Abstract
Over the past four decades, rates of emotional problems in adolescents have increased in many countries, and outcomes for those with mental health problems have worsened. In this review we explore existing population-based studies to evaluate possible explanations for these trends. We include population-based studies that examine both trends in adolescent emotional problems, as well as risk or protective factors previously hypothesised to be associated with trends in youth depression and anxiety. The available evidence on risk or protective factors trends related to family life, young people’s health behaviours and lifestyle, school environment, peer relationships, as well as poverty. Studies reviewed suggest that trends in emotional problems are associated with increases in parental emotional problems, youth weight-control behaviours and eating disorders, school-related stress, as well as a rise in family poverty and social inequality in the 21st Century. One of the biggest changes in young people’s lives over the last few decades has been the rise of digital media to access information and interact with others, but implications for trends in mental health remain unclear. Other trends are likely to have mitigated against even steeper increases in youth emotional problems, for example improvements in youth substance use and a possible long-term reduction in child maltreatment. Epidemiological studies of unselected cohorts testing explanations for secular trends in mental health are scarce and an urgent priority for future research. Such studies will need to prioritise collection of comparable data in repeated population cohorts. Improving young people’s mental health is a major societal challenge, but considerably more needs to be done to understand the connections between social change and trends in youth mental health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Mental health problems are a leading cause of disease burden amongst adolescents globally. Depression and anxiety are distressing for young people and their families, and they have both immediate and long term consequences for young people’s psychosocial development, their education, and health [1]. Common mental health disorders typically have their origins in the child and adolescent years [2, 3], and collectively, are projected to cost the global economy an estimated US$ 16 trillion between 2011 and 2030 [4]. Improving adolescent mental health thus represents an important global public health challenge.
Evidence on the progress being made to meet this societal health challenge paints a gloomy picture. There is now an abundance of high-quality epidemiological evidence demonstrating that over the past four decades, rates of adolescent mental health problems have increased, inequalities in rates of problems and access to evidence-based support have widened, and outcomes for those with mental health problems have worsened [5, 6].
Cross-cohort comparisons using equivalent, psychometrically robust screens of adolescent depression and anxiety symptoms have shown long-term increases in many countries [7,8,9,10,11,12], but see also exceptions [13]. Direct epidemiological comparisons of unselected cohorts using interview-based assessments of mental health disorders are less widely available, but extant data support these conclusions [14]. At the beginning of the 21st Century, around 1 in 10 young people in the UK met criteria for a psychiatric disorder, increasing to 1 in 8 in 2017, and to 1 in six by 2020 [14]. These increases were most marked for adolescent emotional disorders like depression and anxiety, where more than a 50% increase in prevalence has been observed amongst 11–16-year-olds in the UK [14]. Evidence from Australia comparing parent-reported rates of adolescent psychiatric disorders between 1998 and 2014 also point towards a substantial rise in adolescent major depressive disorder, particularly among females [15]. In the US, annual survey data found an increase in the 12-month prevalence of adolescent major depressive episodes between 2005 to 2014, again most prominently for females [16]. It is clear then that increases in youth depression and anxiety predate the COVID emergency. The impacts of COVID-19 on youth mental health have been reviewed elsewhere [17, 18]. Our aim here is to instead better understand influences that may explain the longer-term trends in youth mental health that predate COVID and are likely to influence patterns of adolescent mental health needs into the future.
1.1 Explaining trends in adolescent mental health
This review examines possible causes of longer-term population level increases in adolescent emotional problems (depression and anxiety). This is important for informing population health interventions to improve adolescent mental health. Testing explanations for trends in youth mental health is challenging because social trends are unlikely to have uniformly impacted young people, and because of methodological differences that can affect comparability of studies of different generations of young people. There is a dearth of studies using comparable sampling frames that also include equivalent measures of potential explanatory factors and mental health. With these caveats in mind, we address in turn potential impacts of changes in family life, lifestyles (including health-related behaviour and digital technology use), school life, peer relationships and poverty on trends in young people’s mental health. Our broad focus is informed by recognition that population-level changes in the prevalence of youth mental health problems very likely reflects the interplay of societal trends affecting young people via changes in individual, family, social and contextual influences [5], as well as the imperative that the population-based approaches to prevention needed to address this accelerating global health emergency [19] require understanding of which potentially modifiable risk and protective factors are implicated in trends in youth emotional problems (and which are not). Our choice of domains of focus was informed by previous reviews of possible explanatory factors of particular salience in the adolescent period that might account for trends in youth mental health [11, 20, 21, 25] and because there is strong evidence both for their relevance to youth emotional problems [1, 22,23,24], and evidence of temporal change in population prevalence.. Note we do not include genetic or biological factors as the aim was to focus on factors that could be feasibly targeted in interventions aimed at improving population mental health. We consider in this review, both positive and negative drivers of trends in youth mental health. In other words, we anticipate that in some areas, improvements might have mitigated against steeper than observed rises in mental health problems.
1.2 Literature search strategy and quality assessment
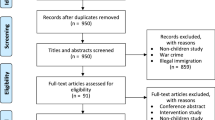
The literature review was conducted between March 2023 and August 2023.We searched publications using PubMed. Initial searches included terms related to time trends (e.g. “secular trend” OR “time trend” OR “temporal trend” OR “national trend” OR “cross-cohort” OR “cross cohort” OR “cohort comparison”), with additional terms related to youth (e.g. “child” or “adolesc*” or “young” or “youth”), emotional problems (e.g. depress* OR emotion* OR “anxi*” OR “internalizing” OR “internalising”) and specific explanatory factors of interest (e.g. maltreatment OR abuse OR harsh parent*). Few studies were identified and therefore broader search terms related to “trends” more generally were subsequently used. Note that given the nature of the terminology, ‘trends’ retrieves many irrelevant articles making a fully systematic review impractical in this field. Where possible we included search terms linked to trends but primarily considered core terms and existing knowledge, and also examined citations lists. Additional papers were identified using citations to and by papers identified in our search. To be included, papers must have either investigated how risk or protective factors related to youth mental health have changed over time, or tested the role of risk or protective factors in explaining increases in youth mental health problems across time. We aimed to specifically identify papers that directly addressed the second of our study questions, and also highlight key reviews and papers related to the first.
Publications were selected if they used epidemiological cohorts to examine trends over any period between 1980 and 2023. This was to align with international evidence showing long-term increases in emotional problems among young people over this period [25, 26]. We do not restrict papers by country or region, and where applicable, note that variations across countries may exist, and that trends in risk factors and emotional problems may be non-linear over the historical period considered in this review. We summarise an overview of findings in Table 1. Details for specific studies selected can be found in Supplementary Table 1 (Trends in family, school, peer and lifestyle factors) and Supplementary Table 2 (Trends in family, school, peer and lifestyle factors and associations with trends in youth emotional problems).
Study quality was assessed using a modified version of the Newcastle–Ottawa Scale (NOS: [27]; see also [28, 29]). Modifications to the quality assessment were to ensure quality assessment was aligned to cohort comparison study design (see [30]) and also to time trends research. In particular, comparability of study cohorts and measures were included as key domains in our quality assessment (Supplementary Table 3).
2 Family factors
Trends in family structure are well documented, with rising rates of parental divorce and separation in the second half of the 20th Century, a shift from marriage to parental cohabitation, and a reduction in family size [31]. However, evidence suggests that these changes have not made a major contribution to trends in youth mental health as similar increases in adolescent emotional problems are observed for young people growing up in different family structures [32,33,34]. Furthermore, family processes (e.g., parenting, parent–child relationship quality) and proximal family risks (e.g. parent mental health, child maltreatment), rather than family structure, better explain youth adjustment. Relatively few studies include comparable measures of specific family processes for different generations of children. Nevertheless, studies are beginning to demonstrate how children’s family environments have changed over time, including changes in parent psychopathology, child maltreatment, and parent–child relationships.
2.1 Parental mental health
One of the best-established risk factors for youth emotional problems is having a parent with depression [1]. Studies using registry data in the UK [34] and Sweden suggest that rates of parent mental health problems have increased over time (see Supplementary Table 1). We identified only one study that has tested the link between trends in parental mental health and youth emotional problems [35]. In the study of two population cohorts, rates of maternal and adolescent emotional problems both increased between 1986 and 2006. Estimated cohort differences in adolescent emotional problems were reduced when accounting for increases in maternal emotional problems, suggesting that increases in maternal emotional problems may have contributed to the increasing prevalence of adolescent emotional problems. Whilst girls had higher levels of emotional problems than boys, with a greater increase over time for girls compared to boys (d’ = 0.37 and 0.13 respectively), there was no difference in the strength of the association between parent and offspring emotional problems for boys and girls (see Supplementary Table 2). Given evidence of intergenerational transmission of risk of depression and anxiety via both heritable and environmental mechanisms [36, 37], it is possible that continuing increases in emotional problems in the current generation of young people will lead to increases in emotional problems in the next generation [5]. It is important to consider that effects were relatively small, suggesting the role of multiple risk factors for youth emotional problems.
