Abstract
Objectives
Smoking rates have declined with a slower pace among those with psychological distress compared to those without. We examined whether other health behaviors (heavy alcohol consumption, physical inactivity, short sleep duration) showed similar trends associated with psychological distress. We also examined differences by age and birth cohort.
Methods
Data were from the annually repeated cross-sectional U.S. National Health Interview Surveys (NHIS) of 1997–2016 (total n = 603,518). Psychological distress was assessed with the 6-item Kessler Psychological Distress Scale (K6).
Results
Psychological distress became more strongly associated with smoking (OR 1.09 per 10 years; 95% CI 1.07, 1.12), physical inactivity (OR 1.08; 1.05, 1.11), and short sleep (OR 1.12; 1.06, 1.18), but less strongly associated with heavy alcohol consumption (OR 0.93; 0.89, 0.98). The associations of smoking and alcohol consumption attenuated with age, whereas the association with physical inactivity strengthened with age. Compared to older birth cohorts, smoking became more strongly associated with psychological distress among younger birth cohorts up to those born in the 1980s.
Conclusions
The strength of associations between psychological distress and health behaviors may vary by time period, age, and birth cohort.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mental disorders are associated with poor physical health and reduced life expectancy [1]. This is partially due to poor health behaviors; mentally distressed individuals are more likely to engage in unhealthy behaviors, such as smoking [2], risky alcohol consumption [3, 4], physical inactivity [5], and short sleep duration [6, 7]. Poor health behaviors, in turn, increase the risk of comorbid physical conditions and early mortality [8].
In the general population, mental health is often measured by indicators of non-specific psychological distress, including symptoms of depression, anxiety, stress, and somatic complaints [9]. Studies in the United States [10,11,12,13] and the United Kingdom [14] have reported psychological distress to be associated with diverging trends in smoking. During the last 10–20 years, smoking rates have declined among those without mental disorders but have remained the same, or declined at a slower pace, among those with mental disorders [10, 14]. These trends suggest that health policies aimed at reducing smoking have not been effective for psychologically distressed individuals, which has led to an increasingly widening health disparity between those with and without mental disorders [10].
Smoking is only one of the important health behaviors; short sleep duration, heavy alcohol consumption, and physical inactivity are among the other health behaviors that are associated with increased morbidity and mortality [8]. The overall population trends in the United States have shown increasing levels of short sleep duration [15] and steady (or slightly increasing) levels of heavy alcohol consumption [16, 17]. The prevalence of physical inactivity in the United States remained quite stable between 1997 and 2007 but has decreased between 2007 and 2016 [18]. Similar to smoking, these health behavior trends might have developed differently among individuals with and without psychological distress. However, it is unknown whether the time trends associated with smoking represents broader patterns in the associations of psychological distress with health behaviors, or whether the time trends are specific to smoking.
Using multiple cross-sectional surveys from the U.S. National Health Interview Surveys (NHIS) between 1997 and 2016, we examined whether the associations between psychological distress and four unhealthy behaviors (smoking, heavy alcohol consumption, physical inactivity, and short sleep duration) changed during this time period, and whether there were age differences in these associations. We also explored potential birth cohort effects using cross-classified random-effects multilevel regressions [19]. However, it is still debated whether any statistical method can reliably separate the contributions of time period, age, and birth cohort [20]. We therefore present the analysis of birth cohort effects only as a supplementary analysis, with the main focus on time period changes that are of primary interest from the perspective of public health.
Materials and methods
Data were from the annual U.S. National Health Interview Surveys (NHIS) of 1997–2016. The total sample size was 603,518 participants (21,237–35,469 participants per survey year) aged 18 years and older. These data have previously been used to examine time period trends in psychological distress and smoking [11, 13]. NHIS is approved by the Research Ethics Review Board of the National Center for Health Statistics and the U.S. Office of Management and Budget. All NHIS respondents provided oral consent prior to participation.
