, and the outcome that resulted. We then highlighted the outcomes and limitations of the study and how these could be applied to clinical practice. The clinical vignette and multimedia adjunct were similarly discussed. The discussion then transitioned to the students’ subjective experiences on the rotation thus far. A focus was placed on framing the disparities they identified in the discussion using the surgical framework taught during our didactic session. The last part of the discussion was dedicated to defining how the students could make changes in their clerkships by (1) improving and increasing their personal interactions with their patients, (2) creating strategies for discussing barriers of care and social determinants of health with their patients, and (3) discussing their findings with their teams to help improve the care of their patients. In line with these goals, the students were given a question bank for how to ask their patients about various social determinants of health. This toolkit was presented at the 2022 Ochsner Chapter of Gold Humanism Honor Society Healing the Heart of Healthcare Conference [19] and is available in the Supplementary Information.
-
i.
-
F.
Implementation [26]
-
i.
Setting: This course took place at a large academic institution in an urban and suburban environment with a diverse patient population. Each clerkship (spanning two months) was split up into 3 groups of 10–20 students each. The curriculum was given halfway between the clerkship. Two of the groups were on the main campus and the curriculum was delivered in person in a small classroom setting. The remaining group comprised students from various external campuses and this session was given virtually. A total of 16 sessions spanning from September 2022 to July 2023 were given with 5 sessions given virtually.
-
ii.
Participants: All students were required to participate in the curriculum. The curriculum was administered to a total of 223 third-year medical students’ halfway through their 2-month surgical clerkship. A pre-session survey was completed by 221 students for a response rate of 99%. This curriculum was offered halfway through the rotation, so we could assess how students felt about how disparities were addressed and how comfortable they felt addressing disparities before the implementation of our session. Data were collected from September to July over the course of 16 sessions. A total of 52 students completed the session virtually. Post-session surveys were completed by all students at the end of the in-person or virtual session.
-
iii.
Facilitators: Facilitators included resident members of the DEI committee and staff surgeons that head the medical student clerkships. Those heading the discussion session were given a standardized set of materials and discussion questions to facilitate the didactic session and discussion.
-
i.
-
G.
Evaluation [26]: Our curriculum was assessed using Kirkpatrick’s Levels of Evaluation [34, 35]. We started off by assessing reaction by asking whether learners enjoyed and benefited from our curriculum with a series of questions employing a standard Likert scale. Next, we assessed if they had any knowledge acquisition with a series of questions over the didactic portion of the curriculum. This survey is available in the Supplemental Information.
-
A.
-
II.
Statistical analysis: Surveys created with Qualtrics were used to collect the data and exported into an excel document. All analyses were done using Microsoft Excel. PivotTables were employed for explanation of demographics as well as to analyze Likert-style questions. Personal identification was not collected to protect student anonymity and data were, therefore, pooled for analysis. An independent samples Student’s t test was employed to assess the difference in knowledge scores. Fisher’s tests were performed to determine if there was a significant difference in Likert scale responses when grouping the responses into an affirmative response (grouping “strongly agreed” and “agreed”) and a negative response (grouping “disagreed” and “strongly disagreed”). Fisher’s tests were performed with both the “Neutral” responses excluded and included as a negative response. A p < 0.05 was considered significant. Thematic analysis was done using an iterative process. Initially, the data were reviewed, and data were coded to represent overarching messages. A reviewing of the coded data resulted in the development of several themes including: “awareness,” “advocate,” “ask”, “empower”, and “bias”. The final data were re-analyzed with these grouped “themes” by reviewing the 83 comments left by the medical students in the post-session survey using Excel’s word-search and the “countif” function. The relevant comments were grouped by these words as “themes” to be displayed in the final report.
-
III.
Figures/tables/graphs/surveys: Figures were created using biorender.com. Graphs were created in Microsoft Excel. Tables were created in Microsoft Word. Surveys were created using Qualtrics. Since responders did not answer every question, the total “n” responses for each question are displayed in the table or figure legends.
Results
Cohort characteristics
All students completing the medical student clerkship were required to participate in the curriculum. Two hundred and twenty-three students participated in the curriculum at our single institution from September 2022 through July 2023 in sixteen sessions utilizing three different modules with five sessions given virtually using an online platform (a total of fifty-two students). The sessions were administered as a part of the third-year surgical clerkship halfway through the rotation. The breakdown of the demographics and future specialty of interest are detailed in Table 2, which includes the total “n” that completed the answers to each question in the pre-session survey. The cohort is a heterogenous population that nonetheless largely comprises those that identify as Caucasian and Non-Hispanic which is reflective of the population of the state of this study. Of the group, approximately a quarter of the cohort is directly interested in a field that involves surgery and peri-operative care and management.