2.2 Child maltreatment
Child maltreatment refers to experiences of physical, sexual, emotional abuse and neglect [38], and is an important and likely causal risk factor for child psychopathology [39] including emotional problems [40, 41]. There are major challenges in accurately monitoring the population prevalence of child maltreatment due to ethical and practical challenges in population-based surveys, the possibility of under-reporting by informants, and due to the fact that the majority of maltreatment experiences are not known to authorities and so will not be reflected in official records [42]. Nevertheless, rates of child maltreatment appear to have declined substantially in the US since the early 1990s (1992–2018) when assessed using child protection or maltreatment data [43]. Evidence from the UK using official government records, shows similar declines in maltreatment, with reductions of child cruelty and neglect from 1983–2016 [44]. One UK population prevalence survey examining trends in abuse and neglect also suggested a decrease in emotional and physical abuse (but not neglect) from 1998 to 2009 [40]. However, not all findings are consistent: a review of child maltreatment using data about child protection across six indicators found little evidence of long-term change in rates of maltreatment [45]. In the UK there have been increases in child protection registrations for emotional abuse and neglect and increases in children entering care from 2000–2016 [42, 44, 46], although this may be due to changes in practice, reporting, or shifts in maltreatment.
We identified only one study examining the role of parental maltreatment on trends in adolescent mental health, and this focused on conduct problems, with evidence that declining levels in family violence during the period 2007–2015 may help to explain reductions in youth aggression [47]. We did not identify any studies that examined trends in maltreatment in relation to youth trends in emotional problems. Nevertheless, given the apparent opposite long-term trends in maltreatment and adolescent emotional problems, it seems likely that any reduction in child maltreatment would have mitigated against even greater increases in youth emotional problems.
There are several possible reasons why rates of maltreatment have shown a long-term reduction. These include economic changes, public health measures, shifts in societal attitudes and changes in policy and legal frameworks, but these require further investigation.
It is also important not to be complacent. The prevalence of child maltreatment remains high and for most forms of abuse, rates reported in unselected epidemiological surveys are many times higher than those identified by police and other authorities. In addition, it is important not to assume that long-term improvements have or will continue into the future. The past decade has seen increased pressures for families and communities due to austerity, increases in family poverty, and cut-backs to social and community sources of support [48,49,50]. Research highlights that economic hardship and greater social inequality is associated with increased risk for abuse [51, 52]. Furthermore, the Covid-19 pandemic and ‘lockdowns’ may also have increased risks for child maltreatment and harsh parenting [53,54,55,56,57]. Importantly, whilst administrative data (e.g., social services records, police reports) suggested a reduction in official notifications of child maltreatment compared to prior to the pandemic [58], this is likely explained by reduced access to schools, health and other family services that are typically involved in the identification of maltreatment warning signs. Indeed, there were increases in hospital admissions linked to maltreatment [59] suggesting a potential increase in prevalence or severity of maltreatment in the population, highlighting that at that time only the most severe cases of maltreatment might be identified. Urgent priorities for future research are to more effectively monitor trends in maltreatment using multiple data sources [60] and to identify how trends in maltreatment are linked with trends in adolescent emotional problems.
2.3 Parenting and parent–child relationships
The quality of the parent–child relationships and parenting have been associated with risk for adolescent emotional problems (e.g., warmth, support, communication, quality time; [61, 62]). A limitation of many studies that examine trends in parent–child relationships is that they have used proxy measures such as frequency of family activities or time spent together (e.g., [63,64,65,66,67]). Time diary studies suggest increases in time spent of parents with children, especially fathers [66,67,68], but a decrease in joint family meals [63, 67]. Such studies do not provide information regarding the quality of time spent between parents and children. More limited evidence suggests that there have been changes in the quality of parent–child and family relationships [68,69,70]. A number of studies suggest increases in proportion of adolescents who find their mother or father easy to talk to in Europe from early to mid-2000s [71, 72]). A UK study also provided evidence of stable or increasing emotional support, communication, and quality time with parents from 1986–2006 [73]. Overall, there is little evidence of a decline in family relationship quality [5].
Where trends in parent–child relationships have been examined in relation to child outcomes, this has primarily been in relation to externalising problems and risky behaviours (e.g., [72, 74, 75]). We identified two studies that examined trends in parent–child relationship quality and changes in youth emotional problems. One study employed a sample of Scottish adolescents and found that young people reported declines in family relationship quality between the mid-1980s and mid-2000s including increased worry about family stability and relationships and more frequent arguments with parents [76]). These changes in the parent–child relationship had a moderate impact on increases in adolescent depression from 1987–2006, and such associations appeared to be stronger for girls compared to boys [76]. A more recent study from the Netherlands reported improvements in parent-adolescent communication (in 2017 compared to 2013) which functioned as a protective factors against a downward trend in emotional wellbeing. Again associations were stronger for girls compared to boys [77].We identified no other studies that examined changes in parent–child relationship quality and youth emotional problems. Therefore, while the majority of research suggests there has not been a general decline in parenting, given inconsistent evidence, further research is needed.
2.4 Inter-parental conflict
Despite the well-established role of interparental conflict for youth adjustment, including emotional problems (see [78]), few studies examine trends in interparental relationship quality. We identified no studies that investigated trends in interparental relationship quality below the threshold of domestic violence/safeguarding, and none that examined trends in interparental relationship quality in relation to trends in youth mental health. In addition, although evidence suggests reductions in youth exposure to domestic violence, trends in domestic violence may not be linear. Recent economic recessions [79], and Covid-19 lockdowns [54, 55, 58, 80] have been linked to increases in domestic violence. It will be important to continue to examine potential changing trends in domestic violence (and other constructs within the interparental relationship), and their associations with trends in youth mental health.
A challenge for the field is to move beyond charting change in family demographics (family type, marital status, parental age, family size) to better understanding how the nature and quality of family life is changing. As highlighted, only few studies have tested how family dynamics are changing over time, and fewer still have tested the contribution of such change to children and young people’s mental health. It is important to consider how increases in emotional problems in young people might also impact on family relationships and parents’ own mental health. Finally, a number of studies suggest that trends in family processes, such as parenting may vary by socioeconomic status (SES) [73, 81, 82]. These studies highlight that social change may not have impacted on the family lives of young people uniformly [6, 29, 83]. Future research should examine factors, such as SES, that moderate/modify trends in family processes and youth mental health.
3 Lifestyle and health-related factors
There is considerable interest in modifiable lifestyle factors that could underpin mental health promotion, prevention, and management of common mental health problems in the community [1, 21, 84]. Evidence suggests that healthy sleep, diet and physical exercise are associated with lower rates of mental health problems, while substance use and problematic internet use are associated with a greater risk of mental health problems. Identifying causal effects that rule out the effects of confounders and reverse causation can be challenging, and there are only very few randomized controlled trials in children and adolescents. Nevertheless, it is plausible that any deleterious change in young people’s lifestyles and habits that impact mental health at the individual-level, such as sleep, diet, use of alcohol and drugs, could also play a role in determining population-level mental health trends.
3.1 Sleep
Meta-analytic evidence shows a robust but small prospective association between disturbed sleep and subsequently increased depression symptoms [85]. With respect to secular trends, most studies of adolescent sleep have considered sleep duration rather than sleep quality. Current sleep guidelines for adolescents recommend eight hours of sleep per night [86]. Many young people regularly sleep less than this. For example, in the US, in 2015 more than 40% of adolescents reported sleeping less than seven hours on a typical night [87]. Very large surveys of young people in Europe [11, 88], North America [89,90,91,92], and Japan [93] suggest that the last two decades have seen an increase in the proportion of young people who sleep for durations considered insufficient. This follows reductions in sleep duration over the course of the 20th Century [94]. Findings on trends are robust for younger and older adolescents, males and females, and for different demographic groups. It appears decreased sleep is due to later bedtimes rather than earlier waking [11, 93] because with a small number of exceptions (such as California in the US), the start of the school day has not changed.
Far fewer studies have tested secular trends in sleep quality, and there are none to our knowledge that have used objective measures like polysomnography or actigraphy. Several studies have examined trends in self-reported insomnia symptoms (primarily difficulties falling asleep). Here, evidence of secular change is mixed. A review of large school-based surveys across Europe found that there was a modest increase in self-reported sleep difficulties in many but not all countries (an overall increase in prevalence of 17.5 to 20.8% between 2002 and 2014; [88]). In contrast, in Japan evidence suggests symptoms of insomnia and poor self-rated sleep quality had reduced between 2004 and 2017 [93], while a Canadian study of 12–24 year olds found no change in sleep difficulties between 2011 and 2018 [95]. To our knowledge, no study has directly tested the contribution of secular change in sleep to observed trends in youth mental health.
3.2 Substance use
A comprehensive review of trends in smoking, drinking and alcohol use is beyond the scope of this paper (see recent reviews e.g., [96,97,98]. Evidence shows that the global prevalence of cigarette smoking by young people reduced in the majority of countries in the 21st Century, but that the use of other tobacco products remained stable or had increased [96]. Many countries have seen an increase in electronic cigarette use (‘vaping’) [99]. For adolescent alcohol use—including regular drinking, early alcohol initiation, and binge drinking—evidence reveals declines over time. This is observed consistently across high-income countries for both boys and girls [97, 100], but there are regional variations in the global reduction of alcohol use [97], and alcohol use remains a major contributor to the burden of disease amongst young people [101].