Psychological distress was assessed using the 6-item Kessler Psychological Distress Scale (K6) [9] with the items asking about frequency of experiencing the symptoms in the past 30 days, rated on a 5-point Likert scale (0 = none of the time, 4 = all the time). The six items were summed together, and higher values indicated higher psychological distress. Detailed wordings of the health behavior questions are reported in the supplementary material. Smoking status was based on a question on whether the participant was currently smoking or not. Physical inactivity was assessed with questions on the frequency of moderate and vigorous physical activities lasting at least 10 min, and physical inactivity was determined as not participating in at least weekly moderate or vigorous leisure-time aerobic activity lasting at least 10 min (versus more than 10 min of either types of leisure-time activity). Heavy alcohol consumption was assessed with two questions (frequency of drinking and average number of drinks when drinking), and heavy alcohol consumption defined as drinking more than 7 alcohol units per week for women and more than 14 units for men (versus those drinking less or not at all). Short sleep duration was assessed with one question (average number of sleep hours), and short sleep duration was defined as 6 h or less (versus 7–9 h of sleep); given that long sleep duration has also been associated with poor health [21], for the analysis of sleep duration we excluded participants who reported sleep duration of 10 h or more. Questions on sleep duration were administered from 2004 onwards, so the time period for sleep duration spanned from 2004 to 2016. Age was categorized into 5-year intervals (youngest age group 18–19, oldest ≥ 85), and both age and time period were used as categorical variables to allow the associations to follow non-linear patterns.
Statistical analysis
When assessing age patterns, we fitted logistic regression models with age (as dummy-coded variable), sex (0 = men, 1 = women), race/ethnicity (0 = non-Hispanic White, 1 = Black, 2 = Hispanic, 3 = other), psychological distress, and the interaction effect between age and psychological distress as predictor variables. When assessing time period effects, age was modeled with linear and quadratic terms (and their interaction effects with psychological distress), and time period and its interaction effects with psychological distress as categorical variables. We used the K6 scale as a continuous variable in order not to lose information with categorization. The K6 scale is sometimes used as a categorical variable, with a cutoff score of ≥ 5 indicating at least moderate psychological distress and ≥ 13 indicating serious psychological distress [22]. We rescaled the continuous K6 scale by first determining the average K6 scores in the groups with no psychological distress (i.e., K6 < 5, average score 0.9) and at least moderate psychological distress (i.e., K6 ≥ 5, average score 9.2), and then divided the original K6 score with the difference between these scores (i.e., by 8.3). This way the odds ratios we report represent the average difference between those with and without at least moderate psychological distress, because a one-unit difference corresponds to an 8.3-point difference on the original K6 scale. The prevalences of health behaviors were calculated for these scores of the K6 scale (i.e., 0.9 vs 9.2) to illustrate the health behavior trends by levels of psychological distress. The rescaling did not influence the relative ranking of the participants on the K6 scale, and the results would have been substantially the same with a categorical K6 variable (data not shown). All logistic regression models were fitted using sampling weights.
Results
The mean age of the participants was 47.5 years (standard deviation = 18.0), 56.0% were women, 66.7% were non-Hispanic white, 14.3% Black, and 13.9% Hispanic. Smoking and physical inactivity decreased over time, short sleep duration increased slightly, and psychological distress and alcohol consumption remained fairly stable (Table 1).
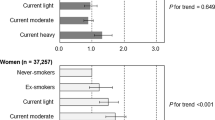
Figure 1 shows the odds ratios for psychological distress associated with health behaviors in different years with linear trends fitted through the estimates (the quadratic trends were not significant for any of the health behaviors). Between 1997 and 2016, psychological distress became more strongly associated with smoking (linear trend OR 1.09 per 10 years, 95% CI 1.07, 1.12; corresponding to an increase from OR = 2.02 in 1997 to OR 2.39 in 2016) and physical inactivity (linear trend OR 1.08 per 10 years, 95% CI 1.05, 1.11; corresponding to an increase from OR 1.24 in 1997 to OR 1.44 in 2016) but less strongly associated with heavy alcohol consumption (linear trend OR 0.94 per 10 years, 95% CI 0.89, 0.98; corresponding to a decrease from OR 1.76 in 1997 to OR 1.54 in 2016). Between 2004 and 2016, the association with short sleep duration also became stronger (linear trend OR 1.12 per 10 years, 95% CI 1.06, 1.18; corresponding to an increase from OR 2.13 in 2004 to OR 2.43 in 2016). Figure 2 shows the population prevalences of health behaviors by study year and level of psychological distress, as derived from the logistic regression models.
