Abstract
International guidelines recommend the use of standardized outcome measures post-stroke. The aim of this study was to delineate and evaluate the implementation of four motor function outcome measures. This study describes the application of a multifaceted strategy that integrates various approaches to augment implementation. The study was conducted among physical therapists in a sub-acute neurorehabilitation hospital. The implementation process was guided by the Knowledge-to-Action Cycle, and a taxonomy for implementation outcomes was systematically employed to analyze and evaluate the implementation process. Focus group interviews were conducted both prior and 6 months subsequent to an implementation period. Additionally, data from healthcare records were extracted to monitor the penetration of the new procedures. All 70 employed physical therapists underwent training on the application of the four selected outcome measures. Barriers identified in the focus group interviews encompassed perceived acceptability and appropriateness of the outcome measures, time consumption for testing, and perceived lack of relevance for certain patients. These barriers were mitigated through local adaptions. However, 6 months post-implementation, the adoption and penetration of the new procedures were only partially satisfactory. Some physical therapists still expressed reluctance toward employing outcome measures, and findings from the healthcare records corroborated the interview results. Specifically, adherence to testing procedures surpassed the pre-defined threshold of 75% for only one outcome measure at one pre-defined time point. A persistent effort is required to enhance acceptability, adoption, penetration, and to ensure the sustainability of the new procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The burden of stroke is increasing globally both in developed and developing countries. Stroke is already the second leading cause of death and disability worldwide and affects a large number of people (Krishnamurthi et al., 2020). The American Heart Association has estimated that the prevalence of stroke in adults is 2.7% in the United States, and each year approximately 795,000 people experience a stroke (Benjamin et al., 2018). In 2017, nearly 250,000 people in Denmark lived with a stroke (Sundhedsstyrelsen, 2020). Relevant outcome measures, that quantify the level of motor impairment and function post-stroke, are crucial for monitoring changes in a patient's functional status during neurorehabilitation and a prerequisite for providing effective treatment. International and national guidelines recommend the use of evidence-based standardized outcome measures after stroke (Danmark, 2020; Kwakkel et al., 2017; Moore et al., 2018; Pohl et al., 2020). These measures can support the patient-centered planning and evaluation of rehabilitation and may visualize the personal improvement of the patient (Gubrium et al., 2003; Oyake et al., 2020). Furthermore, the effectiveness of physical therapy interventions can be evaluated reliably, and consequently aid the generation of new knowledge (Danmark, 2020; Kwakkel et al., 2017; Moore et al., 2018; Pohl et al., 2020). If the same set of outcome measures could be applied across all healthcare sectors, communication between healthcare professionals would be enhanced (Maribo et al., 2018). Hereto, the Stroke Recovery and Rehabilitation Roundtable has published guidelines specifying the assessment in clinical rehabilitation settings, including clearly defined assessment time points post-injury (Pohl et al., 2020). Recently, two clinical guidelines for the use of standardized outcome measures were published in Denmark (Danmark, 2020; Rehabiliteringsforum, 2022). However, they are not broadly implemented and there is a wide variation in the use of outcome measures throughout the country (Danmark, 2020; Maribo et al., 2018).
A previous study has shown that despite the availability of valid and reliable outcome measures, physical therapists in clinical settings may have reservations about the standardization of the rehabilitation practice (Jaeger Pedersen & Kaae Kristensen, 2016). Thus, to advance the implementation of evidence into practice and support the routine use of standardized outcome measures, a specific focus should be on implementation research (Eng et al., 2019; Juckett et al., 2022). Implementation research includes the use of models and frameworks which provide a structure and terminology for a systematic evaluation of the implementation process and its outcomes (Nilsen, 2015; Proctor et al., 2011). The knowledge translation process from research to practice can be guided and continuously evaluated with the help of a process model such as the Knowledge-to-Action Cycle (Moore et al., 2022; Nilsen, 2015). The Knowledge-to-Action Cycle consists of seven iterative phases for knowledge transfer. These phases include identifying knowledge gaps; adapting knowledge to the local context; assessing barriers and facilitators to knowledge use; selecting, tailoring, and implementing interventions for evidence translation; monitoring knowledge use; outcome evaluation; and finally sustaining knowledge use (Moore et al., 2022; Nilsen, 2015).
The aim of the present study was to delineate and evaluate the implementation process of four standardized motor function outcome measures applied in a neurorehabilitation hospital.
Design and Method
In this implementation study, the development and use of a multifaceted implementation strategy to enhance knowledge transfer is elucidated. The study combined a qualitative and a quantitative part, termed a mixed-methods approach (Bazeley, 2018; Richards et al., 2019). In the qualitative part, focus group interviews were applied, and in the quantitative part, the timely assessment with the implemented outcome measures was investigated in a cross-sectional design based on routinely collected healthcare data.