Trends in drug use are less clear. Some studies suggest an overall decline in many countries for cannabis and other illicit drugs by young people in the 21st Century [102], whilst others suggest that cannabis use has remained stable or increased [103, 104]. There are suggestions that where cannabis use has been decriminalised or legalised this has led to an increase in use, at least in adults [98]. While cannabis remains the most common illicit drug used by young people, there are important variations in trends for other drugs [102]. One important issue is that there are changes in the potency of some drugs such as cannabis [104], and evidence suggests that high potency cannabis is more strongly associated with common mental health problems including anxiety disorders [105]. In general, however, it appears unlikely that secular changes in adolescent substance use account for the increase in depression and anxiety observed in young people, given overall reductions or stable trends in most forms of adolescent substance use.
Where time trends studies have directly tested associations between substance use and mental health in the same samples (e.g. [106,107,108]; or [109] in adults), evidence is largely consistent with this conclusion; two studies found no evidence that the increase in youth mental health problems can be attributed to changes in substance use risk [107, 108], however, another suggested that increases in cannabis use and alcohol use in Norwegian samples in the 1990s might have made a small contribution to an increase in depressive symptoms in young people over that time period [108]. Conversely, it is possible that increases in youth mental health problems might have been more marked had it not been for overall long-term improvements in many forms of substance use in many countries. The patterning of mental health problems has also changed, with studies suggesting that young people who engage in substance misuse are now at relatively higher risk of mental health difficulties than in previous generations [106], consistent with similar data from adult samples [109, 110]. This means that while the population prevalence of some forms of problematic substance misuse like smoking and alcohol use have declined over time, substance users are more likely to present with mental health difficulties, and trends over time may be greater for those with higher levels of substance use.
3.3 Physical activity and sedentary behaviour
The World Health Organisation (WHO) recommends that people under the age of 18 undertake at least 60 min of moderate-to-vigorous activity per day, but globally only 20% meet this threshold [111], and most exceed recommended limits on sedentary behaviour [112, 113]. Evidence suggests that exercise is likely protective, and excessive sedentary behaviour a risk for mental health problems, especially depression [113,114,115,116,117]. Understanding trends in youth physical activity is therefore important.
Studies that have examined trends in physical activity, sedentary behaviour, and fitness provide only partial support for the hypothesis that changes over time have contributed to increases in youth depression and anxiety. Evidence on pre-pandemic 21st Century trends suggest that rates of physical activity remained relatively stable or even showed a small increase in young people [113]. At the same time, some, but not all, studies suggest an increase in sedentary behaviour—linked to an increase in digital screen time [112, 118]. Two large meta-analyses of studies using tests of physical fitness (endurance, strength, speed, flexibility) also point to a decline in physical fitness in children and adolescents, especially endurance [119, 120].
Few, if any, studies have directly tested whether trends in youth physical activity, fitness and sedentary behaviour account for the increase in youth depression and anxiety. Many studies have been limited by reliance on self-report measures of activity. Furthermore, mechanisms underlying links between physical activity and mental health are complex, reflecting shared confounding (e.g. social adversity), bidirectional associations (with mental health also influencing activity levels), and potential mediation via biological, social, and psychological pathways.
It is also important to consider young people’s motivations for exercising. Emerging evidence suggests a substantial population-level increase in exercising as a weight-control behaviour [121, 122]. A comparison of two British population cohorts born in 1970 and 2000 found that the prevalence of exercising to lose weight amongst 15–16 year olds increased from 6 to 60% over this 30-year period [122]. Further, the study showed that exercising as a weight-control behaviour became more strongly associated with symptoms of depression in the more recent generation, especially in females. This is important given evidence of increases in rates of eating disorders both in clinical settings and in population-based surveys of young people [123]. More generally, evidence suggests that unhealthy BMI has become more strongly associated with depression among young people today [106].
3.4 Impacts of the digital age
There has been a well-documented increase in the ubiquity of digital media and electronic device use in society, particularly amongst adolescents [117, 118]. Largely correlational evidence highlights associations between the total daily amount of online activity (social media use especially) and mental health: UK and US studies suggest that heavy users (> 2 h per day) are approximately twice as likely to experience depression and low wellbeing than light users [124, 125]. Furthermore, excessive social media use is related to risks of online harassment, poor sleep, low self-esteem, and poor body image [124], each of which are linked in turn with symptoms of depression. However, whether and to what degree social media use and other digital activity can have harmful effects on young people’s mental health is strongly debated (e.g.; [126, 127]). Robust evidence using causally informative designs is limited, and it is likely that associations will vary according to the nature of young people’s interactions with their digital environments, as well by young people’s developmental maturity and sex [128].
Twenge [118] suggests several ways in which generational changes in young people’s use of digital media might result in secular increases in the prevalence of youth emotional problems. Digital device use can reduce opportunities for in-person social interactions or change the nature of social interactions, including through cyberbullying or exposure to harmful online content, as well as interfere with healthy and sufficient sleep. However, evidence highlights that digital exclusion during COVID lockdowns was linked to increased youth mental health difficulties [129], suggesting a more complex relationship. In our view, it will be critical to move beyond simple ‘quantity’ measures of digital use towards a richer characterisation of the ‘quality’ of young people’s digital environments and their online social interactions. Taking into account young people’s views and advice will be critical for delivering meaningful answers to these important questions.
4 School factors
The social and economic demands placed on young people today are markedly different from those of previous generations. Adolescents face a more competitive job market when they finish school, with rises in skill and educational requirements [130] as well as knowledge-intensive jobs [131]. This added pressure has likely also changed how adolescents interact with their social and academic environment.
4.1 School stress
Multiple educational reforms have taken place in the UK (as in many countries), with increased emphasis on grading, assessing, and testing children as a means of tracking progress, increasing accountability, and improving educational outcomes [132]. More demanding and ambitious standards set for pupils, together with greater regularity of assessment, can be a significant source of anxiety. Indeed, several studies have noted increased school-related stress, academic pressure and burnout among adolescents in more recent generations [133,134,135,136], although there is variation across countries [137]. with some noting smaller changes across time [138].
Female adolescents in particular have become increasingly worried about doing well at school, with evidence that this is a long-term trend [76, 139, 140]. One hypothesis is that increases in youth emotional problems, together with a widening gender gap in mental health problems, can be attributed in part to greater educational pressure [76, 141], with one study suggesting that around 50% of the growing gender gap for internalising problems could be attributed to increases in school-related stress [139].
A recent study with over 150,000 adolescents from 33 countries, found stronger associations between school stress and mental health problems between 2002 and 2014 [131]. This was particularly the case for countries in which the gross domestic product (GDP) per capita was higher, and where there had been a rise in tertiary attainment [131]. In other words, school stress became more predictive of mental health as countries grew richer and more educated. Note that these findings were based on cross-sectional data, therefore causal inferences are limited. They were also based on European countries, and there is likely to be variation between these findings and those from lower income countries. Nonetheless, the findings point towards a potential, albeit small role, for school stress in Europe, and more broadly, societal pressures and educational systems as predictors of increased youth mental health problems. These societal pressures appear to be particularly prevalent among females, which has been suggested to be because females are more dependent on education for their labour market opportunities [131]. Females typically outnumber males in higher education settings in high-income countries, which may mean that females experience pressure more strongly.
4.2 School belonging, engagement, and satisfaction
Research suggests there have been reductions in feelings of school belonging [141, 142] and school satisfaction over time [143], although there is variation by both gender and country, and no evidence to date that these factors have implications for trends in youth emotional problems. One study that did examine the consequences of high-stake testing in relation to mental health found support for a negative impact through academic self-esteem [142]. In particular, it was found that an educational reform in Sweden, which increased the use of grading, assessments, and test-based teaching, had an adverse impact on self-esteem which in turn, increased psychosomatic symptoms among adolescents. The negative effects were generally greater among females, widening the existing gender differences in mental health across time. It was suggested that by making the relative performance of pupils more explicit, intense grading systems heighten social comparison and competition, which may further intensify stress and emotional problems. In support of this, whole-school interventions focused on improving both the academic (teaching and learning) and community climate (relationships) have had beneficial effects on overall school climate and pupil mental health [20]. A broader understanding of changes in educational and school factors (e.g., curriculum, policies, practices and culture), as well as pupil experiences (e.g., feelings of belonging and connectedness to school), could help shed light on whether any school-level changes have led to improvements in youth mental health.
5 Peers
Peer relationships play a vital role in shaping child and adolescent mental health [143]. When there are problems, such as isolation or experiences of bullying, this can pose a risk to both concurrent and later mental health [144]. Conversely, friendships are an important source of wellbeing and peer support can play an important role in promoting resilience in the face of adversity [145]. Yet little attention has been devoted to understanding how social relationships have changed over time [146], and even fewer studies have explored whether secular changes in social relationships are related to increasing emotional problems.
Data available on trends in peer relationships is mixed. In England, declining rates of bullying were reported from adolescents between 2002 and 2014, particularly among males [147], yet cross-cohort studies reported increases in parent-rated peer problems between 2005 and 2015 [11]. Surveys from Scotland revealed similarly mixed results, with fewer individuals aged 11 to 15 years reporting that their classmates were kind and helpful to them in 2014 compared to in 2002, but stable rates of bullying were also noted between 2002 and 2010 [148]. Research conducted across Europe and North America noted decreasing or stable rates of bullying among males in 31 out of 37 countries between 2002 and 2014, and in 29 out of 37 countries for females [147]. This has led some to argue that changes in bullying are unlikely to account for the rise in youth mental health problems [149].