Associations of psychological distress with health behaviors by study year. The values are odds ratios (and 95% confidence intervals) per 8.3 points of the continuous K6 scale (average difference between people with no vs at least moderate psychological distress) that were derived from the logistic regression models, adjusted for sex, age, and race/ethnicity (n = 603,518). The linear trends are fitted to the odds ratio estimates, weighted by the inverse of the standard error of the estimates
Population prevalences of health behaviors by study year and levels of psychological distress (no versus at least moderate psychological distress). Values are proportions derived from logistic regression models, adjusted for sex, age, and race/ethnicity. Black circles are for participants with at least moderate psychological distress, while white circles are for participants with no psychological distress. The linear trends are fitted by weighting the points by the inverse of the standard error of the estimates. Note the differences in y-axis ranges
Figure 3 shows the strength of associations between psychological distress and health behaviors by age (see Supplementary Table 1 for the parameter estimate details for age groups). The association of psychological distress with smoking decreased from over OR 2.0 before age 40 to OR 1.2 at age 80. The association with heavy alcohol consumption also attenuated with age. The association of psychological distress with physical inactivity grew stronger up to age 60 after which it remained stable. Psychological distress was most strongly related to short sleep among 18–19 year olds, but there was no clear trend across older ages. Figure 4 shows the population prevalences of health behaviors by age group and level of psychological distress, as derived from the logistic regression models.
Associations of psychological distress with health behaviors by 5-year age groups. The values are odds ratios (and 95% confidence intervals) per 8.3 points of the continuous K6 scale (average difference between people with no vs at least moderate psychological distress) that derived from the logistic regression models, adjusted for sex, time period, and race/ethnicity (n = 603,518). The quadratic trends are fitted to the odds ratio estimates, weighted by the inverse of the standard error of the estimates
Population prevalences of health behaviors by age group and levels of psychological distress (no versus at least moderate psychological distress). Values are proportions derived from logistic regression models, adjusted for sex, age, and race/ethnicity. Black circles are for participants with at least moderate psychological distress, while white circles are for participants with no psychological distress. The quadratic trends are fitted by weighting the points by the inverse of the standard error of the estimates. Note the differences in y-axis ranges
The details of the full cross-classified random-effects regression models including time period, age, and birth cohort effects are reported in Supplementary Table 1. There was a cohort effect for smoking indicating that psychological distress became more strongly related to smoking among younger birth cohorts, but among those born in the 1990s the association again attenuated (Fig. 5). There was no evidence for other cohort effects.
Birth cohort effect for smoking derived from cross-classified multilevel regression (see Supplementary Table 2 for details). Values are odds ratios (and 95% confidence intervals) per 8.3 points of the continuous K6 scale (average difference between people with no vs at least moderate psychological distress) by decade of birth, adjusted for sex, age, race/ethnicity and time period
Discussion
Previous studies have shown that the relative risk of smoking associated with psychological distress has become stronger in the last 20 years, because the prevalence of smoking has declined more rapidly among those without psychological distress than among those with psychological distress [10,11,12,13,14] The current results suggest that other health behavior correlates of psychological distress have also changed during the last 10–20 years in the United States: psychological distress has become more strongly associated with physical inactivity and short sleep duration, but less strongly related with heavy alcohol consumption.
The previously reported time trends of psychological distress and smoking suggest that the public health improvements have not reached people with mental health problems as effectively as those without mental health problems [10]. We observed that the associations of short sleep and physical inactivity with psychological distress also strengthened over time, suggesting a broader worsening health behavior profile associated with psychological distress that covers other health behaviors besides smoking. Heavy alcohol consumption became less strongly associated with psychological distress, implying that not all adverse health behaviors necessarily follow a common trend of worsening associations with psychological distress. This weakening association was mostly driven by the slightly steeper increase in heavy alcohol consumption among people with no distress, implying no major changes among psychologically distressed people.
All the associations between psychological distress and health behaviors varied with age. Short sleep duration was strongly associated with psychological distress among the 18–19 year olds, after which the association became weaker and remained stable. Sleep time recommendations [23] suggest that adolescents need more sleep than adults (8–10 h vs 7–9 h), so short sleep of ≤ 6 h may indicate a more detrimental sleep deprivation for those younger than 20 years; this could explain the stronger association with psychological distress among younger individuals. With increasing age, psychological distress became less strongly associated with smoking and heavy alcohol consumption. These patterns might reflect age differences in psychiatric comorbidity. For example, externalizing psychiatric problems (e.g., substance abuse) reach their peak prevalence in young adulthood and decline thereafter [24]. The associations of physical inactivity with psychological distress strengthened with age, which may reflect the increasing role of physical limitations with age [25].