There is good exposure to disparities education in UME, but not in the surgical clerkship
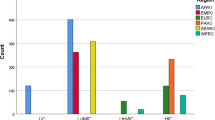
In the pre-session survey, participants were asked about their exposure to healthcare disparity education in both their pre-clinical and clinical medical school years (Fig. 2). Participants stated they had prior dedicated training in health disparities integrated throughout the UME curriculum during pre-clinical (83%) and clinical (89%) experiences, which demonstrates an overall good exposure to disparity education in UME.
(n = 208) Disparity Education in UME: The graph on the left demonstrates that 83% of participants felt that they “agreed or strongly agreed” that they had exposure to disparities education during their pre-medical undergraduate medical education while the graph on the right demonstrates that 89% of participants “agreed or strongly agreed” that they had exposure to disparities education during their clinical undergraduate medical education experiences
The next set of questions displayed in Fig. 3 looked specifically at surgical disparities. Only 31% of students agreed surgical disparities had been discussed during their rotation thus far. Furthermore, only 68% felt comfortable identifying social determinants of health in their surgical patients at the halfway point of the rotation.
(n = 207): Discussion and identification of surgical disparities. The graph on the left demonstrates that only 31% of participants felt that they “agreed or strongly agreed” that they had any discussion on disparities and SDH on their surgical rotation prior to the onset of this curriculum. The graph on the right demonstrates that 68% of participants felt that they “agreed or strongly agreed” that they could identify social determinants of peri-operative health in their surgical patients
Improved recognition of disparities
After curriculum participation, 90% of students endorsed an improved understanding of healthcare disparities and 88% stated they felt more aware of the disparities they had seen on their surgical rotation thus far (Fig. 4). There was a significant improvement in self-reported identification of social determinants of peri-operative health—improving significantly by twenty percent from 68% to 88% after implementation of our curriculum [Fisher’s exact test: p < 0.0001, 20% (95% CI: 12%-28%)] (Fig. 5). This difference is still significant when excluding “neutral” responses with 97% reporting that they “agreed or strongly agreed” that they felt comfortable identifying peri-operative disparities on the post-test compared to 88% on the pre-test (p = 0.0023).
(n = 223) Post-session assessment of disparities in surgery. The graph on the left demonstrates that 90% of participants “agreed or strongly agreed” that our curriculum had improved their understanding and framing of surgical disparities in healthcare. The graph on the right demonstrates that 88% of participants “agreed or strongly agreed” that our curriculum had helped them feel more aware of surgical disparities that they had encountered on their rotations thus far
Improved knowledge acquisition
We asked a series of questions both in the pre- and post-session surveys that assessed topics that were discussed during our didactic portions and guided discussion.
Pooled scores of all participants presented as a percentage score showed that on the pre-test (n = 197 responders), the average score was 58.9% ± 20.5%.On the post-test (n = 201 responders), the average score was 78.3% ± 19.9% which represents a significant knowledge acquisition (p < 0.0001) (Table 3).
Virtual sessions overall did not diminish overall benefit
Of the 223 participants, 52 participated in the session virtually. Analyses comparing the Likert-style responses of virtual and in-person responders are shown in Table 4.
Seventy-seven percent of students in the virtual session “agreed or strongly agreed” that they had an improved understanding and framing of surgical disparities as compared to 93% in the in-person session (p = 0.0014). However, when “neutral” responses were excluded, this difference disappears with 97.56% of virtual respondents and 98.77% of in-person respondents reporting that they had an improved understanding and framing of surgical disparities (p = 0.4937). Seventy-nine percent of students in the virtual session “agreed or strongly agreed” that they felt more aware of the disparities they had seen on their surgical rotation thus far compared to 90% in the in-person session. This difference almost approaches significance when looking at all the responses (p = 0.0528), but is definitely not significant when excluding “neutral” response (97.47% versus 97.62%; p > 0.9999). Eighty-one percent of students in the virtual session “agreed or strongly agreed” that they felt more comfortable identifying social determinants of peri-operative health after this intervention compared to 85% of in-person respondents. This difference is not significant when looking at all the responses (p = 0.5184) and when excluding “neutral” response (100% versus 96.25%; p = 0.3478). Assessment of knowledge scores revealed a pooled percentage of 79.8% ± 16.0% which represents no significant difference in knowledge acquisition when compared to the pooled average post-test score (p = 0.675).
