Abstract
Medical surveillance for alcohol abuse and dependency at work is mandatory for a list of high-risk occupations. The occupational physician is the only figure entitled to perform alcohol and laboratory tests on employees. This study aims to investigate alcohol-induced injuries in healthcare workers, by using Carbohydrate-Deficient Transferrin (CDT) as a marker during medical surveillance visits. A retrospective study was carried out in an Italian healthcare unit. The sample consisted in 75 healthcare workers who sustained an occupational injury. To assess alcohol consumption, CDT levels were tested as well as serum alanine transaminase (ALT), aspartate transaminase (AST), gamma-glutamyltransferase (GGT), mean corpuscular volume (MCV). No worker had positive CDT levels (cut-off 2%); 12% of cases (5 male and 4 female workers) had γ-GT level higher than normal range (cut-off: 36 U/L). Most injuries (53.33%) occurred during morning shifts, 33.33% during afternoon shifts and 13.33% during night shifts. Female workers had a higher injury rate (73%); biological injuries were the most frequent (36%), followed by slipping and falling 33%. This study seems to indicate that alcohol does not represent an important cause of occupational injuries, as no cases of workplace injury were found positive for CDT. CDT as a biomarker in health surveillance programs could be used to assess alcohol consumption when used alongside other biochemical parameters, and its routine use during medical surveillance could act as a deterrent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Occupational injury was defined by the Italian National Insurance Institute for Occupational Injuries and Illnesses (INAIL) as an accident with a violent cause taking place during work and resulting in worker’s death, full or partial permanent disability, or full temporary disability leading to an absence from work lasting more than three days. Worldwide there are approximately 317 million nonfatal occupational injuries and 321,000 occupational fatalities occur globally each year, meaning 151 workers sustain a work-related accident every 15 s according to the International Labour Organizzation (ILO) [1]. Several risk factors have been found to increase the risk of occupational injuries, such as the lack of safety culture at work, poor workplace health and safety practices, inadequate use of protective equipment, hazardous job tasks, inadequate or ineffective safety training [2]. Work injuries may also occur if workers adopt hazardous behaviors, if they do not comply with workplace safety policies, or when they are physically present at work, but they are not able to fully perform their duties because of physical or mental impairments. Injuries can be one of many adverse consequences of substance use and misuse, and are often suspected to contribute to occupational injuries.
According to ILO estimates, 10–20% of all occupational injuries can be attributed to alcohol use; the World Health Organization (WHO), has also highlighted that 30% of annual injuries globally are related to hazardous alcohol consumption. In Italy, almost 100,000 work injuries and 15,000 fatal occupational injuries yearly, may be associated to alcohol use or misuse, representing approximately 10–40% of all occupational injuries. This percentage includes more than 90,000 drunk-driving crashes per year happening during working hours or commuting time [3].
There are several factors that may explain why drinking small amounts of alcohol while working may increase a worker’s risk of being injured in the workplace. The acute effects of alcohol consumption on impairments in reaction time, reasoning, coordination, care, and judgment, have been well documented [4, 5]. In addition, alcohol use that occurs hours before workers begin their shift can cause spillover effects, such as fatigue and hangovers, that may independently increase injury risk [6, 7]. An alternative explanation linking substance misuse to occupational injuries is based on the hypothesis that people more inclined to misuse alcohol and other substances may be more likely to be engaged in other behaviors increasing the risk of injury, a concept defined as deviance proneness [7, 8].