Participants and Setting
The study was conducted at an inpatient neurorehabilitation hospital with a total of 115 beds at 10 wards for patients with acquired brain injuries. Patients are in the early to late sub-acute phase and require comprehensive rehabilitation. The content of rehabilitation is individually tailored to the patient's needs and abilities and the length of stay varies. The rehabilitation services are interdisciplinary and the patient and their relatives agree on their rehabilitation goals with a team of professionals (medical doctor, occupational therapist, physical therapist, speech therapist, and neuropsychologist).
This implementation study had its outset in professional development within physical therapy. It focused specifically on this profession as the implementation concerned outcome measures for motor function. At the neurorehabilitation hospital, the four chosen outcome measures should be administered by physical therapists and all 70 employed physical therapists were the target group for this implementation study. Each ward is assigned clinical specialists, who are responsible for professional development, upskilling, and implementation. Furthermore, the hospital entails a multidisciplinary research unit.
Methods and Materials
The implementation process was led by a team of seven physical therapists, including researchers and clinical specialists with a responsibility for the implementation of knowledge.
The Knowledge-to-Action Cycle was applied to guide the transfer of knowledge from evidence into clinical practice (Moore et al., 2022; Nilsen, 2015). To evaluate the success of the implementation and gain insights into if, how, and why it succeeded or failed, the implementation outcomes introduced by E. Proctor et al. were applied (Nilsen, 2015; Proctor E, 2011) Briefly described this taxonomy consists of eight conceptually distinct implementation outcomes—acceptability, adoption, appropriateness, feasibility, fidelity, implementation cost, penetration, and sustainability (Proctor et al., 2011).
Conceptualizing and measuring implementation outcomes will advance the understanding of the implementation process among members of the implementation team. While the Knowledge-to-Action Cycle consists of a practical guide for the implementation process, the outcome taxonomy by Proctor et al. provides a framework to evaluate implementation outcomes within each phase of the implementation (Nilsen, 2015; Proctor et al., 2011).
The Consolidated Framework for Implementation Research (CFIR) can be used to identify the multi-level factors (the individuals involved, inner and outer setting) which play a role in the implementation of the four outcome measures (Damschroder et al., 2009; Proctor et al., 2013). In the present study, the (CFIR) was applied to take into account the different stakeholders of the implementation process.
The implementation process is displayed in Table 1 and described below.
Phase 1: Identify the Problem and Select Knowledge
Standardized outcome measures were not routinely applied in the neurorehabilitation hospital. To assure acceptability among implementation stakeholders, the implementation team defined and agreed on the following selection criteria for measures to be implemented (see Table 1): I. Recommended in international and national guidelines for the assessment of motor function of both upper and lower extremities in patients with acquired brain injury (Danmark, 2020; Kwakkel et al., 2017; Pohl et al., 2020). II. Well-established clinimetric properties such as reliability, validity, and responsiveness to change. III. Applicable to most patients in the hospital, ranging from patients with severe motor and cognitive deficits to those with only minor affections. IV. Outcome measures that were easy to conduct, required a minimum of equipment and took little time to administer, were preferred.
Phase 2: Adapt to Local Context
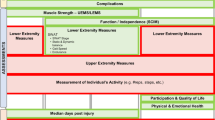
Prior to implementation, descriptions and manuals of the selected outcome measures were made available to all physical therapists on a shared digital platform. In addition, a local clinical guideline, including a flowchart depicting the conditions and time points for the administration of the outcome measures, was designed (see Fig. 1: Outcome Measures Flowchart).
Outcome Measure Flowchart. Time points for assessments: First assessment: within a maximum of 7 days after admittance to the rehabilitation hospital. Discharge assessment: a maximum of 7 days before discharge. 4 weeks (± 3 days) after injury. 3 months (± 3 days) after injury. 6 months (± 3 days) after injury. If the time points for the assessments are close to admission to or discharge from the hospital, the 4 weeks (or 3 months) assessment is prioritized
Phase 3: Assess Barriers and Facilitators
An iterative process to identify barriers and facilitators was applied before and during implementation. Hereto, the physical therapists were encouraged to pose questions to the implementation team on the shared digital platform.
The first round of semi-structured focus group interviews was performed pre-implementation. The aim was to explore the attitudes toward expected acceptability, adoption, perceived appropriateness, and feasibility of the four outcome measures (see interview guide in Supplementary Material 1). Knowledge obtained from the focus groups was used to shape and adjust the implementation process.
Before implementation, the managers of all ten wards were asked to invite two physical therapist, preferably with varied experience within the field of neurorehabilitation, for a first round of focus group interviews. The focus group interviews started with a few broad questions about what the participants considered important factors for the use of outcome measures. Afterward, the questions were specifically about each of the four measures. An experienced qualitative researcher moderated the interviews and was aware of ensuring a confident atmosphere that invited discussion. A fellow researcher participated as an observer, asking clarifying and supplementary questions. The interviews were audio-recorded and transcribed verbatim. Data from this first round of interviews were analyzed pre-implementation in NVivo V.12 and a thematic content analysis was performed (Elo & Kyngas, 2008; Ohman, 2005). The information gained was synthesized and continually discussed among the authors (Malterud, 2001).