Thematic analysis
After the implementation of the curriculum, participants were asked if they would change anything in their medical career going forward. Five themes emerged from the free-text responses given: (1) students wanted to be more aware of disparities in their patients, (2) students wanted to advocate more for their patients, (3) students wanted to spend more effort in asking about social determinants of health, (4) students felt like the curriculum helped them feel more empowered to recognize and mitigate healthcare disparities, and (5) students overall wanted to be more aware of their biases and those of providers around them (Table 5).
Discussion
Regardless of the specialty that the medical students will go into, many will participate in the complex care of surgical patients. A curriculum that not only supports the UME education that they receive, but also helps the students to apply what they have learned to the care of surgical patients was needed—both in their roles as medical students and future roles as physician providers. Although the medical students at our institution demonstrated an exposure to disparity education in their undergraduate medical education prior to starting their surgical clerkship, there was a significant lack of education in identification and comfort with disparities in the peri-operative care of surgical patients. Our curriculum addresses our goals (1) to train future physicians and surgeons to recognize how surgical disparities impact the patients they serve—demonstrated by improved knowledge gain and a subjective reporting of improved ability to recognize and identify healthcare disparities in surgical patients. Similarly, the comments from our thematic analyses highlights how we accomplished our goal to (2) reinvigorate humanism in the care of surgical patients through a better understanding of surgical healthcare disparities by having students report that they felt empowered, wanted to improve their interactions and advocacy for their patients, and work to be more aware of their personal biases. Although the scope of our data and analyses does not address our long-term goal of (3) affecting patient outcomes through improved recognition and mitigation of surgical inequities, this is a future goal.
The literature demonstrates a significant paucity in the availability of broad-based surgery-specific education on healthcare disparities in undergraduate medical education. The few curricula available are limited by small sample sizes [22, 25] or by being too specifically targeted at a specific surgical specialty [23, 24]. The strength of our curriculum is in the framework and delivery which is best illustrated in Fig. 1, allowing us to have a high-quality session targeted at general care of surgical patients and delivered in a condensed period of time. This allowed us to easily implement the module into our existing didactic surgical clerkship curriculum to our entire cohort of medical students during the period of our study. In addition, the design and flexibility of the curriculum allow us to continue to build and add modules focusing on different disparities within various frameworks easily. And finally, the setup of the curriculum design makes it easy to translate to other specialties and other surgical programs at different institutions, which will help us further expand our reach.
Our study did have a few key limitations. Although this study has a large sample size compared to other studies on surgical disparities curricula, it is limited similarly to those because it was given at a single institution. Because of time constraints, this curriculum is limited to a singular intervention. Although the materials of each module (pre-session reading and clinical vignette) highlight a specific surgical disparity factor, we did discuss the entirety of the Surgical Disparities Framework within the didactic component and address the interplay of all of the factors in relation to the pre-session materials, vignette, and student clinical experiences during the discussion. Finally, our post-session survey tests likeability and learning from our curriculum (Kirkpatrick levels 1 and 2), but does not test retention and overall behavior modification (Kirkpatrick level 3) [35].
Future directions involve completing a Kirkpatrick level 3 evaluation of our curriculum by following our medical students from this year into next year to look at the effects of our intervention on students in their fourth-year surgical sub-internship. We also plan to expand our module cache to have multiple modules that highlight each factor in the Surgical Disparities Framework. And finally, we plan to expand the resources that we offer students to address healthcare inequities. Currently the last portion of the curriculum is targeted to providing medical students with strategies to discover disparities with their patients and providing students with a handout of ways to question patients about the social determinants of health that may affect their health outcomes. We hope to expand the toolkit to include in-hospital translation resources, social work and case management resources, and more strategic resources for our students to have access to during their clinical rotation to address the health inequities they identify. With these in place, we hope to translate our curriculum design and product to other institutional surgical programs and assess the overall effect of our curriculum.
Conclusion
Our Surgical Disparities Curriculum provides a novel solution for training medical students to recognize disparities in the care of surgical patients. Our curriculum briefly reviews concepts that are taught in pre-clinical courses but specifically allows students to apply those concepts as well as the NIH-ACS Surgical Disparities Framework to surgical cases and their experiences on their clerkship so far. The intervention we provided improved our students’ ability to recognize and identify disparities in the peri-operative care of their patients and empowered our students to want to make key changes in their medical career to address disparities. We hope to continue to assess the benefits of our curriculum, expand the breadth and content of our curriculum with the aid of other content area experts, and share our curriculum with other surgical programs. Addressing disparities in surgical healthcare is a vital component to improving care for our patients—and to do so, we must train our providers. We believe our curriculum provides a key step in this process by starting this process in medical student education. By providing medical students with the tools necessary to identify and address healthcare disparities, our Surgical Disparities Curriculum represents a critical step toward developing and delivering equitable and high-quality care for all patients.