In order to minimize the burden that alcohol use and misuse may have in terms of adverse work-related outcomes and behaviors, Italian policymakers (through the Leg. Decree 125/2001) have prohibited both alcohol sale and use in all workplaces, and have introduced alcohol screening tests on on-duty workers (“on site alcohol test” by detecting ethanol in biological sample such as serum, urine, breath). A few years later, the subsequent Law on Occupational Safety and Health (Leg. Decree 81/2008) has incorporated provisions related to medical surveillance about alcohol consumption in the workplace. Medical surveillance for alcohol abuse and dependency at work are mandatory for those occupations for which there is a high risk of accidents at work, or for the security, safety and health of third parties, as well as those characterized by high responsibility toward other people, such as teachers or healthcare workers. For this reason, this study was performed on people practicing their profession in hospitals, because alcohol consumption by healthcare workers, even in small amounts, may be dangerous not just for the workers doing it but also for the third parties involved in their profession (i.e.: patients). The occupational physician is the only figure entitled by law to perform alcohol-related laboratory tests on employees who undergo medical surveillance. While the detection of ethanol in biological samples, such as serum, urine, or breath, is broadly recognized as the standard method to discern the compliance with the prohibition of alcohol consumption at work, there is not a unanimous consensus on the screening instruments used for the workplace surveillance of alcohol dependence [3, 9]. Currently a wide array of indirect alcohol consumption biomarkers is used, such as gamma-glutamyltransferase (GGT), alanine transaminase (ALT), aspartate transaminase (AST), and mean corpuscular volume (MCV), as well as carbohydrate-deficient transferrin (CDT). They have suboptimal specificity and sensibility values so they are often used together in order to improve the ability to detect alcohol abuse and the consequent early liver damage. Among these biomarkers, the relative amount CDT (%CDT), is the most specific serum biomarker indicating heavy alcohol consumption even though its diagnostic sensitivity is low [10,11,12]. CDT refers to a temporary alteration in the glycosylation pattern of transferrin resulting in an increase in the relative amounts of disialo- and asialo-transferrin (and a decrease in tetra-asialo-transferrin) that occurs as a result of sustained heavy alcohol consumption (thresholds range from 50 to 80 g of alcohol/day for at least 2 weeks). Altered transferrin glycosylation patterns return to baseline levels within 2 to 5 weeks following complete abstinence from alcohol [13,14,15].
Several analytical methods based on immunological, high-performance liquid chromatography (HPLC), immunoassays with column separation (ELISA) and capillary electrophoresis (CE) techniques, have been proposed for CDT routine measurements. Coccini et al. [11] who compared %CDT value achieved by HPLC and ELISA within the same worker sample found difference in the analyzed measurements. This indicates that the ELISA method caused 5 to 10% false positive results in comparison with the HPLC method.
In 2018, the health surveillance of healthcare workers (HCWs) employed in a large Local health Unit in Rome was carried out. The WHO defines HCWs as those who “study, advise on, or provide preventive, curative, rehabilitative and promotional health services”, therefore the employees on the Local Health Unit falling into this category were included in the study upon giving informed consent to participate [16]. Despite the lack of a validated national protocol for the screening of high-risk levels of alcohol consumption in workplace, guidelines established by medical experts working in the Local Health Unit the study was performed in, were used for workplace surveillance regarding alcohol dependence [17]. In accordance with these guidelines, all HCWs who underwent routine health checks were tested for serum ALT, AST, GGT, MCV and CDT levels.
The aim of this retrospective study was, firstly, to investigate whether there is any difference between HCWs who sustained an injury at work and healthy colleagues in high-risk alcohol consumption, according to CDT and other alcohol biomarkers. The research hypothesis was that a difference would be found in the alcohol consumption prevalence between cases (HCWs who sustained injuries) and controls (HCWs who did not sustain injuries). The alcohol screening was performed by evaluating CDT, GGT, AST, ALT and MCV in all workers, both injured HCWs and controls. Data on drinking patterns in HCWs allowed the researchers to verify whether blood parameters including CDT and liver function tests, that are currently used in routine health surveillance, have a real discriminatory power in identifying a risk condition and/or chronic alcohol abuse. The information provided by this study will be useful for directing specific training initiatives targeting HCWs and aimed at raising awareness on the prevention of work accidents.
2 Methods
A retrospective analysis of laboratory data from HCWs employed in two different hospitals (hereinafter named Hospital “A” and Hospital “B”), located in one of the larger Local Health Unit in Rome, where CDT was included in routine workplace health assessment. For the purpose of this study, occupational injury was defined as damage to the body, regardless of its severity, resulting from a workplace accident.
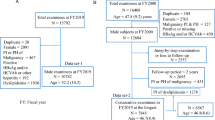
Data on occupational injuries was obtained from medical reports completed at the worksite medical center. For each injured worker, data on type of injury and how it had occurred was collected, as well as data on workers’ occupational history at the injury date (such as job title and work category). Cases (n = 75, 20 males and 55 females) were defined as workers who sustained an occupational injury in 2018. All cases worked in Hospital “A” when the injury occurred. Controls (n = 110, 33 males and 77 females) were selected from the cohort of workers who did not sustain an injury in 2018, and in the same period of time were working at the same Local Health Unit, at the Hospital “B”. The percentages according to gender were similar for cases and controls, in order to match the samples according to gender.