Lower rates of reported bullying over time in many countries may be due to the increased adoption and success of anti-bullying strategies [150]. Students report feeling safer and more supported by adults in school when it comes to bullying, according to data from over 245,000 students in the US [151]. These improvements to rates of school bullying have been suggested to have prevented further upward trends in emotional problems. Indeed, a comparison of trends in emotional problems unadjusted or adjusted for trends in peer victimisation between 2005 and 2017 in the Netherlands supports this conclusion [77]. It was noted that the decline in victimisation may explain why emotional wellbeing only declined slightly between 2013 and 2017, despite increases in school pressure.
The literature on time trends in peer difficulties has focused predominantly on changes in traditional peer victimisation [147], but recent years has seen more widespread concern about online experiences of bullying [39]. A meta-analysis of studies that have incorporated measures of cyberbullying since the mid-2000s found that while face-to-face physical or verbal bullying decreased from 20% in 1998 to 10% in 2017, and from 23% in 2005 to 9% in 2017, cyberbullying increased from 10% in 2000 to over 16% in 2017 [152]. Research in Australia noted a rise in cyberbullying between 2015 and 2020 [153], with findings in the US also noting a shift towards increased cyberbullying between 2016 and 2021 [154].
5.1 Loneliness
Increases in communication online may also have had a negative impact on in-person connections. Between the late 1970s and 2017, the number of teens in the US who ‘meet up with their friends almost every day’ dropped from around 52% of children to just 28% in 2017 [155]. The average time spent socialising in person with friends also decreased. These reductions were particularly apparent from 2010, when digital media use proliferated [156] and rates of reported loneliness increased [157]. Loneliness is important for mental health, and findings have shown that nearly twice as many adolescents displayed high levels of loneliness in 2018 compared to in 2012 [157]. Yet research studies examining changes to rates of loneliness in relation to changing mental health are lacking. The degree to which changing friendship quality, bullying and loneliness have influenced emotional problems in adolescence therefore remains an important avenue for further study.
A key challenge for future research is to understand how the quality of relationships among peers has changed. Most research has focused on bullying and peer problems as opposed to peer support and friendships. Young people today may be reliant on different types of support or contact with peers. For instance, research should explore how young people are engaging with the internet to connect with peers, and how this may be influencing their behaviours and subsequent mental health. Such research should be mindful that certain sub-groups, namely those from minority and less affluent households, have witnessed a greater rise in online harassment over time [158], as well as greater increases in loneliness [159]. Further research should therefore consider possible moderating effects of socioeconomic status.
6 Poverty
Many of the explanatory factors included in our review are disproportionately experienced by those experiencing social or economic disadvantage, and in many cases trends in these risk factors were worse for more disadvantaged children. Poverty is an important, and likely causal [160], risk factor for mental health problems for young people. International evidence demonstrates that despite some global progress in alleviating extreme poverty, inequalities have increased in the majority of countries [161, 162]. Even in high income countries child poverty has substantial impacts on life course outcomes, and impacts of poverty on youth mental health have become more pronounced over time [17, 50, 163]. More than a decade of austerity measures in many countries has led to increases in child poverty and increasingly stretched mental health services for young people. The global economic cost-of-living crisis means that there is a strong likelihood that the mental health crisis will deepen as the current generation of children grow up [164]. Failure to reduce widening social inequalities could result in further secular increases in mental health problems, and most prominently for those from disadvantaged backgrounds [165].
7 Concluding comments
This study reviewed existing evidence of secular trends in known risk and protective factors associated with youth depression and anxiety. Our search of the literature revealed that epidemiological studies of unselected cohorts examining predictors of increasing mental health trends are scarce, and it is clear that despite the increased concern for child and adolescent mental health over the years, more needs to be done to understand and prevent further increases in problems. Nonetheless, the studies included in this review suggest that increasing trends in youth mental health are likely driven by multi-faceted changes to young people’s lives. Our review highlights some risk factors that play a likely role, including increased parental emotional problems, increased school-related stress among adolescents, and increases in poverty. Evidence also suggests that in some instances, changing trends may have mitigated further increases in emotional problems. This was the case for reduced rates of some types of child maltreatment, bullying and substance misuse. It is important to note that only very few studies have directly tested the contribution of trends in risk factors to trends in youth mental health or considered the role of protective influences. In addition, while most studies had representative samples and identical or highly similar measures, most relied on self-reports or single item measures. Information gathered from multiple informants could further aid our understanding of how factors may have changed over time.
Despite the broad scope of the current review, it is important to recognise that it should not be considered exhaustive with respect to all possible drivers of trends in youth mental health. For example, specific important stressful events such as discrimination and sexual harassment were not included as no population-based studies were identified. Studies investigating the role of broader cultural factors such as changes in globalisation, individualism or materialism, were also not found, but are likely to be shaping societies in profound ways [166]. It is possible that these changing risk factors may have impacted rates of youth emotional problems, Furthermore, it was beyond the scope of the review (and indeed the available evidence) to consider whether different explanations are needed to explain trends for specific marginalised groups of young people. It is well-established that risks of emotional problems are substantially increased for young people who are neurodiverse, LGBTQ + or who belong to other marginalised groups, and it is certainly possible that societal trends will have impacted differentially on these groups [167, 168]. One difficulty is that repeat epidemiological surveys of youth mental health are typically insufficiently powered to provide firm evidence on variation in prevalence trends for minority groups, let alone the scope to test whether and how explanations for trends might differ.
Future work should also aim to establish the direction of associations. It is possible that some of the observed changes in hypothesised explanatory factors are in fact a result of increases in youth mental health problems. Cross-cohort studies that also include within-cohort longitudinal data are rare but particularly valuable for examining this question. In addition, it is also important to consider potential methodological artefacts that might contribute to cross-cohort differences in youth mental health, and care is needed to ensure the robustness of observed findings to differences in patterns of confounding or differences in sample selection (see [27] for further details and for a guide on conducting cross-study research).
The majority of studies reviewed focused on dimensional measures of emotional problems, with very few testing how trends in risk factors relate to trends in emotional disorder. However, epidemiological studies testing prevalence trends are consistent in showing increases in both symptoms and disorder [23]. In the UK, evidence also highlights that cross-cohort differences in prevalence are greater for higher symptom severity thresholds [70]. More generally, it is important to recognise that subclinical threshold symptoms of disorders such as anxiety and depression are strong predictors of subsequent emotional disorder and are associated with functional impairment and poor long term health and social outcomes [1].
One of the greatest challenges to time trends research is the extent to which trends capture true increases in prevalence over time, or changes in informant-reports of mental health. Some have proposed that increased public awareness and efforts to reduce symptoms has paradoxically contributed towards the rise in reports of symptoms [169]. In particular, the “prevalence inflation hypothesis” argues that improved recognition and more accurate reporting of mental health problems may have led to over-interpretation, whereby individuals label milder and more transient forms of stress as a mental health symptom. It is suggested that this self-diagnosis can result in a self-fulfilling prophecy which in turn drives further awareness efforts [169]. One study testing this possible self-report bias looked at whether self-reported mental health problems vary as a function of changes in public stigma towards mental illness [170]. Self-reports of symptoms were compared in 2009 and 2017–2019, alongside stigma-related indicators at both the regional and national level. The overall prevalence of self-reported mental health problems increased over time, as did variation by region, but at the same time, all indicators of stigma improved. The regions with the greatest improvements to stigma, however, did not correspond to the regions with the largest increases in self-reported symptoms. This does not provide support for the hypothesis that increased awareness efforts may be driving increased reporting of mental health problems. It is important to note that this study used a cross-sectional ecological design, whereby self-reported symptoms and stigma were aggregated at the regional as opposed to individual level. Other evidence also supports the view that increases in youth emotional problems are likely not simply a consequence of greater awareness and openness in reporting of psychopathology. In particular, there is strong evidence for specificity; for example, there has been much increased awareness of neurodevelopmental conditions such as ADHD, but no systematic increase in parent or self-reports of ADHD in epidemiological studies [22]. Similarly, there is also specificity by age, with greater secular increases in emotional problems among adolescents compared to in children [171]. Furthermore, given evidence that long-term increases in emotional problems may be more pronounced for adolescent females than males, it is of interest to consider explanatory factors that have shown more pronounced trends for girls [172]. The current review provides further evidence around several areas where girls appear more affected by changes over time, including increased worries about family relationships, school and exam-related stress, and weight-control behaviours. Further research should continue to explore subgroups who may be at heightened risk, and could include other high risk subgroups like those of sexual minorities or those with chronic physical health conditions.
A final research priority is that studies about trends in youth mental health must be broadened to low and middle income countries (LMIC). The majority of young people globally live in LMICs, and these countries may be particularly affected by rapid social change [173, 174]. However, global coverage of epidemiological data on children’s mental health is limited, and a particularly notable gap concerns opportunities for cross-cohort comparisons in order to examine trends in prevalence of mental health prevalence and their causes in LMIC settings [175]. Almost all the evidence identified in this review is based on children and adolescents from high-income countries. There is also little understanding of potential cultural differences in adolescent development, as well as on differences between societies in prevalence and trends of relevant social risk factors for adolescent emotional problems. There is currently insufficient evidence on links between trends in youth mental health and exposure to a range of traumatic experiences including war, natural disasters, and the HIV/AIDS and other pandemics. Looking to the future, implications of climate change for young people’s lives will likely vary substantially between countries, but there is an absence of data on implications for international differences in trends in youth mental health [176]. More generally, combining opportunities for cross-country and cross-time cohort comparisons provides an invaluable method of identifying potentially causal risks at a population-level particularly where there are differences in trends in purported explanatory factors.