Phase 4: Select and Tailor Implementation
The implementation team met regularly throughout the implementation period to discuss and adjust procedures and to secure the implementation.
Phase 5: Monitor Knowledge Use
The knowledge transfer was evaluated in terms of acceptability, appropriateness, feasibility, adoption, fidelity, and penetration. A second round of focus group interviews was conducted 6 months into the implementation process. The aim was to explore changes in perceptions of the acceptability and feasibility. The interview guide had a similar structure for both rounds of interviews, but questions about the implementation process, changes of practice, and experiences were highlighted in the second round of focus group interviews. Participants attending the first and the second round of interviews did not need to be the same.
Phase 6: Evaluate Outcomes
Fidelity toward the procedures for the application of outcome measures (according to Fig. 1) along with penetration defined as the integration of a practice within a service system (Proctor et al., 2011) was monitored. Six months post-implementation (June 2021), the anonymized data for all in-patients during this month (1th–30th June 2021) were extracted from the electronic healthcare records and categorized according to the respective time point (admission, 4 weeks, 3 months from incident, and discharge). The proportion of patients either “correctly assessed” (i.e., timely) or “incorrectly assessed” (i.e., no assessment or too late/ too early) with each of the four outcome measures was estimated for each respective time point. Before the implementation, the team had agreed on a satisfactory penetration rate of at least 75% “correctly assessed” eligible patients with the four measures at the four pre-defined points in time.
Phase 7: Sustaining Knowledge Use
In order to increase the level of penetration and foster sustainability, follow-up meetings with all clinical specialists and individual physical therapists were held and a sustainability plan was created jointly. Further steps to secure long-term sustainability were initiated.
Ethical Considerations
The study was conducted in accordance with the Helsinki Declaration 2018. Informed written consent was obtained from the focus group interview participants. Anonymity was preserved by changing names and identifiable places or situations. According to the Danish Regional Scientific Ethical Committee regulations and due to the nature of the study, the study was categorized as a quality assurance and development project and did not require ethical approval. Data extraction from the electronic healthcare records was approved by the hospital management.
Results
A summary of the results is presented in Table 1. We elaborate on certain aspects of the different phases below.
Knowledge Selection
The following outcome measures fulfilled the selection criteria defined in phase 1 and were selected for implementation: Functional Ambulation Categories, Ten-meter Walk Test, Timed Up and Go, and Fugl-Meyer Motor Assessment Upper Extremity (Fugl-Meyer) (Danmark, 2020; Kwakkel et al., 2017; Moore et al., 2018; Pohl et al., 2020). The Functional Ambulation Categories is a 6-point functional walking test that evaluates ambulation ability (Holden et al., 1984; Mehrholz et al., 2007). The patient can score from a minimum of 0 (inability to walk or needing the assistance of two persons for ambulation) to a maximum of 5 (fully independent ambulation) (Lundquist & Brunner, 2023; Holden et al., 1984; Mehrholz et al., 2007).
For patients who can walk independently, defined as a Functional Ambulation Categories score ≥ 3, the Ten-meter Walk Test and the Timed Up and Go should be applied subsequently. The Ten-meter Walk Test measures walking velocity for a 10-m distance and has shown good clinimetric properties (Andersen & Kristensen, 2019; Cheng et al., 2021; van Bloemendaal et al., 2012). The Timed Up and Go measures the time it takes a subject sitting in an armchair to stand up, walk forward three meters, and return to the seated position. Thus, the Timed Up and Go performance adds elements of leg strength and balance to the test battery. The Timed Up and Go is valid and reliable (Hafsteinsdottir et al., 2014). The Fugl-Meyer measures the movement, coordination, and reflexes of the upper extremity and has proven valid and reliable (Lundquist & Maribo, 2017). The total score ranges from 0 to 66 points (Lundquist & Maribo, 2017), with higher scores indicating better function.
Barriers and Facilitators Identified Pre-implementation
The first round of focus group interviews (three groups) was performed in December 2020, 1 month before the start of the implementation. Characteristics of focus group participants are displayed in Table 2.
Three main themes considered important to the participants and relevant for the approaching implementation of outcome measures evolved and are presented below: Practical obstacles, appropriateness and feasibility of quantitative measurements, and visible improvement. Main quotations are displayed in Table 3.
Practical Obstacles
The majority of the physical therapists were familiar with the Ten-meter Walk Test and the Timed Up and Go and acceptability of these two measures was generally high. In contrast, both the Functional Ambulation Categories and the Fugl-Meyer were new to most therapists and the impending obligation to use these two measures caused frustration and a somehow lower acceptability. The Fugl-Meyer is quite detailed, and the therapists expressed concern that they would have to rely on the manual and that assessment would be time-consuming. In addition, all patients should be assessed at fixed time points after stroke, see Fig. 1. The physical therapists imagined that it would be a challenge to remember assessment time points relative to the index date.