The γ-glutamyl transpeptidase (GGT), aspartate aminotransferase and alanine aminotransferase (AST-ALT), and mean corpuscular volume (MCV), as well as carbohydrate-deficient transferrin (CDT), were assessed through a blood test during the routine medical surveillance. Therefore, for the purpose of this study, these values were extracted from workers’ personal record; no additional blood tests were performed on the HCWs. The carbohydrate-deficient transferrin (CDT), was analyzed as the percentage of transferrin (%CDT) at both Hospital “A” and Hospital “B”, using the immunoturbidimetric assay immunonephelometric assay in 185 subjects who participated in the study. To identify alcohol abusers, two different threshold values were used. A cut-off of 2% CDT was applied in Hospital “A” (Agilent Bio-Rad hplc chromatography high quality), while Hospital “B” biochemistry adopted an higher cut-off of 2.4% CDT (Siemens Bn Pro-Spec immunophelometric assay). The alcohol screening was considered positive when workers %CDT result exceeded the cutoff limit.
All workers gave their consent for personal data processing, in compliance with GDPR 2016/679 at the hiring and during the following health visits. The research was conducted in accordance with the Helsinki declaration and approved by the ASL ROMA 2 Ethics Committee (02 mar 2020, N°438).
2.1 Statistical analysis
A descriptive analysis of work injuries which occurred in 2018 was carried out, in order to assess which injuries were more prevalent in the HCWs samples in the two hospitals of the same Local Health Unit. The distribution of %CDT values in the sample was evaluated by Shapiro-Wilk test. Since two different %CDT cut-off limits were adopted, the workers (both cases and controls) were categorized into four subgroups based on serum total %CDT concentrations. The potential correlation between the likelihood of injuries and %CDT values were analyzed by Fisher test for categorical variables in both cases and controls, while the Mann Whitney test was used to explore the distribution of CDT values in male and female subgroups. The comparison of average %CDT values in cases and controls was carried out using the non-parametric Wilcoxon rank-sum, while GGT, MCV, ALT and AST data were analyzed by the Mann-Whitney test because they had an uneven distribution.
In this study, the STATA16 software was used to perform statistical analyses.
3 Results
In 2018, 75 injuries occurred among health care workers employed in “Hospital “A”. Occupational injuries resulted in a period of absence from work that varied from 0 to 30 days; the average duration of absence was 5–6 days with a Standard Deviation (SD) of ± 7.56. Most injuries (53.33%) occurred during morning shifts (n = 40), 33.33% (n = 25) during afternoon shifts, and 13.33% (n = 10) during night shifts. Female workers had a higher injury rate than male colleagues: 73% versus 27% (n = 55 and n = 20 respectively). As for the type of occupational injury, biological injuries (36%, n = 27) were the most common ones, followed by slipping and falling (33%, n = 25), commuting accidents (15%, n = 11), musculoskeletal injuries caused by manual handling (9%, n = 7) and verbal/physical aggressions (7%, n = 5).
One HCW resulted positive to CDT testing in the control group, no positives were found in case group; no correlation between positive CDT and occupational injuries in cases and controls was found. Out of the 185 subjects who participated in the study, only one screened positive with CDT value exceeding the cut-off. There was no positive result among workers who sustained an injury in 2018 so they were identified as nonhazardous drinkers; a positive result was found in the control group. Because two different cut-offs were applied to %CDT analysis (2% for cases and 2,4%for controls), a classification of the %CDT data was performed according to interquartile ranges, in order to compare the two groups. In the case group, the majority of subjects (62.67%; n = 47) had %CDT values in the first quartile (from 0.5 to 1), 28% (n = 21) had % CDT ranged from 1 to 1.5; 0.67% (n = 5) had %CDT lower than 0.5; 0.03% (n = 2) had %CDT higher than 1.5%. In the control group, the majority of subjects (81%, n = 89) had %CDT values in the second quartile (from 1.2 to 1.8), 0.8% (n = 9) had %CDT ranged from 0.6 to 1.2%, 1% (n = 11) had %CDT ranged from 1.8 to 2.4%; 0.9% (n = 1) had %CDT higher than 2.4%. The comparison between the two groups showed that %CDT values were higher in workers who did not report any injuries when compared with those with injuries (Fig. 1).
The analysis of the %CDT distribution according to the gender did not find any significant difference between male and female workers (Table 1).