Overall, much more needs to be done to understand how, when, and why youth emotional problems are increasing in order to improve the outlook for children and young people. Preventing further increases and reducing secular trends is not only crucial for children’s current and future mental health, but also for the wider society and global economy.
Data availability
We do not analyse or generate any datasets. Further information about the data that support the findings of this study can be found in the relevant papers.
References
Thapar A, Eyre O, Patel V, Brent D. Depression in young people. Lancet. 2022. https://doi.org/10.1016/S0140-6736(22)01012-1.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–660.
Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27(1):281–95.
Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, Chisholm D, Collins PY, Cooper JL, Eaton J, Herrman H, Herzallah MM, Huang Y, Jordans MJD, Kleinman A, Medina-Mora ME, Morgan E, Niaz U, Omigbodun O, Prince M, et al. The Lancet Commission on global mental health and sustainable development. Lancet (London, England). 2018;392(10157):1553–98.
Collishaw S, Sellers R. Trends in child and adolescent mental health prevalence, outcomes, and inequalities. In: Taylor E, Verhulst F, Wong JCM, Yoshida K, editors. Mental health and illness of children and adolescents. Singapore: Springer Singapore; 2020. p. 63–73. https://doi.org/10.1007/978-981-10-2348-4_9.
Sellers R, Warne N, Pickles A, Maughan B, Thapar A, Collishaw S. Cross-cohort change in adolescent outcomes for children with mental health problems. J Child Psychol Psychiatry. 2019;60(7):813–21.
Blomqvist I, HenjeBlom E, Hägglöf B, Hammarström A. Increase of internalized mental health symptoms among adolescents during the last three decades. Eur J Pub Health. 2019;29:925.
Keyes KM, Gary D, O’Malley PM, Hamilton A, Schulenberg J. Recent increases in depressive symptoms among US adolescents: trends from 1991 to 2018. Soc Psychiatry Psychiatr Epidemiol. 2019;54(8):987–96.
Mishina K, Tiiri E, Lempinen L, Sillanmäki L, Kronström K, Sourander A. Time trends of Finnish adolescents’ mental health and use of alcohol and cigarettes from 1998 to 2014. Eur Child Adolesc Psychiatry. 2018;27:1633–43.
Thorisdottir IE, Asgeirsdottir BB, Sigurvinsdottir R, Allegrante JP, Sigfusdottir ID. The increase in symptoms of anxiety and depressed mood among Icelandic adolescents: time trend between 2006 and 2016. Eur J Pub Health. 2017;27(5):856–61.
Patalay P, Gage SH. Changes in millennial adolescent mental health and health-related behaviours over 10 years: a population cohort comparison study. Int J Epidemiol. 2019;48(5):1650–64.
Jorm AF, Kitchener BA. Increases in youth mental health services in Australia: have they had an impact on youth population mental health? Aust N Z J Psychiatry. 2021;55(5):476–84.
Pitchforth J, Fahy K, Ford T, Wolpert M, Viner RM, Hargreaves DS. Mental health and well-being trends among children and young people in the UK, 1995–2014: analysis of repeated cross-sectional national health surveys. Psychol Med. 2018;49:1275–85.
Vizard T, Sadler K, Ford T, Newlove-Delgado T, McManus S, Marcheselli F, et al. Mental health of children and young people in England. Health Soc Care Inf Centre. 2020; 1–53.
Sawyer MG, Reece CE, Sawyer AC, Johnson SE, Lawrence D. Has the prevalence of child and adolescent mental disorders in Australia changed between 1998 and 2013 to 2014? J Am Acad Child Adolesc Psychiatry. 2018;57(5):343–50.
Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6): e20161878.
Jones E, Mitra AK, Bhuiyan AR. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Environ Res Public Health. 2021;18(5):2470. https://doi.org/10.3390/ijerph18052470.
Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, Kontopantelis E, Webb R, Wessely S, McManus S, Abel KM. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2021;7(10):883–92.
McGorry PD, Mei C, Chanen A, Hodges C, Alvarez-Jimenez M, Killackey E. Designing and scaling up integrated youth mental health care. World Psychiatry. 2022;21:61–76.
Smith DJ, Rutter M. Psychosocial disorders in young people: time trends and their causes. New Jersey: Academia Europaea/John Wiley; 1995.
Hagell A. Changing adolescence: social trends and mental health. Policy Press. 2012.
Rapee RM, Creswell C, Kendall PC, Pine DS, Waters AM. Anxiety disorders in children and adolescents: a summary and overview of the literature. Behav Res Therapy. 2023;168: 104376.
Shinde S, Weiss HA, Varghese B, Khandeparkar P, Pereira B, Sharma A, Gupta R, Ross DA, Patton G, Pate V. Promoting school climate and health outcomes with the SEHER multi-component secondary school intervention in Bihar, India: a cluster-randomised controlled trial. Lancet. 2018;392:2465–77.
Loewen OK, Maximova K, Ekwaru JP, Faught EL, Asbridge M, Ohinmaa A, Veugelers PJ. Lifestyle behavior and mental health in early adolescence. Pediatrics. 2019. https://doi.org/10.1542/peds.2018-3307.
Collishaw S. Annual research review: secular trends in child and adolescent mental health. J Child Psychol Psychiatry. 2015;56(3):370–93.
Moreno-Agostino D, Wu YT, Daskalopoulou C, Hasan MT, Huisman M, Prina M. Global trends in the prevalence and incidence of depression: a systematic review and meta-analysis. J Affect Disord. 2021;281:235–43.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/.
Zeng X, Zhang Y, Kwong JS, Zhang C, Li S, Sun F, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid-based Med. 2015;8(1):2–10.
Bann D, Wright L, Goisis A, Hardy R, Johnson W, Maddock J, et al. Investigating change across time in prevalence or association: the challenges of cross-study comparative research and possible solutions. Discov Soc Sci Health. 2022;2(1):18.
Office for National Statistics. Divorces in England and Wales: 2019. London: The Stationery Office; 2020.
Collishaw S, Goodman R, Pickles A, Maughan B. Modelling the contribution of changes in family life to time trends in adolescent conduct problems. Soc Sci Med. 2007;65(12):2576–87.
Seltzer JA. Family change and changing family demography. Demography. 2019;56:405–26.
Abel KM, Hope H, Swift E, Parisi R, Ashcroft DM, Kosidou K, et al. Prevalence of maternal mental illness among children and adolescents in the UK between 2005 and 2017: a national retrospective cohort analysis. Lancet Public Health. 2019;4(6):e291–300.
Schepman K, Collishaw S, Gardner F. Do changes in parent mental health explain trends in youth emotional problems? Soc Sci Med. 2011;73:293–300.
Tully EC, Iacono WG, McGue M. An adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. Am J Psychiatry. 2008;165(9):1148–54.
Natsuaki MN, Shaw DS, Neiderhiser JM, Ganiban JM, Harold GT, Reiss D, Leve LD. Raised by depressed parents: is it an environmental risk? Clin Child Fam Psychol Rev. 2014;17(4):357–67.
Gilbert R, Kemp A, Thoburn J, Sidebotham P, Radford L, Glaser D, Macmillan HL. Recognising and responding to child maltreatment. Lancet. 2009;373(9658):167–80.
Jaffee SR, Strait LB, Odgers CL. From correlates to causes: can quasi-experimental studies and statistical innovations bring us closer to identifying the causes of antisocial behavior? Psychol Bull. 2012;138(2):272.
Radford L, Corral S, Bradley C, Fisher H, Bassett C, Howat N, Collishaw S. Child abuse and neglect in the UK today. London: NSPCC; 2011.
Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373(9657):68–81. https://doi.org/10.1016/S0140-6736(08)61706-7.
Bentley H, et al. How safe are our children?: an overview of data on adolescent abuse. London: NSPCC; 2020.
Finkelhor D. Trends in adverse childhood experiences (ACEs) in the United States. Child Abuse Negl. 2020;108: 104641.
Degli Esposti M, Humphreys DK, Jenkins BM, Gasparrini A, Pooley S, Eisner M, Bowes L. Long-term trends in child maltreatment in England and Wales, 1858–2016: an observational, time-series analysis. Lancet Public Health. 2019;4(3):e148–58.
Gilbert R, Fluke J, O’Donnell M, Gonzalez-Izquierdo A, Brownell M, Gulliver P, Janson S, Sidebotham P. Child maltreatment: variation in trends and policies in six developed countries. Lancet. 2012;379(9817):758–72. https://doi.org/10.1016/S0140-6736(11)61087-8.
Degli Esposti M, Taylor J, Humphreys DK, Bowes L. iCoverT: A rich data source on the incidence of child maltreatment over time in England and Wales. PLoS ONE. 2018;13(8): e0201223.
Frøyland LR, von Soest T. Trends in the perpetration of physical aggression among Norwegian adolescents 2007–2015. J Youth Adolesc. 2018;47(9):1938–51.
Marazziti D, Avella MT, Mucci N, Della Vecchia A, Ivaldi T, Palermo S, Mucci F. Impact of economic crisis on mental health: a 10-year challenge. CNS Spectr. 2021;26(1):7–13.
Schenck-Fontaine A, Pines-Gassman A. Income inequality and child maltreatment risk during economic recession. Child Youth Serv Rev. 2020;112: 104926.