Smoking was the only health behavior for which there was any evidence for a birth cohort effect in the association with psychological distress. The association grew stronger in younger birth cohorts from the 1910s to the 1980s. A birth cohort effect for smoking is plausible, as most adult smokers have started to smoke already in adolescence [17, 26]. Adolescents with a propensity to mental health problems may have been less aware of the adverse effects of smoking, thereby increasing the relative risk associated with psychological distress in more recent birth cohorts who have become increasingly aware of the health risks of smoking. In older birth cohorts, when smoking was more common across the population, smoking may have been less selective with respect to adolescent mental health problems, [27]. However, the association seems to have returned to its 1910s level for those born in the 1990s; more data in the coming years are needed to test whether this trend holds in the younger birth cohorts. Also, it must be emphasized that the statistical separation of age, period, and cohort effects is not straightforward, and that even the random-effects modeling may have its limitations [20].
The current findings need to be considered within some limitations. First, psychological distress may influence health behaviors, but unhealthy behaviors may also increase psychological distress [2,3,4,5,6,7] The current data cannot determine the temporal order (or common causes) of the associations; longitudinal studies would be particularly valuable to clarify this issue. Second, psychological distress and health behaviors were all self-reported, which may have biased the true associations between psychological distress and health behaviors. Third, some might argue that short sleep duration should not be considered as a health behavior in relation to psychological distress, as sleep problems are often included as symptoms of poor mental health [6]. From this perspective, the strengthening association between distress and short sleep duration would still hold, but it would indicate that short sleep duration has become a more prominent symptom characterizing psychological distress. Fourth, we did not have data on all relevant health behaviors, for example, on dietary patterns. Finally, the current data do not yet provide information on the mediating mechanisms that link psychological distress to health behaviors differently by time period and age. These might include changes in health literacy, socioeconomic disparities, or people’s coping styles with distress, among other factors. Identifying these mechanisms will be important for understanding how psychological distress becomes associated with adverse health behaviors that increase the health burden of distress.
In conclusion, the current findings extend previous results on how psychological distress has become more strongly associated with smoking in the last 20 years. In addition to smoking, we observed strengthening associations with short sleep duration and physical inactivity. Heavy alcohol consumption became slightly more common among those with no psychological distress, thus weakening the association between distress and heavy alcohol consumption. The associations between psychological distress and health behaviors also varied by age, suggesting considerable heterogeneity in how psychological distress and poor health behaviors are connected across the life span.
References
Viron MJ, Stern TA (2010) The impact of serious mental illness on health and healthcare. Psychosomatics. 51(6):458–465. https://doi.org/10.1176/appi.psy.51.6.458
Leventhal AM, Zvolensky MJ (2015) Anxiety, depression, and cigarette smoking: a transdiagnostic vulnerability framework to understanding emotion–smoking comorbidity. Psychol Bull 141(1):176–212. https://doi.org/10.1037/bul0000003
Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC (1997) Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry 54(4):313–321. https://doi.org/10.1001/archpsyc.1997.01830160031005
Hakulinen C, Jokela M (2018) Alcohol use and personality trait change: pooled analysis of six cohort studies. Psychol Med 1:1. https://doi.org/10.1017/s0033291718000636
Teychenne M, Ball K, Salmon J (2010) Sedentary behavior and depression among adults: a review. Int J Behav Med. 17(4):246–254. https://doi.org/10.1007/s12529-010-9075-z
Harvey AG (2008) Insomnia, psychiatric disorders, and the transdiagnostic perspective. Curr Dir Psychol Sci 17(5):299–303. https://doi.org/10.1111/j.1467-8721.2008.00594.x