Despite the fact that %CDT was in the normal range, 12% of cases (5 male and 4 female workers) and 5% of controls (5 male and 1 female workers) had γGT level exceeding cut-off(36 U/L); 11% of cases (6 male and 2 female workers) and 0.9% of controls (1 woman) had ALT exceeding cut-off. One case (1 man) had AST value higher than cut-off and only 1 control (1 man) had higher MCV than average (Table 2).
Table 3 shows that there was significant difference in mean ALT serum level (p < 0.001) and average MCV (p < 0.001) results between injured HCWs and controls.
4 Discussion
There are several reasons for employers to focus on problems related to alcohol use and abuse in the workplace, such as the associated risk of accidents leading to injury, the increased risks of poor-health and absenteeism, reduced productivity, and negative effects on the working atmosphere, which may all lead to increased costs for both employers and employees [11]. A number of studies indicated that alcohol use and misuse increase the risk of occupational injuries in many occupations, but, to the best of the authors’ knowledge, no studies investigated the association between alcohol consumption and occupational injuries in the healthcare sector. With this in mind, this retrospective observational study investigated whether there is any difference between HCWs who sustained an injury at work (cases) and healthy colleagues (controls), in high-risk alcohol consumption.
No correlation was found between injury and problematic use of alcohol in this study. Therefore, the null hypothesis was rejected and the alternative hypothesis was accepted. In addition, data on CDT was extremely low, with just one positive case at the screening test out of 185 subjects sampled. Working under the influence of alcohol did not seem to be a significant problem among the HCWs, and neither was working after a high alcohol intake the days before.
Regarding non-specific alcohol markers, the observation of higher γGT, AST, ALT levels in cases in comparison with controls is not sufficient to state that these alterations may be related to alcohol use. The results from this study, however, partly agree with the observation that a higher percentage of injured workers had high levels (exceeding normal range) of γGT, AST and ALT when compared with controls, arising doubts on the accuracy of CDT’s discriminatory power in case of moderate drinking [18]. This study’s finding that alcohol consumption does not affect the likelihood of being injured at work disagrees with previous findings provided by studies conducted in other occupations, and the lack of data on this topic in the healthcare sector excludes any meaningful comparison. Compared to the general population, HCWs seemed to follow a healthier lifestyle especially regarding the low rate of drinking, according to Rosta et al. [19], Allamani et al. [20] and Simione and Gnagnarella [21].
Although heavy-drinking rates are lower in healthcare and social assistance settings in comparison with other industries, according to data provided by Larson et al. in 2007 [22], in the sample from this study only one case of problematic alcohol use has emerged. Given that the exclusive use of CDT as a screening tool in this study may have overlooked a part of the high risk population, with the sample representing almost 7–8% of HCWs employed in the hospitals of the Local health Unit, we would have expected an higher percentage of HCWs being positive for the CDT screening than what was observed.
The gathered data also disagrees with other studies on alcohol consumption and hazardous drinking behaviors. In these studies—conducted on similar populations of healthcare professionals, during the screening routine and without investigating about the injury correlation –more cases of alcohol-related problems were reported when compared with the study performed for this research. Obadeji et al. [23] reported a 5.9% prevalence of hazardous or harmful drinkers among 256 Nigerian HCWs in the medical and surgical specialties; Saridi et al. [24] found a low alcohol consumption among 579 health professionals during the economic crisis in Greece; Issa et al. [25] found a 4.1% percentage of hazardous alcohol users among 241 Nigerian doctors; Aguocha et al. [26] reported 1.7% of resident doctors and 2.7% non-resident doctors have alcohol use problems among 450 Nigerian healthcare professionals.
In order to explain the data that emerged from this study, the role of the supervisory authorities on the alcohol-correlated problems must be explained; in application of the current legislation in Italy, the supervisory authorities have established very strict measures on workers found to be in breach of the alcohol consumption in the workplace law. In particular, the routine use of CDT is not a standard practice in all health units in Italy, and therefore applying this measure in mandatory health surveillance in the selected hospitals for this study may have acted as a strong deterrent to workers.
If the CDT measurement as a tool acting as alcohol consumption deterrent was confirmed by further investigations, its use in health surveillance protocols could be maintained to fit this purpose. One leading finding of this study is the lack of difference in alcohol consumption between males and females according to CDT. The results do not support the previous findings that being male tends to correlate significantly with more hazardous drinking among HCWs [19, 23, 25].