Marmot M. Health equity in England: the Marmot review 10 years on. BMJ. 2020;368: m693. https://doi.org/10.1136/bmj.m693.
Conrad-Hiebner A, Byram E. The temporal impact of economic insecurity on child maltreatment: a systematic review. Trauma Violence Abuse. 2020;21(1):157–78.
Schenck-Fontaine A, Gassman-Pines A. Income inequality and child maltreatment risk during economic recession. Child Youth Serv Rev. 2020;112: 104926.
Schneider W, Waldfogel J, Brooks-Gunn J. The Great Recession and risk for child abuse and neglect. Child Youth Serv Rev. 2017;72:71–81.
Long M, Huang J, Peng Y, Mai Y, Yuan X, Yang X. The short-and long-term impact of CoViD-19 lockdown on child maltreatment. Int J Environ Res Public Health. 2022;19(6):3350.
Loiseau M, Cottenet J, Bechraoui-Quantin S, Gilard-Pioc S, Mikaeloff Y, Jollant F, et al. Physical abuse of young children during the COVID-19 pandemic: alarming increase in the relative frequency of hospitalizations during the lockdown period. Child Abuse Neglect. 2021;122: 105299.
Lawson M, Piel MH, Simon M. Child maltreatment during the COVID-19 pandemic: consequences of parental job loss on psychological and physical abuse towards children. Child Abuse Negl. 2020;110: 104709.
Sari NP, van IJzendoorn MH, Jansen P, Bakermans-Kranenburg M, Riem MM. Higher levels of harsh parenting during the COVID-19 lockdown in the Netherlands. Child Maltreat. 2021;10775595211024748.
Vermeulen S, Alink LR, van Berkel SR. Child maltreatment during school and childcare closure due to the CoViD-19 pandemic. Child Maltreat. 2022;10775595211064885
Metcalf S, Marlow JA, Rood CJ, Hilado MA, DeRidder CA, Quas JA. Identification and incidence of child maltreatment during the covid-19 pandemic. Psychol Public Policy Law. 2022;28(2):267–79. https://doi.org/10.1037/law0000352.
Rapp A, Fall G, Radomsky AC, Santarossa S. Child maltreatment during the CoViD-19 pandemic: a systematic rapid review. Pediatr Clin. 2021;68(5):991–1009.
Kim YJ, Moon SS, Kim YK, Boyas J. Protective factors of suicide: religiosity and parental monitoring. Child Youth Serv Rev. 2020;114: 105073.
Yap MBH, Pilkington PD, Ryan SM, Jorm AF. Parental factors associated with depression and anxiety in young people: a systematic review and meta-analysis. J Affect Disord. 2014;156:8–23.
Gardner F, Collishaw S, Maughan B, Scott J, Schepman K, Hagell A. Trends in parenting: can they help explain time trends in problem behaviour. Changing Adolesc Soc Trends Mental Health. 2012;75–91.
Gauthier AH, Smeeding TM, Furstenberg FF Jr. Are parents investing less time in children? Trends in selected industrialized countries. Popul Dev Rev. 2004;30(4):647–72.
Sayer LC, Bianchi SM, Robinson JP. Are parents investing less in children? Trends in mothers’ and fathers’ time with children. Am J Sociol. 2004;110(1):1–43.
Vokáčová J, Badura P, Pavelka J, Kalman M, Hanus R. Brief report: changes in parent–adolescent joint activities between 2002 and 2014 in the Czech Republic, Health Behaviour in School-aged Children (HBSC) study. J Adolesc. 2016;51:1–5.
Walton K, Kleinman KP, Rifas-Shiman SL, Horton NJ, Gillman MW, Field AE, et al. Secular trends in family dinner frequency among adolescents. BMC Res Notes. 2016;9(1):1–5.
Clark T, Fleming T, Bullen P, Crengle S, Denny S, Dyson B, et al. Health and well-being of secondary school students in New Zealand: trends between 2001, 2007 and 2012. J Paediatr Child Health. 2013;49(11):925–34.
Fleming TM, Clark T, Denny S, Bullen P, Crengle S, Peiris-John R, et al. Stability and change in the mental health of New Zealand secondary school students 2007–2012: results from the national adolescent health surveys. Aust N Z J Psychiatry. 2014;48(5):472–80.
Lewycka S, Clark T, Peiris-John R, Fenaughty J, Bullen P, Denny S, Fleming T. Downwards trends in adolescent risk-taking behaviours in New Zealand: exploring driving forces for change. J Paediatr Child Health. 2018;54(6):602–8.
Brooks F, Zaborskis A, Tabak I, CarmenGranadoAlcón MD, Zemaitiene N, de Roos S, Klemera E. Trends in adolescents’ perceived parental communication across 32 countries in Europe and North America from 2002 to 2010. Eur J Public Health. 2015;25(suppl_2):46–50.
Vokáčová J, Vašíčková J, Hodačová L, Půžová Z, Tabak I. Trends in parent-adolescent communication in the Czech Republic between 2002 and 2014: results of the HBSC Study. Cent Eur J Public Health. 2017;25(Supplement 1):S36–41.
Collishaw S, Gardner F, Maughan B, Scott J, Pickles A. Do historical changes in parent-child relationships explain increases in youth conduct problems? J Abnorm Child Psychol. 2012;40:119–32.
Larm P, Livingston M, Svensson J, Leifman H, Raninen J. The increased trend of non-drinking in adolescence: the role of parental monitoring and attitudes toward offspring drinking. Drug Alcohol Rev. 2018;37:S34–41.
De Looze ME, van Dorsselaer SA, Monshouwer K, Vollebergh WA. Trends in adolescent alcohol use in the Netherlands, 1992–2015: differences across sociodemographic groups and links with strict parental rule-setting. Int J Drug Policy. 2017;50:90–101.
Sweeting H, West P, Young R, Der G. Can we explain increases in young people’s psychological distress over time? Soc Sci Med. 2010;71(10):1819–30.
De Looze ME, Cosma AP, Vollebergh WAM, Duinhof EL, de Roos SA, van Dorsselaer S, von Bon-Martens MJH, Vonk R, Stevens GWJM. Trends over time in adolescent emotional wellbeing in the Netherlands, 2005–2017: links with perceived schoolwork pressure, parent-adolescent communication and bullying victimization. J Youth Adolesc. 2020;49:2124–35.
Harold GT, Sellers R. Annual research review: Interparental conflict and youth psychopathology: an evidence review and practice focused update. J Child Psychol Psychiatry. 2018;59(4):374–402.
Medel-Herrero A, Shumway M, Smiley-Jewell S, Bonomi A, Reidy D. The impact of the Great Recession on California domestic violence events, and related hospitalizations and emergency service visits. Prev Med. 2020;139: 106186.
Piquero AR, Jennings WG, Jemison E, Kaukinen C, Knaul FM. Domestic violence during the COVID-19 pandemic—evidence from a systematic review and meta-analysis. J Crim Just. 2021;74: 101806.
Neumark-Sztainer D, Wall M, Fulkerson JA, Larson N. Changes in the frequency of family meals from 1999 to 2010 in the homes of adolescents: trends by sociodemographic characteristics. J Adolesc Health. 2013;52(2):201–6.
Prickett KC, Augustine JM. Trends in mothers’ parenting time by education and work from 2003 to 2017. Demography. 2021;58(3):1065–91.
Collishaw S, Furzer E, Thapar AK, Sellers R. Brief report: a comparison of child mental health inequalities in three UK population cohorts. Eur Child Adolesc Psychiatry. 2019;28(11):1547–9.
Manger S. Lifestyle interventions for mental health. Aust J Gener Pract. 2019;48(10):670–3.
Marino C, Andrade B, Campisi SC, Wong M, Zhao H, Jing X, et al. Association between disturbed sleep and depression in children and youths: a systematic review and meta-analysis of cohort studies. JAMA Netw Open. 2021;4(3):e212373–e212373.
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–3.
Twenge JM, Krizan Z, Hisler G. Decreases in self-reported sleep duration among U.S. adolescents 2009–2015 and association with new media screen time. Sleep Med. 2017;39:47–53. https://doi.org/10.1016/j.sleep.2017.08.013.
Ghekiere A, Van Cauwenberg J, Vandendriessche A, Inchley J, Gaspar de Matos M, Borraccino A, et al. Trends in sleeping difficulties among European adolescents: are these associated with physical inactivity and excessive screen time? Int J Public Health. 2019;64(4):487–98.
Cole AG, Laxer RE, Patte KA, Leatherdale ST. Can we reverse this trend? Exploring health and risk behaviours of grade 12 cohorts of Ontario students from 2013–2019. Int J Environ Res Public Health. 2021;18(6):3109.
Wheaton AG, Claussen AH. Short sleep duration among infants, children, and adolescents aged 4 months–17 years—United States, 2016–2018. MMWR Morbid Mortal Wkly Rep. 2021;70(38):1315–21. https://doi.org/10.15585/mmwr.mm7038a1.
Keyes KM, Maslowsky J, Hamilton A, Schulenberg J. The great sleep recession: changes in sleep duration among US adolescents, 1991–2012. Pediatrics. 2015;135(3):460–8.
Williams PG, Cribbet MR, Rau HK, Gunn HE, Czajkowski LA. The effects of poor sleep on cognitive, affective, and physiological responses to a laboratory stressor. Ann Behav Med. 2013;46(1):40–51.