Based on this feedback, all four outcome measures got a new and designated field in the electronic healthcare record to make it clearly visible in the physical therapists’ examination sheet. Thus, the physical therapists were aided in remembering when to test the patient.
Appropriateness of Applying Standardized Outcome Measures
The physical therapists questioned the appropriateness of the four outcome measures to their clinical practice. Points of criticism were that I. Quality of movement might be reduced to a quantitative measurement with little relevance for the individual patient; II. Physical performance could be judged more sufficiently in the patient´s natural environment; III. Outcome measures should be conducted and repeated too often; IV. Outcome measures were irrelevant for many patients due to the severity of their impairment. For instance, non-ambulatory patients could not perform Ten-meter Walk Test and Timed Up and Go. The perceived irrelevance for many patients was the main reason why some physical therapists found the measures unacceptable and inappropriate.
The concerns expressed were addressed by simplifying the registration procedures for patients where specific measures were not relevant. Moreover, the benefits of standardized measures were made explicit again.
On the positive side, several physical therapists found the outcome measures feasible and appreciated the systematic approach to the patient which ensures that functional movement is examined comprehensively.
Visible Improvement
In all interviews, the physical therapists agreed that outcome measures can be feasible as they illustrate functional status and improvement and thus could be a natural part of the physical therapists’ practice. Most patients will experience functional improvement during rehabilitation and being able to quantify this progress can motivate the patients. The physical therapists also acknowledged the benefits of being able to track even minor improvements with the help of frequent and standardized assessments.
Tailored Implementation
The implementation team met regularly throughout a 6-month implementation period to discuss and adjust procedures. Several discussion and practice meetings were arranged for the physical therapists to deepen their knowledge and settle doubts about the correct performance of the outcome measures. Still, these efforts mainly addressed and improved feasibility. A lack of acceptability and adoption, stemming from the perception that the outcome measures were unsuitable for some patients, posed an ongoing challenge and received dedicated focus from the implementation team. Consequently, in response to the concerns of the physical therapists, it was decided that patients who were either physically incapable of executing the outcome measures or cognitively unable to adhere to the procedure could be exempt from testing. Instead, “not relevant” should be documented in the electronic healthcare record, including the reason for this rating.
Barriers and Facilitators after 6 Months
A second round of focus group interviews was performed 6 months into the implementation, in June 2021. The main findings are summarized below:
Practical Obstacles
Six months after implementation, the acceptability of the Fugl-Meyer had improved. While the Fugl-Meyer was still challenging to use, the general view was that with experience, it had become easier. However, many physical therapists continued to find it challenging to use the Functional Ambulation Categories. As a response, the manual was extended with case descriptions.
Appropriateness of Applying Standardized Outcome Measures
Many physical therapists continued to find the outcome measures unacceptable and inappropriate for a range of patients. The ease of testing procedure—that certain patients did not need testing—and also the ease of documentation procedures were welcomed. The overall impression from this second round of interviews was that the changes in procedures had increased the adoption of the chosen outcome measures.
The physical therapists still disagreed on whether outcome measures were a positive contribution to their clinical practice or not. While the majority praised the advantages, some physical therapists were still dismissive of the use of four outcome measures for all patients, despite adjustments in procedures. Yet, many acknowledged the value of having a shared language based on the assessment results.
Visible Improvement
Six months of experience with the use of outcome measures appeared to have broadened the perspectives beyond the individual patient in the present hospital setting. A greater awareness existed, that assessment could enhance communication and aid transfer across healthcare sectors. The physical therapists generally agreed that this would benefit the patients by ensuring an appropriate treatment level when the patient is transferred to municipal treatment and rehabilitation (i.e., primary healthcare sector). There was also increasing awareness about the importance of generating standardized data on a group level for all patients admitted to the neurorehabilitation hospital. In summary, this broadened perspective seemed to have added to the adoption of the four outcome measures and increased the penetration within the organization, i.e., more therapists were willing to comply.
Fidelity to Standardized Outcome Measures after 6 Months
Six months post-implementation data for 100% of in-patients were extracted from the electronic healthcare records and included in the analysis. Defined time points for assessment were admission, discharge, 4 weeks, and 3 months after the incident brain injury (Fig. 1). While all patients should be assessed on admission and discharge, not all patients would be in the hospital at 4 weeks or 3 months post-stroke e.g., due to a shorter rehabilitation duration. For this reason, the potential number of patients varied for the four time points with the highest numbers at admission and discharge.
While the Fugl-Meyer and the Functional Ambulation Categories could be administered to patients regardless of their functional level, the Ten-meter Walk Test and Timed Up and Go could only be administered to patients with an independent functional gait (i.e., Functional Ambulation Categories ≥ 3).