This pilot study has some limitations, first of all the small sample size. The second limitation is represented by the absence of self-reported individual data on workers’ drinking patterns. However, the use of self-reported questionnaires or semi structured interviews in an occupational setting where the use or abuse of alcohol is heavily sanctioned may force the worker not to answer honestly; some studies have indicated that non-respondents generally drink more, or that alcohol misuse is more common in this group [27]. Another limit of the study design is the adoption of two different cut-off limits for identifying high risk drinkers, 2% and 2.4% respectively for cases and controls. This limit was partially overcame by dividing the sample in interquartiles and interpreting %CDT as a categorical variable according to the values exceeding the cut off, therefore considered as “positive”, and those below the cut-off, considered as “negative”.
5 Conclusions
In this study in the healthcare sector, alcohol plays a minor role in the occurrence of occupational injuries, as no injury cases had CDT values over the cut-off. The prevalence of alcohol consumption posing a risk among HCWs was low; blood parameters routinely used to screen chronic alcohol intake among HCWs have been shown to be insufficient in identifying a risk condition. Although no injury cases were found to have CDT values over the cut-off, the use of CDT in health surveillance protocols could play a role as a specific biomarker of alcohol consumption (not as a marker of alcohol abuse or dependence), as well as a deterrent for operators in order not to incur in important work sanctions, as they are encouraged to strictly comply with alcohol regulations. These findings deserve further investigations to assess the exact role of CDT in health surveillance protocols for occupational screening, and a similar study in a larger population may be instrumental to assess if alcohol consumption plays a role in workplace injuries, as well as further evaluate the role of CDT in alcohol consumption assessment.
Data Availability
Data from this research is available upon reasonable request.
Code Availability
Not applicable.
References
ILO calls for urgent global action to fight occupational diseases. Published April 26., 2013. Accessed April 6, 2021. http://www.ilo.org/hanoi/Informationresources/Publicinformation/Pressreleases/WCMS_211708/lang--en/index.htm.
Abdalla S, Apramian SS, Cantley LF, Cullen MR. Occupation and Risk for Injuries. In: Mock CN, Nugent R, Kobusingye O, Smith KR, eds. Injury Prevention and Environmental Health. 3rd ed. The International Bank for Reconstruction and Development / The World Bank; Accessed April 6, 2021. http://www.ncbi.nlm.nih.gov/books/NBK525209/. 2017.
Spigno F, Debarbieri N, Traversa F. Lavoro e dipendenza da sostanze psicoattive: idoneità alla mansione e prospettive di prevenzione alla luce delle recenti innovazioni normative. G Ital Med Lav Ergon. 2007;29(2):158–65.
Perrine MW. Alcohol influences on driving-related behavior: A critical review of laboratory studies of neurophysiological, neuromuscular, and sensory activity. J Saf Res. Published online 1973.
Egervari G, Siciliano CA, Whiteley EL, Ron D. Alcohol and the brain: from genes to circuits. Trends Neurosci. 2021;44(12):1004–15. https://doi.org/10.1016/j.tins.2021.09.006.
Yesavage JA, Leirer VO. Hangover effects on aircraft pilots 14 hours after alcohol ingestion: a preliminary report. Am J Psychiatry. 1986;143(12):1546–50. https://doi.org/10.1176/ajp.143.12.1546.
Toney-Butler TJ, Siela D. Recognizing Alcohol and Drug Impairment in the Workplace in Florida. In: StatPearls. StatPearls Publishing; 2023. http://www.ncbi.nlm.nih.gov/books/NBK507774/. Accessed 6th April 2023.
Spicer RS, Miller TR. Impact of a workplace peer-focused substance abuse prevention and early intervention program. Alcohol Clin Exp Res. 2005;29(4):609–11. https://doi.org/10.1097/01.alc.0000158831.43241.b4.
Borrelli I, Santoro P, Gualano M, et al. Alcohol consumption in the workplace: a comparison between European Union Countries’ policies. Int J Environ Res Public Health. 2022;19:16964. https://doi.org/10.3390/ijerph192416964.
Helander A, Wielders JPM, Jeppsson JO, et al. Toward standardization of carbohydrate-deficient transferrin (CDT) measurements: II. Performance of a laboratory network running the HPLC candidate reference measurement procedure and evaluation of a candidate reference material. Clin Chem Lab Med. 2010;48(11):1585–92. https://doi.org/10.1515/CCLM.2010.322.