Rosenström T, Jokela M, Puttonen S et al (2012) Pairwise measures of causal direction in the epidemiology of sleep problems and depression. PLoS One 7(11):1. https://doi.org/10.1371/journal.pone.0050841
Cuijpers P, Schoevers RA (2004) Increased mortality in depressive disorders: a review. Curr Psychiatry Rep 6(6):430–437. https://doi.org/10.1007/s11920-004-0007-y
Kessler RC, Barker PR, Colpe LJ et al (2003) Screening for serious mental illness in the general population. Arch Gen Psychiatry 60(2):184–189. https://doi.org/10.1001/archpsyc.60.2.184
Cook BL, Wayne GF, Kafali EN, Liu Z, Shu C, Flores M (2014) Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA 311(2):172–182. https://doi.org/10.1001/jama.2013.284985
Lawrence D, Williams JM (2015) Trends in smoking rates by level of psychological distress–Time series analysis of US National Health Interview Survey data. Nicotine Tob Res. https://doi.org/10.1093/ntr/ntv272
Steinberg ML, Williams JM, Li Y (2015) Poor mental health and reduced decline in smoking prevalence. Am J Prev Med 49(3):362–369. https://doi.org/10.1016/j.amepre.2015.01.016
Kulik MC, Glantz SA (2017) Softening among U.S. smokers with psychological distress: More quit attempts and lower consumption as smoking drops. Am J Prev Med. 53(6):810–817. https://doi.org/10.1016/j.amepre.2017.08.004
Szatkowski L, McNeill A (2015) Diverging trends in smoking behaviors according to mental health status. Nicotine Tob Res 17(3):356–360. https://doi.org/10.1093/ntr/ntu173
Ford ES, Cunningham TJ, Croft JB (2015) Trends in self-reported sleep duration among US adults from 1985 to 2012. Sleep 38(5):829–832
Dawson DA, Goldstein RB, Saha TD, Grant BF (2015) Changes in alcohol consumption: united States, 2001–2002 to 2012–2013. Drug Alcohol Depend 148:56–61. https://doi.org/10.1016/j.drugalcdep.2014.12.016
Cdc. National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health (2014) The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); Atlanta: Centers for Disease Control and Prevention
Clarke TC, Norris T, Schiller JS (2017) Early release of selected estimates based on data from the 2016 national health interview survey. National Center for Health Statistics. https://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201705.pdf
Yang Y, Land KC (2008) Age–period–cohort analysis of repeated cross-section surveys fixed or random effects? Sociol Methods Res Sage Publ 36(10):297–326. https://doi.org/10.1177/0049124106292360
Bell A, Jones K (2018) The hierarchical age–period–cohort model: why does it find the results that it finds? Qual Quant 52(2):783–799. https://doi.org/10.1007/s11135-017-0488-5
Strine TW, Chapman DP (2005) Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Med 6(1):23–27. https://doi.org/10.1016/J.SLEEP.2004.06.003
Prochaska JJ, Sung H-Y, Max W, Shi Y, Ong M (2012) Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res 21(2):88–97. https://doi.org/10.1002/mpr.1349
Hirshkowitz M, Whiton K, Albert SM et al (2015) National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health 1(4):233–243. https://doi.org/10.1016/j.sleh.2015.10.004
Chan YF, Dennis ML, Funk RR (2008) Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. J Subst Abuse Treat 34(1):14–24. https://doi.org/10.1016/j.jsat.2006.12.031
Lin S, Beck AN, Finch BK, Hummer RA, Master RK (2012) Trends in US older adult disability: exploring age, period, and cohort effects. Am J Public Health 102(11):2157–2163. https://doi.org/10.2105/AJPH.2011.300602
Freedman KS, Nelson NM, Feldman LL (2012) Smoking initiation among young adults in the United States and Canada, 1998–2010: a systematic review. Prev Chronic Dis 9(5):E05. https://doi.org/10.5888/pcd9.110037
U.S. Department of Health and Human Services (2014) The Health Consequences of Smoking—50 Years of Progress. A Report of the Surgeon General. Atlanta: Centers for Disease Control and Prevention (US), National Center for Chronic Disease Prevention and Health Promotion
Acknowledgements
Open access funding provided by University of Helsinki including Helsinki University Central Hospital. MJ was supported by the Academy of Finland (311578). TR was supported by the Emil Aaltonen Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicting interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Jokela, M., García-Velázquez, R., Gluschkoff, K. et al. Health behaviors and psychological distress: changing associations between 1997 and 2016 in the United States. Soc Psychiatry Psychiatr Epidemiol 55, 385–391 (2020). https://doi.org/10.1007/s00127-019-01741-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-019-01741-7