In June 2021, 6 months into the implementation, 59 patients were admitted, and 65 patients were discharged from the hospital. In addition, 52 and 25 patients were present at the hospital 4 weeks and 3 months post-stroke, respectively. Data from 100% of these records were included in the analysis. The number of patients being correctly assessed (i.e., timely assessment according to Fig. 1) was highest on admission for all four outcome measures, varying from 56 to 88% of patients (see Supplementary Material 2 for details on Proportion of Patients Assessed in Adherence with the Local Clinical Guideline). At 4 weeks and 3 months post-stroke, and at discharge, 5–57% of patients were correctly assessed. Only Functional Ambulation Categories on admission (88%) was above the pre-defined threshold for satisfactory penetration of 75% for successful implementation.
Sustaining and Extending the Use of Standardized Outcome Measures
To increase penetration of the implemented procedures and sustain and enforce the use of outcome measures, several steps were taken. First, it was decided that newly employed physical therapists will receive training on outcome measures as part of their routine introduction program. Second, to support and remind the physical therapists of the use of outcome measures, the clinical specialists commenced presenting a digital outcome measure status overview at routine patient evaluation meetings at the wards. The digital status overview draws upon electronic healthcare records. By displaying different colors indicating whether the individual patient has already been assessed (green color), should be assessed within 2–3 days (yellow color), or needs to be assessed today (red color), individual physical therapists may be prompted and motivated to perform assessment timely. Moreover, steps to re-motivate physical therapists will be taken if adherence to outcome measures is unsatisfactory at a certain ward. Finally, feedback on the improvement of patients on a hospital level will be provided at relevant professional meetings.
Discussion
The Knowledge-to-Action Cycle was used to guide the implementation of four outcome measures. During a 6-month implementation period, experiences with the measures were gathered among physical therapists, and the implementation was evaluated and adjusted in accordance with the taxonomy for implementation outcomes by Proctor et al. The local physical therapists were expected to and did intend to use the four outcome measures. Six months after implementation, the acceptance among the physical therapists had increased but a substantial number still expressed some reluctance toward their use. Data from the electronic healthcare records corroborated interview findings, showing that the adoption and penetration of the new outcome measures procedures were not yet satisfying as the number of patients being correctly assessed surpassed the pre-defined threshold of 75% for only one outcome measure at one pre-defined time point.
Comparison with Previous Findings
Physical therapists expressed that standardized outcome measures could be motivating for patients as results quantified and illustrated their progress. Hereby, our findings are in line with other research in the field (Gubrium et al., 2003; Oyake et al., 2020). Some of the physical therapists also recognized the outcome measures as a way to ensure consistency through the rehabilitation process over time and across sectors. This corresponds to one of the Danish Health Authority's goals for the recommendation of specific outcome measures for acquired brain injury (Danmark, 2020).
One core idea in current rehabilitation research is to obtain standardized measurements of sensorimotor recovery at distinct time points to support comparability across treatment settings (Kwakkel et al., 2017; Moore et al., 2018). However, in the present setting, acceptability and appropriateness remained challenging, as many physical therapists expressed that the four measures neither fitted all patients nor facilitated rehabilitation. These findings are not unique as others have found that therapists do not routinely or systematically use standardized outcome measures in their clinical practice, but prefer to rely on their clinical judgment and the patient's verbal report (Jaeger Pedersen & Kaae Kristensen, 2016; Siegert, 2012). In the present study, some of the physical therapists expressed the concern that the compulsory introduction of standardized outcome measures limited their own clinical scope and was in contrast to their fundamental approach focusing on person-centered rehabilitation. To address these concerns, it is necessary to communicate that there should be no contradiction in standardized outcome measures and person-centered rehabilitation. However, the present study and the newly published Danish white book on rehabilitation confirm these challenges and dilemmas (Rehabiliteringsforum, 2022).
In the present setting, a persistent focus on the implementation and use of outcome measures is needed to ensure penetration and sustainability. This finding is corroborated by other studies, that confirm that the implementation of outcome measures can be a lengthy and tedious process (Alt Murphy et al., 2021; Jaeger Pedersen & Kaae Kristensen, 2016).
Methodological Considerations
Within implementation science, several frameworks and terminologies can be used to guide and evaluate implementation efforts (Damschroder et al., 2009; Moore et al., 2022; Proctor et al., 2011). A strength of the present study is the use of the Knowledge-to-Action cycle to guide the implementation process and knowledge translation. For standardization and ease of comparison with other studies, an implementation outcome taxonomy was used (Proctor et al., 2011). The combination of a process model supplemented by a specific outcome taxonomy provided a structure to identify crucial elements for implementation and helped to address barriers and evaluate the implementation (Bazeley, 2018; Moore et al., 2022; Nilsen, 2015; Proctor et al., 2011; Richards et al., 2019). When linking the implementation outcomes to the Knowledge-to-Action Cycle, it was clear that acceptability, appropriateness, and feasibility were the implementation outcomes most salient at the early Knowledge-to-Action phases, adoption and fidelity most salient at the early to mid-phases, while penetration and sustainability were salient in the late phases. This is in line with the implementation science literature, suggesting that studies usually capture fidelity during initial implementation, while penetration and sustainability will be more salient at the end of an implementation period (Proctor et al., 2011).