Coccini T, Crevani A, Acerbi D, et al. Comparative HPLC and ELISA studies for CDT isoform characterization in subjects with alcohol related problems. Prospective application in workplace risk-prevention policy. G Ital Med Lav Ergon. 2008;30(2):119–27.
Borrelli I, Gualano M, Perrotta A, Rossi M, Santoro P, Moscato U. The use of carbohydrate-deficient transferrin in occupational setting: a systematic review. Occup Med Health Aff. 2022;10:1000411. https://doi.org/10.4172/2329-6879.1000411.
Landberg E, Påhlsson P, Lundblad A, Arnetorp A, Jeppsson JO. Carbohydrate composition of serum transferrin isoforms from patients with high alcohol consumption. Biochem Biophys Res Commun. 1995;210(2):267–74. https://doi.org/10.1006/bbrc.1995.1656.
Stibler H. Carbohydrate-deficient transferrin in serum: a new marker of potentially harmful alcohol consumption reviewed. Clin Chem. 1991;37(12):2029–37.
Trbojević-Akmačić I, Vučković F, Pribić T, et al. Comparative analysis of transferrin and IgG N-glycosylation in two human populations. Commun Biol. 2023;6:312. https://doi.org/10.1038/s42003-023-04685-6.
World Health Organization. Classifying health workers: mapping occupations to the international standard classification.
D’Oca D, D’Orsi F, Giuggioli V et al. Linee guida per la sorveglianza sanitaria dei lavoratori. Published online 2009.
Arndt T. Carbohydrate-deficient transferrin as a marker of chronic alcohol abuse: a critical review of preanalysis, analysis, and interpretation. Clin Chem. 2001;47(1):13–27.
Rosta J. Hazardous alcohol use among hospital doctors in Germany. Alcohol Alcohol. 2008;43:198–203. https://doi.org/10.1093/alcalc/agm180.
Allamani A, Beccaria F, Voller F. The puzzle of italian drinking: Trends in alcohol consumption, harms and policy: Italy 1990–2010. Nordic Stud Alcohol Drugs. 2010;27(5):465–78. https://doi.org/10.1177/145507251002700504.
Simione L, Gnagnarella C. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. Front Psychol. 2020. https://doi.org/10.3389/fpsyg.2020.02166.
Larson S, Eyerman J, Foster M, Gfroerer J. Worker Substance Use and Workplace Policies and Programs. Published online January 1, 2007.
Obadeji A, Oluwole LO, Dada MU, Oshatimi MA. Alcohol use and psychological wellbeing of health workers in a nigerian hospital: an exploratory study. Malawi Med J. 2018;30(1):31–6. https://doi.org/10.4314/mmj.v30i1.7.
Saridi M, Karra A, Kourakos M, Souliotis K. Assessment of alcohol use in health professionals during the economic crisis. Br J Nurs. 2016;25(7):396–8. https://doi.org/10.12968/bjon.2016.25.7.396.
Issa BA, Yussuf AD, Abiodun OA, Olanrewaju GT, Kuranga TO. Hazardous alcohol use among doctors in a nigerian tertiary hospital. West Afr J Med. 2012;31(2):97–101.
GU A, Onyeama G, Bakare M, Igwe M. Alcohol use problems among resident doctors in a Nigerian tertiary hospital. Pioneer Med J. 2016;5:1–13.
Mäkelä P, Fonager K, Nordlund S, Sabroe S, Simpura J, Drug Research. Drinking habits in the Nordic Countries - Research - Aarhus University. In: Vol 2. SIFA Rapport. National Institute for Alcohol and ; 1999. https://pure.au.dk/portal/en/publications/drinking-habits-in-the-nordic-countries(e4722570-954c11da-bee9-02004c4f4f50).html. Accessed 6th April 2021.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, IB and UM; Methodology, MRG, IC, VD, PES; Formal Analysis, IB, MRG, UM and PES; data gathering, IC,VD; Investigation, IC, VD and IB; Writing— Original Draft Preparation, IB, IC, VD; Writing—Review and Editing, MFR, MRG; supervision, UM. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was conducted in accordance with the Declaration of Helsinki and approved by the ASL ROMA 2 Ethics Committee (02 mar 2020, N°438). Written informed consent was obtained for all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Borrelli, I., Gualano, M.R., Rossi, M.F. et al. Alcohol consumption in healthcare workers and risk of workplace injury: a case-control study. Discov Sustain 4, 22 (2023). https://doi.org/10.1007/s43621-023-00137-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43621-023-00137-7