Otsuka Y, Kaneita Y, Spira AP, Mojtabai R, Itani O, Jike M, et al. Trends in sleep problems and patterns among Japanese adolescents: 2004 to 2017. Lancet Reg Health West Pac. 2021;9: 100107.
Matricciani L, Olds T, Petkov J. In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev. 2012;16(3):203–11.
Wiens K, Bhattarai A, Pedram P, Dores A, Williams J, Bulloch A, Patten S. A growing need for youth mental health services in Canada: examining trends in youth mental health from 2011 to 2018. Epidemiol Psychiatr Sci. 2020. https://doi.org/10.1017/S2045796020000281.
Ma C, Xi B, Li Z, Wu H, Zhao M, Liang Y, Bovet P. Prevalence and trends in tobacco use among adolescents aged 13–15 years in 143 countries, 1999–2018: findings from the Global Youth Tobacco Surveys. Lancet Child Adolesc Health. 2021;5(4):245–55.
Vashishtha R, Pennay A, Dietze P, Marzan MB, Room R, Livingston M. Trends in adolescent drinking across 39 high-income countries: exploring the timing and magnitude of decline. Eur J Pub Health. 2021;31(2):424–31.
Hall W, Leung J, Lynskey M. The effects of cannabis use on the development of adolescents and young adults. Annu Rev Dev Psychol. 2020;2:461–83.
Miech R, Johnston L, O’Malley PM, Bachman JG, Patrick ME. Trends in adolescent vaping, 2017–2019. N Engl J Med. 2019;381(15):1490–1.
Inchley J, Currie D, Vieno A, Torsheim T, Ferreira-Borges C, Weber MM et al. Adolescent alcohol-related behaviours: trends and inequalities in the WHO European Region, 2002–2014: observations from the Health Behaviour in School-aged Children (HBSC) WHO collaborative cross-national study. World Health Organization. Regional Office for Europe. 2018.
Carvalho AF, Heilig M, Perez A, Probst C, Rehm J. Alcohol use disorders. Lancet. 2019;394(10200):781–92.
Johnston L, Miech R, O'Malley P, Bachman J, Schulenberg J, Patrick M. Monitoring the future: national survey results on drug use 1975-2019: overview, key findings on adolescent drug use. Institute for Social Research. University of Michigan 2019. 2020.
Page N, Hallingberg B, Brown R, Lowthian E, Hewitt G, Murphy S, Moore G. Change over time in adolescent smoking, cannabis use, and their association: findings from the School Health Research Network in Wales. J Public Health. 2021;43(4):e620–8.
Wilson J, Freeman TP, Mackie CJ. Effects of increasing cannabis potency on adolescent health. Lancet Child Adolesc Health. 2019;3(2):121–8.
Hines LA, Freeman TP, Gage SH, Zammit S, Hickman M, Cannon M, et al. Association of high-potency cannabis use with mental health and substance use in adolescence. JAMA Psychiat. 2020;77(10):1044–51.
Gage SH, Patalay P. Associations between adolescent mental health and health-related behaviors in 2005 and 2015: a population cross-cohort study. J Adolesc Health. 2021;69(4):588–96.
Mishina K, Tiiri E, Lempinen L, Sillanmäki L, Kronström K, Sourander A. Time trends of Finnish adolescents’ mental health and use of alcohol and cigarettes from 1998 to 2014. Eur Child Adolesc Psychiatry. 2018;27(12):1633–43.
von Soest T, Wichstrom L. Secular trends in depressive symptoms among Norwegian adolescents from 1992 to 2010. J Abnorm Child Psychol. 2014;42:403–15.
Jokela M, García-Velázquez R, Gluschkoff K, Airaksinen J, Rosenström T. Health behaviors and psychological distress: changing associations between 1997 and 2016 in the United States. Soc Psychiatry Psychiatr Epidemiol. 2020;55:385–91.
Sellers R, Warne N, Rice F, Langley K, Maughan B, Pickles A, et al. Using a cross-cohort comparison design to test the role of maternal smoking in pregnancy in child mental health and learning: evidence from two UK cohorts born four decades apart. Int J Epidemiol. 2020;49(2):390–9.
Chaput JP, Willumsen J, Bull F, Chou R, Ekelund U, Firth J, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int J Behav Nutr Physical Act. 2020;17:1–9.
Inchley J, Currie D, Jewell J, Breda J, Barnekow V. Adolescent obesity and related behaviours: trends and inequalities in the WHO European Region, 2002–2014: observations from the Health Behaviour in School-aged Children (HBSC) WHO collaborative cross-national study. World Health Organization. Regional Office for Europe. 2017.
Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1· 6 million participants. Lancet Child Adolesc Health. 2020;4(1):23–35.
Bellón JÁ, Conejo-Cerón S, Sánchez-Calderón A, Rodríguez-Martín B, Bellón D, Rodríguez-Sánchez E, et al. Effectiveness of exercise-based interventions in reducing depressive symptoms in people without clinical depression: systematic review and meta-analysis of randomised controlled trials. Br J Psychiatry. 2021;219(5):578–87.
Chaplin AB, Daniels NF, Ples D, Anderson RZ, Gregory-Jones A, Jones PB, Khandaker GM. Longitudinal association between cardiovascular risk factors and depression in young people: a systematic review and meta-analysis of cohort studies. Psychol Med. 2021. https://doi.org/10.1017/S0033291721002488.
US Department of Health and Human Services. Physical activity guidelines advisory committee. 2018 physical activity guidelines advisory committee scientific report. Published online. 2018.
Roman-Juan J, Roy R, Jensen MP, Miró J. The explanatory role of sedentary screen time and obesity in the increase of chronic back pain amongst European adolescents: The HBSC study 2002–2014. Eur J Pain. 2022;26(8):1781–9.
Twenge JM. Increases in depression, self-harm, and suicide among US adolescents after 2012 and links to technology use: possible mechanisms. Psychiatr Res Clin Pract. 2020;2(1):19–25.
Fühner T, Kliegl R, Arntz F, Kriemler S, Granacher U. An update on secular trends in physical fitness of children and adolescents from 1972 to 2015: a systematic review. Sports Med. 2021;51:303–20.
Eberhardt T, Niessner C, Oriwol D, Buchal L, Worth A, Bös K. Secular trends in physical fitness of children and adolescents: a review of large-scale epidemiological studies published after 2006. Int J Environ Res Public Health. 2020;17(16):5671.
Dzielska A, Kelly C, Ojala K, Finne E, Spinelli A, Furstova J, Fismen AS, Ercan O, Tesler R, Melkumova M, Canale N, Nardone P, Gudelj Rakic J, Dalmasso P. Weight reduction behaviors among European adolescents-changes from 2001/2002 to 2017/2018. J Adolesc Health. 2020;66(6S):S70–80. https://doi.org/10.1016/j.jadohealth.2020.03.008.
Solmi F, Sharpe H, Gage SH, Maddock J, Lewis G, Patalay P. Changes in the prevalence and correlates of weight-control behaviors and weight perception in adolescents in the UK, 1986–2015. JAMA Pediatr. 2021;175(3):267–75.
Wu J, Liu J, Li S, Ma H, Wang Y. Trends in the prevalence and disability-adjusted life years of eating disorders from 1990 to 2017: results from the Global Burden of Disease Study 2017. Epidemiol Psychiatr Sci. 2020;29:E191. https://doi.org/10.1017/S2045796020001055.
Kelly Y, Zilanawala A, Booker C, Sacker A. Social media use and adolescent mental health: findings from the UK millennium cohort study. EClinicalMedicine. 2018;6:59–68.
Twenge JM, Campbell WK. Media use is linked to lower psychological well-being: evidence from three datasets. Psychiatr Q. 2019;90(2):311–31.
Orben A, Przybylski AK. The association between adolescent well-being and digital technology use. Nat Hum Behav. 2019;3(2):173–82.
Twenge JM, Haidt J, Joiner TE, Campbell WK. Underestimating digital media harm. Nat Hum Behav. 2020;4(4):346–8.
Orben A, Przybylski AK, Blakemore SJ, Kievit RA. Windows of developmental sensitivity to social media. Nat Commun. 2022;13(1):1649.
Metherell TE, Ghai S, McCormick EM, Ford TJ, Orben A. Digital access constraints predict worse mental health among adolescents during COVID-19. Sci Rep. 2022;12:19088. https://doi.org/10.1038/s41598-022-23899-y.
Tåhlin M, Westerman J. Youth employment decline and the structural change of skill. Eur Soc. 2020;22(1):47–76.
Högberg B. Educational stressors and secular trends in school stress and mental health problems in adolescents. Soc Sci Med. 2021;270: 113616.
Department for Education. Primary assessment and accountability under the new national curriculum. 2013. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/298568/Primary_assessment_and_accountability_under_the_new_curriculum_consultation_document.pdf
Bersia M, Berchialla P, Charrier L, Lemma P, Borraccino A, Nardone P, Pierannunzio D, Ciardullo S, Comoretto RI, Dalmasso P. Mental well-being: 2010–2018 trends among ITALIAN adolescents. Int J Environ Res Public Health. 2022;19(2):863.
Cosma A, Stevens GWJM, Vollebergh WAM, De Looze M. Time trends in schoolwork pressure among Dutch adolescents, 2001–2017: gender and educational differences. Scand J Public Health. 2022. https://doi.org/10.1177/14034948211018388.