We applied the CFIR to take into account the different stakeholders of an implementation process. The focus of this study was on the inner setting. However, without preparatory work concerning the outer setting, the implementation would not have been possible. This includes obtaining approval and constant support from the hospital directors who assigned resources to the implementation process.
Focus group interviews constituted an important element in the present implementation. It has been emphasized that a successful implementation requires that clinicians consider an introduced change in practice as meaningful for themselves and their patients (Jaeger Pedersen & Kaae Kristensen, 2016; Varsi et al., 2015). In line with this, the first round of focus group interviews served to include and engage the therapists. Their beliefs and attitudes expressed in the interviews were used to make relevant adjustments to the implementation process.
Focus groups are an appropriate method to illuminate the norms and perceptions of groups (Krueger & Casey, 2015; Wilkinson, 1998) and to identify barriers. With these barriers addressed, the use of standardized outcome measures could be adapted to fit the local setting. In the present study, credibility was ensured by the involvement of several researchers with different positions and perspectives who could discuss and supplement each other in the analysis of focus group findings (Elo & Kyngas, 2008; Malterud, 2001; Ohman, 2005).
Data from the health care records could be included for 100% of all patients in rehabilitation at 6-month post-implementation. Thus, the fidelity toward the procedures and levels of penetration reflect reality. In contrast, only a subset of physical therapists participated in the focus group interview. A limitation of the present study might be if physical therapists with an interest in outcome measures or implementation have been more eager to participate in the focus group interviews. If so, the expressed perceptions may well be more positive than what is the case among therapists in general. On the other hand, therapists with a strong opinion against outcome measures may volunteer to support the status quo.
Perceived barriers and facilitators for the implementation of outcome measures depend on the clinical setting and will differ between sites (Damschroder et al., 2009). As a consequence, findings from the current study will not necessarily be generalizable to other settings. Nevertheless, the systematic use of an implementation strategy even before the start of implementation can be transferred to other contexts. Additionally, the clear and in-depth description of the implementation strategy can be generalized to other settings.
Future Directions
In the present setting, a persistent focus must be on the penetration and sustainability of the use of outcome measures. The pre-defined threshold of 75% for fidelity to testing procedures must be reached for all four outcome measures at all time points. Ideally, over time this threshold should be increased.
While most physical therapists focused on the usability of outcome measures in daily clinical routines, from a patient perspective, a seamless transfer over time and across healthcare sectors is crucial to optimize rehabilitation (Danmark, 2020). Consequently, we see the need to emphasize this aspect to aid clinicians to widen their perspective and acknowledge the importance. The communication of our results may help to foster the implementation of these and other outcome measures across health sectors as already recommended in national guidelines.
Using standardized outcome measures at pre-defined time points may aid the generation of high-quality research data from routinely gathered clinical data. This holds especially if the pre-defined time points are internationally acknowledged benchmarks for rehabilitation (Kwakkel et al., 2017). Hence, when the routinely collected data are used in future research projects this may strengthen a feeling of ownership among physical therapists and motivate for standardized documentation. Also, exploring the use and gains of the outcome measures during the entire rehabilitation process across healthcare sectors would be of interest.
Conclusion
Following the implementation period, most physical therapists acknowledged the benefits of the standardized assessment at pre-defined time points for all patients. The major barriers identified were time consumption, practical obstacles, and low perceived benefit. This was mirrored in the relatively low proportion of patients being timely assessed with the included measures. An ongoing focus should be on reducing practical obstacles and engaging physical therapists in discussions on how outcome measures may support clinical practice.
Data Availability
Anonymized transcribations of focus group data is available on request.
References
Alt Murphy, M., Björkdahl, A., Forsberg-Wärleby, G., & Persson, C. U. (2021). Implementation of evidence-based assessment of upper extremity in stroke rehabilitation: From evidence to clinical practice. Journal of Rehabilitation Medicine, 53(1), jrm00148. https://doi.org/10.2340/16501977-2790
Andersen, C. W., & Kristensen, M. T. (2019). Performance stability and interrater reliability of culturally adapted 10-meter walking test for danes with neurological disorders. Journal of Stroke and Cerebrovascular Diseases, 28(9), 2459–2467. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.06.021
Bazeley, P. (2018). Integrating analyses in mixed methods research (Vol. 1). Sage.