Disclosures
Dr. Dimitros Stefanidis, MD, PhD. Consultant for Applied Medical and J&J. Research Support from Intuitive and Benton Dickinson.
Data availability
The raw data that support the findings of this study are available on request from the corresponding author.
Abbreviations
- UME:
-
Undergraduate medical education
- DEI:
-
Diversity, equity, inclusion
References
Lucas FL, Stukel TA, Morris AM, Siewers AE, Birkmeyer JD. Race and surgical mortality in the United States. Ann Surg. 2006;243:281–6. https://doi.org/10.1097/01.sla.0000197560.92456.32.
Bennett KM, Scarborough JE, Pappas TN, Kepler TB. Patient socioeconomic status is an independent predictor of operative mortality. Ann Surg. 2010;252:552–7. https://doi.org/10.1097/SLA.0b013e3181f2ac64.
Torain MJ, Maragh-Bass AC, Dankwa-Mullen I, et al. Surgical disparities: a comprehensive review and new conceptual framework. J Am Coll Surg. 2016;223:408–18. https://doi.org/10.1016/j.jamcollsurg.2016.04.047.
Herrera-Escobar JP, Seshadri AJ, Rivero R, et al. Lower education and income predict worse long-term outcomes after injury. J Trauma Acute Care Surg. 2019;87:104–10. https://doi.org/10.1097/ta.0000000000002329.
Thornton RL, Glover CM, Cené CW, Glik DC, Henderson JA, Williams DR. Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Aff (Millwood). 2016;35:1416–23. https://doi.org/10.1377/hlthaff.2015.1357.
Britton BV, Nagarajan N, Zogg CK, et al. US surgeons’ perceptions of racial/ethnic disparities in health care: a cross-sectional study. JAMA Surg. 2016;151:582–4. https://doi.org/10.1001/jamasurg.2015.4901.
Jerath A, Austin PC, Ko DT, et al. Socioeconomic status and days alive and out of hospital after major elective noncardiac surgery: a population-based cohort study. Anesthesiology. 2020;132:713–22. https://doi.org/10.1097/aln.0000000000003123.
Paro A, Hyer JM, Diaz A, Tsilimigras DI, Pawlik TM. Profiles in social vulnerability: the association of social determinants of health with postoperative surgical outcomes. Surgery. 2021;170:1777–84. https://doi.org/10.1016/j.surg.2021.06.001.
Gupta A, Cadwell JB, Merchant AM. Social determinants of health and outcomes of ventral hernia repair in a safety-net hospital setting. Hernia. 2021;25:287–93. https://doi.org/10.1007/s10029-020-02203-9.
Kong A, Buscemi J, Stolley MR, et al. Hip-hop to health jr. randomized effectiveness trial: 1-year follow-up results. Am J Prevent Med. 2016;50:136–44. https://doi.org/10.1016/j.amepre.2015.07.008.
Fox M. Social determinants of health and surgery: an overview. Bulletin. Chicago: American College of Surgeons; 2021.
Wesselman H, Ford CG, Leyva Y, et al. Social determinants of health and race disparities in kidney transplant. Clin J Am Soc Nephrol. 2021;16:262–74. https://doi.org/10.2215/cjn.04860420.
Titan A, Graham L, Rosen A, et al. Homeless status, postdischarge health care utilization, and readmission after surgery. Med Care. 2018;56:460–9. https://doi.org/10.1097/mlr.0000000000000915.
Takirambudde S, Ruffolo LI, Wakeman DS, Dale Bs Ba BS, Arca MJ, Wilson NA. Social determinants of health are associated with postoperative outcomes in children with complicated appendicitis. J Surg Res. 2022;279:692–701. https://doi.org/10.1016/j.jss.2022.06.059.
Durazzo TS, Frencher S, Gusberg R. Influence of race on the management of lower extremity ischemia: revascularization vs amputation. JAMA Surg. 2013;148:617–23. https://doi.org/10.1001/jamasurg.2013.1436.
Janeway M, Wilson S, Sanchez SE, Arora TK, Dechert T. Citizenship and social responsibility in surgery: a review. JAMA Surg. 2022;157:532–9. https://doi.org/10.1001/jamasurg.2022.0621.