Högberg B, Lindgren J, Johansson K, Strandh M, Petersen S. Consequences of school grading systems on adolescent health: evidence from a Swedish school reform. J Educ Policy. 2021;36(1):84–106.
Read S, Hietajärvi L, Salmela-Aro K. School burnout trends and sociodemographic factors in Finland 2006–2019. Soc Psychiatry Psychiatr Epidemiol. 2022;57(8):1659–69.
Löfstedt P, García-Moya I, Corell M, Paniagua C, Samdal O, Välimaa R, Lyyra N, Currie D, Rasmussen M. School satisfaction and school pressure in the WHO European region and north America: an analysis of time trends (2002–2018) and patterns of co-occurrence in 32 countries. J Adolesc Health. 2020;66(6S):S59–69.
Cosma A, Stevens G, Martin G, Duinhof EL, Walsh SD, Garcia-Moya I, Kӧlt ̋o A, Gobina I, Canale N, Catunda C, Inchley J, de Looze M. Cross-national time trends in adolescent mental well-being from 2002 to 2018 and the explanatory role of schoolwork pressure. J Adolesc Health. 2022;66(6S), S50–S58.
Högberg B, Strandh M, Hagquist C. Gender and secular trends in adolescent mental health over 24 years—the role of school-related stress. Soc Sci Med. 2020;250: 112890.
West P, Sweeting H. Fifteen, female and stressed: changing patterns of psychological distress over time. J Child Psychol Psychiatry. 2003;44(3):399–411.
Högberg B, Lindgren J. From a crisis of results to a crisis of wellbeing—education reform and the declining sense of school belonging in Sweden. Comp Educ. 2022;59:18–37.
Högberg B, Petersen S, Strandh M, Johansson K. Determinants of declining school belonging 2000–2018: the Case of Sweden. Soc Indic Res. 2021;157:783–802.
Moore GF, Cox R, Evans RE, Hallingberg B, Hawkins J, Littlecott HJ, Long SJ, Murphy S. School, peer and family relationships and adolescent substance use, subjective wellbeing and mental health symptoms in Wales: a cross sectional study. Child Indic Res. 2018;11:1951–65.
Armitage JM, Wang RAH, Davis OSP, Bowes L, Haworth CMA. Peer victimisation during adolescence and its impact on wellbeing in adulthood: a prospective cohort study. BMC Public Health. 2021;21:148. https://doi.org/10.1186/s12889-021-10198-w.
Collishaw S, Hammerton G, Mahedy L, Sellers R, Owen MJ, Craddock N, Thapar AK, Harold GT, Rice F, Thapar A. Mental health resilience in the adolescent offspring of parents with depression: a prospective longitudinal study. Lancet Psychiatry. 2016;3(1):49–57.
Verdery A, Campbell C. Social support in America: stratification and trends in access over two decades. Soc Forces. 2019;98(2):725–52.
Cosma A, Walsh SD, Chester KL, Callaghan M, Molcho M, Craig W, Pickett W. Bullying victimization: time trends and the overlap between traditional and cyberbullying across countries in Europe and North America. Int J Public Health. 2020;65:75–85.
Teuton J. Social isolation and loneliness in Scotland: a review of prevalence and trends. Edinburgh: NHS Health Scotland; 2018.
Källmén H, Hallgren M. Bullying at school and mental health problems among adolescents: a repeated cross-sectional study. Child Adolesc Psychiatry Ment Health. 2021. https://doi.org/10.1186/s13034-021-00425-y.
Gaffney H, Ttofi MM, Farrington DP. Effectiveness of school-based programs to reduce bullying perpetration and victimization: an updated systematic review and meta-analysis. Campbell Syst Rev. 2021;17(2): e1143.
Waasdorp TE, Pas ET, Zablotsky B, Bradshaw CP. Trends in bullying and related attitudes among 4th- to 12-graders. Pediatrics. 2017;139(6):e2016–615.
Kennedy RS. Bullying trends in the United States: a meta-regression. Trauma Violence Abuse. 2021;22(4):914–27.
Trompeter N, Jackson E, Sheanoda V, Luo A, Allison K, Bussey K. Cyberbullying prevalence in Australian adolescents: time trends 2015–2020. J Sch Violence. 2022;21(3):252–65.
Patchin JW, Hinduja, S. Cyberbullying statistics 2021 age, gender, sexual orientation, and race. Cyberbullying Research Center (cyberbullying.org). 2021.
Twenge J, Spitzberg BH, Campbell K. Less in-person social interaction with peers among US adolescents in the 21st century and links to loneliness. J Soc Pers Relationsh. 2019;36(6):1892–913.
Twenge JM, Joiner TE, Rogers ML, Martin GN. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clin Psychol Sci. 2018;6(1):3–17.
Twenge JM, Haidt J, Blake AB, McAllister C, Lemon H, Le Roy A. Worldwide increases in adolescent loneliness. J Adolesc. 2021;93:257–69.
Madsen KR, Holstein BE, Damsgaard MT, Rayce SB, Jespersen LN, Due P. Trends in social inequality in loneliness among adolescents 1991–2014. J Public Health. 2019;41(2):e133–40.
Mitchell KJ, Wolak J, Finkelhor D. Trends in youth reports of sexual solicitations, harassment and unwanted exposure to pornography on the Internet. J Adolesc Health. 2007;40(2):116–26.
Ridley M, Rao G, Schilbach F, Patel V. Poverty, depression, and anxiety: causal evidence and mechanisms. Science. 2020;370(6522): eaay0214. https://doi.org/10.1126/science.aay0214.
Victora CG, Hartwig FP, Vidaletti LP, Martorell R, Osmond C, Richter LM, Stein AD, Barros AJ, Adair LS, Barros FC, Bhargava SK. Effects of early-life poverty on health and human capital in children and adolescents: analyses of national surveys and birth cohort studies in LMICs. Lancet. 2022;399(10336):1741–52.
Torikka A, Kaltiala-Heino R, Rimpelä A, et al. Self-reported depression is increasing among socio-economically disadvantaged adolescents—repeated cross-sectional surveys from Finland from 2000 to 2011. BMC Public Health. 2014;14:408.
Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, Bergeron A, Cutler D. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315(16):1750–66.
Broadbent P, Thomson R, Kopasker D, McCartney G, Meier P, Richiardi M, McKee M, et al. The public health implications of the cost-of-living crisis: outlining mechanisms and modelling consequences. Lancet Reg Health Europe. 2023. https://doi.org/10.1016/j.lanepe.2023.100585.
McElroy E, Tibber M, Fearon P, Patalay P, Ploubidis GB. Socioeconomic and sex inequalities in parent-reported adolescent mental ill-health: time trends in four British birth cohorts. J Child Psychol Psychiatry. 2022. https://doi.org/10.1111/jcpp.13730.
Eckersley R. Is modern Western culture a health hazard? Int J Epidemiol. 2006;35(2):252–8.
Russell S, Fish J. Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annu Rev Clin Psychol. 2016;12:465–87.
Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. 2016;387(10024):1240–50.
Foulkes L, Andrews JL. Are mental health awareness efforts contributing to the rise in reported mental health problems? A call to test the prevalence inflation hypothesis. New Ideas Psychol. 2023;69: 101010.
Gagné T, Henderson C, McMunn A. Is the self-reporting of mental health problems sensitive to public stigma towards mental illness? A comparison of time trends across English regions (2009–19). Soc Psychiatry Psychiatr Epidemiol. 2022; 1–10.
Armitage JM, Kwong ASF, Tseliou F, Sellers R, Blakey R, Anthony R, Rice F, Thapar A, Collishaw S. Cross-cohort change in parent-reported emotional problem trajectories across childhood and adolescence in the UK. Lancet Psychiatry. 2023;10(7):509–17.
Keyes KM, Platt JM. Annual research review: sex, gender, and internalizing conditions among adolescents in the 21st Century—trends, causes, consequences. J Child Psychol Psychiatry. 2023. https://doi.org/10.1111/jcpp.13864.
Patton GC, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387:2423–78.
Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, Chisholm D, Collins PY, Cooper JL, Eaton J, Herrman H, Herzallah MM, Huang Y, Jordans MJD, Kleinman A, Medina-Mora ME, Morgan E, Niaz U, Omigbodun O, Prince M, et al. The Lancet Commission on global mental health and sustainable development. Lancet. 2018;392(10157):1553–98.
Erskine HE, Baxter AJ, Patton G, Moffitt TE, Patel V, Whiteford HA, Scott JG. The global coverage of prevalence data for mental disorders in children and adolescents. Epidemiol Psychiatric Sci. 2017;26(4):395–402.
Charlson F, Ali S, Benmarhnia T, Pearl M, Massazza A, Augustinavicius J, Scott JG. Climate change and mental health: a scoping review. Int J Environ Res Public Health. 2021;18(9):4486.
Funding
Wolfson Centre for Young People’s Mental Health, Wolfson Foundation, and the Rudd Family Foundation.
Author information
Authors and Affiliations
Contributions
JMA, RS and SC each wrote a section of the first draft. JA drafted the introduction and concluding paragraphs with subsequent input from RS and SC. All authors reviewed the manuscript and contributed to editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Armitage, J.M., Collishaw, S. & Sellers, R. Explaining long-term trends in adolescent emotional problems: what we know from population-based studies. Discov Soc Sci Health 4, 14 (2024). https://doi.org/10.1007/s44155-024-00076-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44155-024-00076-2