Benjamin, E. J., Virani, S. S., Callaway, C. W., Chamberlain, A. M., Chang, A. R., Cheng, S., Chiuve, S. E., Cushman, M., Delling, F. N., Deo, R., de Ferranti, S. D., Ferguson, J. F., Fornage, M., Gillespie, C., Isasi, C. R., Jiménez, M. C., Jordan, L. C., Judd, S. E., Lackland, D., & Muntner, P. (2018). Heart disease and stroke statistics-2018 update: A report from the american heart association. Circulation, 137(12), e67–e492. https://doi.org/10.1161/cir.0000000000000558
Cheng, D. K., Dagenais, M., Alsbury-Nealy, K., Legasto, J. M., Scodras, S., Aravind, G., Takhar, P., & Salbach, N. M. (2021). Distance-limited walk tests post-stroke: A systematic review of measurement properties. NeuroRehabilitation, 48(4), 413–439. https://doi.org/10.3233/NRE-210026
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science IS. https://doi.org/10.1186/1748-5908-4-50
Danmark, S. (2020). Anbefalinger til nationale redskaber til vurdering af funktionsevne - hos voksne med erhvervet hjerneskade. (Elektronisk ISBN: 978–87–7014–134–5). Retrieved from www.sst.dk
Elo, S., & Kyngas, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. https://doi.org/10.1111/j.1365-2648.2007.04569.x
Eng, J. J., Bird, M. L., Godecke, E., Hoffmann, T. C., Laurin, C., Olaoye, O. A., Solomon, J., Teasell, R., Watkins, C. L., & Walker, M. F. (2019). Moving stroke rehabilitation research evidence into clinical practice: Consensus-based core recommendations from the stroke recovery and rehabilitation roundtable. International Journal of Stroke, 14(8), 766–773. https://doi.org/10.1177/1747493019873597
Gubrium, J. F., Rittman, M. R., Williams, C., Young, M. E., & Boylstein, C. A. (2003). Benchmarking as everyday functional assessment in stroke recovery. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 58(4), S203-211. https://doi.org/10.1093/geronb/58.4.s203
Hafsteinsdottir, T. B., Rensink, M., & Schuurmans, M. (2014). Clinimetric properties of the timed up and go test for patients with stroke: A systematic review. Topics in Stroke Rehabilitation, 21(3), 197–210. https://doi.org/10.1310/tsr2103-197
Holden, M. K., Gill, K. M., Magliozzi, M. R., Nathan, J., & Piehl-Baker, L. (1984). Clinical gait assessment in the neurologically impaired. Reliability and Meaningfulness. Physical Therapy, 64(1), 35–40. https://doi.org/10.1093/ptj/64.1.35
Jaeger Pedersen, T., & Kaae Kristensen, H. (2016). A critical discourse analysis of the attitudes of occupational therapists and physiotherapists towards the systematic use of standardised outcome measurement. Disability and Rehabilitation, 38(16), 1592–1602. https://doi.org/10.3109/09638288.2015.1107630
Juckett, L. A., Wengerd, L. R., Banhos, M., & Darragh, A. R. (2022). Conducting implementation research in stroke rehabilitation: A case example and considerations for study design. Neurorehabilitation and Neural Repair, 36(12), 770–776. https://doi.org/10.1177/15459683221138747
Krishnamurthi, R. V., Ikeda, T., & Feigin, V. L. (2020). Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: A systematic analysis of the global burden of disease study 2017. Neuroepidemiology, 54(2), 171–179. https://doi.org/10.1159/000506396
Krueger, R., & Casey, M. (2015). Planning the focus group study. In: Focus groups: A Practical Guide for Applied Research. (5rd ed ed., pp. 19–37). SAGE Publications.
Kwakkel, G., Lannin, N. A., Borschmann, K., English, C., Ali, M., Churilov, L., Saposnik, G., Winstein, C., van Wegen, E. E., Wolf, S. L., Krakauer, J. W., & Bernhardt, J. (2017). Standardized measurement of sensorimotor recovery in stroke trials: Consensus-based core recommendations from the Stroke Recovery and Rehabilitation Roundtable. International Journal of Stroke : Official Journal of the International Stroke Society, 12(5), 451–461. https://doi.org/10.1177/1747493017711813
Lundquist, C. B., & Brunner, I. C. (2023). Cross-cultural adaptation of the Functional Ambulation Categories (FAC) in Danish patients with acquired brain injury. Disability and Rehabilitation, 1–8. https://doi.org/10.1080/09638288.2023.2261371
Lundquist, C. B., & Maribo, T. (2017). The Fugl-Meyer assessment of the upper extremity: Reliability, responsiveness and validity of the Danish version. Disability and Rehabilitation, 39(9), 934–939. https://doi.org/10.3109/09638288.2016.1163422
Malterud, K. (2001). Qualitative research: standards, challenges, and guidelines. Lancet (London, England), 358(9280), 483–488.