Lim GHT, Sibanda Z, Erhabor J, Bandyopadhyay S. Students’ perceptions on race in medical education and healthcare. Perspect Med Educ. 2021;10:130–4. https://doi.org/10.1007/s40037-020-00645-6.
Prince ADP, Green AR, Brown DJ, et al. The clarion call of the COVID-19 pandemic: how medical education can mitigate racial and ethnic disparities. Acad Med. 2021;96:1518–23. https://doi.org/10.1097/acm.0000000000004139.
Landry Am. Integrating health equity content into health professions education. AMA J Ethics. 2021;23:E229-234. https://doi.org/10.1001/amajethics.2021.229.
Weiner S. Medical Schools Overhaul Curricula to Fight Inequities. AAMCNEWS. 2021. https://www.aamc.org/news/medical-schools-overhaul-curricula-fight-inequities.aamc.org.
Backhus LM, Lui NS, Cooke DT, Bush EL, Enumah Z, Higgins R. Unconscious bias: addressing the hidden impact on surgical education. Thorac Surg Clin. 2019;29:259–67. https://doi.org/10.1016/j.thorsurg.2019.03.004.
Janeway MG, Lee SY, Caron E, et al. Surgery service learning in preclinical years improves medical student attitudes toward surgery, clinical confidence, and social determinants of health screening. Am J Surg. 2020;219:346–54. https://doi.org/10.1016/j.amjsurg.2019.11.010.
Goodsell KE, Familusi O, Mulvey HE, Williams C, Yeguez A, Brooks AD. Teaching what matters: integrating health equity education into the core surgery clerkship. Surgery. 2022;171:1505–11. https://doi.org/10.1016/j.surg.2021.10.010.
Rhodin KE, Hong CS, Olivere LA, et al. Implementation of a surgical oncology disparities curriculum for preclinical medical students. J Surg Res. 2020;253:214–23. https://doi.org/10.1016/j.jss.2020.03.058.
Zhao CS, Owei L, Card E, et al. Introducing surgical equity into contemporary medical education: results from operation equity, a pilot curriculum. J Surg Educ. 2023;80:528–36. https://doi.org/10.1016/j.jsurg.2022.12.004.
Kern DE. Curriculum development for medical education: a six step approach. Baltimore: Johns Hopkins University Press Baltimore; 1998.
Zaidi MY, Doster DL, House MG, Dunnington GL, Choi JN. The disparity morbidity and mortality conference: a mechanism to identify and remedy health care inequity. Ann Surg. 2022;276:e205–7. https://doi.org/10.1097/sla.0000000000005570.
Presser L. The black american amputation epidemic, vol. 2022. New York: ProPublica; 2020.
Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial disparities in pain management of children with appendicitis in emergency departments. JAMA Pediatr. 2015;169:996–1002. https://doi.org/10.1001/jamapediatrics.2015.1915.
Jackson G. Pain and prejudice: a call to arms for women and their bodies: little, Brown Book Group. 2019, https://books.google.com/books?id=3YKaDwAAQBAJ.
Leech MM, Briggs A, Loehrer AP. Surgical diseases are common and complicated for criminal justice involved populations. J Surg Res. 2021;265:27–32. https://doi.org/10.1016/j.jss.2021.02.050.
Pazzanese C. Supreme Court may halt health care guarantees for inmates. Harvard Gazette. 2023.
Eriksen MB, Frandsen TF. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. J Med Libr Assoc. 2018;106:420–31. https://doi.org/10.5195/jmla.2018.345.
Sweet LR, Palazzi DL. Application of Kern’s Six-step approach to curriculum development by global health residents. Educ Health (Abingdon). 2015;28:138–41. https://doi.org/10.4103/1357-6283.170124.
Kirkpatrick DL. Evaluating training programs: the four levels: First edition. San Francisco: Berrett-Koehler; Emeryville, CA : Publishers Group West. [1994] ©1994; 1994, https://search.library.wisc.edu/catalog/999764622302121.
Funding
This work was supported by an institutional Primary Care Reaffirmation for Indiana Medical Education (PRIME) grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file 1:
(PDF 123 KB)
Supplementary file 2:
(PDF 175 KB)
Supplementary file 3:
(PDF 49 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Manohar, K., Krusing, M., Braafladt, S. et al. Creating a more equitable future: development, implementation, and evaluation of a novel surgical disparities curriculum for medical students. Global Surg Educ 3, 38 (2024). https://doi.org/10.1007/s44186-024-00227-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44186-024-00227-8