Maribo, T., Nielsen, J. F., & Nielsen, C. V. (2018). Wide variation in function level assessment after stroke in Denmark. Dan Med J, 65(10). https://www.ncbi.nlm.nih.gov/pubmed/30269746
Mehrholz, J., Wagner, K., Rutte, K., Meissner, D., & Pohl, M. (2007). Predictive validity and responsiveness of the functional ambulation category in hemiparetic patients after stroke. Archives of Physical Medicine and Rehabilitation, 88(10), 1314–1319. https://doi.org/10.1016/j.apmr.2007.06.764
Moore, J. L., Mbalilaki, J. A., & Graham, I. D. (2022). Knowledge translation in physical medicine and rehabilitation: A citation analysis of the knowledge-to-action literature. Archives of Physical Medicine and Rehabilitation, 103(7S), S256–S275. https://doi.org/10.1016/j.apmr.2020.12.031
Moore, J. L., Potter, K., Blankshain, K., Kaplan, S. L., O’Dwyer, L. C., & Sullivan, J. E. (2018). A core set of outcome measures for adults with neurologic conditions undergoing rehabilitation: A clinical practice guideline. Journal of Neurologic Physical Therapy, 42(3), 174–220. https://doi.org/10.1097/NPT.0000000000000229
Nilsen, P. (2015). Making sense of implementation theories, models and frameworks IS. Implementation Science. https://doi.org/10.1186/s13012-015-0242-0
Ohman, A. (2005). Qualitative methodology for rehabilitation research. Journal of Rehabilitation Medicine, 37(5), 273–280. https://doi.org/10.1080/16501970510040056
Oyake, K., Suzuki, M., Otaka, Y., Momose, K., & Tanaka, S. (2020). Motivational strategies for stroke rehabilitation: a delphi study. Archives of Physical Medicine and Rehabilitation, 101(11), 1929–1936. https://doi.org/10.1016/j.apmr.2020.06.007
Pohl, J., Held, J. P. O., Verheyden, G., Alt Murphy, M., Engelter, S., Floel, A., Keller, T., Kwakkel, G., Nef, T., Ward, N., Luft, A. R., & Veerbeek, J. M. (2020). Consensus-based core set of outcome measures for clinical motor rehabilitation after stroke-a delphi study. Frontiers in Neurology, 11, 875. https://doi.org/10.3389/fneur.2020.00875
Proctor, E. S. H., Raghavan, R., Hovmand, P., Aarons, G., Bunger, A., et al. (2011). Outcomes for implementation. Research: Conceptual distinctions, measurement challenges, and research agenda. Mental Health Services Research, 38, 65–76.
Proctor, E. K., Powell, B. J., & McMillen, J. C. (2013). Implementation strategies: Recommendations for specifying and reporting. Implementation Science, 8, 139. https://doi.org/10.1186/1748-5908-8-139
Rehabiliteringsforum, D. (2022). Hvidbog om rehabilitering (1 ed., Vol. 1.edt). Rehabiliteringsforum Danmark, Aarhus.
Richards, D. A., Bazeley, P., Borglin, G., Craig, P., Emsley, R., Frost, J., Hill, J., Horwood, J., Hutchings, H. A., Jinks, C., Montgomery, A., Moore, G., Plano Clark, V. L., Tonkin-Crine, S., Wade, J., Warren, F. C., Wyke, S., Young, B., & O’Cathain, A. (2019). Integrating quantitative and qualitative data and findings when undertaking randomised controlled trials. British Medical Journal Open, 9(11), e032081. https://doi.org/10.1136/bmjopen-2019-032081
Siegert, R. J. (2012). Outcome measurement in rehabilitation In: S. G. Dean (Ed.), Interprofessional Rehabilitation. A person-centered approach. (Vol. 1). Wiley-Blackwell.
Sundhedsstyrelsen. (2020). Anbefalinger for tværsektorielle forløb for voksne med erhvervet hjerneskade-apopleksi og transitorisk cerebral iskæmi (TCI) - traume, infektion, tumor, subarachnoidalblødning og encephalopati. Retrieved from ISBN: 978–87–7014–133–8
van Bloemendaal, M., van de Water, A. T., & van de Port, I. G. (2012). Walking tests for stroke survivors: A systematic review of their measurement properties. Disability and Rehabilitation, 34(26), 2207–2221. https://doi.org/10.3109/09638288.2012.680649
Varsi, C., Ekstedt, M., Gammon, D., & Ruland, C. M. (2015). Using the consolidated framework for implementation research to identify barriers and facilitators for the implementation of an internet-based patient-provider communication service in five settings: A qualitative study. Journal of Medical Internet Research, 17(11), e262. https://doi.org/10.2196/jmir.5091
Wilkinson, S. (1998). Focus groups in health research: Exploring the meanings of health and illness. Journal of Health Psychology, 3(3), 329–348. https://doi.org/10.1177/135910539800300304
Acknowledgements
We thank the focus group participants for sharing their time and reflections.
Funding
Open access funding provided by Central Region of Denmark. We have not received any funding for this study.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the article. Details: Authorship credit should be based on (1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical Approval
According to Danish Scientific Ethical Committee Region Midt Unit regulations and due to the nature of the study, the study was categorized as a quality assurance and development project and did not require ethical approval.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lundquist, C.B., Lillelund, S., Hansen, G.M. et al. Implementation of Standardized Outcome Measures for Motor Function in a Neurorehabilitation Hospital. Glob Implement Res Appl 4, 179–191 (2024). https://doi.org/10.1007/s43477-023-00103-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43477-023-00103-5